Published online Sep 6, 2022. doi: 10.12998/wjcc.v10.i25.9028
Peer-review started: March 23, 2022
First decision: May 30, 2022
Revised: July 11, 2022
Accepted: August 1, 2022
Article in press: August 1, 2022
Published online: September 6, 2022
Processing time: 156 Days and 8.9 Hours
A large ganglionic cyst extending from the hip joint to the intrapelvic cavity through the sciatic notch is a rare space-occupying lesion associated with compressive lower-extremity neuropathy. A cyst in the pelvic cavity compressing the intrapelvic-sciatic nerve is easily missed in the diagnostic process because it usually presents as atypical symptoms of an extraperitoneal-intrapelvic tumor. We present a case of a huge ganglionic cyst that was successfully excised laparoscopically and endoscopically by a gynecologist and an orthopedic surgeon.
A 52-year-old woman visited our hospital complaining of pain and numbness in her left buttock while sitting. The pain began 3 years ago and worsened, while the numbness in the left lower extremity lasted 1 mo. She was diagnosed and unsuccessfully treated at several tertiary referral centers many years ago. Magnetic resonance imaging revealed a suspected paralabral cyst (5 cm × 5 cm × 4.6 cm) in the left hip joint, extending to the pelvic cavity through the greater sciatic notch. The CA-125 and CA19-9 tumor marker levels were within normal limits. However, the cyst was compressing the sciatic nerve. Accordingly, endoscopic and laparoscopic neural decompression and mass excision were performed simultaneously. A laparoscopic examination revealed a tennis-ball-sized cyst filled with gelatinous liquid, stretching deep into the hip joint. An excisional biopsy performed in the pelvic cavity and deep gluteal space confirmed the accumulation of ganglionic cysts from the hip joint into the extrapelvic intraperitoneal cavity.
Intra- or extra- sciatic nerve-compressing lesion should be considered in cases of sitting pain radiating down the ipsilateral lower extremity. This large juxta-articular ganglionic cyst was successfully treated simultaneously using laparoscopy and arthroscopy.
Core Tip: A huge juxta-articular ganglionic cyst originating from the hip joint, passing through the sciatic notch, and growing in the intrapelvic cavity is likely to exhibit sciatic nerve compression symptoms. The authors report a case in which laparoscopy and arthroscopy were performed simultaneously to treat the ganglionic cyst.
- Citation: Choi WK, Oh JS, Yoon SJ. Simultaneous laparoscopic and arthroscopic excision of a huge juxta-articular ganglionic cyst compressing the sciatic nerve: A case report. World J Clin Cases 2022; 10(25): 9028-9035
- URL: https://www.wjgnet.com/2307-8960/full/v10/i25/9028.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i25.9028
Ganglion cyst is the most common type of mass lesion around the hip joint[1]. However, a large ganglionic cyst extending from the hip joint to the intrapelvic cavity through the sciatic notch is a rare cystic form associated with buttock pain in musculoskeletal disorders[2,3].
Sciatica secondary to intrapelvic cystic lesions is a rare. A cystic lesion in the pelvic cavity com
Here, we present the case of a 52-year-old woman with sciatica caused by a large ganglionic cyst that was treated collaboratively by an orthopedic surgeon and gynecologist using simultaneous endoscopic and laparoscopic approaches. To our knowledge, this is the first report of concomitant removal of a huge ganglion cyst extending the hip joint to the pelvic cavity using laparoscopy and arthroscopy.
A 52-year-old woman visited our clinic complaining of pain in the left hip and numbness in the lower extremity of the ipsilateral side when sitting or walking.
The left pelvic and posterior hip pain began 3 years prior and worsened, while the radiating pain to the entire ipsilateral lower extremity increased in intensity over 3 mo.
She was previously diagnosed with a paraovarian cyst and was continuously followed up in the gynecologic department at a tertiary referral hospital. However, her symptoms did not improve, despite various conservative treatments.; She was, therefore, referred to another obstetrics and gynecology department of another tertiary university hospital for operative treatment.
Diagnostic pelviscopy and laparoscopic adnexectomy were performed. However, no specific findings that could cause pain in the female organs were observed during the former procedure; hence, the operation was terminated. She was told that the current symptoms were not seemingly related to gynecologic problems, so she visited our orthopedic surgery department.
