Published online May 26, 2022. doi: 10.12998/wjcc.v10.i15.5077
Peer-review started: December 10, 2021
First decision: January 26, 2022
Revised: January 30, 2022
Accepted: March 26, 2022
Article in press: March 26, 2022
Published online: May 26, 2022
Processing time: 165 Days and 6.3 Hours
Cardiac transplantation is considered the standard treatment for refractory end-stage heart failure. Worldwide, 5074 heart transplantations were performed in 2015. About 100 heart transplants are performed at the authors’ center each year. The usual complications of heart transplantation include graft rejection, infection, and graft dysfunction. Aortic dissection after heart transplantation is very rare and is a serious complication that requires a hybrid procedure.
A 58-year-old female patient was admitted to Union Hospital Affiliated to Tongji Medical College of Huazhong University of Science and Technology in July 2020 because of unprovoked low back pain without precipitating causes. Magnetic resonance imaging and computed tomography angiography showed type A aortic dissection with an aberrant right subclavian artery. After admission, urapidil was used to control blood pressure. Ten days later, the patient underwent ascending aortic and aortic arch replacement, subclavian artery reconstruction, and endovascular repair of abdominal and thoracic aortic aneurysms. A cardiopulmonary bypass was established through the right femoral artery and femoral vein. The aberrant right subclavian artery, innominate artery, left common carotid artery, and left subclavian artery were blocked, and the left and right common carotid arteries were cannulated for bilateral cerebral perfusion.
The right axillary artery could not be selected for cardiopulmonary bypass intubation because of aberrant right subclavian artery.
Core Tip: There is a risk of hypertension after heart transplantation. Hypertension is a risk factor for aortic dissection that needs surgery. Hybrid procedure shortened the operation time and reduced complications. In this case, the patient had an aberrant right subclavian artery, and unilateral antegrade cerebral perfusion through the right axillary artery cannot be performed.
- Citation: Zeng Z, Yang LJ, Zhang C, Xu F. Type A aortic dissection following heart transplantation: A case report. World J Clin Cases 2022; 10(15): 5077-5081
- URL: https://www.wjgnet.com/2307-8960/full/v10/i15/5077.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i15.5077
Heart transplant recipients are at risk for post-transplantation complications such as rejection, infection, and graft dysfunction[1]. Post-transplantation aortic dissection is rare. The course of the disease and its surgical management are reported here.
A 58-year-old female patient was admitted to our center because of low back pain without precipitating causes.
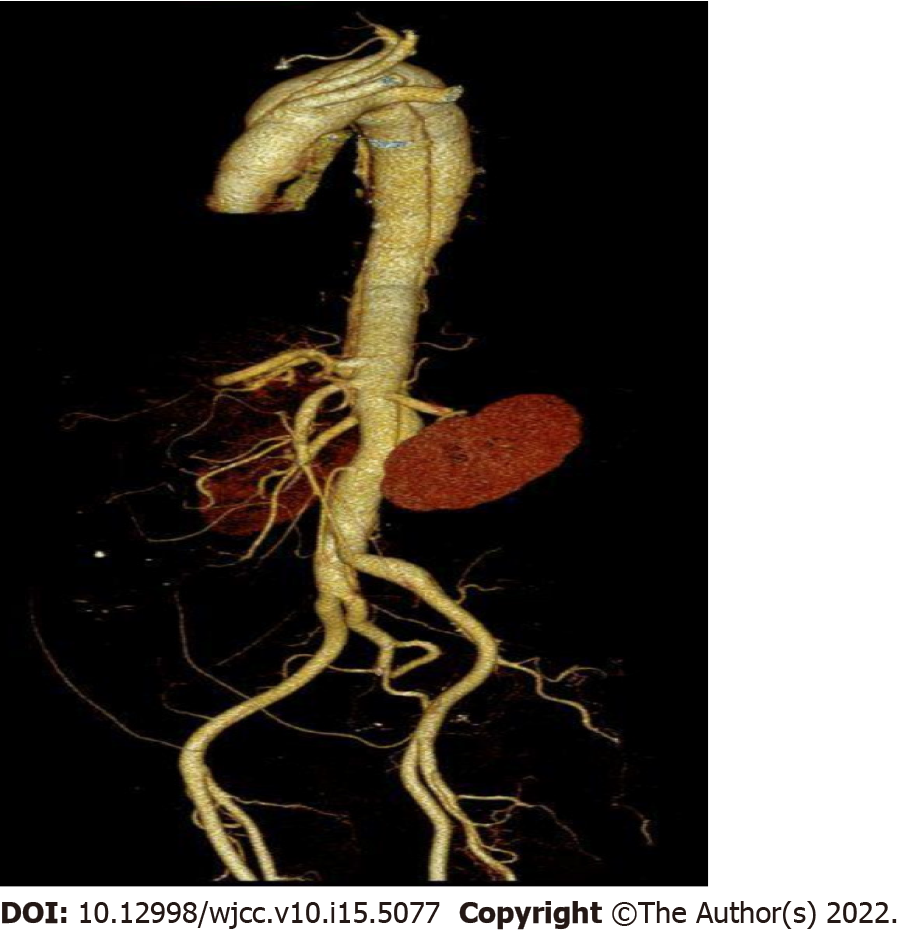
Magnetic resonance imaging (MRI) showed a type A aortic dissection involving the aortic arch and extending to the ascending aorta up to the end of the left common iliac artery with an anomalous right subclavian artery (ARSA) (Figure 1).
