Published online Jun 26, 2022. doi: 10.12998/wjcc.v10.i18.6241
Peer-review started: November 30, 2021
First decision: March 11, 2022
Revised: March 16, 2022
Accepted: April 27, 2022
Article in press: April 27, 2022
Published online: June 26, 2022
Processing time: 198 Days and 14.1 Hours
At present, cases of esophageal neuroendocrine tumors combined with cardia adenocarcinoma are extremely rare worldwide, and there are no clinical reports. Herein, we describe such a case for clinical reference.
The presence of cardia cancer and esophageal neuroendocrine tumors in a single patient has not yet been reported. The patient in this case underwent prompt endoscopic treatment and additional surgical resection. Pathology revealed the following: The distance between the cardia cancer and the esophageal neuroendocrine tumors was small, approximately 3 mm. Vascular invasion was observed. The esophageal neuroendocrine tumor was determined to be grade G3. According to the treatment guidelines, after the patient received an explanation of their condition, additional surgical procedures were provided in a timely manner. Early detection and early treatment can successfully prolong survival and improve the quality of life of patients.
Early detection and early treatment can successfully prolong survival and improve the quality of life of such patients.
Core Tip: Cases of esophageal neuroendocrine tumors combined with moderately differentiated gastric cardia adenocarcinoma are very rare. Pathology is the gold standard for diagnosis. Endoscopy and additional surgical resection proved to be successful in our case. Early detection and early treatment are both of great significance to the life and health of patients. Considering the successful resection of this case, we provide this case report to serve as a clinical reference.
- Citation: Kong ZZ, Zhang L. Esophagogastric junctional neuroendocrine tumor with adenocarcinoma: A case report. World J Clin Cases 2022; 10(18): 6241-6246
