Published online Apr 26, 2022. doi: 10.12998/wjcc.v10.i12.3930
Peer-review started: September 28, 2021
First decision: November 11, 2021
Revised: November 22, 2021
Accepted: March 6, 2022
Article in press: March 6, 2022
Published online: April 26, 2022
Processing time: 204 Days and 19.9 Hours
Both autoimmune pancreatitis (AIP) and gastric varices are related to various diseases. However, AIP complicated by gastric varices is extremely rare, and has only been reported in a few studies. Here, we report a case of AIP complicated by gastric varices in a female Chinese patient.
A 59-year-old Chinese woman was admitted to our hospital with mild abdominal pain. Computed tomography and magnetic resonance cholangiopancreatography revealed a diffusely enlarged pancreas, an obstructed splenic vein and slight splenomegaly. Esophagogastroduodenoscopy showed gastric varices in the partial gastric fundus and the red-color sign was positive. Blood chemistry showed that IgG4 was notablely elevated. The patient was diagnosed with AIP complicated by gastric varices. Steroid therapy was administered to this patient with the risk of gastrointestinal bleeding. After one year of therapy, the pancreas, spleen and splenic vein recovered to the normal states, and the gastric varices had disappeared.
We present this case together with evidence from the literature to demonstrate the effectiveness of steroid therapy in the treatment of AIP complicated by gastric varices.
Core Tip: Autoimmune pancreatitis (AIP) complicated by gastric varices is extremely rare. We report a case of AIP complicated by gastric varices. With one year of steroid therapy, the enlarged pancreas, obstructed splenic vein and slight splenomegaly recovered to the normal states. At the same time, the gastric varices disappeared. After 3 years of follow-up, the patient did not have any of the symptoms as previously described.
- Citation: Hao NB, Li X, Hu WW, Zhang D, Xie J, Wang XL, Li CZ. Steriod for Autoimmune pancreatitis complicating by gastric varices: A case report. World J Clin Cases 2022; 10(12): 3930-3935
- URL: https://www.wjgnet.com/2307-8960/full/v10/i12/3930.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i12.3930
Autoimmune pancreatitis (AIP) is accepted as a unique clinical entity worldwide. The prevalence rate of AIP in Japan was 2.2 per 100000 people[1]. Using this prevalence, it was estimated that the number of AIP patients in China would be approximately 29 thousand[2]. A large multicenter study from 10 different countries reported that therapy with steroid could significantly induce clinical remission in 99% of type 1 AIP and 92% of type 2 AIP patients[3]. However, few studies have reported the role of steroid therapy in AIP complicated by gastric varices. In this study, we summarize the effects of steroid therapy in a case of AIP complicated by gastric varices.
A 59-year-old Chinese woman was admitted to the hospital with the symptoms of mild abdominal discontinuous pain for approximately 4 mo.
The patient suffered from symptoms of mild abdominal discontinuous pain for approximately four months, accompanied by abdominal distension and poor appetite. The patient’s intake was decreased by almost 1/2 compared with normal, and induced a weight loss of 5 kg. In the last month, the symptoms of abdominal pain and distension were worse than before, accompanied by fatigue, but without nausea and vomiting.
No special previous medical history was reported.
No special personal or family histories were found.
Epigastric tenderness without rebound or guarding was found. No other positive signs were found.
Routine blood tests showed a hemoglobin (Hb) of 81 g/L (N:113-151 g/L), red blood cell of 2.88 × 1012/L (N: 3.68-5.13 × 1012/L). Other tests, such as white blood cell, platelet and neutrophil were all normal. Serum protein electrophoresis showed an increased incidence of polyclonal α1-globulinemia of 4.7% (N: 1.1-3.7%), α2-globulinemia of 15.2% (N: 8.5-14.5%) and γ-globulinemia of 26.1% (N: 9.2–18.2%). Other blood chemistry parameters such as tumor markers, liver and kidney function, coagulation tests and amylase levels were all within normal limits. Serology for hepatitis B and C and autoimmune serology, including anti-neutrophil cytoplasmic antibody and antinuclear antibody were all negative. The serum level of IgG4 was detected and was significantly elevated at 3670 mg/L (N: 80-1400 mg/L).
