Published online Aug 16, 2022. doi: 10.12998/wjcc.v10.i23.8088
Peer-review started: April 6, 2022
First decision: June 16, 2022
Revised: June 26, 2022
Accepted: July 11, 2022
Article in press: July 11, 2022
Published online: August 16, 2022
Processing time: 116 Days and 17.6 Hours
When the coronavirus disease 2019 (COVID-19) pandemic spread globally from the Hubei region of China in December 2019, the impact on elderly people was particularly unfavorable. The mortality associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection was highest in older individuals, in whom frailty and comorbidities increased susceptibility to severe forms of COVID-19. Unfortunately, in older patients, the course of COVID-19 was often characterized by significant cardiovascular complications, such as heart failure decompensation, arrhythmias, pericarditis, and myopericarditis. Ensuring that the elderly have adequate therapeutic coverage against known cardiovascular diseases and risk factors is particularly important in the COVID-19 era. Beta blockers are widely used for the treatment and prevention of cardiovascular disease. The clinical benefits of beta blockers have been confirmed in elderly patients, and in addition to their negative chronotropic effect, sympathetic inhibition and anti-inflammatory activity are theoretically of great benefit for the treatment of COVID-19 infection. Beta blockers have not been clearly shown to prevent SARS-CoV-2 infection, but there is evidence from published studies including elderly patients that beta blockers are associated with a more favorable clinical course of COVID-19 and reduced mortality. In this minireview, we summarize the most important evidence available in the literature on the usefulness of beta blocker therapy for older patients in the context of the COVID-19 pandemic.
Core Tip: This minireview offers an original and innovative summary of recent studies of the usefulness of beta blocker therapy for the elderly in the coronavirus disease 2019 (COVID-19) pandemic. We discuss the pharmacologic benefits of beta blocker therapy for older subjects and report the results of early studies highlighting the favorable effects of beta blockers on elderly patients affected by COVID-19.
- Citation: Santillo E, Migale M. Beta receptor blocker therapy for the elderly in the COVID-19 era. World J Clin Cases 2022; 10(23): 8088-8096
- URL: https://www.wjgnet.com/2307-8960/full/v10/i23/8088.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i23.8088
The current coronavirus disease 2019 (COVID-19) pandemic is one of the most pressing public health problems worldwide because of excessive mortality and the economic impact on health systems[1,2]. Indeed, despite the development of several specific vaccines for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the application of stringent preventive measures to limit the transmission of the infection, COVID-19 has continued to spread in recurrent waves, with the ability of the virus to mutate rapidly[3].
The elderly, especially those who are frail and with comorbidities, are particularly vulnerable to COVID-19[4,5]. It is widely recognized that SARS-CoV-2 infection causes higher hospitalization and mortality rates in older than in younger individuals[6,7]. Initially, COVID-19 was viewed as a predominantly respiratory disease, but recent studies have shown that SARS-CoV-2 infection can also be considered a vascular disease, given that endothelial and thrombotic processes are fundamental etiopathogenic actors in the development of the disease[8]. Furthermore, COVID-19 is characterized by frequent cardiovascular complications, such as heart failure decompensation and arrhythmias[9]; indeed, cardiovascular drugs, such as heparin and antihypertensive drugs, have been investigated for their possible use in the prevention and treatment of SARS-CoV-2 infection and its complications[10,11].
Beta blockers have been used for decades for arterial hypertension, heart failure, ischemic heart disease, and arrhythmias in geriatric patients[12-14]. They may also be protective in patients with COVID-19. In this minireview, we discuss the most significant pathophysiological and clinical evidence suggestive of the usefulness of beta blockers in elderly patients during the COVID-19 pandemic, beginning with their pharmacologic properties.
Beta blockers are widely used in cardiology and have other indications, such as headaches (migraine), glaucoma, or essential tremor[15]. As the prevalence of hypertension, heart failure, and arrhythmias is particularly high in geriatric age groups, beta blockers are often prescribed to elderly patients[16,17]. Depending on the selectivity of binding to various beta-adrenergic receptors (i.e., beta-1, beta-2, or beta-3 receptor), beta blockers are classified as nonselective or beta-1-selective. Most bind to beta-1 receptors, causing their inhibition and resulting in negative chronotropic and inotropic effects that reduce cardiac work and oxygen consumption[18]. Beta blockers also protect the heart from the negative effects of excess of catecholamines secondary to sympathetic overstimulation, receptor downregulation, and desensitization, as occurs in heart failure[19,20]. Beta blockers decrease the activity of the renin-angiotensin-aldosterone system by inhibiting renal beta-1 receptors[21]. Inhibition of beta-2 receptors causes some of the adverse effects of beta blockers, such as bronchoconstriction and peripheral vasoconstriction, and inhibition of beta-3 receptors decreases lipolysis in peripheral adipose tissue[22]. Some beta blockers increase the expression and/or activity of beta-3 receptors in the heart, which improves myocardial metabolism in the failing myocardium[23]. Nonselective beta blockers, such as carvedilol, inhibit alpha-adrenergic receptors, causing vasodilation and reduced blood pressure[24]. The binding of beta blockers to adrenergic receptors starts a complex cascade of proteins involved in the genesis of cardiac remodeling, such as mitogen-activated protein kinases, Gs-adenylyl cyclase-cyclic AMP and phosphoinositide 3-kinase signaling[25]. It has been reported that beta-receptor desensitization reduces the therapeutic activity of beta blockers in the elderly and in heart failure patients[26,27]. Studies conducted in aged heart failure patients have clearly confirmed the benefits of beta blockers on relevant clinical endpoints, such as hospitalization and symptoms[28,29].