- URL: https://www.wjgnet.com/2307-8960/full/v10/i18/6241.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i18.6241
At present, cases of esophageal neuroendocrine tumors (NETs) combined with cardia adenocarcinoma are extremely rare worldwide. The presence of cardia cancer and esophageal NETs (E-NETs) in a single patient has not yet been reported. Herein, we describe such a case for clinical reference.
A 76-year-old man was hospitalized due to the presence of a cardia mass.
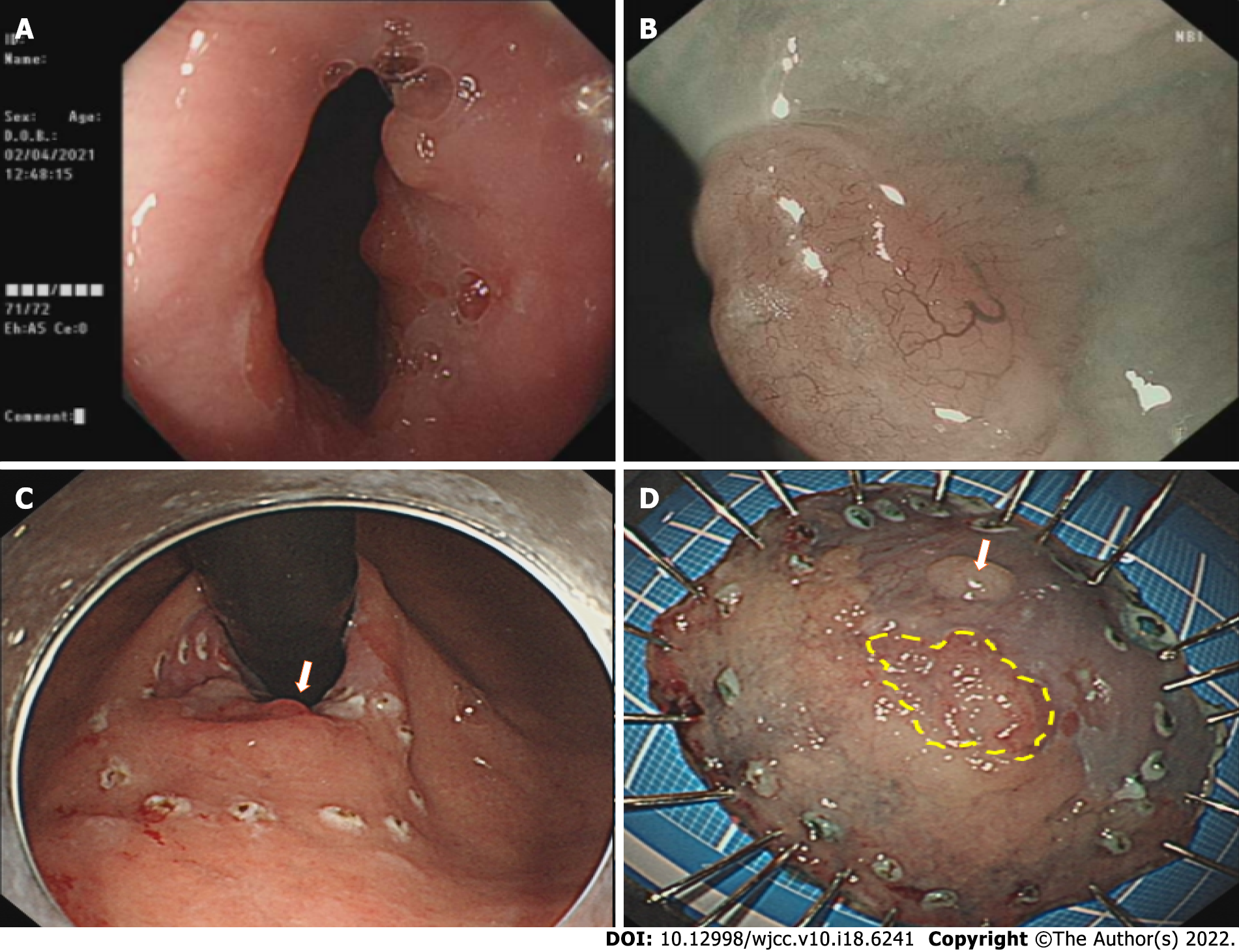
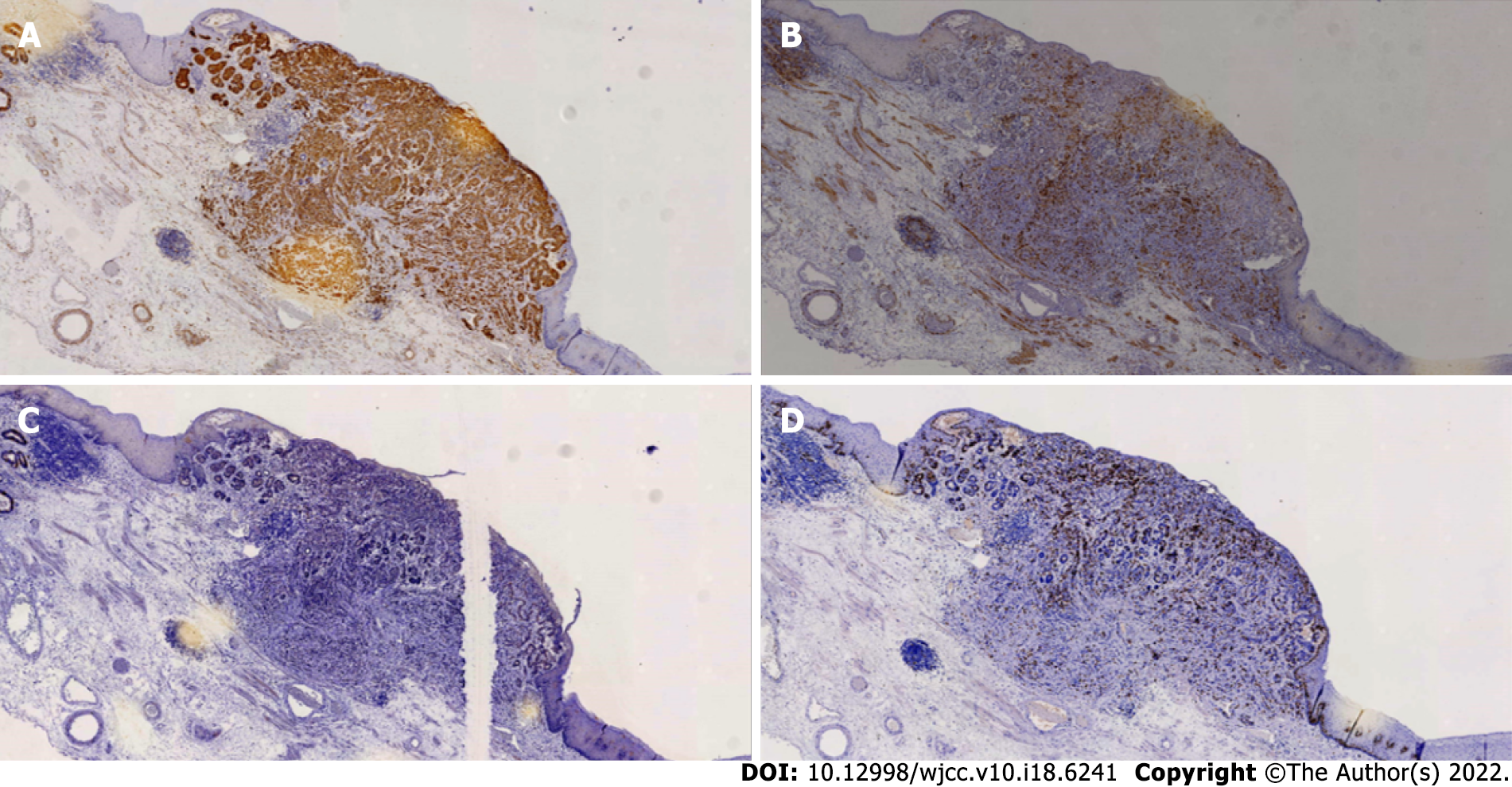
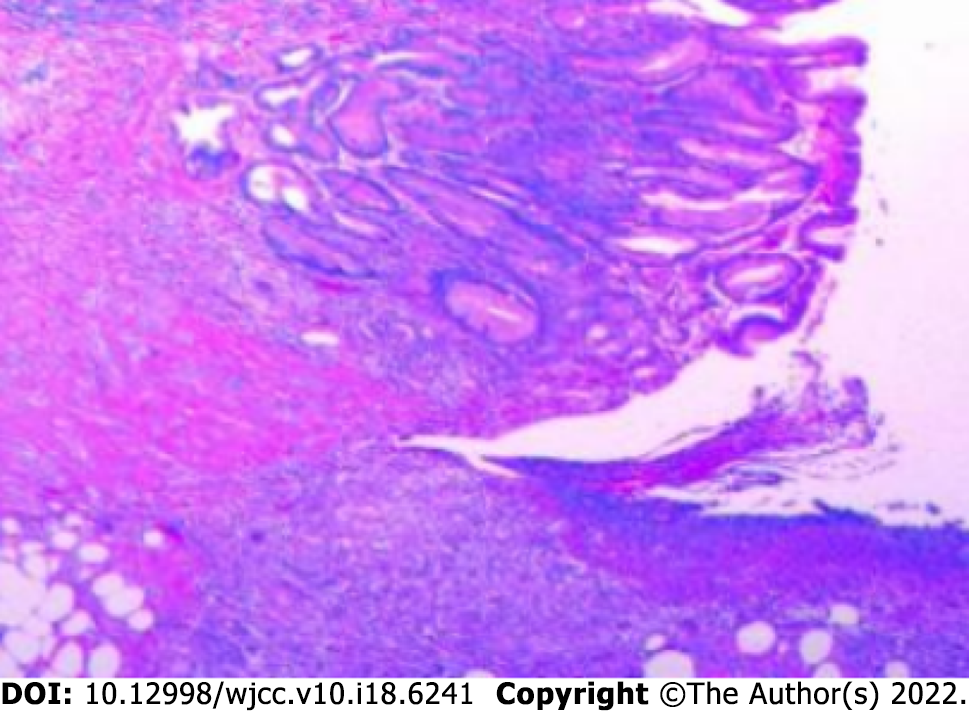
Previous gastroscopy showed a 0-IIa-like cardia lesions and chronic atrophic gastritis with erosions. The pathological examination revealed the following: Tubular adenoma with high-grade intraepithelial neoplasia; mild chronic atrophic gastritis of the antrum; intestinal metaplasia; and Helicobacter pylori infection (Figure 1).
