Published online Aug 16, 2022. doi: 10.12998/wjcc.v10.i23.8107
Peer-review started: November 29, 2021
First decision: May 11, 2022
Revised: May 20, 2022
Accepted: July 11, 2022
Article in press: July 11, 2022
Published online: August 16, 2022
Processing time: 245 Days and 5.6 Hours
Total knee arthroplasty (TKA) has been shown to improve quality of life and reduce pain. High-flexion activities such as squatting, kneeling, and floor transfers are mainly listed as demanding tasks. Among them, squatting is an important position.
To provide a new squat position classification and evaluate the different squatting positions of a series of patients after primary TKA.
From May 2018 to October 2019, we retrospectively reviewed 154 video recordings of the squatting-related motions of patients after TKA. Among the included patients, 119 were women and 35 were men. Their mean age at the index surgery was 61.4 years (range, 30 to 77).
The median follow-up was 12 mo (range, 6 to 156 mo). We classified those squatting-related motions into three major variations according to squatting depth: Half squat, parallel squat, and deep squat. The angles of hip flexion, knee flexion, and ankle dorsiflexion were measured in the screenshots captured from the videos at the moment of squatting nadir. A total of 26 patients were classified as half squats, 75 as parallel squats, and 53 as deep squats. The angles of hip flexion, knee flexion, and ankle dorsiflexion all differed significantly among the three squatting positions (P < 0.001). In the parallel squat group, the mean knee flexion angle (°) was 116.5 (SD, 8.1; range, 97 to 137). In the deep squat group, the mean knee flexion angle (°) was 132.5 (SD, 9.3; range, 116 to 158).
Among the three squatting positions, deep squat showed the highest hip, knee, and ankle flexion angles, followed by the parallel squat. With the improvement of squatting ability, the patient's postoperative satisfaction rate was also significantly enhanced. However, the different squatting abilities of the patients cannot be effectively distinguished from the scoring results (P > 0.05). Our squatting position classification offers a pragmatic approach to evaluating patients’ squatting ability after TKA.
Core Tip: Few studies have focused on squatting ability after total knee arthroplasty (TKA). Most squatting-related items in patient-reported outcome measures present as binary options of “can” or “cannot” or a subjective sense of difficulty along with this motion. The main finding of this study is the squatting position classification based on squatting depth. And our squatting position classification offers a pragmatic approach to evaluating patients’ squatting ability after TKA.
- Citation: Li TJ, Sun JY, Du YQ, Shen JM, Zhang BH, Zhou YG. Different squatting positions after total knee arthroplasty: A retrospective study. World J Clin Cases 2022; 10(23): 8107-8114
- URL: https://www.wjgnet.com/2307-8960/full/v10/i23/8107.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i23.8107
Total knee arthroplasty (TKA) has been shown to improve quality of life and reduce pain. However, functional deficits can still be observed to persist after surgery[1]. The unfulfillment of preoperative expectations has been reported as one of the main determinants of postoperative dissatisfaction[2,3]. High-flexion activities such as squatting, kneeling, and floor transfers are mainly listed as demanding tasks. Among them, squatting is an important position especially for Asian, African, and Middle East populations, which can be used for a number of activities, including toileting, household chores, socializing, working, and religious acts[4].
During postoperative follow-up, clinicians often rely on patient-reported outcome measures (PROMs) to quantify the trajectory of functional recovery of TKA patients[5]. Few studies have focused on squatting ability after TKA. Although squatting-related items have been involved in some PROMs, they merely appear as binary options of “can” or “cannot”, or descriptions of the ease or complexity of accomplishing the task[6-8]. No further divisions or descriptions of squatting depth have been highlighted in those studies and scales. Even the specially developed questionnaire, “High-flexion Knee Scoring System”, or the isolated subdomain “floor life” in the “Korean Knee Score”, is inadequate to evaluate squatting ability and completeness in detail[9,10].
Current research on squatting depth is mainly performed among powerlifters. Depending on the squatting depth, the Olympic barbell squat can be classified into four fundamental variations: Quarter squat, half squat, parallel squat, and deep squat. The knee flexion angle increases according to the sequence mentioned above[11,12].
