Published online Sep 6, 2022. doi: 10.12998/wjcc.v10.i25.9121
Peer-review started: April 13, 2022
First decision: May 31, 2022
Revised: June 13, 2022
Accepted: July 25, 2022
Article in press: July 25, 2022
Published online: September 6, 2022
Processing time: 134 Days and 1.8 Hours
Radiation therapy (RT) for nasopharyngeal cancer can cause several complications. In rare cases, an internal carotid artery pseudoaneurysm can occur, which can be fatal. We report the experience of a nasopharyngeal cancer patient who underwent radiation therapy and subsequently developed a fatal pseudoaneurysm of the petrous internal carotid artery.
A 39-year-old man was diagnosed with nasopharyngeal cancer 2 years ago (American Joint Committee on Cancer Stage T3N2M0) and received concurrent chemoradiation therapy. He subsequently relapsed and received chemotherapy. One week after the 4th cycle of chemotherapy, he was admitted to the emergency room of our hospital because of massive epistaxis accompanied by a headache. A pseudoaneurysm of the petrous internal carotid artery was confirmed by digital subtraction angiography (DSA). Stent-assisted endovascular coil embolization was performed and complete occlusion was achieved. No pseudoaneurysm was observed on DSA after coil embolization; however, intermittent epistaxis was maintained even after coil embolization. After seven days, a diagnostic laryn
This case highlights a rare, serious complication of RT in nasopharyngeal cancer and how it should be recognized and treated.
Core Tip: We report a patient who developed pseudoaneurysm in a nasopharyngeal cancer patient. By reporting our mistakes, we hope that our readers will not make the same mistakes as us.
- Citation: Park JS, Jang HG. Endovascular treatment of a ruptured pseudoaneurysm of the internal carotid artery in a patient with nasopharyngeal cancer: A case report. World J Clin Cases 2022; 10(25): 9121-9126
- URL: https://www.wjgnet.com/2307-8960/full/v10/i25/9121.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i25.9121
Nasopharyngeal cancer (NPC) is a major type of head and neck cancer[1]. The main treatment for this cancer is radiation therapy[2]. However, radiation therapy destroys the normal tissues surrounding the tumor, which can lead to complications such as mucositis, dry mouth, dysphagia, hearing and visual loss, throat problems, neurological damage, carotid artery stenosis, and nasal or nasopharyngeal bleeding[3]. A pseudoaneurysm of the internal carotid artery (ICA), which is a serious complication of radiation therapy in NPC patients, can cause massive epistaxis with high mortality[4]. We report the experience of a NPC patient who underwent radiation therapy and subsequently developed a fatal pseudoaneurysm of the petrous ICA.
A 41-year-old man had an epistaxis.
A 41-year-old man was admitted to the emergency department of our hospital for epistaxis, accompanied by a headache.
The patient was diagnosed on the 31st April 2019 with NPC stage T2N2M0 and underwent concurrent chemoradiation therapy at a total radiation dose of 67.2 Gy/28 frs. The cancer recurred a year later, and salvage radiation therapy and chemotherapy were administered. One week after the 4th cycle of chemotherapy, he was admitted to the emergency department of our hospital.
This patient had no special personal or family history.
There were no specific findings on physical examination other than epistaxis.
There were no specific findings on laboratory test.