The patient’s medical history was unremarkable.
The patient’s personal/family history was unremarkable.
No remarkable characteristics were found during the physical examination.
The laboratory results were all normal.
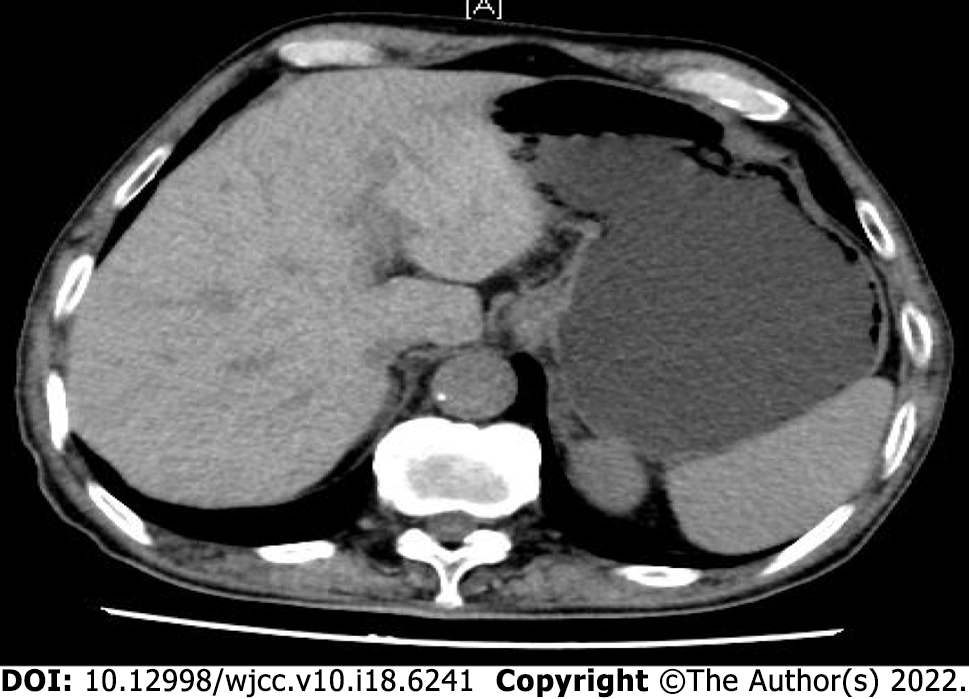
Previous gastroscopy showed a 0-IIa-like lesion of the cardia and chronic atrophic gastritis with erosions. Enhanced computed tomography scan of the full abdomen was performed after hospitalization, which revealed that the local gastric wall of the gastric cardia was slightly thickened, no significantly enlarged lymph node shadow was seen around the cardia, and the rest of the region appeared unchanged (Figures 2-4).
