Published online Jun 16, 2022. doi: 10.12998/wjcc.v10.i17.5841
Peer-review started: December 12, 2021
First decision: February 8, 2022
Revised: February 18, 2022
Accepted: April 9, 2022
Article in press: April 9, 2022
Published online: June 16, 2022
Processing time: 178 Days and 18.7 Hours
Barrett’s esophagus is a known complication of long-standing gastroesophageal reflux disease, and it is a potential risk factor of developing esophageal adenocarcinoma.
Here, we present a case of a 47-year-old male patient referred to the gastroenterology clinic for upper endoscopy because he has a long-standing history of heartburn and vomiting after meals. On examination, he had characteristic findings of self-induced vomiting as abrasions and callosities on the dorsum of the right hand and dental erosions. A detailed history revealed that he had 17 years of binge eating with self-induced vomiting. His upper endoscopy showed gastroesophageal reflux grade D with salmon-red mucosal projections, and the biopsy revealed intestinal mucosal metaplasia.
This case emphasized the importance of considering upper endoscopy screening for Barrett’s esophagus in patients with eating disorders, especially those with self-induced vomiting, as in bulimia nervosa.
Core Tip: Barrett’s esophagus is a known complication of long-standing gastroesophageal reflux disease. Here, we present a case of a 47-year-old male patient with a long-standing history of heartburn and vomiting after meals. Upper endoscopy showed gastroesophageal reflux grade D with intestinal mucosal metaplasia. This emphasized the importance of considering upper endoscopy screening for Barrett’s esophagus in patients with eating disorders, especially those with self-induced vomiting, as in bulimia nervosa.
- Citation: Gouda A, El-Kassas M. Barrett’s esophagus in a patient with bulimia nervosa: A case report. World J Clin Cases 2022; 10(17): 5841-5845
- URL: https://www.wjgnet.com/2307-8960/full/v10/i17/5841.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i17.5841
Barrett’s esophagus is the condition in which metaplastic columnar epithelial cells with gastric and intestinal features replace the stratified squamous epithelium that normally lines the distal esophagus. The condition develops due to chronic gastroesophageal reflux disease (GERD) and is a significant risk factor for adenocarcinoma of the esophagus[1]. Bulimia nervosa is characterized by recurrent episodes of binge eating followed by inappropriate compensatory behavior to prevent weight gain, such as self-induced vomiting, misuse of medications such as laxatives, diuretics, insulin, or thyroid hormone[2].
Binge eating disorder represents a real health problem. Low treatment rates highlight the importance of questioning patients about eating problems even when not mentioned in their presenting complaints[3]. The complications that occur with bulimia nervosa can affect many organ systems and depend upon the method and frequency of purging (i.e. self-induced vomiting or misuse of laxatives, diuretics, or enemas)[4]. Gastrointestinal complications of bulimia nervosa can include GERD and Barrett’s esophagus[5].
We present a case of a 47-year-old male patient referred for upper endoscopy for having heartburn and vomiting after meals.
The patient denied any history of eating or psychological disorders.
Upon intense history taking and after several attempts, the patient reported a 17-year history of having frequent heavy meals and drinking large amounts of carbonated drinks up to 10 cans every day, followed by self-induced vomiting using the index finger of the right hand. This condition confirms the diagnosis of bulimia nervosa. The patient also reported heavy smoking of Shisha.
His body mass index was maintained throughout this period, with no significant medical history.
Upon physical examination, abrasions and callosities were noticed on the dorsum of the right hand (Russell’s sign of self-induced vomiting, Figure 1A), and teeth erosions were observed (Figure 1B).
Routine laboratory investigations were within the accepted ranges.