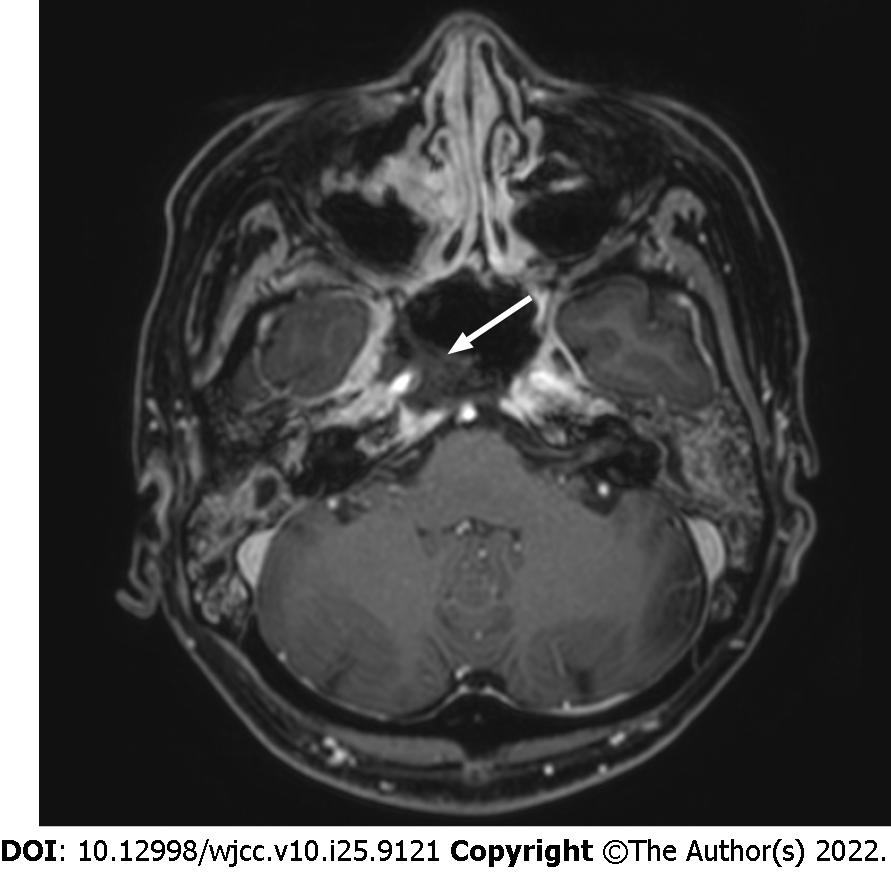
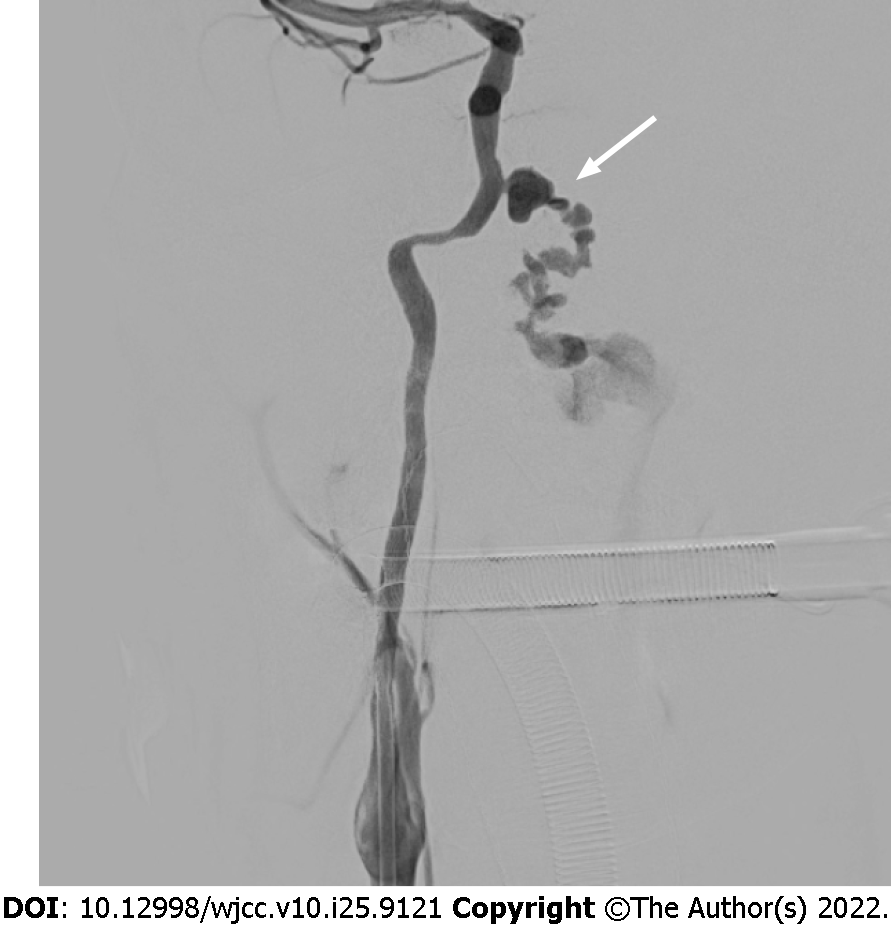
We performed a nasopharyngeal magnetic resonance imaging, which showed destruction of the petrous bone, sphenoid sinus floor, and clivus. In addition, necrosis of the soft tissues from the nasopharynx to the oropharynx, including the ICA was observed (Figure 1). Digital subtraction angiography (DSA) was performed for embolization because epistaxis occurred continuously. Incidentally, angiography of the right ICA revealed a ruptured 9 mm × 5 mm pseudoaneurysm in the petrous (Figure 2). Subsequently, stent-assisted endovascular coil embolization was planned.
