Published online Sep 6, 2022. doi: 10.12998/wjcc.v10.i25.8872
Peer-review started: February 18, 2022
First decision: June 15, 2022
Revised: June 24, 2022
Accepted: July 20, 2022
Article in press: July 20, 2022
Published online: September 6, 2022
Processing time: 188 Days and 22.7 Hours
Misuse of disinfectants during the coronavirus disease 2019 pandemic has led to several poisoning incidents. However, there are few clinical case reports on poisoning caused by improper mixing of household disinfectants.
To summarize the clinical characteristics and treatment effects of chlorine poisoning caused by improper mixing of hypochlorite bleach with acidic cleaning agents.
METHODS
We retrospectively analyzed baseline and clinical data, clinical symptoms, and treatment methods of seven patients with chlorine poisoning who were admitted to the National Army Poisoning Treatment Center.
Among the seven patients, the average poisoning time (exposure to admission) was 57 h (4-240 h). All patients were involved in cleaning bathrooms. Chest computed tomography scans revealed bilateral lung effusions or inflammatory changes in five patients. The partial pressure of oxygen decreased in six patients, and respiratory failure occurred in one. Five patients had different degrees of increase in white blood cell count. Humidified oxygen therapy, non-invasive mechanical ventilation, anti-inflammatory corticosteroids, antioxidants, and antibiotics were administered for treatment. The average length of hospital stay was 7 d (4-9 d). All seven patients recovered and were discharged.
Improper mixing of household disinfectants may cause damage to the respiratory system due to chlorine poisoning. Corticosteroids may improve lung exudation in severe cases, and symptomatic supportive treatment should be performed early.
Core Tip: During the coronavirus disease 2019 pandemic, disinfectants should be used carefully. Improper mixing of household disinfectants may cause damage to the respiratory system due to chlorine poisoning. Corticosteroids may improve lung exudation in severe cases, and symptomatic supportive treatment should be performed early.
- Citation: Lin GD, Wu JY, Peng XB, Lu XX, Liu ZY, Pan ZG, Qiu ZW, Dong JG. Chlorine poisoning caused by improper mixing of household disinfectants during the COVID-19 pandemic: Case series. World J Clin Cases 2022; 10(25): 8872-8879
- URL: https://www.wjgnet.com/2307-8960/full/v10/i25/8872.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i25.8872
There are several types of household disinfection products, and the incidence of poisoning by misuse and accidental intake of such products remains high[1-4]. Among them, inhalation-induced poisoning accounts for a large proportion of cases and causes serious injuries[3,4]. In China, 84 types of sodium hypochlorite-based disinfectants and toilet cleaning solutions (containing diluted hydrochloric acid) are widely used in households; with several poisoning incidents involving these products[4]. With the heightened awareness of infection and viruses, the use of household disinfectants increased significantly during the coronavirus disease 2019 (COVID-19) pandemic[5-7]. Moreover, incorrect use of disinfectants is common[6]. Furthermore, inefficient household disinfection has been observed, despite the belief that disinfectants can eliminate COVID-19[2,7,8]. Household disinfectants may cause toxic reactions and produce toxic gases, including chlorine[2-4,9]. Chlorine exposure is usually caused by accidental release of chlorine vapor from swimming pools, improper mixing of hypochlorite bleach and acid cleaners, school laboratory experiments, and industrial or chemical transportation accidents[9-13]. Due to its high toxicity and common availability, chlorine gas has also been used in terrorist attacks and as an agent for chemical warfare[11,12]. Despite its widespread use, there are a few clinical case reports on acute chlorine inhalation poisoning caused by improper mixing of household disinfectants and toilet cleaning solutions[3]. Clinicians lack a deep understanding of the possible clinical manifestations and prognoses of such patients. In this study, we summarized the clinical data of seven patients admitted to our center during the COVID-19 pandemic with acute chlorine inhalation poisoning caused by improper mixing of disinfectants and toilet cleaning solutions. These findings can enable improvement in the treatment of future cases.
We collected and retrospectively analyzed the clinical data, diagnostic details, and treatment procedures of seven patients with acute chlorine inhalation poisoning caused by improper mixing of disinfectants and toilet cleaning solutions, who were admitted to the National Army Poisoning Treatment Center from March 2020 to September 2021. All patients had a history of inhaling chlorine gas, an irritant produced by improper mixing of toilet cleaning solutions with one of the 84 disinfectants widely used in Chinese households. The collected data included: sex, age, underlying disease, poisoning time, and cause of poisoning; clinical manifestations: main symptoms, related laboratory tests, and imaging data; and the following data on the diagnosis and treatment process: treatment methods, hospitalization days, prognosis, and follow-up prognosis. All patients provided informed consent, and the retrospective study design was approved by the appropriate ethics review board of our hospital.