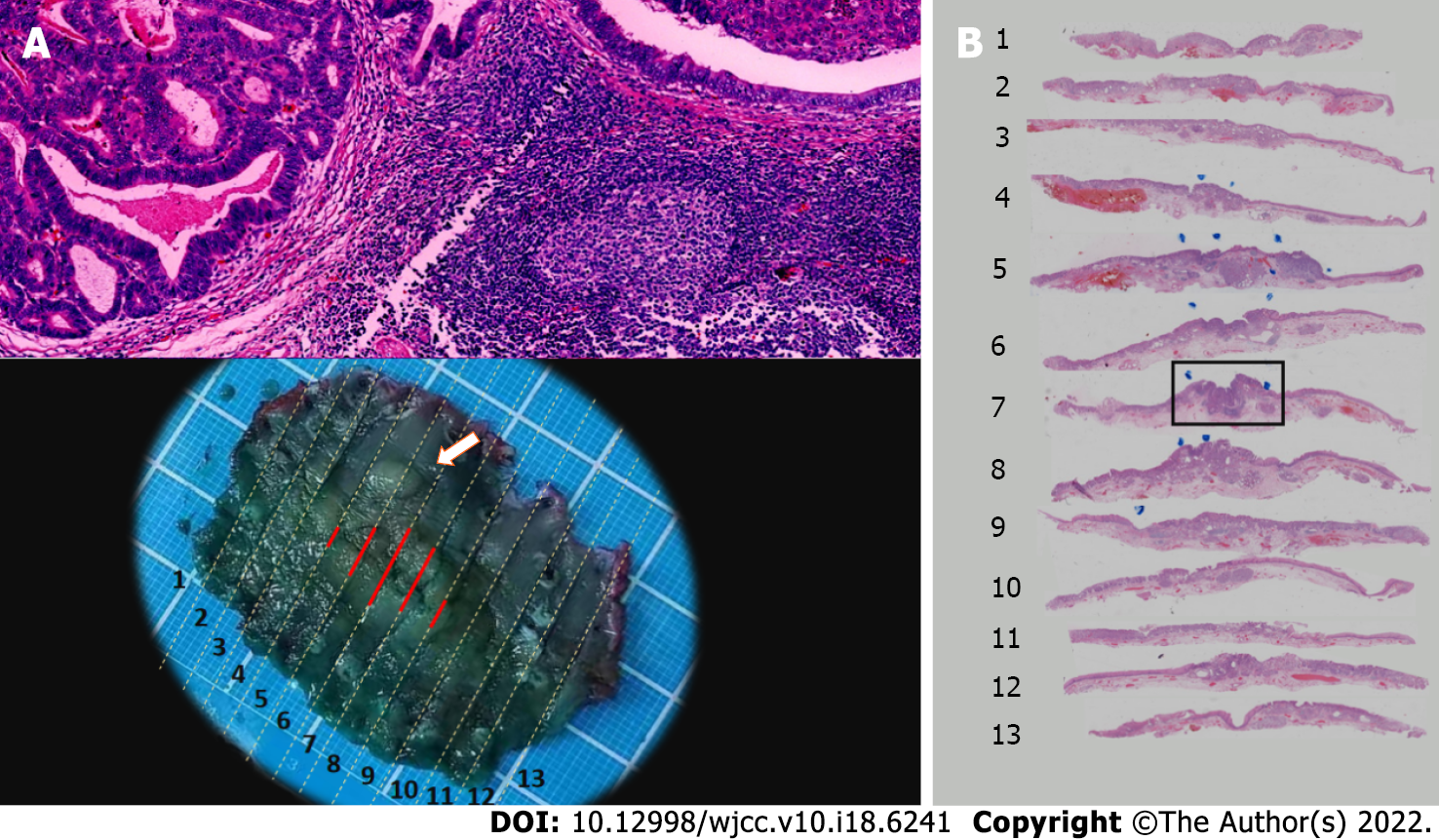
The final diagnosis was differentiated cardia adenocarcinoma and E-NET (G3).
Endoscopic submucosal dissection and surgical resection were performed.