The aim of this study was to provide a new squat position classification and to evaluate patients’ squatting ability after TKA.
The inclusion criteria were as follows: (1) Patients who underwent primary TKA; and (2) Patients who were followed for at least 6 mo postoperatively. The exclusion criteria included: (1) Patients with multiple comorbidities that would limit their activity level; (2) Patients whose videos did not record squatting-related motions; (3) Patients who performed squatting with the aid of holding; and (4) Patients who could not lift their heels from the ground without help.
This study is a descriptive and retrospective analysis of clinical data. Our Institution Review Board approved the study. From May 2018 to October 2019, we acquired 236 video recordings of the functional recovery of patients after TKA, which were carried out by a professional team in actual clinical settings, including outpatient clinics and hospital wards. A total of 154 patients (228 knees) were included, of whom 119 were women and 35 were men. Their mean age at the index surgery was 61.4 years (range, 30 to 77 years). The median follow-up was 12 mo (range, 6 to 156). Demographic and clinical data, including diagnosis, age, sex, weight, height, and operative recordings, were collected from the electronic medical records, and body mass index was calculated. Within this cohort, the diagnosis was osteoarthritis in 147 patients and rheumatoid arthritis in 7. Among them, six patients had a stiff knee, and three had an ankylosed knee. The indications for TKA were severe pain associated with stiffness and limitations of daily activities. Primary TKAs were completed by two senior surgeons. A midline straight longitudinal skin incision and a standard medial parapatellar approach were employed in all knee surgeries. Follow-up evaluation was performed at regular intervals (6 wk, 3 mo, 1 year, and yearly thereafter). The details of the patients are summarized in Table 1. Patients were asked to respond to a questionnaire measuring satisfaction with the outcomes of TKA based on a 5-point Likert rating (varying from "very satisfied" through "very dissatisfied"). All patients used high flexion prosthesis (PFC Sigma PS150; DePuy, Warsaw, IN, United States).
| Variation | Half squat | Parallel squat | Deep squat | P value |
| Patients n | 26 | 75 | 53 | |
| Gender, n (%) | ||||
| Male | 3 (11.5) | 20 (26.7) | 12 (22.6) | |
| Female | 23 (88.5) | 55 (73.3) | 41 (77.4) | |
| Age (yr) | 62.5 ± 11.4 | 61.6 ± 8.5 | 60.6 ± 6.9 | |
| Height (cm) | 160.7 ± 6.8 | 160.7 ± 7.2 | 161.9 ± 7.5 | |
| Weight (kg) | 67.3 ± 9.4 | 68.7 ± 10.4 | 67.9 ± 11.3 | |
| BMI (kg/m2) | 25.9 ± 2.6 | 26.6 ± 3.6 | 25.8 ± 3.4 | |
| Side, n (%) | ||||
| Unilateral | 14 (53.8) | 40 (53.3) | 26 (49.1) | |
| Bilateral | 12 (46.2) | 35 (46.7) | 27 (50.9) | |
| High-flexion TKA, n (%) | 23 (88.5) | 63 (84) | 51 (96.2) | |
| Patellar resurfacing, n (%) | 22 (84.6) | 56 (74.7) | 40 (75.5) | |
| Follow-up (months), median (Q1-Q3) | 6 (6-60) | 8 (6-120) | 12 (6-156) | |
| Pre-op knee flexion | 76.8 ± 8.3 | 86.8 ± 9.3 | 105.4 ± 8.4 | |
| Mean stool frequency (every 3 d) | 1.8 (0-5) | 2.6 (1-5) | 3.5 (1-6) | |
| Satisfaction rate (%) | 65.4 | 80 | 96.2 | |
| KSS (Post-TKA) | 76 ± 4.9 | 76.3 ± 6.8 | 79.2 ± 8.2 | > 0.05 |
| HSS (Post-TKA) | 79 ± 5.8 | 78.6 ± 6.3 | 80.6 ± 6.6 | > 0.05 |
Squatting is defined as a position where the legs are extremely flexed, bringing the body down over the feet. This position demands maximal flexion at the hip, knee, and ankle joints. In each video, the patient was asked to stand sideways and try to squat with legs moving symmetrically according to his capability. From a standing position, the patient was verbally cued to squat down to the nadir. The patient held the position for 2 s and then returned to the relaxed standing position. This procedure was repeated three times. During the squat executions, the patient was “guarded” by one of his/her relatives.