There are several pharmacologic reasons why treatment with beta blockers may be of benefit for patients with SARS-CoV-2 infection. First, the entry of SARS-CoV-2 into cells involves the binding of viral spike proteins to angiotensin-converting enzyme 2 (ACE2)[30]. ACE2 is expressed in various cells, such as cardiomyocytes, endothelial cells, alveolar macrophages, and type II pneumocytes[31]. SARS-CoV-2 entry downregulates ACE2 receptors, which is followed by dysregulation of the ACE2-mediated pathway that protects against inflammation, and the adverse ACE-mediated axis[32]. Beta blockers downregulate ACE2, thereby reducing the virus' ability to attack cells[33]. However, as beta blockers reduce renin production, they may protect against SARS-CoV-2 infection by preventing the pro-inflammatory action promoted by angiotensin 2[34]. Cardiovascular complications are among the most frequent and feared COVID-19 complications, and beta blocker therapy might help prevent them or result in a milder clinical course. Beta blockers have been used to treat heart failure and arrhythmias secondary to COVID-19 infection[35,36], and treatment of myocarditis associated with COVID-19 may also benefit from the administration of beta blockers[37]. Some beta blockers, such as nebivolol, improve endothelial function by promoting nitric oxide bioavailability[38], which may be protective in diseases like COVID-19 in which endothelial dysfunction is involved[39].
Beta blockers have favorable anti-inflammatory activity that is potentially useful in preventing the cytokine storm of COVID-19[40]. In particular, beta blockers reduce interleukin-6 and decrease the activation of NOD-, LRR- and pyrin domain-containing protein 3 inflammasomes[41]. Hypoxia that occurs in the course of severe SARS-CoV-2 bronchopneumonia results in overactivation of the sym
With the outbreak of the COVID-19 pandemic, a concern of physicians and researchers was that certain chronically taken medications could promote SARS-CoV-2 infection or induce an unfavorable course, especially in geriatric patients[44]. However, the safety of beta blockers regarding the eventual predisposition or worse clinical course of COVID-19 was already evident from the results of early studies in the elderly. A large retrospective study in Spain of 34,936 hypertensive patients of 70.9 ± 11.3 years of age verified that beta blockers are not associated with an increased risk of a subsequent diagnosis with COVID-19[45]. Other studies have ruled out the existence of any association between inpatient mortality from COVID-19 and beta blocker use, including patients in their 90s[46,47]. A meta-analysis of 53 studies of the association of antihypertensive medications with COVID-19 incidence and mortality found a neutral effect of the beta blocker class[48]. There was no association between use of beta blockers and COVID-19 incidence (odds ratio [OR]: 1.03; 95% confidence interval [CI]: 0.78–1.35) or severity (OR: 1.23; 95%CI: 0.74- 2.04). However, only 3 of the 10 studies on beta blockers in the meta-analysis included patients older than 65 years of age, making it difficult to generalize the results to geriatric populations. On the other hand, there is evidence that beta blocker therapy causes clinical improvement and improved survival in patients with COVID-19, including those in older age groups[49-52]. Consistently, the benefits of beta blockers in COVID-19 infection are confirmed by the observation that discontinuation of beta blocker therapy outside the guidelines results in increased in-hospital mortality in COVID-19 patients[53].
Some studies have not found decreased COVID-19 severity in elderly people taking beta blockers. It cannot be excluded that this finding may have resulted from a lack of statistical power[48,54], but a retrospective study excluded the preventive efficacy of beta blockers against COVID-19 infectious risk[55]. Existence of the clinical benefits of beta blockers has been investigated in critically ill COVID-19 patients. A case-control study including 20 patients with acute respiratory distress syndrome and requiring mechanical ventilation found that infusion of the beta blocker metoprolol (15 mg daily for 3 d) improved both oxygenation and the degree of lung inflammation. The investigators argued that metoprolol acted by stunning neutrophils and abrogating exacerbated inflammation[56].
Another mechanism by which metoprolol in infusion could have ameliorated the oxygenation of critical patients with COVID 19 is hemodynamic. In fact, it has been hypothesized that metoprolol, through a reduction in cardiac output, may have consequently reduced the intrapulmonary shunts, therefore improving the ventilation-perfusion ratio[57]. Overall, the available study results exclude that beta blocker therapy may favor worsening of the course of COVID-19 and SARS-CoV-2 infection (Table 1). Conversely, some studies found that elderly patients taking beta blocker therapy had a more favorable clinical COVID-19 course. Nevertheless, the results of the available studies must be interpreted with caution because of possible bias related to small sample size and to the diverse pharmacological properties possessed by the various beta blockers.