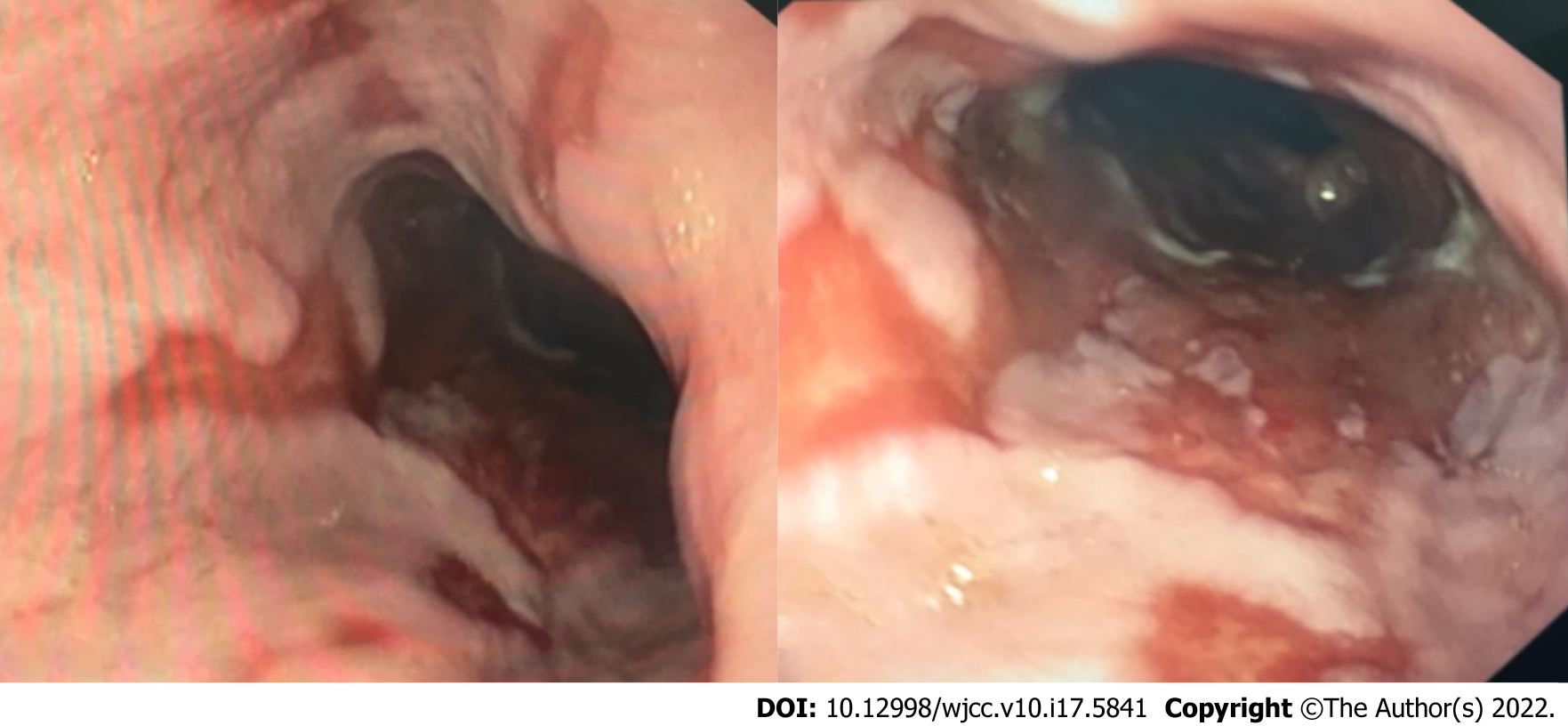
Upper endoscopic examination showed incompetent dilated cardia with GERD grade D (Los Angeles classification). The lesions started 25 cm from the incisors. Salmon-red mucosal projections into the esophageal lumen and mucosal islands were observed. Multiple biopsies were taken, which later showed metaplastic columnar epithelium typical for Barrett’s esophagus without dysplasia (Figure 2).
The patient was diagnosed with bulimia nervosa and Barrett’s esophagus.
Long-term acid suppression was decided as a treatment for Barrett’s esophagus, in addition to the scheduling of an endoscopic surveillance program.
Patient was referred for psychiatric consultation.
GERD symptoms in patients with eating disorders such as bulimia nervosa are usually linked to repeated, self-induced vomiting, but the relationship is still unclear[6]. Acid exposure is not limited to purging patients; binge eating itself, which is commonly associated with various esophageal disorders, could be a risk factor for GERD[7].
Repeated acid exposure can be associated with the development of Barrett’s esophagus, whereby the esophageal squamous epithelium is replaced by metaplastic columnar epithelium, being more susceptible to malignancy[8]. Theoretically speaking, prolonged standing self-induced vomiting may be associated with the development of Barrett’s esophagus, but there is no definitive conclusion can be reached due to lack of data[9]. Barrett’s esophagus is associated with a 30-fold increased risk of developing esophageal adenocarcinoma over the general population[10]. Moreover, there are few case reports of patients with bulimia nervosa presenting with worsening epigastric pain and reflux who were finally diagnosed with esophageal adenocarcinoma[11].