Descriptive statistics were used to summarize the data; results are reported as the mean (minimum-maximum). No imputation was performed for missing data. Analysis was performed using Stata 15.1 software.
The patients included three men and four women, with an average age of 48.8 years (18-67 years). The patients were diagnosed with chlorine poisoning caused by inhalation after each patient confirmed the mixing of two types of household disinfection products to clean household items or toilets, and witnessed the subsequent production of a yellow-green gas. The average poisoning time (time from exposure to the chlorine till admission) was 57 h (4-240 h). All poisoning incidents occurred while disinfecting a room during the COVID-19 pandemic. The patient data are summarized in Table 1.
| Age, (yr) | Sex | Comorbidities | Initial symptoms | Admission time | PaO2/FiO2 | Computed Tomography | Major treatments | |
| 1 | 60 | F | Hypertension, hyperthyroidism | Breathlessness, difficulty breathing, headache, dizziness | 3 h | 318.10 | Bilateral lung effusions | Humidified oxygen; methylprednisolone(80 mg for 3d, 40 mg for 3d); inhalated budesonide and bromhexine; cefmetazole anti-infection |
| 2 | 61 | M | None | Breathlessness | 10 d | 372.38 | Bilateral interstitial exudations | Humidified oxygen; methylprednisolone(80 mg for 3 d, 40 mg for 3 d); inhaled budesonide and bromhexine; azithromycin anti-infection |
| 3 | 60 | F | None | Fatigue, breathlessness, coughing, choking of the pharynx, dizziness, headache, transient unconsciousness, urinary incontinence | 24 h | 215.52 | Bilateral lung effusions | Humidified oxygen; methylprednisolone (80 mg for 3 d, 40 mg for 3 d); inhaled budesonide and bromhexine; cefmetazole anti-infection |
| 4 | 18 | F | None | Dizziness, coughing, nausea, vomiting | 6 h | 396.19 | Striped shadow under the pleura of the right lung | (pre-hospital) Dexamethasone(10 mg); humidified oxygen; mthylprednisolone(40 mg for 3 d) |
| 5 | 56 | M | Smoking history of 30 years | Chest tightness, breathlessness | 12 h | 342.86 | Bilateral lung emphysema and bullae | Humidified oxygen; inhaled budesonide and bromhexine; methylprednisolone(80 mg for 3 d, 40 mg 3 d); moxifloxacin anti-infection |