| Ref. | Study type | Study aim | Subjects | Study findings |
| Yan F et al[49], 2020 | Multicenter retrospective | Examine association between clinical outcomes with the use of antihypertensive drugs | 665 hypertensive COVID-19 patients (mean age: 64.6 ± 11.8 yr) | Reduced dyspnea in BB users; improved clinical indices |
| Rey JR et al[53], 2020 | Prospective | Study cardiovascular outcomes in patients with COVID-19 and a prior diagnosis of heart failure | 3080 hospitalized COVID-19 patients (mean age: 62.3 ± 20.3 yr) | ↑ in-hospital mortality associated to withdrawal of BB (HR: 4.15; 95%CI: 1.61–10.71) |
| Liu Y et al[54], 2020 | Retrospective | Association between antihypertensive use and disease severity of COVID-19 patients | 46 elderly hypertensive COVID-19 patients (> 65 yr in age) | BB use not associated to less disease severity (OR: 0.49; 95%CI: 0.2–1.98) |
| Saifi Said E et al[51], 2021 | Retrospective | Examine factors associated with survival in older people with COVID-19 | 34 inpatients with COVID-19 ( 90 yr in age) | Better survival in patients treated with BB vs non-treated (P = 0.008 by Kaplan-Meier analysis) |
| Couchana L et al[52], 2021 | Retrospective multicenter cohort study | Investigate association between antihypertensive agent use and in-hospital mortality | 8078 patients hospitalized for COVID-19 (median age: 75.4 yr) | ↓Risk of mortality in BB users (aOR: 0.80; 95%CI: 0.67-0.95) |
| Clemente-Moragón A et al[56], 2021 | Pilot randomized controlled trial | Evaluate the effects of intravenous metoprolol on lung inflammation and oxygenation | 20 COVID-19 patients with ARDS (median age: 60 yr) | Intravenous metoprolol reduced lung inflammation, improved oxygenation, and was safe |
| Blanc F et al[55], 2021 | Retrospective case-control | Find a pharmacological preventive treatment of COVID-19 in elderly patients | 89 COVID-19 patients (mean age: 84.4 yr) compared with 90 non-COVID-19 patients (mean age: 83.8 yr); 40.78% on BB therapy | taking BB does not reduce risk of COVID-19 infection (OR: 1.28; 95%CI: 0.71–2.31, P = 0.7909) |
| Vrillon A et al[47], 2020 | Prospective cohort | Describe clinical features and outcome of COVID-19 elderly inpatients | 76 COVID-19 inpatients (median age: 90 yr) | No difference in BB therapy between survivors vs non-survivors (P = 0.796) |
| Vila-Corcoles A et al[45], 2020 | Population-based retrospective cohort | Investigate relationships between antihypertensive drug use and COVID-19 infection | 34,936 ambulatory hypertensive adults (> 50 yr of age; mean age: 70.9 ± 11.3 yr) | Receiving BB did not significantly alter the risk of PCR-confirmed COVID-19 (HR: 0.97; 95%CI: 0.68-1.37, P = 0.844) |
| Polverino F et al[46], 2020 | Nationwide observational retrospective | Whether hypertension medications may increase the risk of death | 3179 COVID-19 inpatients (58% of patients ≥ 65 yr of age) | Hypertension medication does not significantly increase COVID-19-related deaths in an older population (OR: 0.85; 95%CI: 0.65–1.12, P = 0.244) |
The safety and benefits of beta blocker therapy for treating COVID-19 in elderly patients have been confirmed by various studies, but others have generated important warnings about the use of beta blockers. A recent retrospective observational study including 298 patients of 58.33 ± 15.52 years of age and with 93 who were ≥ 65 years of age reported that beta blocker therapy was paradoxically associated with increased mortality[58]. However, the authors of the study hypothesized that the concurrent use of other drugs may have confounded the results. In addition, it is also unclear whether previous beta blocker therapy may adversely affect the convalescence of elderly people with COVID-19. A study of 115 patients over 68 years of age with severe COVID-19 found that those with prior beta blocker use had worse lung diffusion of carbon monoxide (commonly known as DLCO) during convalescence (OR: 3.93; 95%CI: 1.05–14.76; P = 0.042)[59]. Those taking renin-angiotensin-aldosterone inhibitors tended to have better DLCO levels.