The patient underwent orthotopic heart transplantation (Bicaval technique) 28 mo ago for dilated cardiomyopathy with a left ventricular ejection fraction of 23%. Her immunosuppressive protocol including tacrolimus (0.5 mg, qod), mycophenolate mofetil (0.5 g, q12h), and prednisone (20 mg, bid). The donor was a 24-year-old man with no reported medical history.
The patient also had hypertension and diabetes mellitus.
Blood pressure on admission was 147/104 mmHg, and body mass index (BMI) was 30.1 kg/m2.
The value of D-dimer was 0.84 mg/L, and G and GM tests were negative.
On September 3, 2020, MRI showed a type A aortic dissection involving the aortic arch and extending to the ascending aorta up to the end of the left common iliac artery with an ARSA (Figure 1). The echocardiogram showed mild aortic valve insufficiency. The patient was diagnosed with type A aortic dissection.
The patient was diagnosed with type A aortic dissection after heart transplantation.
The patient underwent a hybrid procedure which included ascending aortic and aortic arch replacement, subclavian artery reconstruction, and endovascular repair of abdominal and thoracic aortic aneurysms. A cardiopulmonary bypass was established through the right femoral artery and femoral vein when the core body temperature was lowered to 30-32 ℃. The aberrant right subclavian artery, innominate artery, left common carotid artery, and left subclavian artery were blocked, and the left and right common carotid arteries were cannulated for bilateral cerebral perfusion. The distal port of the No. 24 four-branched artificial vessel was anastomosed with the proximal covered stent of the descending aorta. Cardiopulmonary bypass was resumed, and the body temperature was gradually turned to normal. The proximal port of the four-branched artificial vessel was anastomosed with the proximal autogenous aortic vessels padded with bovine pericardium. The heart restarted spontaneously. The four branches of the aortic arch were reconstructed one by one. A 30 mm × 200 mm aortic-covered stent was implanted through a femoral artery incision (Figure 2).
The procedure lasted 510 min, the cardiopulmonary bypass lasted 133 min, and the ascending aorta was blocked for 10 min. The duration of ventilator assistance was 64.5 h after surgery and the stay time in intensive care units was 8 d for a lung infection and blood pressure control.
On the third day after surgery, the patient was diagnosed with pneumonia and was treated with sulbactam sodium/cefoperazone sodium. During the postoperative period, esmolol hydrochloride and urapidil hydrochloride were used to control blood pressure. Ulinastatin was used to reduce myocardial reperfusion injury. Sulbactam sodium/cefoperazone sodium was used to prevent and control infection. Omeprazole was used to inhibit gastric acid secretion. The patient was discharged home 25 d after surgery without low back pain. One month after discharge, the patient complained of cough and expectoration. Erythrocyte sedimentation rate was 34 mm/h, and C-reactive protein was 35.9 mg/L. The above laboratory tests were normal after anti-infection treatment for 7 d. The patient had no symptoms, cough, or sputum.
Aortic dissection after heart transplantation is very rare and is a serious complication[2]. In this case, the hybrid procedure shortened the operation time and reduced complications. Because the patient had an ARSA, the right axillary artery could not be selected for cardiopulmonary bypass intubation.
Arterial hypertension is one of the most important risk factors for aortic dissection in general and occurs in about 71% of heart transplant patients in the first year after transplantation[3]. Tacrolimus, corticosteroids[4], and post-transplant weight gain are also related to arterial hypertension[5].
The patient had an ARSA, which is encountered in approximately 1% of the population. In this case, the dissection originated from an entry tear in the transverse arch. Of crucial importance, unilateral antegrade cerebral perfusion through the right axillary artery could not be performed.
Type A aortic dissection following heart transplantation is a rare complication that requires emergency surgery. The patient benefited from a hybrid procedure, which shortened the operation time and reduced complications.
| 1. | Writing committee member, Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:e240-e327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1041] [Cited by in RCA: 1589] [Article Influence: 122.2] [Reference Citation Analysis (0)] |
| 2. | Hage A, Hage F, Toeg H, Davies R, Boodhwani M. Aortic dissection following heart transplantation. J Card Surg. 2017;32:156-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Lund LH, Khush KK, Cherikh WS, Goldfarb S, Kucheryavaya AY, Levvey BJ, Meiser B, Rossano JW, Chambers DC, Yusen RD, Stehlik J; International Society for Heart and Lung Transplantation. The Registry of the International Society for Heart and Lung Transplantation: Thirty-fourth Adult Heart Transplantation Report-2017; Focus Theme: Allograft ischemic time. J Heart Lung Transplant. 2017;36:1037-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 493] [Cited by in RCA: 623] [Article Influence: 69.2] [Reference Citation Analysis (1)] |
| 4. | Hošková L, Málek I, Kopkan L, Kautzner J. Pathophysiological mechanisms of calcineurin inhibitor-induced nephrotoxicity and arterial hypertension. Physiol Res. 2017;66:167-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 103] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 5. | Bennett AL, Ventura HO. Hypertension in Patients with Cardiac Transplantation. Med Clin North Am. 2017;101:53-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Cimen SG, Turkey; Jian X, China S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Fan JR