| 6 | 20 | M | Smoking history for 2 years | Chest tightness, cough, choking in the pharynx, breathlessness, difficulty breathing | 17 h | 198.62 | Bilateral lung effusions | Non-invasive mechanical ventilation; methylprednisolone (80 mg for 5 d, 40 mg for 2 d); inhaled budesonide and bromhexine; Moxifloxacin anti-infection |
| 7 | 67 | F | Hypertension history for 24 years | Coughing, breathlessness | 4 d | 210.34 | Increased texture of blood vessels in bilateral Lung and multiple patchy changes under the pleura; bilateral pneumonia changes | Methylprednisolone(80 mg for 3 d, 40 mg for 3 d); inhaled budesonide and bromhexine; moxifloxacin anti-infection |
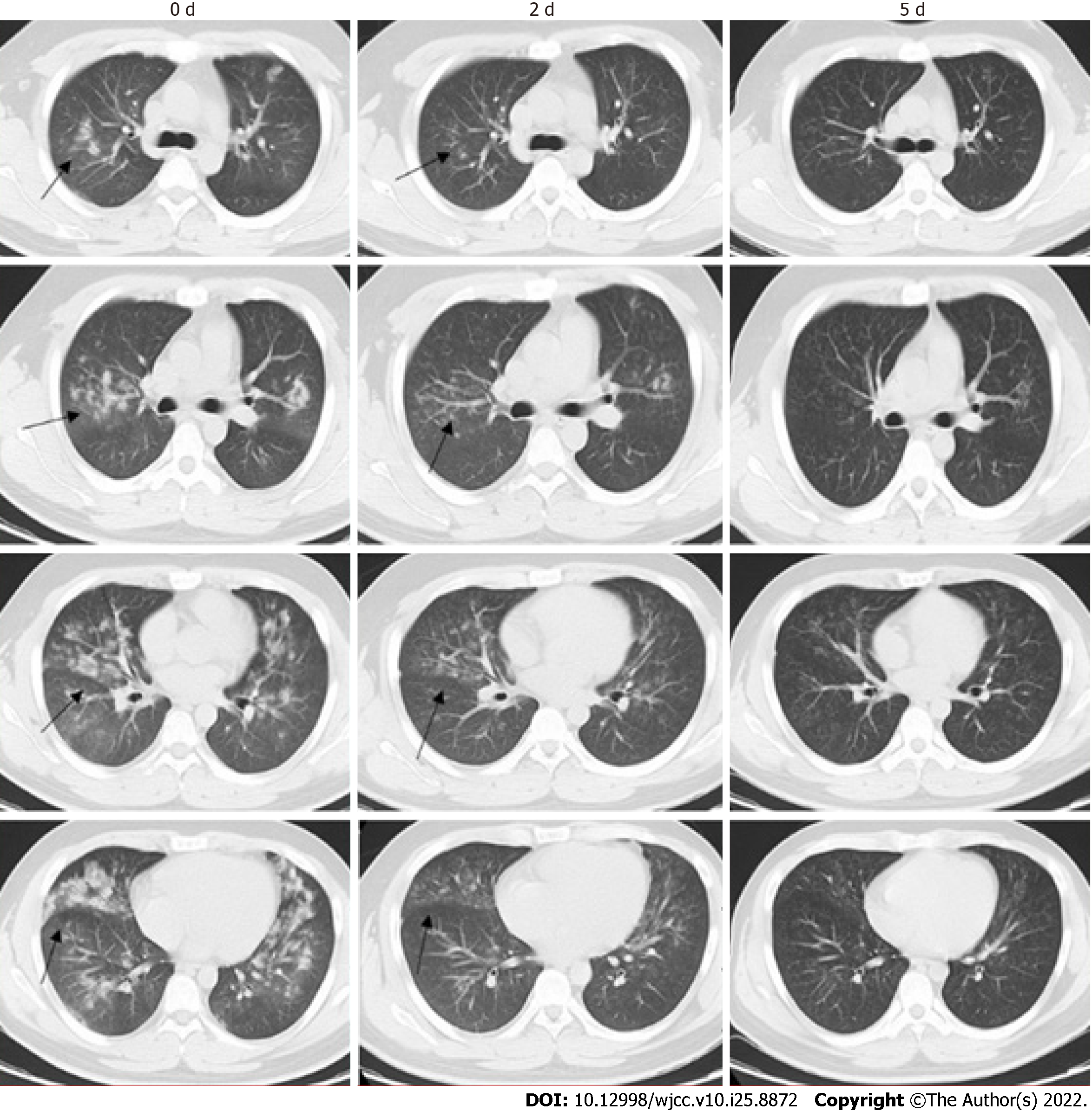
The clinical manifestations and severity of poisoning due to intoxication time, absorption, age, and individual physique differed among the patients included in this study. Among the seven patients, six had mild symptoms, while one had severe symptoms. Additionally, there were six cases with breathlessness, two with dyspnea, three with headache, three with dizziness, three developed a cough, two with pharyngeal discomfort, one with fatigue, one with nausea, and one case of vomiting. One patient developed transient unconsciousness (recovered consciousness in approximately 1 minute) and urinary incontinence. The symptoms are shown in Table 1. The laboratory test results on admission showed an average white blood cell count of 13.61 × 109/L (3.83-19.05 × 109/L). The average oxygen partial pressure was 68.17 mmHg (57.6-83.2 mmHg), and the average oxygenation index was 293.43 mmHg (198.62-396.19 mmHg). Among the patients, three had toxic lung injury (oxygenation index < 300 mmHg), one had an oxygenation index of < 200 mmHg, six had hypoxemia, one had type 1 respiratory failure, and five had bilateral lung effusions or inflammatory changes on chest computed tomography (CT). Chest CT scans of two of the patients showed no obvious exudation or inflammatory changes. The chest CT image of the heaviest patient (Patient 6 in Table 1) is shown in Figure 1. The chest CT images of the other patients are shown in Supplementary material 1.
Six patients received humidified oxygen therapy, and one was treated with non-invasive mechanical ventilation. Anti-inflammatory glucocorticoids (including intravenous methylprednisolone and inhaled hormone; dosage mentioned in Table 1) were administered to relieve bronchospasm and reduce phlegm. Antioxidants and antibiotics were administered to maintain the acid-base electrolyte balance and prevent bacterial infection, respectively. Improvement was observed in all patients post treatment, which was confirmed with consecutive chest CT (Figure 1 and Supplementary materials). The average length of hospital stay was 7 d (4-9 d). All patients recovered and were discharged, with no symptom recurrence observed after follow-up.
The cases reported in this study describe chlorine poisoning caused by improper mixing of toilet cleaning solutions and one of the 84 disinfectants commonly used in Chinese households during the COVID-19 pandemic. The effective ingredients of these products include diluted hydrochloric acid and sodium hypochlorite, which on mixing undergo a chemical reaction to produce chlorine gas. Among the seven patients with chlorine poisoning, one experienced severe symptoms. The chest CT scan revealed significant bilateral lung effusion, and the patient's blood gas analysis indicated type 1 respiratory failure. However, after active treatment, the condition of all patients improved significantly. This study highlights the importance of early detection, diagnosis, and treatment and presents our valuable experience in treating patients with chlorine poisoning.
Chlorine gas is a toxic irritant[9,14]. Due to the difference in concentration, duration of intoxication, and individual sensitivities of patients, acute chlorine gas inhalation can cause varying degrees of damage to the human body and can further become life-threatening[11,15-17]. On inspiration, the chlorine gas reacts with moisture on the mucosal surface of the respiratory tract to generate hypochlorous and hydrochloric acid [11,15]. Hypochlorous acid can be decomposed into hydrochloric acid and new ecological oxygen, causing local irritation and corrosion[4]. Chlorine can combine with reactive oxygen species and other airway fluid components to form a variety of highly active oxidants, which can cause direct oxidative damage to the surrounding airway epithelium[11,15]. Additionally, the migration and activation of inflammatory cells, such as neutrophils, to the affected site, and the subsequent release of oxidants and proteolytic enzymes may cause further damage to the epithelium[15]. Therefore, chlorine poisoning can cause bronchospasm and bronchitis, and in severe cases, pulmonary edema accompanied by damage to the cardiopulmonary and nervous systems[9,18,19]. Acute chlorine poisoning is characterized by acute respiratory system damage[17]. All seven patients in this study had respiratory symptoms, such as wheezing, dyspnea, and pharyngeal discomfort. Imaging results indicated varying degrees of lung damage. Most patients had different degrees of increase in white blood cell counts and high-sensitivity C-reactive protein levels, suggesting an acute inflammatory response. The direct interaction of chlorine and acute inflammatory response may lead to acute toxic lung injury and its associated complications[15]. One patient had transient unconsciousness, suggesting the toxic effects of chlorine on the nervous system[19], which is consistent with previous literature[19].
Current treatment measures in response to acute chlorine inhalation poisoning, which mainly causes toxic lung injury and systemic inflammation, include humidified oxygen therapy, use of corticosteroids (intravenous and inhaled), airway antispasmodic drugs, antioxidants, and inhaled sodium bicarbonate[9,17]. Recent studies suggest TRPV4 inhibitors, dimethylthiourea, and rolipram as therapeutic options, although these have not been clinically used[9,17]. Furthermore, the efficacy of glucocorticoids remains uncertain, and currently, extensive studies to verify the findings are scarce[9]. Here, intravenous methylprednisolone combined with inhaled hormone was employed as the treatment strategy. The effect of this treatment on heavier patients was significant. Corticosteroid therapy can significantly reduce inflammatory exudation caused by chlorine gas, and this study presents clinical experience on using corticosteroids for the treatment of chlorine poisoning[9]. Current treatment measures for hypoxemia and respiratory failure caused by chlorine poisoning include humidified oxygen therapy, non-invasive mechanical ventilation, invasive mechanical ventilation, and extracorporeal membrane oxygenation therapy[9,17,20]. In this study, six patients with hypoxemia received oxygen therapy, and one critically ill patient received non-invasive mechanical ventilation. There was significant improvement in the breathing conditions of all patients. None of the patients received invasive mechanical ventilation. Therefore, we conclude that the treatment should be based on the principles of inflammation control; antioxidant therapy; protection of lung function; prevention and treatment of pulmonary edema; protection of the heart, liver, brain, kidney, and other essential organ functions; and improvement of oxygen delivery.