In some clinical settings in geriatric medicine, such as the management of patients with comorbidities or low life expectancy, the use of beta blockers should be carefully evaluated on a case-by-case basis. A recent systematic review demonstrated that beta blockers were a class of drugs, that if inappropriately used, could adversely affect the prognosis of COVID-19[60]. The review considered drugs with potential negative impact on respiratory diseases, such as asthma, chronic obstructive pulmonary disease and respiratory failure, and therefore expressed a preference for the use of selective beta blockers in the COVID-19 scenario. Finally, it is worth noting that expert opinion recommends the decision to introduce a new drug in elderly subjects, including drugs with antihypertensive effects such as beta blockers, should be based on the expected risk-benefit ratio, especially in patients with comorbidities and reduced life expectancy[61].
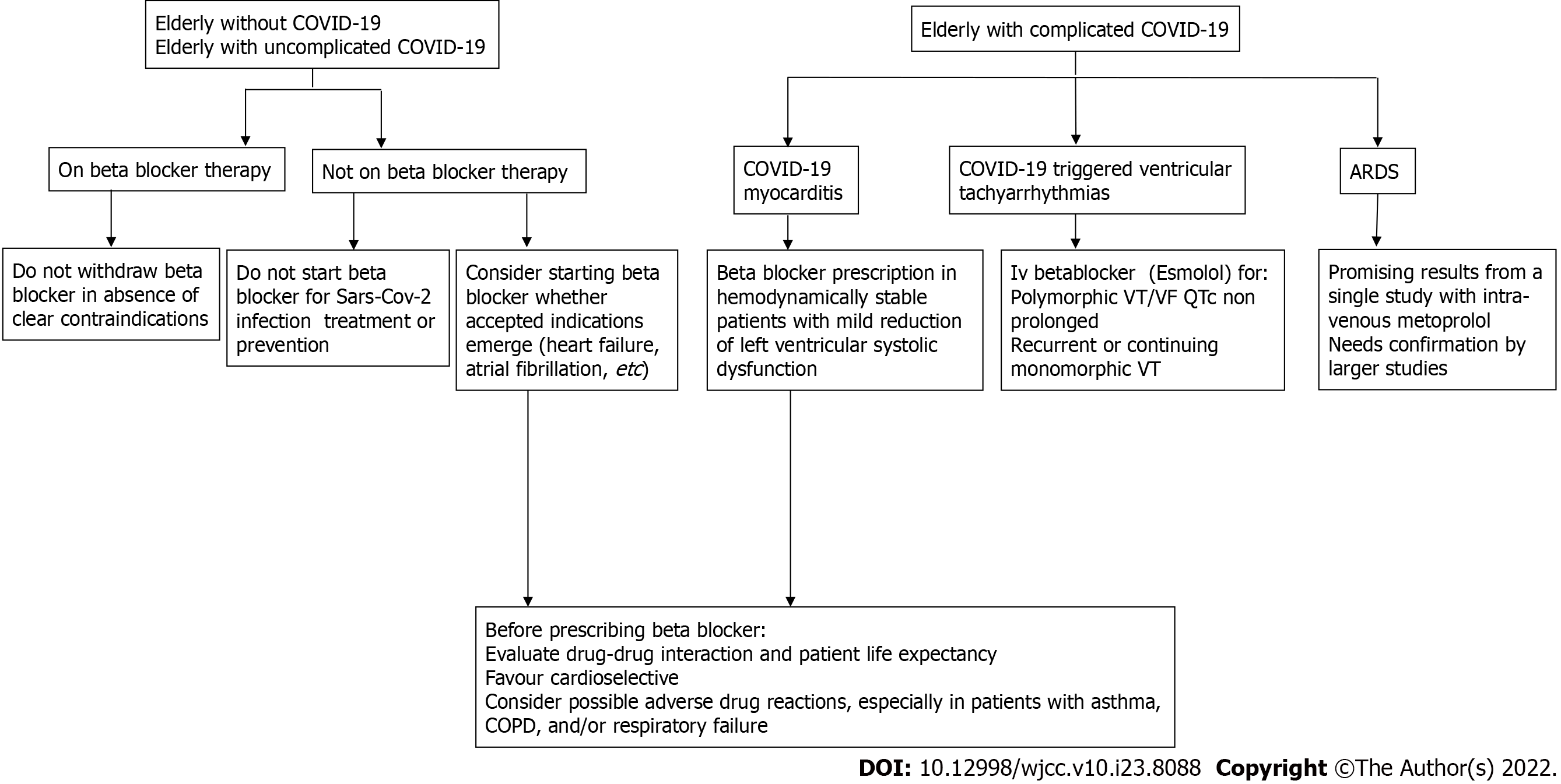
Some strategies for beta blocker use in relation to COVID-19-induced pathologies have already been codified and described in specific guidelines. It is the case of myocarditis that complicates COVID-19 infection. In fact, for COVID-19 myocarditis, beta blockers are recommended in hemodynamically stable subjects with slight reduction of left ventricular function and in stable patients who have had supraventricular arrhythmias[62]. In addition, intravenous administration of a beta blocker (in particular the ultrashort acting Esmolol) has been included in flow charts for the treatment of ventricular tachyarrhythmias triggered by COVID 19 infection[63].
Certainly, promising prospects for the use of beta blockers include the areas of hypertensive urgencies and emergencies in the course of COVID-19 and the treatment of post-COVID autonomic dysfunction[64,65]. On the other hand, strategies for the preventive use of beta blockers, such as the pre-treatment of frail elderly people, are not currently applicable. Indeed, evidence from specific, large clinical trials is lacking. Unfortunately, the design and conduction of these studies appear very problematic for the difficulties of having control groups during pandemic waves, and discriminating the effect of beta blocker from those of other drugs[66].
The available evidence confirms a relevant role for beta blockers for the elderly in the COVID-19 era (Figure 1). There is strong evidence that their discontinuation for fear that they may facilitate the onset of SARS-CoV-2 virus infection is unjustified and COVID-19 should not be a contraindication. By contrast, many studies conducted in geriatric patients found that those with COVID-19 who took beta blockers had less severe infections and better survival. That finding can be interpreted in the light of the pharmacology of the drugs. As discussed, in addition to their primary anti-arrhythmic and anti-ischemic activities, beta blockers also have anti-inflammatory activity and counteract sympathetic hyperactivity that counteract COVID-19 pathogenesis. Some beta blockers (i.e., nebivolol) may produce additional benefits against COVID-19 by increasing nitric oxide bioavailability. Future large studies in elderly patients should clarify the clinical usefulness of beta blocker therapy for the treatment of COVID-19 and the reduction of the risk of fatal complications. Further research is also desirable to investigate the prophylactic use of beta blockers in individuals at risk of contracting severe disease, such as the frail elderly. Finally, future studies should also clarify whether the use of beta blockers in patients already infected with SARS-CoV-2 can reduce post-acute COVID-19 symptomatology and long-term COVID symptoms.