The patient had no significant medical history. No specific genetic diseases were found in the family history.
A bimanual pelvic examination revealed a fixed mass measuring 5 cm × 5 cm × 4 cm that was adherent to the left pelvic wall. An orthopedic physical examination revealed severe tenderness of the left buttock. She complained about being unable to sit for 5 minutes because of intense pain and tenderness in the area. She did not, however, experience any sensations.
Serum tumor markers levles were normal (cancer antigen 125, 11.7 U/mL; cancer antigen 19-9, 30 U/mL). No abnormalities was found in the routine blood and urine analyses.
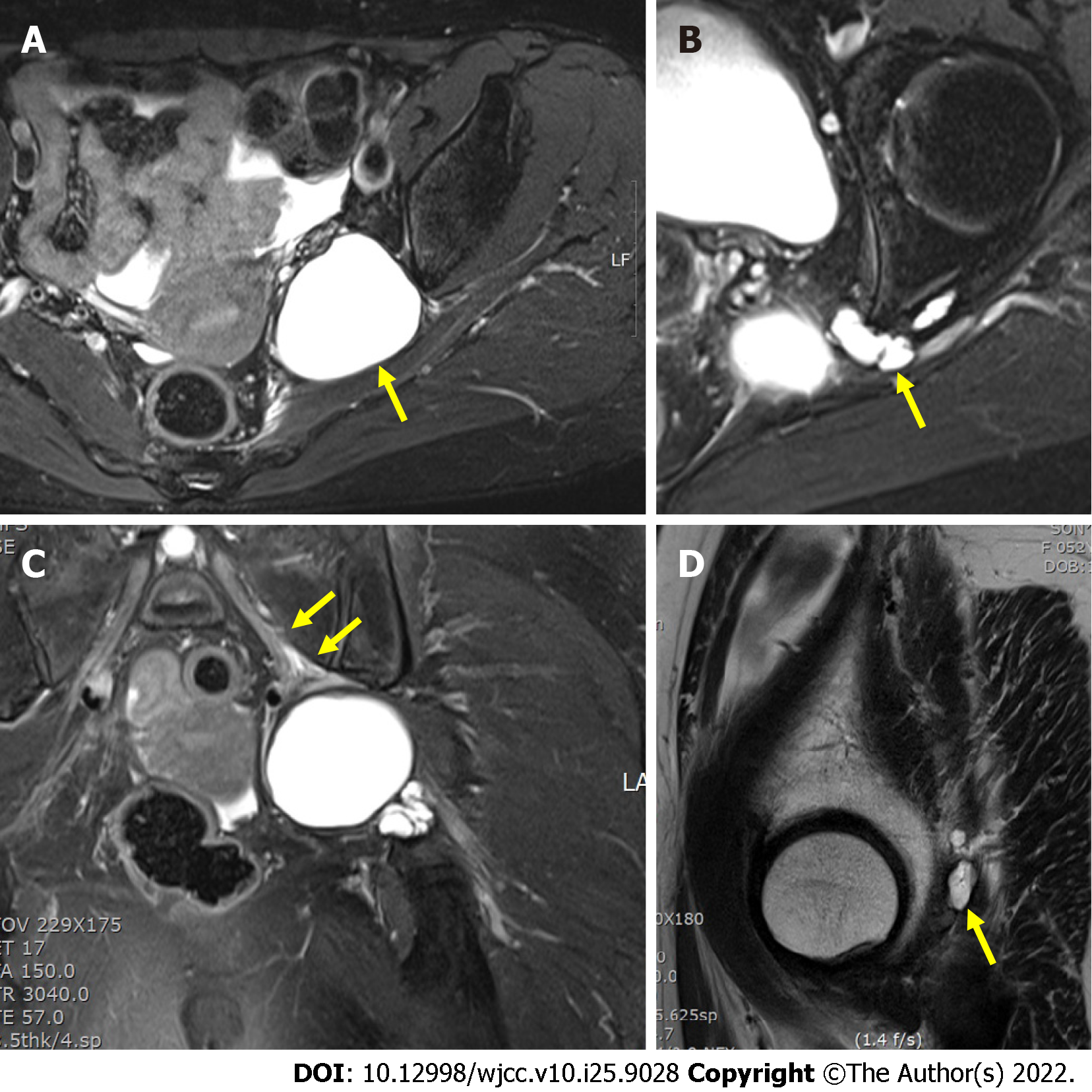
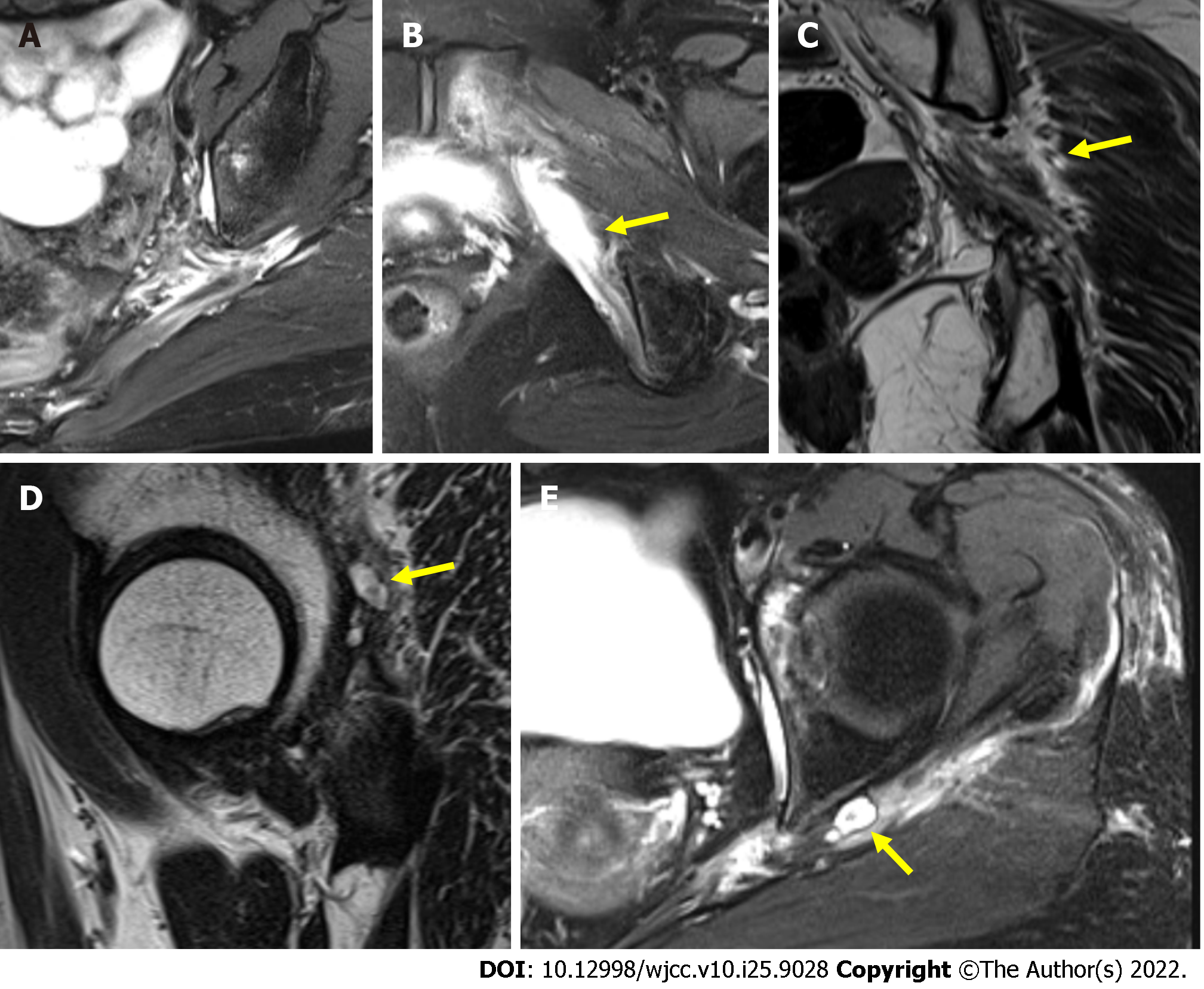
Magnetic resonance imaging (MRI) revealed a huge paralabral cyst 5 cm × 5 cm × 4.6 cm stretched to the greater sciatic notch from the left hip joint (Figure 1). However, the cyst was located close to the sciatic nerve and adhered to the piriformis muscle's intrapelvic portion. Following her admission, she was referred to our hospital’s gynecology and neurology departments to ensure a multidisciplinary approach.