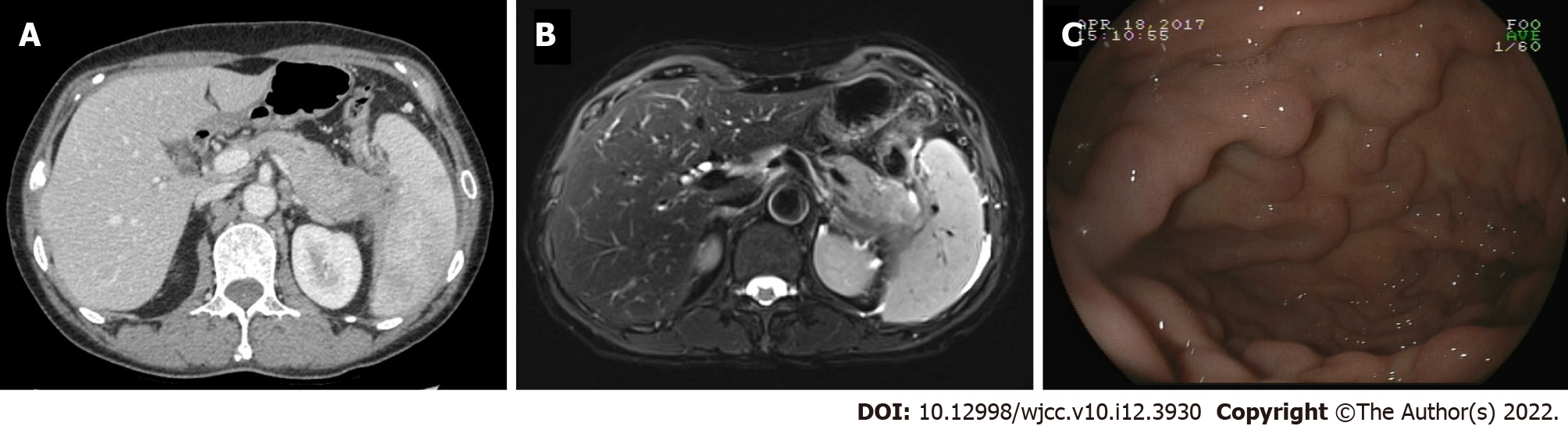
Abdominal computed tomography (CT) revealed a diffusely enlarged pancreas with a capsule-like rim, an obstructed splenic vein, slight splenomegaly and collateral vessels from the gastric fundus (Figure 1A). Magnetic resonance cholangiopancreatography showed the irregular expansion of pancreatic duct in the neck and body of pancreas, and the swelling of pancreas (Figure 1B). Esophagogastroduodenoscopy (EGD) revealed that gastric varices in the partial gastric fundus and the red-color sign were positive (Figure 1C).
Based on these findings, autoimmune pancreatitis complicated by gastric varices was identified.
Oral administration of 24 mg/d methylprednisolone was started for two weeks. Then the treatment was tapered by 4 mg every two weeks and until a maintenance dose of 8 mg/d was reached.
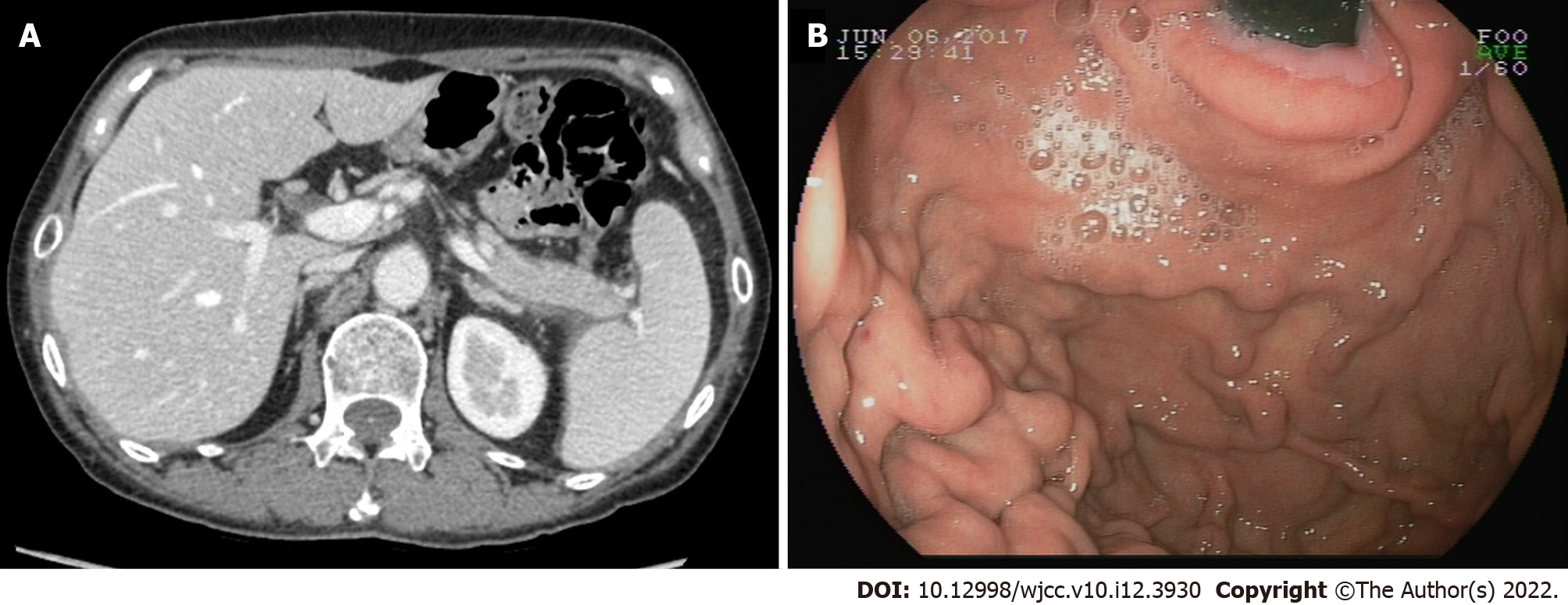
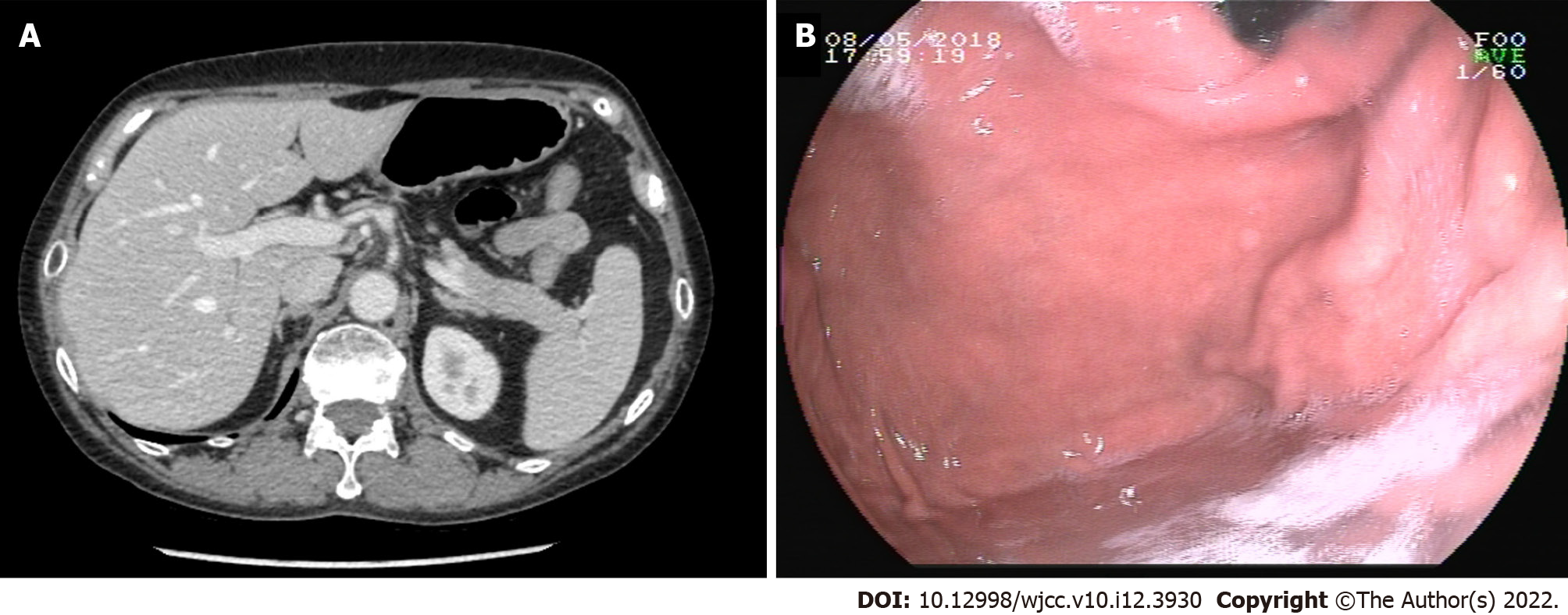
Two months after the initial treatment, an abdominal CT showed that the swelling in the pancreas had improved (Figure 2A). The obstructed splenic vein, splenomegaly and gastric varices with positive red-color signs also showed a slight improvement (Figure 2B). The serum IgG4 had decreased to 1370 mg/L. Five months after the initial treatment, abdominal CT showed that the swelling of the pancreas, the obstructed splenic vein and splenomegaly had further improved (Figure 3A). EGD also showed that the gastric varices had improved, and the red-color signs were negative (Figure 3B). The serum IgG4 decreased to a normal level at 677mg/L. One year after the initial therapy, an abdominal CT showed that the pancreas, splenic vein and spleen were restored to the normal level (Figure 4A). EGD showed that the gastric vertices had disappeared (Figure 4B). The serum IgG4 had decreased to its normal level of 566 mg/L. Finally, the patient was asked to stop steroid therapy. After three years of follow-up, the patient did not experience a recurrent abdominal pain, and she did not have melena.