| 1. | Kaye AD, Okeagu CN, Pham AD, Silva RA, Hurley JJ, Arron BL, Sarfraz N, Lee HN, Ghali GE, Gamble JW, Liu H, Urman RD, Cornett EM. Economic impact of COVID-19 pandemic on healthcare facilities and systems: International perspectives. Best Pract Res Clin Anaesthesiol. 2021;35:293-306. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 132] [Cited by in RCA: 358] [Article Influence: 71.6] [Reference Citation Analysis (0)] |
| 2. | Karlinsky A, Kobak D. Tracking excess mortality across countries during the COVID-19 pandemic with the World Mortality Dataset. Elife. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 329] [Cited by in RCA: 316] [Article Influence: 63.2] [Reference Citation Analysis (0)] |
| 3. | Contreras S, Priesemann V. Risking further COVID-19 waves despite vaccination. Lancet Infect Dis. 2021;21:745-746. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 4. | Yang Y, Luo K, Jiang Y, Yu Q, Huang X, Wang J, Liu N, Huang P. The Impact of Frailty on COVID-19 Outcomes: A Systematic Review and Meta-analysis of 16 Cohort Studies. J Nutr Health Aging. 2021;25:702-709. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 5. | D'ascanio M, Innammorato M, Pasquariello L, Pizzirusso D, Guerrieri G, Castelli S, Pezzuto A, De Vitis C, Anibaldi P, Marcolongo A, Mancini R, Ricci A, Sciacchitano S. Age is not the only risk factor in COVID-19: the role of comorbidities and of long staying in residential care homes. BMC Geriatr. 2021;21:63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 59] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 6. | Mendy A, Apewokin S, Wells AA, Morrow AL. Factors Associated with Hospitalization and Disease Severity in a Racially and Ethnically Diverse Population of COVID-19 Patients. medRxiv. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 58] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 7. | Becerra-Muñoz VM, Núñez-Gil IJ, Eid CM, García Aguado M, Romero R, Huang J, Mulet A, Ugo F, Rametta F, Liebetrau C, Aparisi A, Fernández-Rozas I, Viana-Llamas MC, Feltes G, Pepe M, Moreno-Rondón LA, Cerrato E, Raposeiras-Roubín S, Alfonso E, Carrero-Fernández A, Buzón-Martín L, Abumayyaleh M, Gonzalez A, Fernández Ortiz A, Macaya C, Estrada V, Fernández-Pérez C, Gómez-Doblas JJ. Clinical profile and predictors of in-hospital mortality among older patients hospitalised for COVID-19. Age Ageing. 2021;50:326-334. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 72] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 8. | Siddiqi HK, Libby P, Ridker PM. COVID-19 - A vascular disease. Trends Cardiovasc Med. 2021;31:1-5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 226] [Cited by in RCA: 237] [Article Influence: 47.4] [Reference Citation Analysis (10)] |
| 9. | Hessami A, Shamshirian A, Heydari K, Pourali F, Alizadeh-Navaei R, Moosazadeh M, Abrotan S, Shojaie L, Sedighi S, Shamshirian D, Rezaei N. Cardiovascular diseases burden in COVID-19: Systematic review and meta-analysis. Am J Emerg Med. 2021;46:382-391. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 95] [Cited by in RCA: 87] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 10. | ATTACC Investigators, ACTIV-4a Investigators, REMAP-CAP Investigators, Lawler PR, Goligher EC, Berger JS, Neal MD, McVerry BJ, Nicolau JC, Gong MN, Carrier M, Rosenson RS, Reynolds HR, Turgeon AF, Escobedo J, Huang DT, Bradbury CA, Houston BL, Kornblith LZ, Kumar A, Kahn SR, Cushman M, McQuilten Z, Slutsky AS, Kim KS, Gordon AC, Kirwan BA, Brooks MM, Higgins AM, Lewis RJ, Lorenzi E, Berry SM, Berry LR, Aday AW, Al-Beidh F, Annane D, Arabi YM, Aryal D, Baumann Kreuziger L, Beane A, Bhimani Z, Bihari S, Billett HH, Bond L, Bonten M, Brunkhorst F, Buxton M, Buzgau A, Castellucci LA, Chekuri S, Chen JT, Cheng AC, Chkhikvadze T, Coiffard B, Costantini TW, de Brouwer S, Derde LPG, Detry MA, Duggal A, Džavík V, Effron MB, Estcourt LJ, Everett BM, Fergusson DA, Fitzgerald M, Fowler RA, Galanaud JP, Galen BT, Gandotra S, García-Madrona S, Girard TD, Godoy LC, Goodman AL, Goossens H, Green C, Greenstein YY, Gross PL, Hamburg NM, Haniffa R, Hanna G, Hanna N, Hegde SM, Hendrickson CM, Hite RD, Hindenburg AA, Hope AA, Horowitz JM, Horvat CM, Hudock K, Hunt BJ, Husain M, Hyzy RC, Iyer VN, Jacobson JR, Jayakumar D, Keller NM, Khan A, Kim Y, Kindzelski AL, King AJ, Knudson MM, Kornblith AE, Krishnan V, Kutcher ME, Laffan MA, Lamontagne F, Le Gal G, Leeper CM, Leifer ES, Lim G, Lima FG, Linstrum K, Litton E, Lopez-Sendon J, Lopez-Sendon Moreno JL, Lother SA, Malhotra S, Marcos M, Saud Marinez A, Marshall JC, Marten N, Matthay MA, McAuley DF, McDonald EG, McGlothlin A, McGuinness SP, Middeldorp S, Montgomery SK, Moore SC, Morillo Guerrero R, Mouncey PR, Murthy S, Nair GB, Nair R, Nichol AD, Nunez-Garcia B, Pandey A, Park PK, Parke RL, Parker JC, Parnia S, Paul JD, Pérez González YS, Pompilio M, Prekker ME, Quigley JG, Rost NS, Rowan K, Santos FO, Santos M, Olombrada Santos M, Satterwhite L, Saunders CT, Schutgens REG, Seymour CW, Siegal DM, Silva DG Jr, Shankar-Hari M, Sheehan JP, Singhal AB, Solvason D, Stanworth SJ, Tritschler T, Turner AM, van Bentum-Puijk W, van de Veerdonk FL, van Diepen S, Vazquez-Grande G, Wahid L, Wareham V, Wells BJ, Widmer RJ, Wilson JG, Yuriditsky E, Zampieri FG, Angus DC, McArthur CJ, Webb SA, Farkouh ME, Hochman JS, Zarychanski R. Therapeutic Anticoagulation with Heparin in Noncritically Ill Patients with Covid-19. N Engl J Med. 2021;385:790-802. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 574] [Cited by in RCA: 697] [Article Influence: 139.4] [Reference Citation Analysis (0)] |