We decided to consult the neurology department for the electromyography and nerve conduction studies. The study revealed a mild left sciatic nerve lesion, and the physician recommended a clinical correlation. Accordingly, a laparoscopic examination revealed a tennis ball-sized cystic mass filled with gelatinous liquid stretching deep into the hips, with internal and external iliac vessels. The mass was located below the obturator nerve in the left retroperitoneal space. The mass contained yellowish, sticky, and gelatinous components and was firmly adherent to the surrounding tissues.
The mass was ultimately diagnosed as a juxatarticular ganglionic cyst originating from the hip joint passing through the sciatic notch and growing in the intrapelvic cavity.
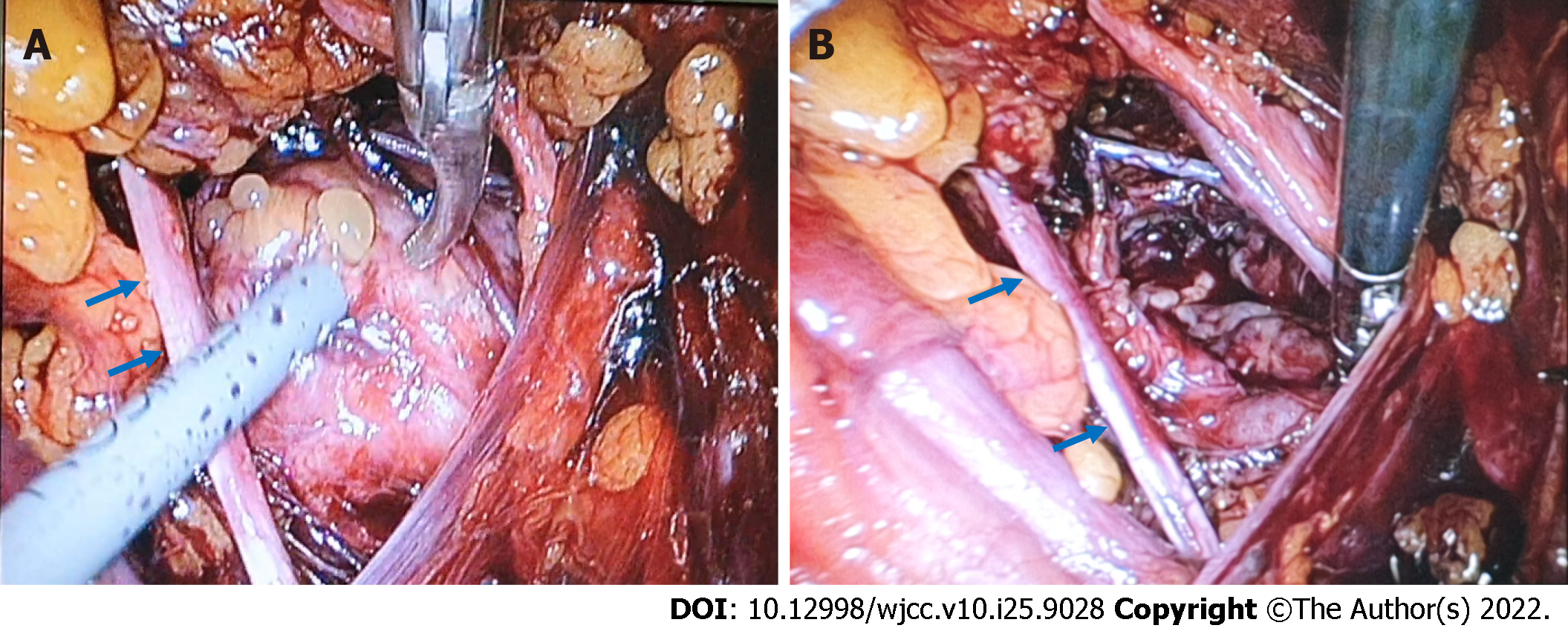
Diagnostic laparoscopy combined with arthroscopy was performed to decompress the sciatic nerve from the intrapelvic cavity to the extrapelvic deep gluteal space. Incomplete decompression of only one space leads to symptomatic relief. The ganglionic materials were aspirated, the cyst was decompressed, and the cyst capsule was excised for histological examination. A tennis ball-sized cystic lesion with yellowish-thick gelatinous fluid was densely adherent to the adjacent nerve (Figure 2).