A series of screenshots at the moment of the squatting nadir were captured from the videos. Independent review of the screenshots was performed by two observers to measure the angles of hip flexion, knee flexion, and ankle dorsiflexion. Actually, the angle of hip flexion represents the forward bending motion contributed by both the hip and spine. Hip flexion was calculated as 180°-(angle between trunk and thigh). Knee flexion was calculated as 180°-(angle between the thigh and calf). Ankle dorsiflexion was calculated as 90°-(angle between the calf and dorsum pedis). All measurements were conducted by using Digimizer v5.4 (Acacialaan, Belgium).
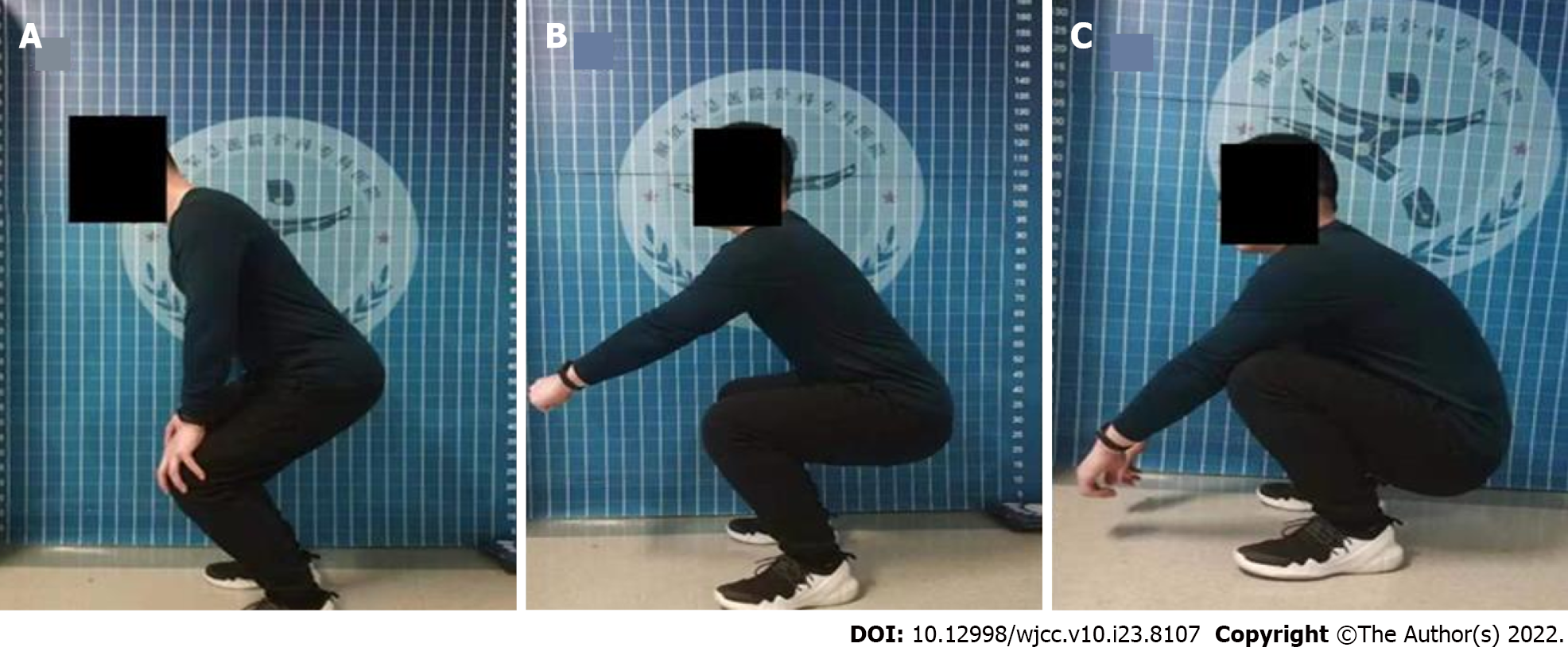
We classified those squatting-related motions into three major variations on the basis of squatting depth: Half squat, parallel squat, and deep squat. In the half squat, the patient descended until reaching 90° of knee flexion. In the parallel squat, the eccentric phase ends when the inguinal fold is in a straight horizontal line with the top of the knee, while in the deep squat the eccentric phase is carried out until the top of the thighs falls below the horizontal plane (Figure 1).
All identifying marks were removed from the videos, which were then sorted and labelled. Two other observers who were not involved in the range of motion (ROM) measurement participated in the classification process. Before embarking on the review, each observer was provided with the same descriptions and diagrams of the different squatting positions. Video reviews were performed independently in random order by each observer on two separate occasions, at least one month apart. Observers repeated their readings without knowledge of the previous results. The order of the videos was randomized using a sequential random number generator to prevent possible recall. Interobserver variability was measured by comparing the sorting of two observers on each occasion, while intraobserver reliability was determined by comparing the two reviews of each observer.
Assessment of inter- and intra-observer consistency was accomplished by the use of the kappa coefficient (κ). According to Landis and Koch[13], agreement was graded as slight (κ = 0 to 0.2), fair (κ = 0.21 to 0.40), moderate (κ = 0.41 to 0.60), substantial (κ = 0.61 to 0.80), or almost perfect (κ = 0.81 to 1.0). For ROM measurement, we used one-way analysis of variance among the three squatting positions. All tests were two-sided and statistical significance was set at P < 0.05. All analyses were carried out using the statistical package SPSS version 26.0 (IBM Inc., Armonk, New York).
A total of 26 patients were classified as half squats, 75 as parallel squats, and 53 as deep squats (Table 1). The results of the ROM measurements are summarized in Table 2. The angles of hip flexion, knee flexion, and ankle dorsiflexion all differed significantly among the three squatting positions (P < 0.001). In the parallel squat group, the mean knee flexion angle (°) was 116.5 (SD, 8.1; range, 97 to 137). In the deep squat group, the mean knee flexion angle (°) was 132.5 (SD, 9.3; range, 116 to 158). Among the three squatting positions, the deep squat showed the highest hip, knee, and ankle flexion angles, followed by the parallel squat. The American Knee Society score and Hospital for Special Surgery score did not significantly differ among the three groups (P > 0.05), but the postoperative patient satisfaction rate improved significantly among the three groups.
Interobserver reliability analysis revealed a kappa coefficient of 0.82 (almost perfect) for the squatting position classification. Intraobserver reliability analysis revealed kappa coefficients of 0.83 (almost perfect) for observer A, and 0.86 (almost perfect) for observer B.
The main finding of this study is the squatting position classification based on squatting depth. The results confirmed that this classification showed excellent reliability, as judged by the inter- and intra-observer variability. From half squat to deep squat, the flexion angles of the hip, knee, and ankle joints all increased with statistical significance, which indicated that deeper squat required more contribution from all those joints. It is the authors’ belief that the use of this classification, based on the squatting depth, will act as a guide for the assessment of patients’ squatting ability after TKA. The squatting position classification offers a pragmatic approach to evaluating patients’ squatting ability after TKA, and this has rarely been studied before. Few of the items in the existing scoring tables have addressed squatting ability, which also indirectly illustrates the current lack of research on squatting. However, squatting is an important position especially for Asian, African, and Middle East populations. This also explains why there was no significant difference in the scoring results among the three groups and the satisfaction rate improved significantly, because there was a significant roof effect due to the lack of assessment of the patient's postoperative squatting ability in the existing scoring table, and the different squatting abilities of the patients cannot be effectively distinguished from the scoring results. Patients after TKA can achieve higher squatting ability through persistent squat exercises. However, according to our clinical experience, if squatting ability does not improve after more than 6 mo of squatting exercises, there is little possibility of further improvement in squatting ability. Interestingly, as the squatting ability increased, the mean stool frequency (every 3 d) also increased. Because the process of defecation requires a certain squatting ability and needs to be maintained in a squatting position for a long time. In addition, squat toilets are still used in many homes and public areas in Asia, requiring a high squatting capacity to complete defecation, which limits patients with poor squatting ability from defecating frequently. This also shows that it is of great clinical significance to assess the squatting ability of patients after surgery.
Notably, few studies have focused on squatting ability after TKA. Most squatting-related items in PROMs present as binary options of “can” or “cannot” or a subjective sense of difficulty along with this motion[6-8]. No further divisions or descriptions of squatting depth have been highlighted in those studies and scales. Our classification of squatting position was raised by reference to the exercise program in athletic training, which was categorized based on the squatting depth[11,12]. Actually, the squatting depth that patients can achieve after TKA is associated with their ability to participate in functional activities especially floor-based lifestyles. For the Asian population, whether to complete the Asian squat movement also determines whether the patient is satisfied after surgery. Since squat stools are prevalent in Asia, patients can use squat stools only if they can at least parallel squat. This also explains that in the results section the patient's satisfaction rate improved significantly with the improvement of squatting ability. Our classification built a hierarchy for assessing patients’ squatting ability. However, the mode in which a patient performs squatting is not exactly the same as that of an athlete. With normal and intact knee joints, an athlete can perform any of the squatting positions effortlessly. In contrast, not all patients can perform deep squats, and some of them reach their limits before deep squats[14]. Therefore, apart from the three finite positions, the angle of knee flexion at the squatting nadir should also be considered.
As one of the high-flexion knee functions, squatting is based on an excellent ROM[4,15]. However, sometimes patients who bend their knees well may not achieve deep squats. Squatting is defined as a position where the legs are extremely flexed during load-bearing conditions. There is a significant need or increased activity of muscles especially the quadriceps, to enhance knee stability[16,17]. Therefore, squatting is a serious challenge for patients with weaker extension strength[18]. Currently, the ROM of the operated knee is used as a key indicator assessing the outcome after TKA in many studies[19-21]. As mentioned above, the ROM is still inadequate in reflecting patients’ high-level functions. This highlights the importance of our classification for the squatting position.
Squatting, one of the high-flexion motions, has blended into the daily lifestyles of people from different corners of the globe. Weiss et al[22] conducted a questionnaire survey including 176 patients to quantify the patient’s function and mobility after knee arthroplasty, and found squatting to be the most difficult activity for them[22]. Ghomrawi et al[23] compared patients’ and surgeons’ recovery expectations prior to primary TKA and found that more than 50% of the patients had higher expectations than their surgeon, which was driven by expectations of high-level activities such as squatting[23]. To fill the gap between surgeons and patients in evaluating the outcome of TKA, numerous PROMs have emerged over the years. Most of them incorporated a section devoted to high-flexion or high-level activities[6,9,10]. Even so, with no further division of squatting positions, respondents might make the wrong tick, which usually causes a ceiling effect along with the questionnaire. Perhaps this could also explain why some comparative studies regarding the outcome after TKA end up with no unexpectedly difference[19,24]. In addition, the squatting variations that we put forward could be helpful for surgeons in evaluating and quantifying their patients’ outcomes after TKA. Specifically, more detailed terminology about squatting positions could be conducive to the homogeneity of results awaiting systematic reviews in this regard.
Before initiation of the study, we set a limit on the observation time and only included patients who underwent primary TKA. However, it is believed that our classification applies equally to the evaluation of the squatting ability of patients who underwent unicompartmental knee arthroplasty or total knee revision. The same goes for patients before surgery or followed for less than 6 mo. Although modern knee prostheses have closely approximated the feel and function of a healthy knee, deep squats cannot be guaranteed for each patient after TKA[15,25]. As our results showed, the knee flexion angle in the deep squat group ranged from 116° to 158°, which is similar to the result summarized by Mulholland and Wyss[4]. Many patients reach their limits at certain points when trying to squat for several reasons[17,26,27]. However, patients are likely to compensate for any functional insufficiency of their knees by adjusting the kinematics and kinetics of other joints. Except for compensation of the hip-spine complex, some patients can achieve deep squatting by lifting their heels up[28], which is more common among patients with limited ROM of the hip joint.