| 11. | Semenzato L, Botton J, Drouin J, Baricault B, Vabre C, Cuenot F, Penso L, Herlemont P, Sbidian E, Weill A, Dray-Spira R, Zureik M. Antihypertensive Drugs and COVID-19 Risk: A Cohort Study of 2 Million Hypertensive Patients. Hypertension. 2021;77:833-842. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 87] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 12. | Oliver E, Mayor F Jr, D'Ocon P. Beta-blockers: Historical Perspective and Mechanisms of Action. Rev Esp Cardiol (Engl Ed). 2019;72:853-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 13. | Stolfo D, Uijl A, Benson L, Schrage B, Fudim M, Asselbergs FW, Koudstaal S, Sinagra G, Dahlström U, Rosano G, Savarese G. Association between beta-blocker use and mortality/morbidity in older patients with heart failure with reduced ejection fraction. A propensity score-matched analysis from the Swedish Heart Failure Registry. Eur J Heart Fail. 2020;22:103-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | Mulder BA, van Veldhuisen DJ, Crijns HJ, Böhm M, Cohen-Solal A, Babalis D, Roughton M, Flather MD, Coats AJ, Van Gelder IC. Effect of nebivolol on outcome in elderly patients with heart failure and atrial fibrillation: insights from SENIORS. Eur J Heart Fail. 2012;14:1171-1178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Farzam K, Jan A. Beta Blockers. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2022. [PubMed] |
| 16. | Fu M. Beta-blocker therapy in heart failure in the elderly. Int J Cardiol. 2008;125:149-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Díez-Villanueva P, Alfonso F. Atrial fibrillation in the elderly. J Geriatr Cardiol. 2019;16:49-53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 18. | Diaconu CC, Marcu DR, Bratu OG, Stanesc AMA, Gheorghe G, Hlescu AA, Mischianu DL Manea M. Beta-blockers in Cardiovascular Therapy: A Review. J Mind Med Sci. 2019;6:216-223. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 19. | Barrese V, Taglialatela M. New advances in beta-blocker therapy in heart failure. Front Physiol. 2013;4:323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 54] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Ahmed A. Myocardial beta-1 adrenoceptor down-regulation in aging and heart failure: implications for beta-blocker use in older adults with heart failure. Eur J Heart Fail. 2003;5:709-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Fung JW, Yu CM, Yip G, Chan S, Yandle TG, Richards AM, Nicholls MG, Sanderson JE. Effect of beta blockade (carvedilol or metoprolol) on activation of the renin-angiotensin-aldosterone system and natriuretic peptides in chronic heart failure. Am J Cardiol. 2003;92:406-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 87] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 22. | Bordicchia M, Pocognoli A, D'Anzeo M, Siquini W, Minardi D, Muzzonigro G, Dessì-Fulgheri P, Sarzani R. Nebivolol induces, via β3 adrenergic receptor, lipolysis, uncoupling protein 1, and reduction of lipid droplet size in human adipocytes. J Hypertens. 2014;32:389-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 23. | Cannavo A, Koch WJ. Targeting β3-Adrenergic Receptors in the Heart: Selective Agonism and β-Blockade. J Cardiovasc Pharmacol. 2017;69:71-78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 72] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 24. | Carreira RS, Monteiro P, Gon Alves LM, Providência LA. Carvedilol: just another Beta-blocker or a powerful cardioprotector? Cardiovasc Hematol Disord Drug Targets. 2006;6:257-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 25. | Yang J, Liu Y, Fan X, Li Z, Cheng Y. A pathway and network review on beta-adrenoceptor signaling and beta blockers in cardiac remodeling. Heart Fail Rev. 2014;19:799-814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 26. | Ferrara N, Komici K, Corbi G, Pagano G, Furgi G, Rengo C, Femminella GD, Leosco D, Bonaduce D. β-adrenergic receptor responsiveness in aging heart and clinical implications. Front Physiol. 2014;4:396. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 111] [Cited by in RCA: 110] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 27. | Lamba S, Abraham WT. Alterations in adrenergic receptor signaling in heart failure. Heart Fail Rev. 2000;5:7-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 28. | Dulin BR, Haas SJ, Abraham WT, Krum H. Do elderly systolic heart failure patients benefit from beta blockers to the same extent as the non-elderly? Am J Cardiol. 2005;95:896-898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 63] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 29. | Sin DD, McAlister FA. The effects of beta-blockers on morbidity and mortality in a population-based cohort of 11,942 elderly patients with heart failure. Am J Med. 2002;113:650-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 104] [Article Influence: 4.3] [Reference Citation Analysis (1)] |
| 30. | Li Y, Zhou W, Yang L, You R. Physiological and pathological regulation of ACE2, the SARS-CoV-2 receptor. Pharmacol Res. 2020;157:104833. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 288] [Cited by in RCA: 262] [Article Influence: 43.7] [Reference Citation Analysis (0)] |
| 31. | de Vries AAF. Renin-angiotensin system inhibition in COVID-19 patients. Neth Heart J. 2020;28:396-405. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 32. | Verdecchia P, Cavallini C, Spanevello A, Angeli F. The pivotal link between ACE2 deficiency and SARS-CoV-2 infection. Eur J Intern Med. 2020;76:14-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 805] [Cited by in RCA: 906] [Article Influence: 151.0] [Reference Citation Analysis (0)] |