The recommended emergency intervention steps during treatment include: (1) Immediate relocation to an open area with fresh air, ensuring an unobstructed respiratory tract, and providing timely and effective oxygen therapy; (2) Providing non-invasive mechanical ventilation or invasive mechanical ventilation when necessary to improve respiratory conditions and increase oxygen delivery; and (3) Early, adequate, short-term administration of corticosteroid therapy to improve pulmonary edema. This study administered 40-80 mg/d of methylprednisolone for 3-7 d. Other treatments included antispasmodic and anti-asthmatic symptomatic treatment, such as supporting essential organ functions, nutritional support, maintenance of water and electrolyte homeostasis, and acid-base balance. In principle, it is not recommended to use antibiotics to treat acute chlorine inhalation poisoning; however, it was administered to prevent opportunistic bacterial infections. Appropriate antibiotics should be administered to treat infections timeously[17]. However, further investigation is required into the advantages and disadvantages of using corticosteroids and antibiotics to prevent infection in acute chlorine inhalation poisoning[17]. Additionally, atomizing bicarbonate to treat the acidic environment of the airways and lungs caused by chlorine poisoning has been attempted; however, the dosage is difficult to determine, and the benefits from the perspective of lung physiology are unclear[17]. Furthermore, new treatment methods (including TRPV4 antagonists, dimethylthiourea, and rolipram) are still experimental.
This study presents the following limitation: our study was limited by its retrospective nature and small sample size. Therefore, more cases should be studied for improved generalizability and understanding of the clinical characteristics and treatment of chlorine poisoning caused by disinfectant mixing.
There are no specific antidotes and effective treatment measures for acute chlorine inhalation poisoning, and comprehensive supportive treatment is the primary treatment method. Additionally, corticosteroids may improve lung exudation. Therefore, it is crucial to understand and prevent acute chlorine inhalation poisoning. Effective and correct utilization of household disinfectants is key to prevent chlorine inhalation poisoning during the COVID-19 pandemic. Hydrochloric acid and sodium hypochlorite disinfectant products, such as commonly used disinfectants and toilet cleaning solutions, should not be mixed. In case of accidental chlorine inhalation poisoning, timely ventilation and hospital medical treatment are required.
The use of household disinfectants increased significantly during the coronavirus disease 2019 (COVID-19) pandemic. But there are a few clinical case reports on acute chlorine inhalation poisoning caused by improper mixing of household disinfectants and toilet cleaning solutions.
We summarized the clinical data of patients admitted to our center during the COVID-19 pandemic with acute chlorine inhalation poisoning caused by improper mixing of disinfectants and toilet cleaning solutions to help improve a clinician's ability to treat future cases.
To help improve a clinician's ability. Seven patients with acute chlorine inhalation poisoning caused by improper mixing of disinfectants and toilet cleaning solutions admitted to the National Army Poisoning Treatment Center from March 2020 to September 2021.
Retrospective descriptive analysis was performed on the clinical data of all patients.
Post poisoning, patients may present with symptoms of breathlessness, dyspnea, headache, nausea, cough, pharyngeal discomfort, fatigue, nausea, and depression. Out of seven patients, one had type 1 respiratory failure, and five had bilateral lung effusions or inflammatory changes on chest computed tomography. Six patients received humidified oxygen therapy, and one was treated with non-invasive mechanical ventilation. All patients were treated with glucocorticoids.
Improper mixing of house disinfectants causes damage to the respiratory system due to chlorine poisoning. Corticosteroids may improve lung exudation, and early symptomatic supportive treatment should be performed.
More case studies are required for improved generalizability and understanding of the clinical characteristics and treatment of chlorine poisoning caused by disinfectant mixing.