The final diagnosis of the presented case was a pseudoaneurysm in an NPC patient caused by radiation treatment.
Vaseline gauze packing was performed as an emergency measures, but a small amount of bleeding continued to occur. The patient developed massive epistaxis during general anesthesia preparation for coil embolization. Under general anesthesia, after a right femoral artery puncture, an 80 cm 7F guide catheter was advanced to the right cervical portion of the ICA. A 6-Fr soft torque able catheter optimized for intracranial access was inserted into the cervical segment of the right ICA under roadmap guidance.
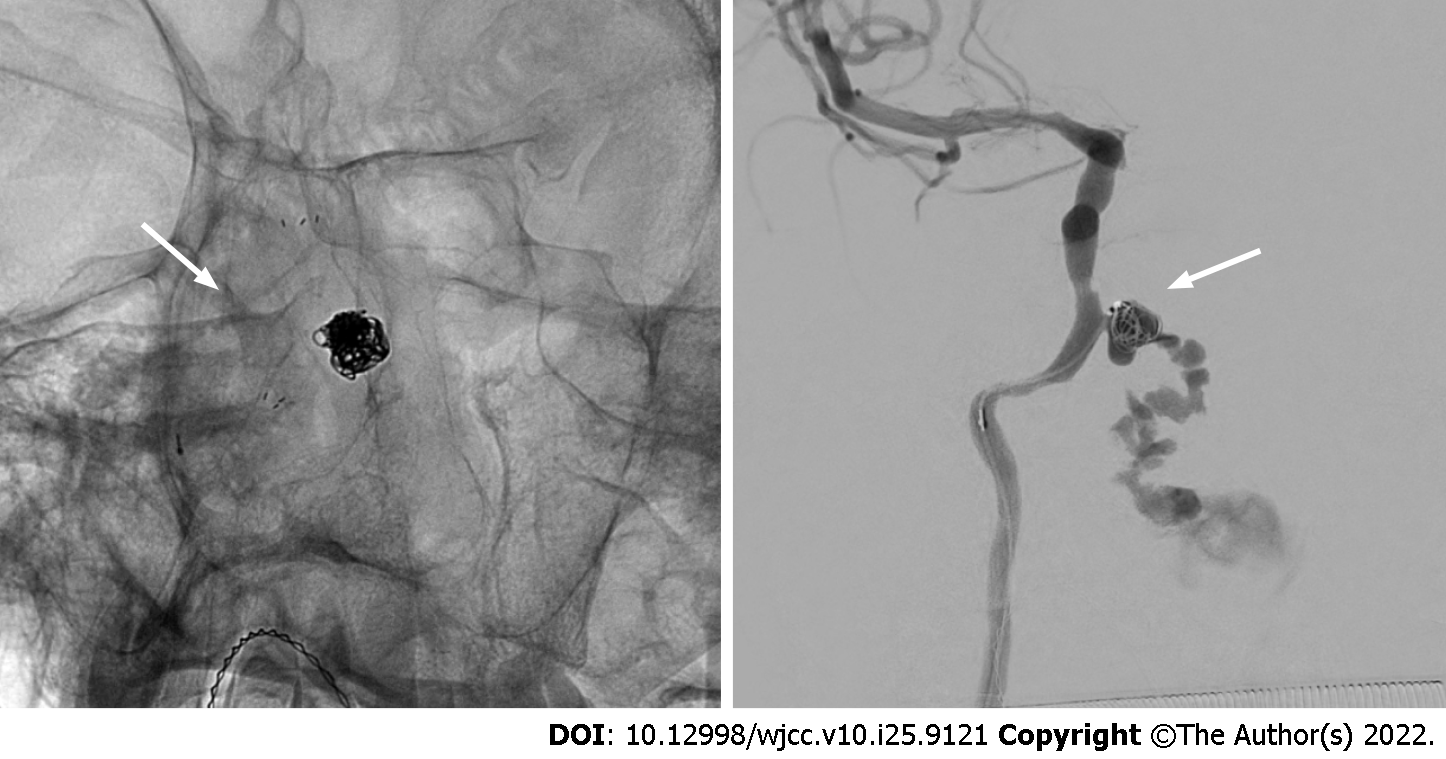
Using roadmap guidance again, a Headway 17 for coil delivery was inserted into the aneurysm sac. Then, a Headway 21 microcatheter was navigated to a carotid segment of right ICA to deliver the stent. After this, a Neuroform Atlas 4.0 mm × 21 mm stent was deployed from the distal to the proximal petrous ICA. After the stent was fully installed, coil embolization was initiated. A Guglielmi’s detachable coil was placed into the aneurysm (Figure 3). The procedure was carried out by pulling out the microcatheter slightly, while identifying the patency of the parent artery. Coils encroaching into the stent were not allowed throughout the procedure. However, bleeding was observed continuously, even after coil packing. While inserting the coil into the initially installed stent located at the orifice of the pseudoaneurysm, we additionally installed a self-expanding closed-cell low-profile visualized intraluminal support jr 3.5 mm × 18 mm stent (Figure 4).