Type 1 AIP is considered a pancreatic manifestation of IgG4 related disease, which also includes a few extra-pancreatic organ diseases such as salivary sclerosingsialadenitis, interstitial nephritis, sclerosing cholangitis lung nodules, mediastinal fibrosis, adenopathy and chronic periaortitis[5,6]. The classical histopathological findings are dense lymphoplasmacytic infiltration, IgG4-positive plasma cell infiltration, storiform fibrosis, obliterative phlebitis and fibrosis without granulocytic infiltration[7]. A large multicenter study found that Type 1 AIP often presents at an older age and is more likely than type 2 AIP to manifest in men[3]. A systematic review in China found that the male to female ratio of type 1 AIP was 4.5:1. The main symptoms in type 1 AIP patients are jaundice (75%), abdominal pain (65%), and weight loss (42%)[2]. In this case report, the patient was a woman, and the main clinical presentation was up abdominal pain and weight loss.
Gastric varices are a relatively common complication in chronic pancreatitis[8]. Chronic pancreatitis leads to splenic vein obstruction and induces sinistral portal hypertension. Finally, gastric varices are formed along the fundus and the greater curvature of the stomach, since the blood flow in the short gastric veins or the gastroepiploic vein is significantly increased. However, AIP complicated by gastric varices has rarely been reported. Ishikawa et al[9] retrospectively reviewed 54 patients who met the international disease diagnostic criteria for AIP and found that 24 of the patients had AIP complicated by peripancreatic vascular involvement. Among these, only one patient (1/54, 1.9%) had gastric varices, 22 patients (22/54, 40.7%) had splenic vein occlusion or stenosis, and 13 patients (13/54, 24.1%) had superior mesenteric-portal vein occlusion or stenosis. In this case, the patient was diagnosed with AIP complicated by splenic vein obstruction and gastric varices.
Steroids are considered a risk factor for gastrointestinal bleeding. More studies are needed to evaluate the merits and disadvantages of using steroid therapy for AIP complicated by peripancreatic vascular involvement, especially gastric varices[10]. Ishikawa and colleagues reported that vascular lesions were significantly improved in 14 of 16 patients who received steroid therapy for AIP complicated by peripancreatic vascular involvement[9]. In contrast, the vascular lesions were exacerbated in 2 of 4 patients who were not treated with steroid therapy after two years. These results indicated that steroid therapy was meaningful. Furthermore, Goto and colleagues reported 3 cases of AIP complicated by gastric varices[11]. In case 1 without splenomegaly, steroid therapy significantly improved the enlarged pancreas and the splenic vein was reperfused. Finally, the gastric varices disappeared after six months of therapy. However, in cases 2 and 3 with splenomegaly, steroid therapy was not very effective. One case showed that steroid therapy only improved AIP but had no influence on gastric varices. In another case, it was found that steroid therapy had no role in either AIP or gastric varices after five months of therapy. These cases revealed that the reason for these patients’ congestive splenomegaly might have been the long duration for which they were affected by sinistral portal hypertension, and the splenomegaly finally led to irreversible spleen vein obstruction[11,12]. In this case, at the time of diagnosis, the patient had a diffusely enlarged pancreas with a capsule-like rim, an obstructed splenic vein, slight splenomegaly and gastric varices. After 1 year of steroid therapy, the capsule-like rim and gastric varices had disappeared, the spleen vein was reperfused, and the spleen was reduced.