| 33. | Vasanthakumar N. Can beta-adrenergic blockers be used in the treatment of COVID-19? Med Hypotheses. 2020;142:109809. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 34. | Alsagaff MY, Mulia EPB. Hypertension and COVID-19: Potential use of beta-blockers and a call for randomized evidence. Indian Heart J. 2021;73:757-759. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 35. | Lin KC, Wang CC, Huang WC, Hwang JJ. Considerations When Managing Heart Failure during the COVID-19 Pandemic-Consensus from the Taiwan Society of Cardiology. Acta Cardiol Sin. 2021;37:125-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 36. | Russo V, Rago A, Carbone A, Bottino R, Ammendola E, Della Cioppa N, Galante D, Golino P, Nigro G. Atrial Fibrillation in COVID-19: From Epidemiological Association to Pharmacological Implications. J Cardiovasc Pharmacol. 2020;76:138-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 37. | Agdamag ACC, Edmiston JB, Charpentier V, Chowdhury M, Fraser M, Maharaj VR, Francis GS, Alexy T. Update on COVID-19 Myocarditis. Medicina (Kaunas). 2020;56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (1)] |
| 38. | Kumar S, Singh B, Kumari P, Kumar PV, Agnihotri G, Khan S, Kant Beuria T, Syed GH, Dixit A. Identification of multipotent drugs for COVID-19 therapeutics with the evaluation of their SARS-CoV2 inhibitory activity. Comput Struct Biotechnol J. 2021;19:1998-2017. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 39. | Bonaventura A, Vecchié A, Dagna L, Martinod K, Dixon DL, Van Tassell BW, Dentali F, Montecucco F, Massberg S, Levi M, Abbate A. Endothelial dysfunction and immunothrombosis as key pathogenic mechanisms in COVID-19. Nat Rev Immunol. 2021;21:319-329. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 726] [Cited by in RCA: 694] [Article Influence: 138.8] [Reference Citation Analysis (0)] |
| 40. | Vasanthakumar N. Beta-Adrenergic Blockers as a Potential Treatment for COVID-19 Patients. Bioessays. 2020;42:e2000094. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 41. | Barbieri A, Robinson N, Palma G, Maurea N, Desiderio V, Botti G. Can Beta-2-Adrenergic Pathway Be a New Target to Combat SARS-CoV-2 Hyperinflammatory Syndrome? Front Immunol. 2020;11:588724. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 42. | Kjeldsen SE, Narkiewicz K, Burnier M, Oparil S. Potential protective effects of antihypertensive treatments during the Covid-19 pandemic: from inhibitors of the renin-angiotensin system to beta-adrenergic receptor blockers. Blood Press. 2021;30:1-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 43. | Heriansyah T, Nur Chomsy I, Febrianda L, Farahiya Hadi T, Andri Wihastuti T. The Potential Benefit of Beta-Blockers for the Management of COVID-19 Protocol Therapy-Induced QT Prolongation: A Literature Review. Scientia Pharmaceutica. 2020;88:55. [DOI] [Full Text] |
| 44. | Vura NVRK, Sandooja R, Firoz A. To do or not to do: Angiotensin converting enzyme inhibitors/angiotensin receptor blocker in COVID-19 elderly patients. EXCLI J. 2021;20:1145-1151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 45. | Vila-Corcoles A, Satue-Gracia E, Ochoa-Gondar O, Torrente-Fraga C, Gomez-Bertomeu F, Vila-Rovira A, Hospital-Guardiola I, de Diego-Cabanes C, Bejarano-Romero F, Rovira-Veciana D, Basora-Gallisa J. Use of distinct anti-hypertensive drugs and risk for COVID-19 among hypertensive people: A population-based cohort study in Southern Catalonia, Spain. J Clin Hypertens (Greenwich). 2020;22:1379-1388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 46. | Polverino F, Stern DA, Ruocco G, Balestro E, Bassetti M, Candelli M, Cirillo B, Contoli M, Corsico A, D'Amico F, D'Elia E, Falco G, Gasparini S, Guerra S, Harari S, Kraft M, Mennella L, Papi A, Parrella R, Pelosi P, Poletti V, Polverino M, Tana C, Terribile R, Woods JC, Di Marco F, Martinez FD; ItaliCO study group. Comorbidities, Cardiovascular Therapies, and COVID-19 Mortality: A Nationwide, Italian Observational Study (ItaliCO). Front Cardiovasc Med. 2020;7:585866. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 62] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 47. | Vrillon A, Hourregue C, Azuar J, Grosset L, Boutelier A, Tan S, Roger M, Mourman V, Mouly S, Sène D, François V, Dumurgier J, Paquet C; for LRB COVID Group. COVID-19 in Older Adults: A Series of 76 Patients Aged 85 Years and Older with COVID-19. J Am Geriatr Soc. 2020;68:2735-2743. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 48. | Ren L, Yu S, Xu W, Overton JL, Chiamvimonvat N, Thai PN. Lack of association of antihypertensive drugs with the risk and severity of COVID-19: A meta-analysis. J Cardiol. 2021;77:482-491. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 49. | Yan F, Huang F, Xu J, Yang P, Qin Y, Lv J, Zhang S, Ye L, Gong M, Liu Z, Wei J, Xie T, Xu KF, Gao GF, Wang FS, Cai L, Jiang C. Antihypertensive drugs are associated with reduced fatal outcomes and improved clinical characteristics in elderly COVID-19 patients. Cell Discov. 2020;6:77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 50] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 50. | Pinto-Sietsma SJ, Flossdorf M, Buchholz VR, Offerhaus J, Bleijendaal H, Beudel M, Volders PGA, Ter Bekke RMA, Dormans T, Zwetsloot PP, de Jager P, Massberg S, Rämer P, Wendtner C, Hoffmann E, Rothe K, Feihl S, Kessler T, Pinto YM, Schunkert H. Antihypertensive drugs in COVID-19 infection. Eur Heart J Cardiovasc Pharmacother. 