| 1. | Ha Y, Kim Y, Song E, Yoo HJ, Kwon JH. Development of a personal passive air sampler for estimating exposure to effective chlorine while using chlorine-based disinfectants. Indoor Air. 2021;31:557-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Quirce S, Barranco P. Cleaning agents and asthma. J Investig Allergol Clin Immunol. 2010;20:542-550. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | McKenzie LB, Ahir N, Stolz U, Nelson NG. Household cleaning product-related injuries treated in US emergency departments in 1990-2006. Pediatrics. 2010;126:509-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Sabato V, Ebo DG. Comment on: Koppelman SJ, Jayasena S, Luykx D, Schepens E, Apostolovic D, de Jong GA, et al. Allergenicity attributes of different peanut market types. Food and chemical toxicology: An international journal published for the British Industrial Biological Research Association 2016. Food Chem Toxicol. 2016;92:256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Yasseen Iii A, Weiss D, Remer S, Dobbin N, MacNeill M, Bogeljic B, et al Increases in exposure calls related to selected cleaners and disinfectants at the onset of the COVID-19 pandemic: data from Canadian poison centres. Health promotion and chronic disease prevention in Canada: research, policy and practice, 2021; 41: 25-29. [RCA] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 6. | Gharpure R, Miller GF, Hunter CM, Schnall AH, Kunz J, Garcia-Williams AG. Safe Use and Storage of Cleaners, Disinfectants, and Hand Sanitizers: Knowledge, Attitudes, and Practices among U.S. Adults during the COVID-19 Pandemic, May 2020. The American Journal of Tropical Medicine and Hygiene, 2020. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Gharpure R, Hunter CM, Schnall AH, Barrett CE, Kirby AE, Kunz J, Berling K, Mercante JW, Murphy JL, Garcia-Williams AG. Knowledge and Practices Regarding Safe Household Cleaning and Disinfection for COVID-19 Prevention - United States, May 2020. MMWR Morb Mortal Wkly Rep. 2020;69:705-709. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 98] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 8. | Chang A, Schnall AH, Law R, Bronstein AC, Marraffa JM, Spiller HA, Hays HL, Funk AR, Mercurio-Zappala M, Calello DP, Aleguas A, Borys DJ, Boehmer T, Svendsen E. Cleaning and Disinfectant Chemical Exposures and Temporal Associations with COVID-19 - National Poison Data System, United States, January 1, 2020-March 31, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:496-498. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 130] [Cited by in RCA: 173] [Article Influence: 28.8] [Reference Citation Analysis (0)] |
| 9. | Huynh Tuong A, Despréaux T, Loeb T, Salomon J, Mégarbane B, Descatha A. Emergency management of chlorine gas exposure - a systematic review. Clin Toxicol (Phila). 2019;57:77-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Na W, Wang Y, Li A, Zhu X, Xue C, Ye Q. Acute chlorine poisoning caused by an accident at a swimming pool. Toxicol Ind Health. 2021;37:513-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Zellner T, Eyer F. Choking agents and chlorine gas - History, pathophysiology, clinical effects and treatment. Toxicol Lett. 2020;320:73-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 12. | Wilken JA, DiMaggio M, Kaufmann M, O'Connor K, Smorodinsky S, Armatas C, Barreau T, Kreutzer R, Ancheta L. Inhalational Chlorine Injuries at Public Aquatic Venues - California, 2008-2015. MMWR Morb Mortal Wkly Rep. 2017;66:498-501. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Cevik Y, Onay M, Akmaz I, Sezigen S. Mass casualties from acute inhalation of chlorine gas. South Med J. 2009;102:1209-1213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Akdur O, Durukan P, Ikizceli I, Ozkan S, Avsarogullari L. A rare complication of chlorine gas inhalation: pneumomediastinum. Emerg Med J. 2006;23:e59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Pesonen M, Vähäkangas K. Chloropicrin-induced toxicity in the respiratory system. Toxicol Lett. 2020;323:10-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Carpenter A, Cox AT, Marion D, Phillips A, Ewington I. A case of a chlorine inhalation injury in an Ebola treatment unit. J R Army Med Corps. 2016;162:229-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Howard C, Ducre B, Burda AM, Kubic A. Management of chlorine gas exposure. J Emerg Nurs. 2007;33:402-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Carlisle M, Lam A, Svendsen ER, Aggarwal S, Matalon S. Chlorine-induced cardiopulmonary injury. Ann N Y Acad Sci. 2016;1374:159-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 19. | Kilburn KH. Brain but not lung functions impaired after a chlorine incident. Industrial health. 2003;41:299. |
| 20. | Matos AM, Oliveira RR, Lippi MM, Takatani RR, Oliveira W Filho. Use of noninvasive ventilation in severe acute respiratory distress syndrome due to accidental chlorine inhalation: a case report. Rev Bras Ter Intensiva. 2017;29:105-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade d (Fair): D
Grade E (Poor): 0
P-Reviewer: Brat K, Czech Republic; Gheshlaghi F, Iran S-Editor: Wang LL L-Editor: A P-Editor: Wang LL