Laparoscopic findings revealed no visible intraperitoneal cysts. However, cystic bulging was observed in the left ovarian fossa. We opened a broad ligament to approach the retroperitoneal space and identified a tennis ball-sized cystic mass below the obturator nerve. We identified the boundary of the cystic mass by excising the surrounding connective tissue and found that it was densely adherent to the sciatic nerve below the cyst.
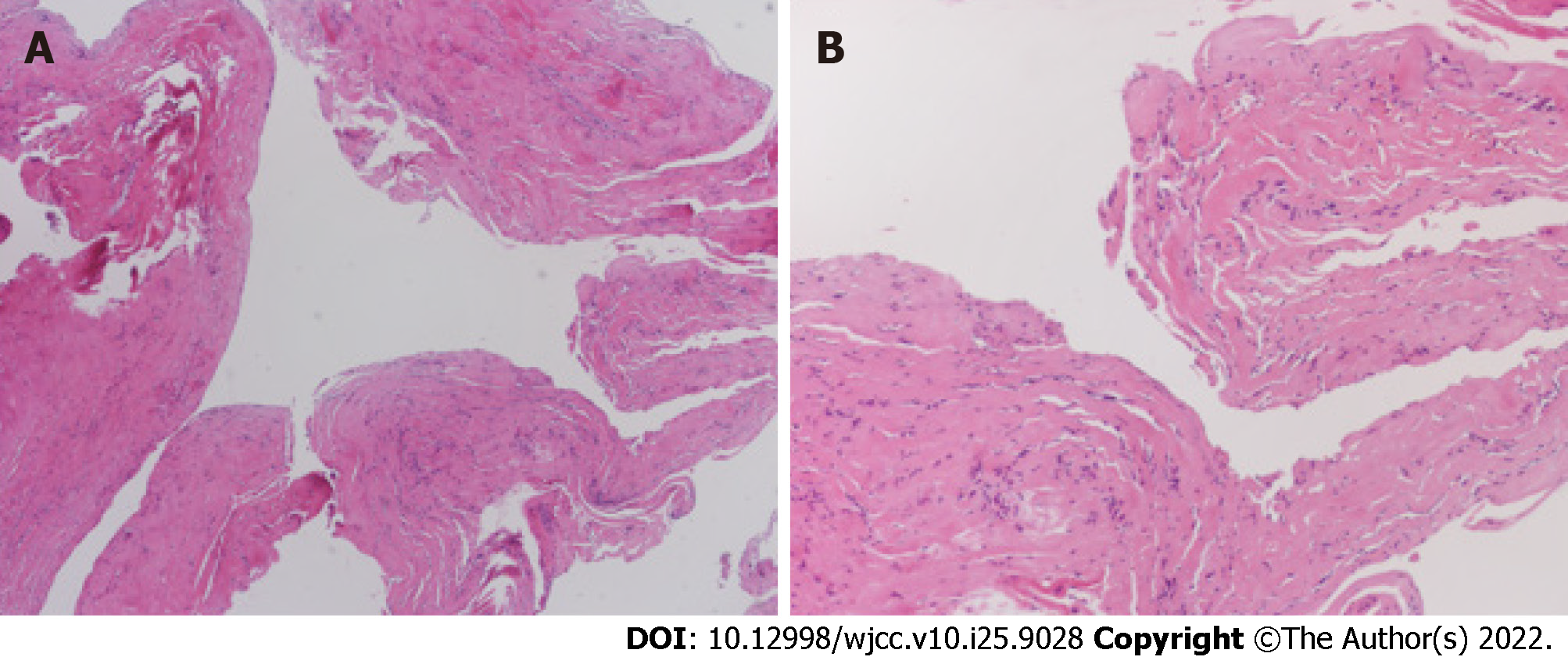
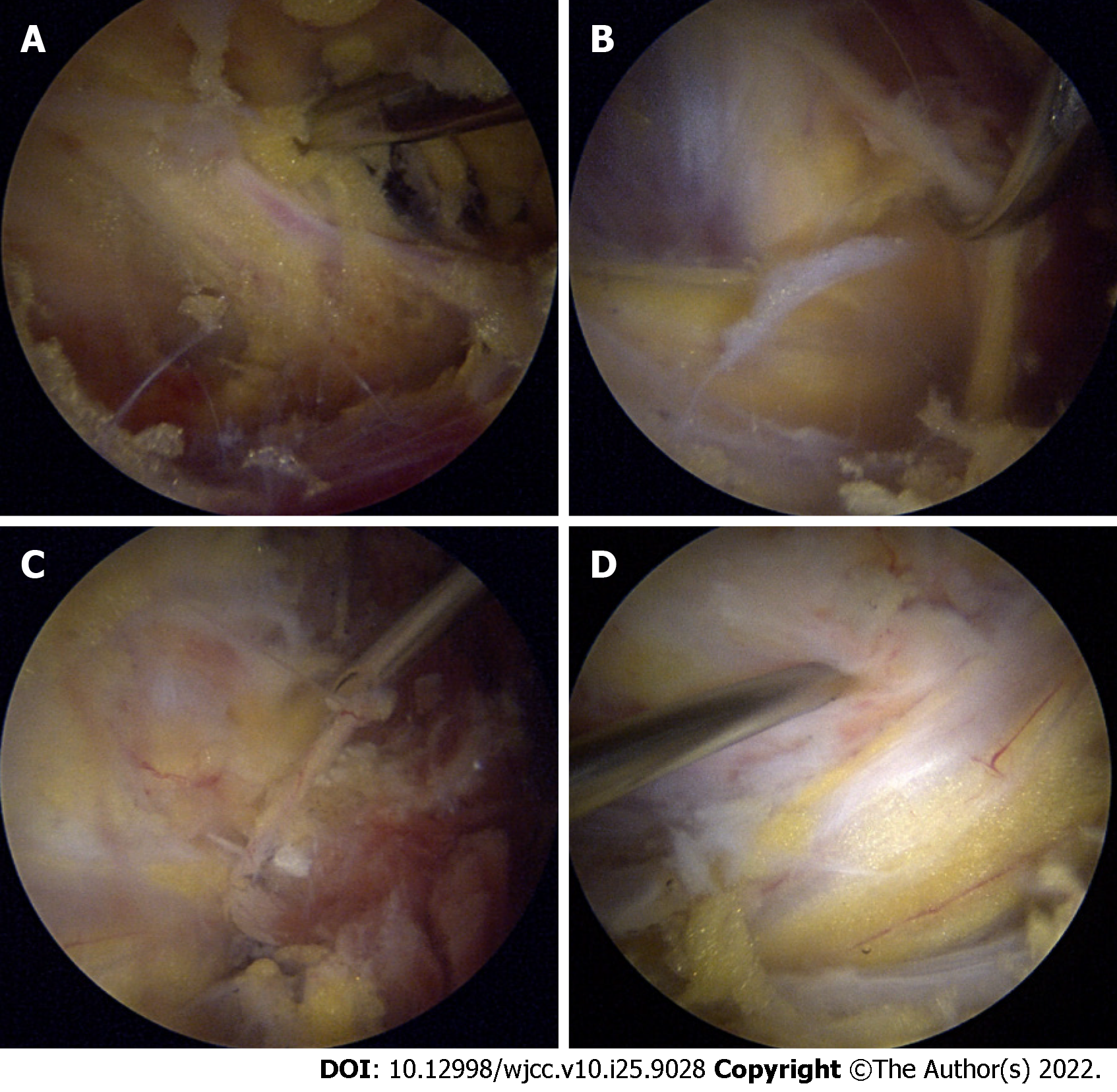
Frozen biopsy was performed intraoperatively to confirm the presence of a ganglionic cyst (Figure 3). Postoperative pathology confirmed the diagnosis of the ganglionic cyst. Diagnostic arthroscopy and endoscopic sciatic nerve decompression were simultaneously performed. A large ganglionic cyst was observed between the greater sciatic notch and the acetabular posterior wall near the left sciatic nerve. The cystic lesion mildly compressed the sciatic nerve. However, its continuity was intact (Figure 4).