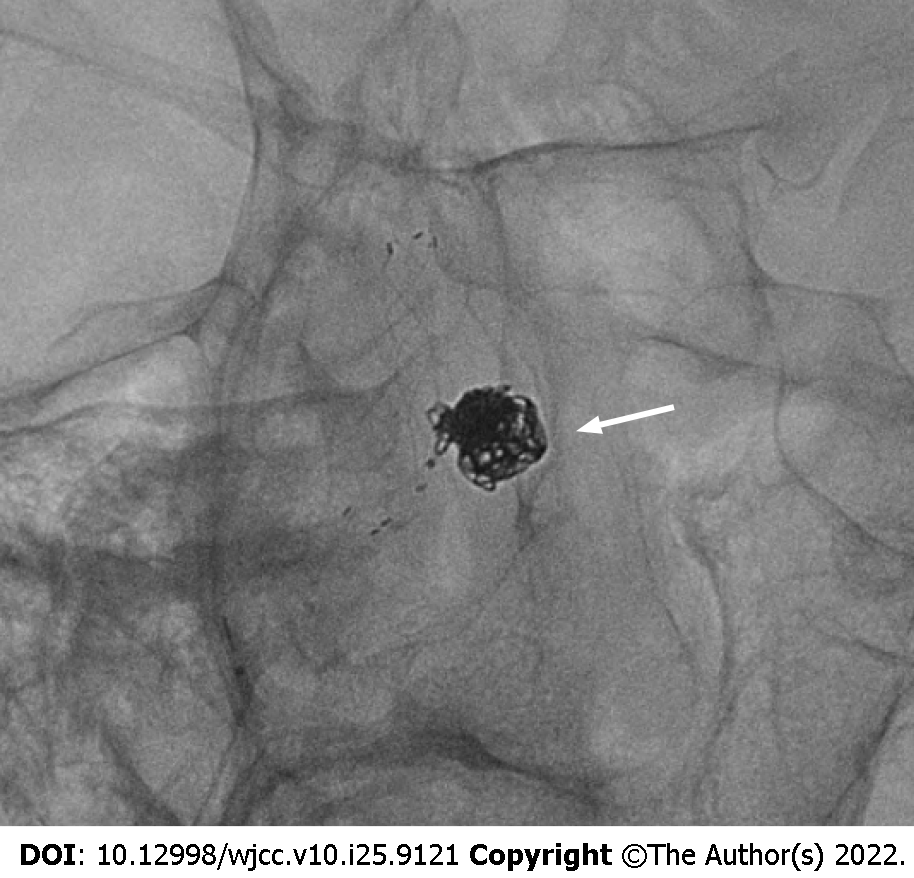
A final angiographic image showed that bleeding was no longer observed, and that the epistaxis that persisted during the intervention was also relieved (Figure 5). No pseudoaneurysm was observed on DSA after coil embolization; however, intermittent epistaxis continued to occur even after coil embolization. After seven days, a diagnostic laryngoscopy was performed.
Massive bleeding occurred after aspiration of the blood clot during the laryngoscopy. The patient subsequently died of hypovolemic shock.