2020;6:415-416. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 51. | Saifi ES, Giorgi-Pierfranceschi M, Salvetti M, Maninetti L, Cavalli I, Muiesan ML. Factors associated with survival in older patients affected by COVID-19: A retrospective cohort study. Arch Gerontol Geriatr. 2021;94:104349. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 52. | Chouchana L, Beeker N, Garcelon N, Rance B, Paris N, Salamanca E, Polard E, Burgun A, Treluyer JM, Neuraz A; AP-HP/Universities/Inserm COVID-19 research collaboration, AP-HP Covid CDR Initiative, and “Entrepôt de Données de Santé” AP-HP Consortium”. Association of Antihypertensive Agents with the Risk of In-Hospital Death in Patients with Covid-19. Cardiovasc Drugs Ther. 2022;36:483-488. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 53. | Rey JR, Caro-Codón J, Rosillo SO, Iniesta ÁM, Castrejón-Castrejón S, Marco-Clement I, Martín-Polo L, Merino-Argos C, Rodríguez-Sotelo L, García-Veas JM, Martínez-Marín LA, Martínez-Cossiani M, Buño A, Gonzalez-Valle L, Herrero A, López-Sendón JL, Merino JL; CARD-COVID Investigators. Heart failure in COVID-19 patients: prevalence, incidence and prognostic implications. Eur J Heart Fail. 2020;22:2205-2215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 107] [Cited by in RCA: 175] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 54. | Liu Y, Huang F, Xu J. Anti-hypertensive Angiotensin II receptor blockers associated to mitigation of disease severity in elderly COVID-19 patients. medRxiv 2020. [DOI] [Full Text] |
| 55. | Blanc F, Waechter C, Vogel T, Schorr B, Demuynck C, Hunyadi CM, Meyer M, Mutelica D, Bougaa N, Fafi-Kremer S, Calabrese L, Schmitt E, Imperiale D, Jehl C, Boussuge A, Suna C, Weill F, Matzinger A, Muller C, Karcher P, Kaltenbach G, Sauleau E. Therapeutic prevention of COVID-19 in elderly: a case-control study. Geroscience. 2021;43:2333-2343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 56. | Clemente-Moragón A, Martínez-Milla J, Oliver E, Santos A, Flandes J, Fernández I, Rodríguez-González L, Serrano Del Castillo C, Ioan AM, López-Álvarez M, Gómez-Talavera S, Galán-Arriola C, Fuster V, Pérez-Calvo C, Ibáñez B. Metoprolol in Critically Ill Patients With COVID-19. J Am Coll Cardiol. 2021;78:1001-1011. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 57. | de Roquetaillade C, Guillemin J, Beaucoté V, Barthelemy R, Chousterman BG. Beta-Blockers in COVID-ARDS: Inflammation or Hemodynamic? J Am Coll Cardiol. 2022;79:e11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 58. | Toprak İD, Sağlam S, Aşikoğlu B, Eruzun H, Öksüz S, Altunok ES. Do age, hypertension, coronary artery disease, ace-I, ARB or beta-blockers therapy increase the risk of mortality in COVID 19 patients? Acta Medica Mediterranea. 2021;37:547. [DOI] [Full Text] |
| 59. | Gori M, Ghirardi A, D'Elia E, Imeri G, Di Marco F, Gavazzi A, Carobbio A, Balestrieri G, Giammarresi A, Trevisan R, Amoroso M, Raimondi F, Novelli L, Magro B, Mangia G, Lorini FL, Fagiuoli S, Barbui T, Rizzi M, Cosentini R, Sironi S, Senni M; of HPG23 Covid-19 Study Group. Association between inhibitors of the renin-angiotensin system and lung function in elderly patients recovered from severe COVID-19. Eur J Prev Cardiol. 2022;29:e196-e199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 60. | Forgerini M, Schiavo G, Lucchetta RC, Carvalho Mastroianni P. Drug interactions for elderly with respiratory disorders and times of covid-19: A systematic scoping review. Vitae. 2020;27:1-14. [DOI] [Full Text] |
| 61. | Aronow WS. Managing the elderly patient with hypertension: current strategies, challenges, and considerations. Expert Rev Cardiovasc Ther. 2020;18:117-125. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 62. | Writing Committee. , Gluckman TJ, Bhave NM, Allen LA, Chung EH, Spatz ES, Ammirati E, Baggish AL, Bozkurt B, Cornwell WK 3rd, Harmon KG, Kim JH, Lala A, Levine BD, Martinez MW, Onuma O, Phelan D, Puntmann VO, Rajpal S, Taub PR, Verma AK. 2022 ACC Expert Consensus Decision Pathway on Cardiovascular Sequelae of COVID-19 in Adults: Myocarditis and Other Myocardial Involvement, Post-Acute Sequelae of SARS-CoV-2 Infection, and Return to Play: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022;79:1717-1756. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 329] [Cited by in RCA: 272] [Article Influence: 68.0] [Reference Citation Analysis (0)] |
| 63. | Task Force for the management of COVID-19 of the European Society of Cardiology. ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic: part 2-care pathways, treatment, and follow-up. Eur Heart J. 2022;43:1059-1103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 98] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 64. | Angeli F, Verdecchia P, Reboldi G. Pharmacotherapy for hypertensive urgency and emergency in COVID-19 patients. Expert Opin Pharmacother. 2022;23:235-242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 65. | Desai AD, Boursiquot BC, Moore CJ, Gopinathannair R, Waase MP, Rubin GA, Wan EY. Autonomic dysfunction post-acute COVID-19 infection. HeartRhythm Case Rep. 2022;8:143-146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 66. | Brüssow H. COVID-19: From pathogenesis models to the first drug trials. Microb Biotechnol. 2020;13:1289-1299. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ahmed SK, Iraq; Gupta S, United States; Sun XD, China; Wang D, Thailand S-Editor: Wang LL L-Editor: A P-Editor: Wang LL