There were three limitations in this study. First, the patients that we included could not constitute a consecutive series due to follow-up bias, so the incidence of different squatting positions could not be determined. Second, our classification mainly focused on the squatting depth, without considering the elapsed time from squatting down to rising up, which was also associated with patient’s activity level. Eventually, we had not yet worked out the connection between the squatting positions and the daily activities that patients can perform, which could be evaluated in future.
In summary, our squatting position classification offers a pragmatic approach to evaluating patients’ squatting ability after TKA, which is one of the most important motions in daily life. However, the relation between squatting position and daily activity requires further investigation.
Total knee arthroplasty (TKA) has been shown to improve quality of life and reduce pain. However, functional deficits can still be observed to persist after surgery.
The unfulfillment of preoperative expectations has been reported as one of the main determinants of postoperative dissatisfaction.
We aimed to provide a new squat position classification and evaluate the different squatting positions of a series of patients who underwent primary TKA.
From May 2018 to October 2019, we retrospectively reviewed 154 video recordings of the squatting-related motions of patients after TKA. Among the included patients, 119 were women and 35 were men. Their mean age at the index surgery was 61.4 years (range, 30 to 77 years).
A total of 26 patients were classified as half squats, 75 as parallel squats, and 53 as deep squats. The angles of hip flexion, knee flexion, and ankle dorsiflexion all differed significantly among the three squatting positions (P < 0.001). In the parallel squat group, the mean knee flexion angle (°) was 116.5 (SD, 8.1; range, 97 to 137). In the deep squat group, the mean knee flexion angle (°) was 132.5 (SD, 9.3; range, 116 to 158).
Among the three squatting positions, deep squat showed the highest hip, knee, and ankle flexion angles, followed by the parallel squat. With the improvement of squatting ability, the patient's postoperative satisfaction rate was also significantly enhanced.
Our squatting position classification offers a pragmatic approach to evaluating patients’ squatting ability after TKA.
| 1. | Disantis AY, Piva SR, Irrgang JJ. Standardized Patient Reported Outcomes Do Not Capture Functional Deficits of Patients Following Contemporary Total Knee Replacement: Descriptive Study. J Exerc Sports Orthop. 2018;5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 2. | Hamilton DF, Lane JV, Gaston P, Patton JT, Macdonald D, Simpson AH, Howie CR. What determines patient satisfaction with surgery? BMJ Open. 2013;3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 291] [Cited by in RCA: 353] [Article Influence: 27.2] [Reference Citation Analysis (0)] |
| 3. | Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006;452:35-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 738] [Cited by in RCA: 850] [Article Influence: 42.5] [Reference Citation Analysis (0)] |
| 4. | Mulholland SJ, Wyss UP. Activities of daily living in non-Western cultures: range of motion requirements for hip and knee joint implants. Int J Rehabil Res. 2001;24:191-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 208] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 5. | Ramkumar PN, Harris JD, Noble PC. Patient-reported outcome measures after total knee arthroplasty: a systematic review. Bone Joint Res. 2015;4:120-127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 125] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 6. | Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, Scott WN. The new Knee Society Knee Scoring System. Clin Orthop Relat Res. 2012;470:3-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 369] [Cited by in RCA: 534] [Article Influence: 38.1] [Reference Citation Analysis (0)] |
| 7. | Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2362] [Cited by in RCA: 2966] [Article Influence: 105.9] [Reference Citation Analysis (0)] |
| 8. | Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, Richmond JC, Shelborne KD. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29:600-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1375] [Cited by in RCA: 1667] [Article Influence: 66.7] [Reference Citation Analysis (0)] |