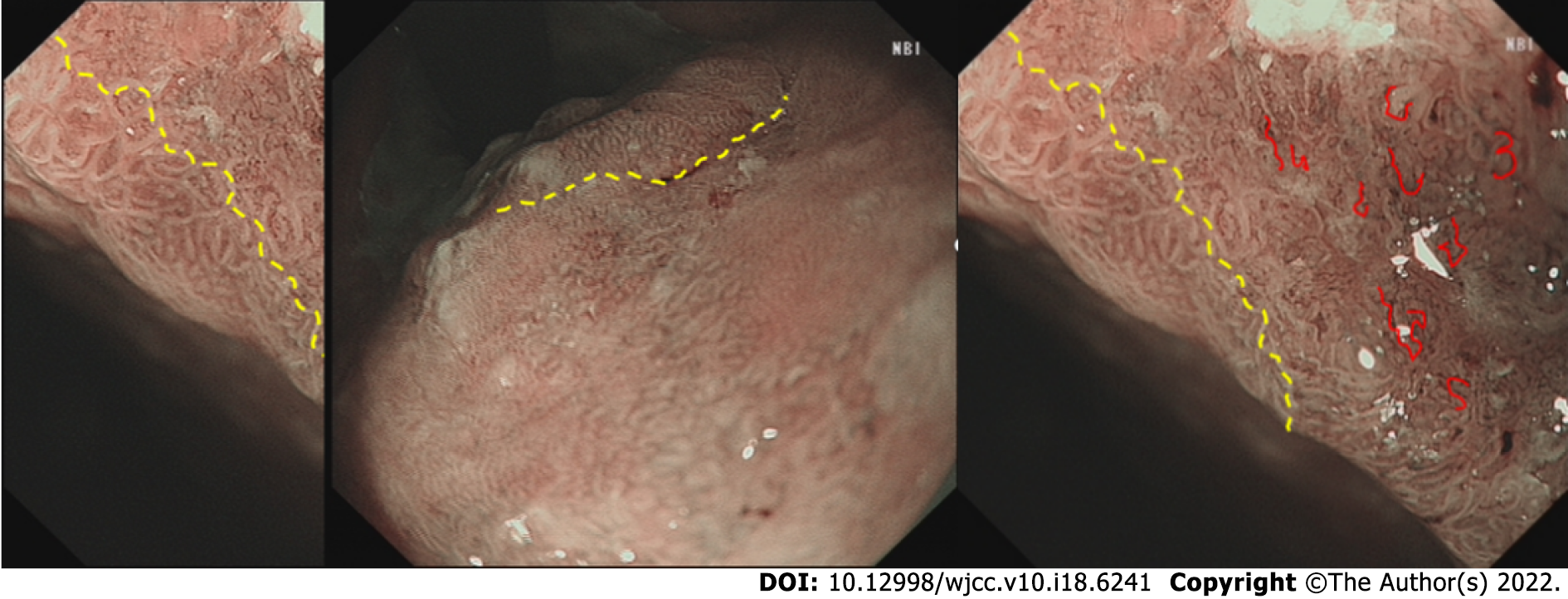
The patient was in good general condition without obvious discomfort (Figures 5 and 6).
NENs are a group of highly heterogeneous tumors originating from neuroendocrine cells. They can occur in many parts of the body but are most often found in the digestive system, followed by the lungs. E-NETs are very rare[1], accounting for only 1.4% of all gastrointestinal pancreatic tumors[2] and 0.15%-2.80% of all esophageal tumors[3]. This is due to the poor development of the neuroendocrine system in this area of the body[2]. The incidence rate varies across countries[4]; these tumors are more commonly found in Asian countries than in Western countries[5]. Studies have found that smoking (present in 49%) and drinking (present in 31%) may be a high-risk factor[6,7]. At present, cases of E-NETs combined with cardia adenocarcinoma are extremely rare worldwide, and there are no clinical reports.
Pathology is the gold standard for the diagnosis of NETs. The proliferation activity of tumor cells can be evaluated by the number of mitotic figures or the Ki-67 index. According to the 2019 WHO classification standards, NETs are divided into three grades: G1, G2, and G3. The classification criteria are as follows: G1 is defined as < 2 mitotic cells/10 high-power fields (HPFs), G2 as 2-20 cells/10 HPFs, and G3 as > 20 cells/10 HPFs. The Ki-67 index is classified as follows: G1, ≤ 2%; G2, 3%-20%; and G3, > 20%[8]. When the Ki-67 index is inconsistent with the mitotic cell classification, it can instead be classified as high or low. DAXX/ATRX and p53/RB mutations can be used to distinguish G3 NETs from neuroendocrine carcinomas (NECs). According to the guidelines, NETs are < 1 cm in size, are grade G1/G2, have a low metastasis rate (< 3%), and do not infiltrate into the muscularis propria (T1 stage). Thus, they are suitable for endoscopic treatment. For tumors or NECs more than 2 cm in diameter, the metastasis rate can reach as high as 60% to 80%, so radical resection is the first choice.