The patient’s sitting pain and numbness improved immediately after the surgery. Postoperative MRI also showed that the cyst was nearly completely resected, but mild edematous changes persisted owing to chronic compression (Figure 5). Long-term follow-up observations showed persistent pain relief and neurological recovery.
In this study, as levels of both cancer markers CA 125 and CA 19-9 were within the normal range, we were able to outweigh the possibility of adnexal or ovarian malignancy. We performed two cancer marker tests in this study: CA 125 and 19-9. CA 125 is the most commonly used serum biomarker for epithelial ovarian cancer (EOC) for monitoring treatment response in patients with known EOC. It is also used alone or in combination with other serum biomarkers and/or intra-pelvic ultrasound to evaluate an adnexal mass. A mucin protein that is usually used to monitor treatment response of pancreatic cancer, gallbladder cancer, cholangiocarcinoma, or ampulla of Vater cancer, CA 19-9 is used additionally in ovarian cancer management and might be elevated in the adnexal tumor.
A ganglion cyst is typically found near large joints, including the hip, shoulder, and knee. Only a few reports have described the compression of neurovascular structures caused by pelvic cavity cysts, with the hip joint being less commonly affected than the others[8].
Elevated intra-articular pressure is required in the hip joint to force synovial fluid into the acetabulum or surrounding soft tissue, which can cause a paralabral ganglion cyst[9,10]. The initial chief complaint of this patient with hypesthesia in the left buttock and numbness in the left lower limb, suggestive of sciatica was the first impression. This case emphasizes that the presentation of symptoms attributable to peripheral neuropathy should raise the suspicion of another cause of these symptoms.
As the cyst grew larger 2 years prior, progressively compressing the sciatic nerve, the patient’s symptoms became more intense. The patient visited the gynecology department of another hospital but was told she did not have a gynecologic cause. She then visited other local orthopedic clinics and was given a probable diagnosis through MRI. She was referred to the gynecological department of our hospital for treatment by an orthopedic surgeon, gynecologist, or general surgeon.
Ultrasonography-guided cyst aspiration can help manage the mass effect of the cyst. However, considering the risk of incomplete evacuation and recurrence, Pachore et al[11] suggested that this should be considered only in patients who underwent minimally invasive procedures and refused any surgical intervention. Given the high rate of recurrence rate after conservative treatment, complete excision is recommended to eliminate the possibility of recurrence[12].
Hip arthroscopy revealed that, the proximity was close to the sciatic notch during sciatic nerve decompression in the deep gluteal space. In addition, if the operation time for arthroscopic sciatic nerve decompression is prolonged, abdominal compartment syndrome may occur because of fluid extravasation. Therefore, simultaneous laparoscopic decompression was required for the intrapelvic ganglionic cyst in this patient, justifying the combined approach.
Orthopedic surgeons and gynecologists believe that surgical cyst resection is necessary. Therefore, complete excision of the cystic mass and neurolysis of the sciatic nerve were performed laparoscopically by a gynecologist and arthroscopically by an orthopedic surgeon. Diagnostic pelviscopy and laparoscopy-assisted cyst resection were performed by a gynecologist who was familiar with the intrapelvic laparoscopic anatomy. An orthopedic surgeon performed extrapelvic cyst removal, including sciatic nerve decompression, via transgluteal arthroscopy. This cooperation provided good results, and the prognosis was also good for the patient.
Chronic pelvic pain is defined as non-cyclic pelvic pain that persists for 6 mo[13]. Its causes are extensive, including urogenital, gastrointestinal, neuromusculoskeletal, and psychosocial aetiologies, and may occur in combination. In patients with chronic pelvic pain accompanying hip pain, visceral pathologies such as uterine fibroids, ovarian tumors, endometriosis, or pelvic congestion syndrome should be differentiated using imaging tests. If no pelvic abnormalities are identified, accurate history-taking and physical examination, including examination of the pelvic floor musculature, can help diagnose the etiology. However, even if visceral pathology is identified, a neuromusculoskeletal etiology should not be excluded if the pattern of chronic pelvic pain does not match its course.
A space-occupying lesion leading to sciatic nerve compression should be considered as a potential etiology when a woman complains of unexplained sitting pain, especially pain that radiates to the ipsilateral lower extremity. The physician should suspect this type of disease if a patient has a gynecological history.