NPC is a relatively common malignant tumor, mainly treated with a combination of chemotherapy and radiation therapy[2]. Radiation therapy is one of the most effective treatments for NPC. However, its side effects include erythema, erosion, ulceration in the skin and mucosa, and in more severe cases, necrosis of the bone and cartilage[3]. One of the most severe complications that can occur is the rupture of major blood vessels, which was first reported in 1959 by Thomas and Forbus[5]. This usually occurs in the petrous and lacerum segments of the ICA and may present with life-threatening epistaxis. Therefore, it is a major post-treatment complication of NPC[6].
The mechanism of radiation-induced vascular injury is not fully understood, but may result from obliteration of the vasa vasorum, premature atherosclerosis, and weakening and necrosis of the arterial wall. Ischemic injury combined with peri-adventitial fibrosis may contribute to the rupture of irradiated large arteries and pseudoaneurysm formation[7]. In these patients, epistaxis can characteristically be observed when a pseudoaneurysm ruptures. The patient in this case also experienced epistaxis and was admitted to the emergency room.
Although our patient had epistaxis, we did not consider it as a symptom of a ruptured pseudoaneurysm. Initially, DSA was performed for embolization of the arterial branches of the external carotid artery, which have the potential to cause epistaxis. However, an unexpected pseudoaneurysm in the petrous ICA was found in the DSA. Only then was it possible to infer that the cause of the epistaxis was radiation-induced rupture of the pseudoaneurysm. Obliteration of the pseudoaneurysm was achieved by embolization; however, the patient had persistent epistaxis and after a careless laryngoscopy that may have been unnecessary, the patient experienced massive rebleeding epistaxis.
Many things were noted throughout the experience of this rare case. First, treatment should have been initiated considering the possibility of an ICA pseudoaneurysm, the most dangerous cause of epistaxis in NPC patients with a history of radiation therapy. Although obliteration of the pseudoaneurysm was confirmed after treatment, it is questionable whether this was the best line of treatment as the decision-making process was made in urgency. Second, due to the characteristics of pseudoaneurysms, a short-term imaging follow-up should have been performed. In addition, a small amount of epistaxis persisted even after coil embolization suggesting regrowth or recanalization of the pseudoaneurysm. If this was recognized in advance, additional treatments could have been implemented. Third, there was an unnecessary and careless laryngoscopy performed. Greater attention should have been paid to the process, and a DSA should have been re-executed rather than a laryngoscopy.
Pseudoaneurysms in NPC is a rare but fatal complication of radiotherapy. In this case, the occurrence of epistaxis may have been a sign of pseudoaneurysm; therefore, in these cases treatment such as embolization should be performed promptly, with careful management being carried out thereafter.
| 1. | Chou J, Lin YC, Kim J, You L, Xu Z, He B, Jablons DM. Nasopharyngeal carcinoma--review of the molecular mechanisms of tumorigenesis. Head Neck. 2008;30:946-963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 248] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 2. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 68648] [Article Influence: 13729.6] [Reference Citation Analysis (201)] |
| 3. | Chua MLK, Wee JTS, Hui EP, Chan ATC. Nasopharyngeal carcinoma. Lancet. 2016;387:1012-1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 787] [Cited by in RCA: 1015] [Article Influence: 101.5] [Reference Citation Analysis (0)] |
| 4. | Nazari P, Tan LA, Wewel JT, Moftakhar R, Kasliwal MK. Massive epistaxis resulting from radiation-induced internal carotid artery pseudoaneurysm. Neurol India. 2017;65:380-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | THOMAS E, FORBUS WD. Irradiation injury to the aorta and the lung. AMA Arch Pathol. 1959;67:256-263. [PubMed] |
| 6. | Hanada Y, Sasai H, Kamakura A, Nakamura M, Sakata Y, Miyahara H. [Rupture of an internal carotid artery pseudoaneurysm after irradiation for a nasopharyngeal carcinoma--case report]. Nihon Jibiinkoka Gakkai Kaiho. 2013;116:606-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Okamura HO, Kamiyama R, Takiguchi Y, Kimizuka K, Ishikawa N, Kishimoto S. Histopathological examination of ruptured carotid artery after irradiation. ORL J Otorhinolaryngol Relat Spec. 2002;64:226-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Oura S, Japan; Wang YJ, China S-Editor: Liu JH L-Editor: A P-Editor: Liu JH