A case of cardia adenocarcinoma combined with E-NETs has not yet been reported. In our patient, after timely endoscopic treatment, pathology revealed that the distance between the cardia cancer and the E-NETs was small, approximately 3 mm, vascular invasion was observed, and the E-NET was determined to be grade G3. According to the treatment guidelines, after the patient received an explanation of their condition, additional surgical procedures were provided in a timely manner. Complete resection of the lesion significantly improved the patient’s quality of life.
| 1. | Chin YP, Lai WF, Chiang MT, Chang SC. Esophageal neuroendocrine tumor with initial presentation as painless forehead and neck masses: A case report. Medicine (Baltimore). 2017;96:e9282. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Lee CG, Lim YJ, Park SJ, Jang BI, Choi SR, Kim JK, Kim YT, Cho JY, Yang CH, Chun HJ, Song SY; Neuroendocrine tumor study group. The clinical features and treatment modality of esophageal neuroendocrine tumors: a multicenter study in Korea. BMC Cancer. 2014;14:569. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 3. | Weinberg JS, Suki D, Hanbali F, Cohen ZR, Lenzi R, Sawaya R. Metastasis of esophageal carcinoma to the brain. Cancer. 2003;98:1925-1933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 91] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Egashira A, Morita M, Kumagai R, Taguchi KI, Ueda M, Yamaguchi S, Yamamoto M, Minami K, Ikeda Y, Toh Y. Neuroendocrine carcinoma of the esophagus: Clinicopathological and immunohistochemical features of 14 cases. PLoS One. 2017;12:e0173501. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 5. | Sorbye H, Welin S, Langer SW, Vestermark LW, Holt N, Osterlund P, Dueland S, Hofsli E, Guren MG, Ohrling K, Birkemeyer E, Thiis-Evensen E, Biagini M, Gronbaek H, Soveri LM, Olsen IH, Federspiel B, Assmus J, Janson ET, Knigge U. Predictive and prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3): the NORDIC NEC study. Ann Oncol. 2013;24:152-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 601] [Cited by in RCA: 742] [Article Influence: 53.0] [Reference Citation Analysis (0)] |
| 6. | Wu IC, Chu YY, Wang YK, Tsai CL, Lin JC, Kuo CH, Shih HY, Chung CS, Hu ML, Sun WC, Wang JP, Wang HP. Clinicopathological features and outcome of esophageal neuroendocrine tumor: A retrospective multicenter survey by the digestive endoscopy society of Taiwan. J Formos Med Assoc. 2021;120:508-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Huang Q, Wu H, Nie L, Shi J, Lebenthal A, Chen J, Sun Q, Yang J, Huang L, Ye Q. Primary high-grade neuroendocrine carcinoma of the esophagus: a clinicopathologic and immunohistochemical study of 42 resection cases. Am J Surg Pathol. 2013;37:467-483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 80] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 8. | Nagtegaal ID, Odze RD, Klimstra D, Paradis V, Rugge M, Schirmacher P, Washington KM, Carneiro F, Cree IA; WHO Classification of Tumours Editorial Board. The 2019 WHO classification of tumours of the digestive system. Histopathology. 2020;76:182-188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2554] [Cited by in RCA: 2759] [Article Influence: 459.8] [Reference Citation Analysis (3)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work noncommercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Casella C, Italy; Chiba H, Japan; Hunasanahalli Giriyappa V, India; Mohamed SY, Egypt; Viswanath Y, United Kingdom S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Fan JR