| 9. | Na SE, Ha CW, Lee CH. A new high-flexion knee scoring system to eliminate the ceiling effect. Clin Orthop Relat Res. 2012;470:584-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 68] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 10. | Kim JG, Ha JK, Han SB, Kim TK, Lee MC. Development and validation of a new evaluation system for patients with a floor-based lifestyle: the Korean knee score. Clin Orthop Relat Res. 2013;471:1539-1547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Hartmann H, Wirth K, Klusemann M. Analysis of the load on the knee joint and vertebral column with changes in squatting depth and weight load. Sports Med. 2013;43:993-1008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 101] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 12. | Pallarés JG, Cava AM, Courel-Ibáñez J, González-Badillo JJ, Morán-Navarro R. Full squat produces greater neuromuscular and functional adaptations and lower pain than partial squats after prolonged resistance training. Eur J Sport Sci. 2020;20:115-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 13. | Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159-174. [PubMed] |
| 14. | Noble PC, Gordon MJ, Weiss JM, Reddix RN, Conditt MA, Mathis KB. Does total knee replacement restore normal knee function? Clin Orthop Relat Res. 2005;157-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 306] [Cited by in RCA: 316] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 15. | Sultan PG, Most E, Schule S, Li G, Rubash HE. Optimizing flexion after total knee arthroplasty: advances in prosthetic design. Clin Orthop Relat Res. 2003;167-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 65] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Escamilla RF. Knee biomechanics of the dynamic squat exercise. Med Sci Sports Exerc. 2001;33:127-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 256] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 17. | D'Lima DD, Poole C, Chadha H, Hermida JC, Mahar A, Colwell CW Jr. Quadriceps moment arm and quadriceps forces after total knee arthroplasty. Clin Orthop Relat Res. 2001;213-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 91] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 18. | Ostermeier S, Stukenborg-Colsman C. Quadriceps force after TKA with femoral single radius. Acta Orthop. 2011;82:339-343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Mehin R, Burnett RS, Brasher PM. Does the new generation of high-flex knee prostheses improve the post-operative range of movement? J Bone Joint Surg Br. 2010;92:1429-1434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | Kim YH, Park JW, Kim JS. Do High-Flexion Total Knee Designs Increase the Risk of Femoral Component Loosening? J Arthroplasty. 2017;32:1862-1868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Crawford DA, Adams JB, Hurst JM, Berend KR, Lombardi AV Jr. Ten-Year Minimum Outcomes and Survivorship With a High Flexion Knee System. J Arthroplasty. 2019;34:1975-1979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Weiss JM, Noble PC, Conditt MA, Kohl HW, Roberts S, Cook KF, Gordon MJ, Mathis KB. What functional activities are important to patients with knee replacements? Clin Orthop Relat Res. 2002;172-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 268] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 23. | Ghomrawi HM, Franco Ferrando N, Mandl LA, Do H, Noor N, Gonzalez Della Valle A. How Often are Patient and Surgeon Recovery Expectations for Total Joint Arthroplasty Aligned? HSS J. 2011;7:229-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 24. | Luo SX, Su W, Zhao JM, Sha K, Wei QJ, Li XF. High-flexion vs conventional prostheses total knee arthroplasty: a meta-analysis. J Arthroplasty. 2011;26:847-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 25. | Morra EA, Rosca M, Greenwald JF, Greenwald AS. The influence of contemporary knee design on high flexion: a kinematic comparison with the normal knee. J Bone Joint Surg Am. 2008;90 Suppl 4:195-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Harbourne AD, Sanchez-Santos MT, Arden NK, Filbay SR. Predictors of return to desired activity 12 months following unicompartmental and total knee arthroplasty. Acta Orthop. 2019;90:74-80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 27. | Gromov K, Korchi M, Thomsen MG, Husted H, Troelsen A. What is the optimal alignment of the tibial and femoral components in knee arthroplasty? Acta Orthop. 2014;85:480-487. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 146] [Cited by in RCA: 189] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 28. | Smith SM, Cockburn RA, Hemmerich A, Li RM, Wyss UP. Tibiofemoral joint contact forces and knee kinematics during squatting. Gait Posture. 2008;27:376-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Holzer LA, Austria; Oommen AT, India S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Fan JR