In summary, we reported a case of AIP complicated by gastric varices in this study. After 1 year of steroid therapy, the patient did not have any symptoms. The pancreas was significantly improved, and the gastric varices disappeared.
| 1. | Kanno A, Nishimori I, Masamune A, Kikuta K, Hirota M, Kuriyama S, Tsuji I, Shimosegawa T; Research Committee on Intractable Diseases of Pancreas. Nationwide epidemiological survey of autoimmune pancreatitis in Japan. Pancreas. 2012;41:835-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 108] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 2. | Meng Q, Xin L, Liu W, Lin H, Tian B, Wang L, Li Z. Diagnosis and Treatment of Autoimmune Pancreatitis in China: A Systematic Review. PLoS One. 2015;10:e0130466. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Hart PA, Kamisawa T, Brugge WR, Chung JB, Culver EL, Czakó L, Frulloni L, Go VL, Gress TM, Kim MH, Kawa S, Lee KT, Lerch MM, Liao WC, Löhr M, Okazaki K, Ryu JK, Schleinitz N, Shimizu K, Shimosegawa T, Soetikno R, Webster G, Yadav D, Zen Y, Chari ST. Long-term outcomes of autoimmune pancreatitis: a multicentre, international analysis. Gut. 2013;62:1771-1776. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 461] [Cited by in RCA: 386] [Article Influence: 29.7] [Reference Citation Analysis (0)] |
| 4. | Shimosegawa T, Chari ST, Frulloni L, Kamisawa T, Kawa S, Mino-Kenudson M, Kim MH, Klöppel G, Lerch MM, Löhr M, Notohara K, Okazaki K, Schneider A, Zhang L; International Association of Pancreatology. International consensus diagnostic criteria for autoimmune pancreatitis: guidelines of the International Association of Pancreatology. Pancreas. 2011;40:352-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1050] [Cited by in RCA: 1083] [Article Influence: 72.2] [Reference Citation Analysis (0)] |
| 5. | Omiyale AO. Autoimmune pancreatitis. Gland Surg. 2016;5:318-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Sureka B, Rastogi A. Autoimmune Pancreatitis. Pol J Radiol. 2017;82:233-239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Shiokawa M, Kodama Y, Kuriyama K, Yoshimura K, Tomono T, Morita T, Kakiuchi N, Matsumori T, Mima A, Nishikawa Y, Ueda T, Tsuda M, Yamauchi Y, Minami R, Sakuma Y, Ota Y, Maruno T, Kurita A, Sawai Y, Tsuji Y, Uza N, Matsumura K, Watanabe T, Notohara K, Tsuruyama T, Seno H, Chiba T. Pathogenicity of IgG in patients with IgG4-related disease. Gut. 2016;65:1322-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 147] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 8. | Ramesh H, Jacob G, Venugopal A, Lekha V, Jacob M. Surgical management of chronic pancreatitis with portal hypertension--a 19-year experience. Surgery. 2008;143:252-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Ishikawa T, Itoh A, Kawashima H, Ohno E, Itoh Y, Nakamura Y, Hiramatsu T, Miyahara R, Ohmiya N, Haruta J, Goto H, Hirooka Y. Peripancreatic vascular involvements of autoimmune pancreatitis. J Gastroenterol Hepatol. 2012;27:1790-1795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Kamisawa T, Yoshiike M, Egawa N, Nakajima H, Tsuruta K, Okamoto A: Treating patients with autoimmune pancreatitis: Results from a long-term follow-up study. Pancreatology : official journal of the International Association of Pancreatology 2005; 5: 234-238; discussion 238-240. [RCA] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 103] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 11. | Goto N, Mimura J, Itani T, Hayashi M, Shimada Y, Matsumori T. Autoimmune pancreatitis complicated by gastric varices: a report of 3 cases. World J Gastroenterol. 2012;18:4228-4232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (1)] |
| 12. | Sakorafas GH, Tsiotou AG. Splenic-vein thrombosis complicating chronic pancreatitis. Scand J Gastroenterol. 1999;34:1171-1177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Omiyale AO, United Kingdom; Pelaez-Luna M, Mexico; Poturoglu S, Turkey S-Editor: Xing YX L-Editor: A P-Editor: Xing YX