We reviewed two case reports on juxta-articular ganglion cysts in South Korea[13]. All patients experienced pain in the lower extremities, a common symptom of sciatica. Park et al[2] presented two patients with radiating pain in the ipsilateral lower leg. Lee et al[13] presented three patients with pain radiating to the posterior aspect of the lower limb, soreness, and foot numbness. In both studies, the researchers treated the patients with arthroscopic cyst resection. None of these cases included ganglion cysts that communicated between the intra- and extrapelvic cavities. The international etiology is well described in a case report by Lee et al[14].
The huge intra- and extrapelvic ganglion involving the lumbosacral trunk could be misdiagnosed as sciatica. When a physician encounters a patient with a gynecologic history who complains of buttock pain, ipsilateral lower limb numbness, or radiating pain, the high suspicion of a space-occupying lesion compressing the adjacent nerve is recommended. This huge juxta-articular ganglionic cyst was successfully treated simultaneously using laparoscopy and arthroscopy.
| 1. | Hwang DS, Noh CK. Comprehensive Review of Advancements in Hip Arthroscopy. Hip Pelvis. 2017;29:15-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Park JH, Jeong HJ, Shin HK, Park SJ, Lee JH, Kim E. Piriformis ganglion: An uncommon cause of sciatica. Orthop Traumatol Surg Res. 2016;102:257-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Yanchun L, Yunhe Z, Meng X, Shuqin C, Qingtang Z, Shuzhong Y. Removal of an endometrioma passing through the left greater sciatic foramen using a concomitant laparoscopic and transgluteal approach: case report. BMC Womens Health. 2019;19:95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Ham DH, Chung WC, Jung DU. Effectiveness of Endoscopic Sciatic Nerve Decompression for the Treatment of Deep Gluteal Syndrome. Hip Pelvis. 2018;30:29-36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Martin HD, Reddy M, Gómez-Hoyos J. Deep gluteal syndrome. J Hip Preserv Surg. 2015;2:99-107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 6. | Park MS, Jeong SY, Yoon SJ. Endoscopic Sciatic Nerve Decompression After Fracture or Reconstructive Surgery of the Acetabulum in Comparison With Endoscopic Treatments in Idiopathic Deep Gluteal Syndrome. Clin J Sport Med. 2019;29:203-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Yoon SJ, Park MS, Matsuda DK, Choi YH. Endoscopic resection of acetabular screw tip to decompress sciatic nerve following total hip arthroplasty. BMC Musculoskelet Disord. 2018;19:184. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Briem T, Haemmerle G, Kramers-de Quervain I, Leunig M. Synovial Ganglion of the Hip as a Rare Cause of L5 Radiculopathy: A Case Report. JBJS Case Connect. 2016;6:e59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Kim SH, Seok H, Lee SY, Park SW. Acetabular paralabral cyst as a rare cause of obturator neuropathy: a case report. Ann Rehabil Med. 2014;38:427-432. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Jones HG, Sarasin SM, Jones SA, Mullaney P. Acetabular paralabral cyst as a rare cause of sciatica. A case report. J Bone Joint Surg Am. 2009;91:2696-2699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Pachore JA, Shah VI, Upadhyay S, Shah K, Seth A, Kshatriya A. Compressive Femoral Mononeuropathy Secondary to Acetabular Labral Tear Associated With Paralabral Ganglion Cyst of an Osteoarthritic Hip: A Case Report. JBJS Case Connect. 2019;9:e0344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Pachore JA, Shah VI, Upadhyay S, Shah K, Seth A, Kshatriya A. Compressive Femoral Mononeuropathy Secondary to Acetabular Labral Tear Associated With Paralabral Ganglion Cyst of an Osteoarthritic Hip: A Case Report. JBJS Case Connect. 2019;9:e0344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Chronic Pelvic Pain: ACOG Practice Bulletin, Number 218. Obstet Gynecol. 2020;135:e98-e109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 111] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 14. | Lee WY, Hwang DS, Kang C, Zheng L. Entrapment Neuropathy of the Sciatic Nerve Caused by a Paralabral Cyst: Three Cases Treated Arthroscopically: A Case Report. JBJS Case Connect. 2016;6:e82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jian X, China; Shariati MBH, Iran S-Editor: Wang LL L-Editor: A P-Editor: Wang LL