In our case, there was a history of upper gastrointestinal problems, which was the chief presenting complaint. On the other hand, a more profound history revealed the riddle of the bulimia nervosa diagnosis that was beneath this presenting ailment. The patient had been suffering from bulimia nervosa for 17 years without a diagnosis because of his unwillingness to consult a therapist or because of the stigma possibly associated with the disease in his imagination. The patient had a history of binge eating episodes, including increased calorie intake and compensatory purging to eliminate the extra food intake. This led to the diagnosis of bulimia nervosa induced Barrett’s esophagus in our case, which is a rare occurrence. Many cohort studies reported that patients with Barrett’s esophagus who received maintenance therapy with proton pump inhibitors had a lower probability of developing neoplastic Barrett’s esophagus than those who did not receive maintenance therapy[12]. Diagnosing Barrett’s esophagus in such cases should make a difference, considering the possibility of prescribing long-term proton pump inhibitors.
A thorough understanding of the risk factors for Barrett’s esophagus is required to combat the rising incidence of this precancerous lesion worldwide. The emerging risk factors for GERD and Barrett’s esophagus must be updated considering the rising incidence of psychological eating disorders in today’s world. Additionally, providers should consider endoscopic evaluation of patients with eating disorders who have persistent symptoms of dyspepsia or vomiting, given the potential risk of esophageal precancerous and cancerous disorders.
| 1. | Que J, Garman KS, Souza RF, Spechler SJ. Pathogenesis and Cells of Origin of Barrett's Esophagus. Gastroenterology. 2019;157:349-364.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 102] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 2. | Torjesen I. Diabulimia: the world's most dangerous eating disorder. BMJ. 2019;364:l982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Benjet C, Bruffaerts R, de Girolamo G, de Graaf R, Maria Haro J, Kovess-Masfety V, O'Neill S, Posada-Villa J, Sasu C, Scott K, Viana MC, Xavier M. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol Psychiatry. 2013;73:904-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 898] [Cited by in RCA: 868] [Article Influence: 66.8] [Reference Citation Analysis (0)] |
| 4. | Forney KJ, Buchman-Schmitt JM, Keel PK, Frank GK. The medical complications associated with purging. Int J Eat Disord. 2016;49:249-259. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 100] [Cited by in RCA: 83] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 5. | Brown CA, Mehler PS. Medical complications of self-induced vomiting. Eat Disord. 2013;21:287-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Denholm M, Jankowski J. Gastroesophageal reflux disease and bulimia nervosa--a review of the literature. Dis Esophagus. 2011;24:79-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Peat CM, Huang L, Thornton LM, Von Holle AF, Trace SE, Lichtenstein P, Pedersen NL, Overby DW, Bulik CM. Binge eating, body mass index, and gastrointestinal symptoms. J Psychosom Res. 2013;75:456-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Lin JA, Woods ER, Bern EM. Common and Emergent Oral and Gastrointestinal Manifestations of Eating Disorders. Gastroenterol Hepatol (N Y). 2021;17:157-167. [PubMed] |
| 9. | Pacciardi B, Cargioli C, Mauri M. Barrett's esophagus in anorexia nervosa: a case report. Int J Eat Disord. 2015;48:147-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Van der Veen AH, Dees J, Blankensteijn JD, Van Blankenstein M. Adenocarcinoma in Barrett's oesophagus: an overrated risk. Gut. 1989;30:14-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 148] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 11. | Shinohara ET, Swisher-McClure S, Husson M, Sun W, Metz JM. Esophageal cancer in a young woman with bulimia nervosa: a case report. J Med Case Rep. 2007;1:160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Marabotto E, Pellegatta G, Sheijani AD, Ziola S, Zentilin P, De Marzo MG, Giannini EG, Ghisa M, Barberio B, Scarpa M, Angriman I, Fassan M, Savarino V, Savarino E. Prevention Strategies for Esophageal Cancer-An Expert Review. Cancers (Basel). 2021;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Egypt
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Nagahara H, Japan; Sato Y, Japan S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR