Published online Apr 26, 2022. doi: 10.12998/wjcc.v10.i12.3907
Peer-review started: September 8, 2021
First decision: November 19, 2021
Revised: November 23, 2021
Accepted: March 7, 2022
Article in press: March 7, 2022
Published online: April 26, 2022
Processing time: 225 Days and 1.9 Hours
In atrophic posterior mandibular areas, where the bone height superior to the inferior alveolar nerve (IAN) is less than 6 mm, short implants are not applicable. Conventional alternatives such as IAN transposition and various alveolar bone augmentation approaches are technically demanding and prone to complications.
Computer-guided dynamic navigation implantation improves the accuracy, predictability, and safety of implant placement. This case report presents a dynamic navigation system-guided trans-IAN implant placement technique, which can successfully treat a posterior mandibular dentition defect when the bone height is only 4.5 mm. The implant was inserted into the buccal side of the IAN and was 1.7 mm away from the IAN. The implantation deviations were controlled within a satisfying range, and the long-term restoration outcome was stable.
Dynamic navigation system-guided trans-IAN implant placement might be a recommended technique for patients with extremely insufficient residual bone height and sufficient bone width in the posterior mandibular area.
Core Tip: In atrophic posterior mandibular areas, where the residual bone height (RBH) superior to the inferior alveolar nerve (IAN) is less than 6 mm, conventional operative treatments are no longer applicable. We present a computer-dynamic navigation system (CADNS) -guided trans-IAN implant placement technique, which successfully treat a posterior mandibular dentition defect when the bone height is only 4.5 mm, resulting with a satisfying implant-restoration. This case demonstrates a novel implantation solution taking advantage of the accuracy and safety of CADNS. CADNS-guided trans-IAN placement could be a recommended technique for patients with an extremely insufficient RBH but sufficient buccal bone width in the posterior mandibular area.
- Citation: Chen LW, Zhao XE, Yan Q, Xia HB, Sun Q. Dynamic navigation system-guided trans-inferior alveolar nerve implant placement in the atrophic posterior mandible: A case report. World J Clin Cases 2022; 10(12): 3907-3915
- URL: https://www.wjgnet.com/2307-8960/full/v10/i12/3907.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i12.3907
Adequate bone height and bone width are essential for dental implant placement. In the posterior mandible, alveolar bone volume could be resorbed too severely to accommodate a dental implant due to persistent periodontal disease, early loss of teeth, or prolonged use of removable prostheses[1]. Short dental implants are recommended when the residual bone height (RBH) is more than 6 mm[2,3]. Vertical bone augmentation approaches [like onlay bone graft, guided bone regeneration, and distraction osteogenesis][1,4] and inferior alveolar nerve (IAN) reposition[5] are recommended when the RBH is less than 6 mm. However, these approaches are technically challenging and accompanied by complications, such as soft tissue dehiscence, barrier membrane exposure[6], infection, displacement of the transport segment[7], and neurosensory abnormalities[5]. Therefore, a minimally invasive, less risky, and more accurate technique is needed for severe atrophic posterior mandible edentulous patients.
Computer-assisted dynamic navigation systems (CADNSs) based on cone-beam computed topography (CBCT) navigation have been introduced into the field of dental implantology to improve the accuracy of implant placement and avoid potential complications[8,9]. A CADNS is a surgical navigation system which can design the location of a virtual implant according to CBCT data. In addition, it allows real-time tracking of implant drills in three dimensions (3D) on a monitor[10]. It is significantly predictable, accurate, and less risky than freehand implant surgeries[11]. Therefore, it is suitable for guiding implant insertion surgery in edentulous patients with critical alveolar bone volumes. This article reports a case using CADNS in the posterior mandible with severe bone resorption to avoid IAN injury. This article follows the recommendations of the CARE guidelines[12].
A 50-year-old woman was referred to our clinic with the chief complaint of loss of posterior mandibular teeth over 5 years. Oral examination showed that teeth 36 and 37 were missing (Figure 1A). Tooth 38 had erupted and was occluded with the upper teeth. The distance between the gingiva and maxillary teeth at the edentulous area was 6-7 mm, while the mesiodistal distance was about 18 mm (Figure 1B).
The patient reported no systemic diseases.
The patient had a free previous medical history.
The patient reported no drug allergy, long-term medication family genetic disease, or smoking.
The patient’s temperature was 36.5 °C, heart rate was 84, blood pressure was 87/61 mmHg, without any other pathological signs.
The blood biochemistry analyses were normal.
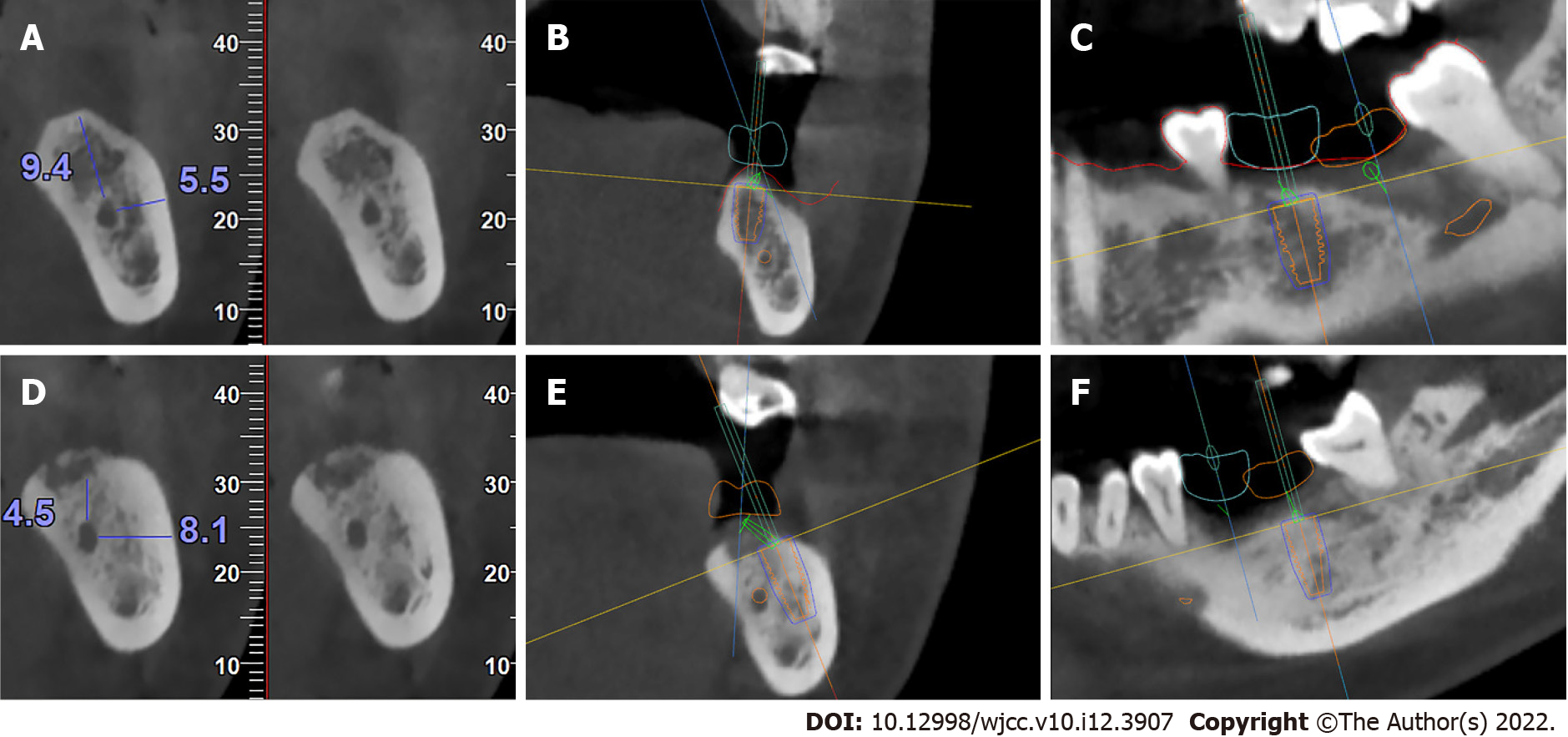
CBCT images showed that the distance from the IAN to the crestal ridge was 9.4 mm, and the distance from the IAN to the buccal cortical bone wall was 5.5 mm at tooth 36 (Figure 2A). The volumes of tooth 37 were 4.5 mm and 8.1 mm, respectively (Figure 2D).
The final diagnosis of the presented case was Kenney III dentition defect.
The vertical bone heights above the IAN at teeth 37 was insufficient for standard-length implant placement. The following treatment options were considered: (1) Short implants, although the shortest implant available was 6 mm, which was not applicable for tooth 37; (2) onlay bone augmentation, although excessive compression would encroach on prosthesis space, and vertical bone augmentation in the posterior area is challenging; (3) IAN reposition, although this approach can lead to neurosensory disturbances and spontaneous mandibular fractures[5]; (4) trans-IAN implant placement guided by a 3D-printed surgical guide, although the upper surface of the 3D guide needs to be 5 mm away from the alveolar ridge, and the full length of the implant drill is 18-22 mm (since the defect site was rather posterior, the surgery would require the patient’s mouth to remain wide open for a long time, which can be challenging for patients); or (5) trans-IAN implant placement guided by a CADNS for tooth 37.
Based on these factors, a trans-IAN implant placement guided by a CADNS was used. Informed consent of the patient was obtained before the surgery.
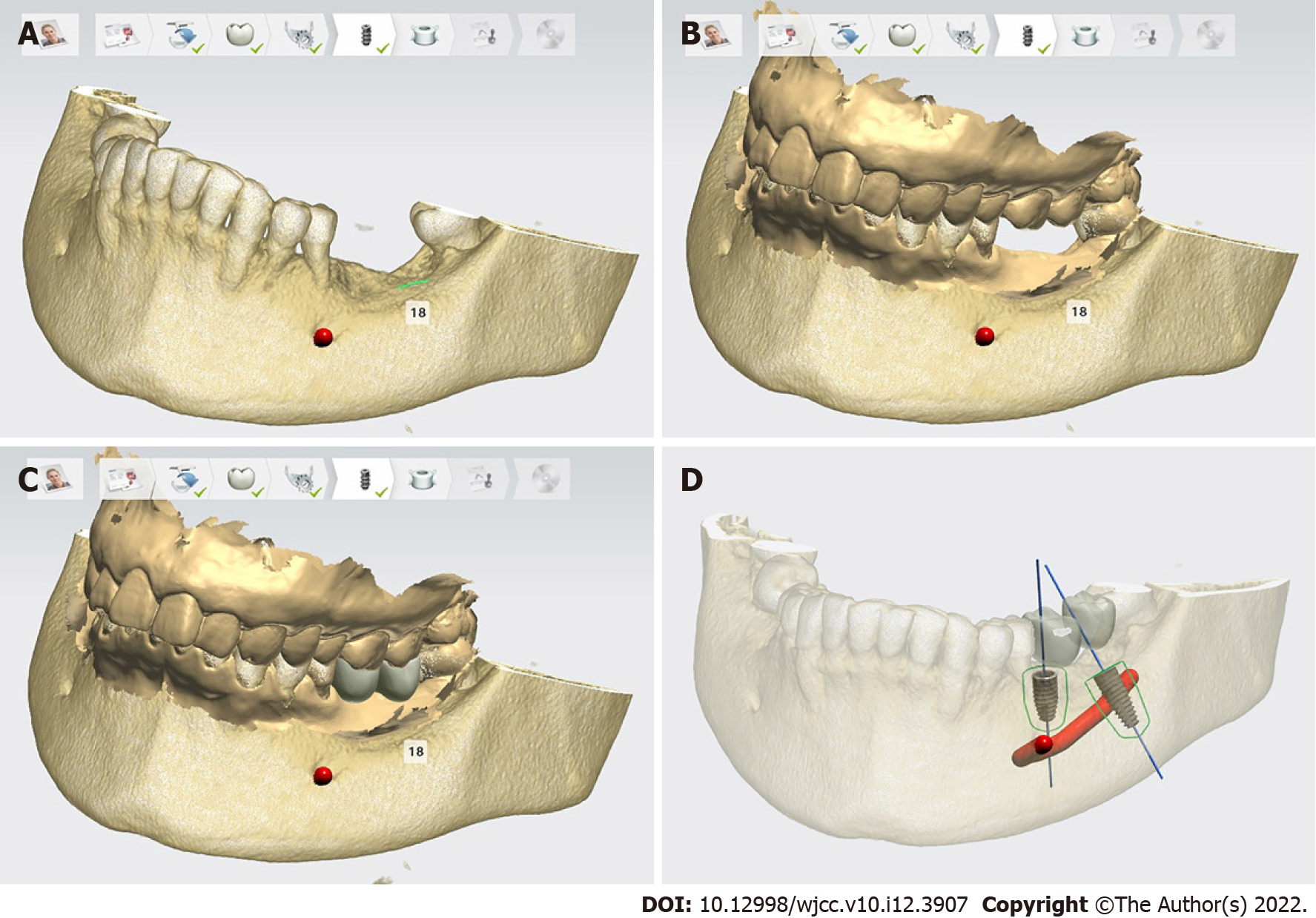
A U-shaped fixture was fixed at the edentulous region after filling with polyether impression material (Figure 1C). Subsequently, both jaws and the U-shaped tube were scanned using CBCT (Figure 1D). The volumetric data was converted into Digital Imaging and Communications in Medicine (DICOM) format. Surface images of dentition and occlusion were obtained by an intraoral optical scanner and were converted to standard tessellation language (STL) format. Both the DICOM and STL files were uploaded into the treatment planning software. The software superimposed the 3D files, and displayed the jaw, dentition (Figure 3A), soft tissue, the alveolar nerve, and occlusion (Figure 3B) in a common coordinate system as a merged file.
Prosthodontic treatment planning included evaluating the occlusion, placing the prosthesis (Figure 3C), choosing the implants below the crowns (Figure 3D), and arranging proper position, length, diameter, and abutment for each implant. Because of the insufficient bone height above the IAN, a 4.1 mm × 8 mm implant (ITI, BLT) and a straight abutment were planned for tooth 36 (Figure 2B and C). In addition, a 4.1 mm × 10 mm trans-IAN implant (ITI, BLT) on the buccal side and an angled abutment were planned for tooth 37 (Figure 2E and F). Screw-retained united crowns were designed. Then, the treatment plan was imported into the dynamic navigation software.
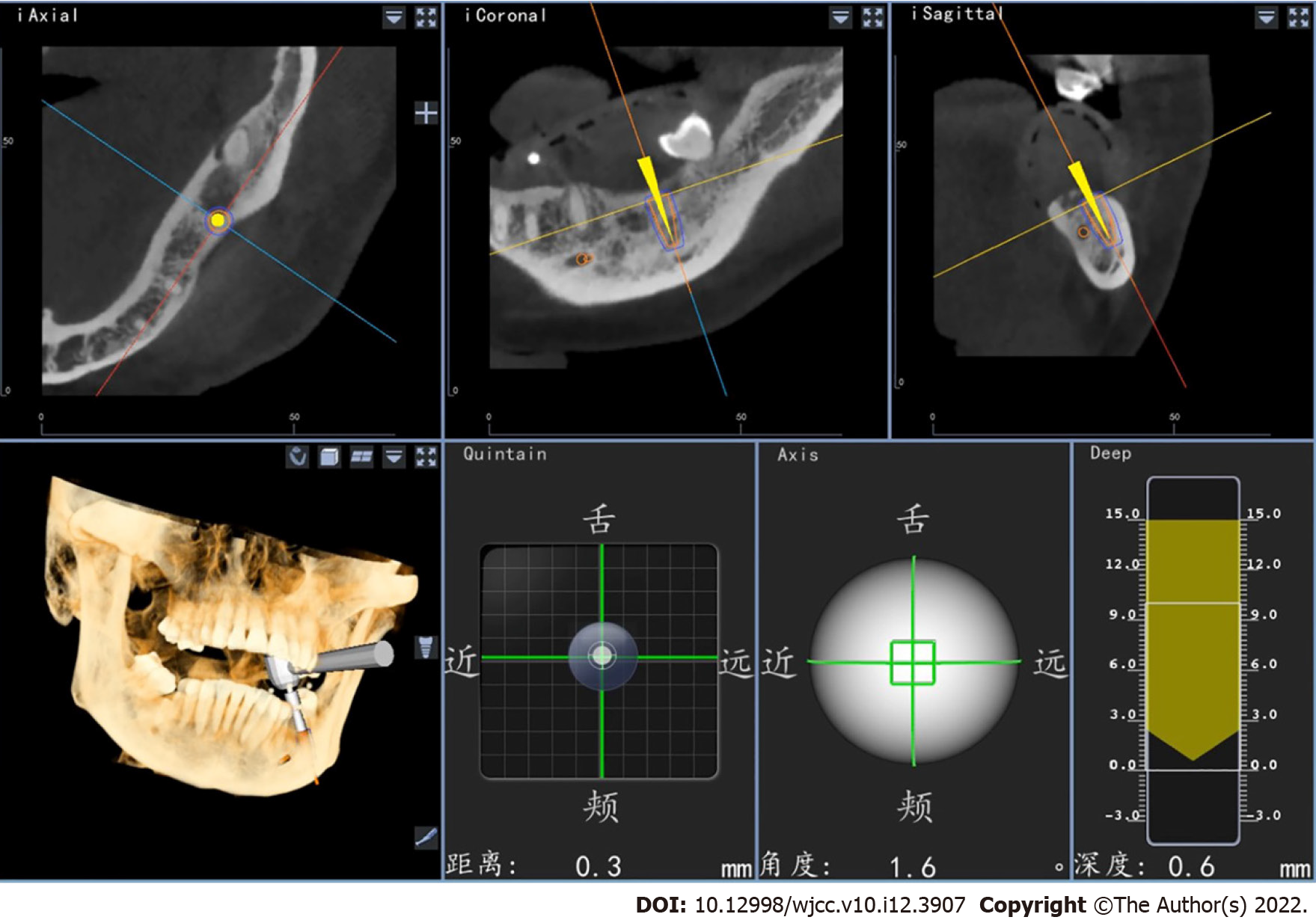
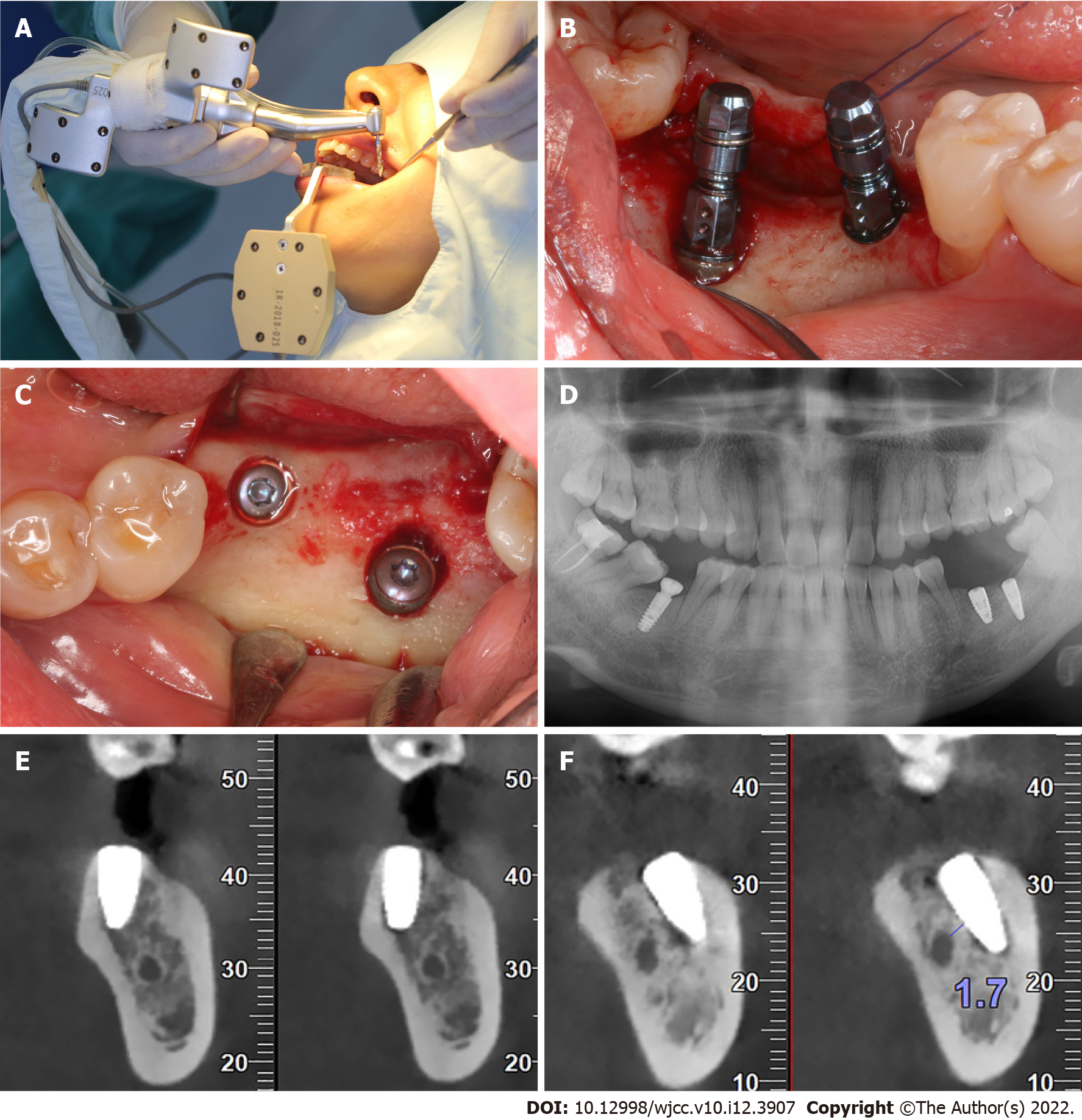
Routine operation disinfection and local infiltration anesthesia were performed. The Digital-care Implant Surgery Navigation System (Dcarer, Suzhou, China) was used to assist the surgery. The instruments were calibrated for tracking by the dynamic system. A reference plate was firmly fixed on the mandibular anterior teeth using self-curing resin. Next, the geometry of the patient-tracking array relative to the reference plate was also registered into the dynamic system. Afterwards, implant placement was conducted according to the preoperative planning (Figure 4) with the guide of a real-time navigation operation view on the monitor (Figure 5A-C). The reference plate was removed after implants insertion. Cover screws were connected, and the wound was sutured.
Postoperative CBCT (Figure 5D-F) showed that safe distances were ensured between implants and the IAN. The implant at tooth 37 was placed through the buccal side of the IAN, and the distance from the IAN to the implant was 1.7 mm (Figure 5F). The preoperative planning and postoperative CBCT images were imported into the navigation software and matched to calculate the deviation. The deviations at teeth 36 and 37 were 0.831 mm and 0.682 mm at the implant shoulders and 0.574 mm and 0.867 mm at the implant tips, respectively. The angular deviations at teeth 36 and 37 were 3.118° and 2.317°, respectively.
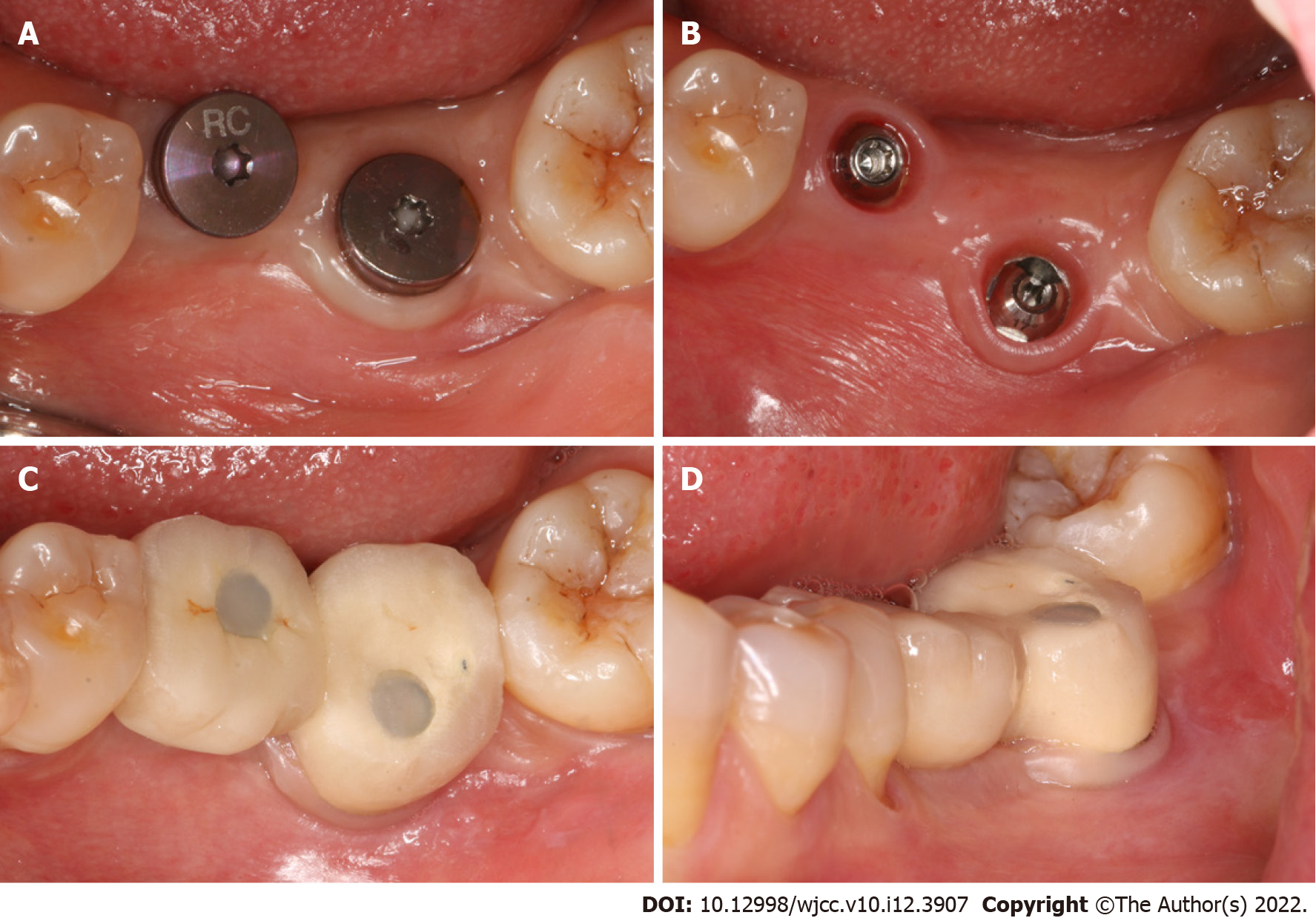
After 4 mo, second-stage surgery was performed (Figure 6A). A 1.5-mm straight composite abutment was placed at the first molar site, and a 2.5-mm 17°-angled composite abutment was placed at the second molar site (Figure 6B). Restoration was finished with the screw-retained porcelain-fused-metal union crowns (Figures 6C and D).
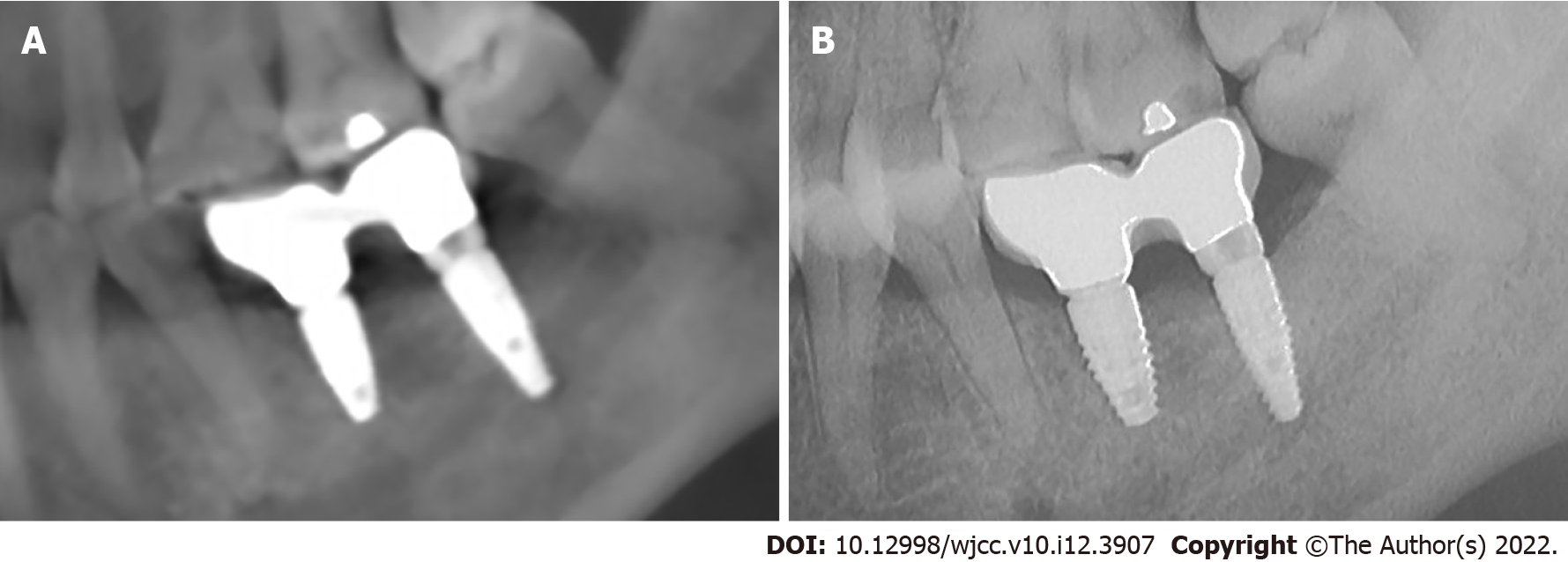
Clinical and CBCT examination after restoration (Figure 7A) showed that the marginal bone was fine, the soft tissues around the implants were healthy, and the adjacency and occlusion were appropriate. CBCT examination at the 6-month follow-up (Figure 7B) revealed that the marginal bone was stable and that the implants’ osseointegration was healthy, which fulfilled the success criteria stated by Papaspyridakos et al[13].
It is challenging to restore a severely atrophic posterior mandible with dental implants. Short implants and vertical bone augmentation are recommended as the priority options in these cases[14]. IAN reposition is also an alternative option when the RBH is less than 6 mm. However, many complications are associated with these treatment options. In this case, the RBH at tooth 37 was 4.5 mm, while there was sufficient bone volume from the IAN to the buccal cortical bone (8.1 mm). Therefore, a tilted implant was inserted into the buccal side of the IAN with guided dynamic navigation. This technique is recommended for patients with sufficient residual alveolar bone width.
In the past decade, computer-guided implantology techniques have been used widely and play important roles in edentulous patients with severe bone resorption with a favorable accuracy and success rate. Computer-guided implantology technologies include static and dynamic navigation. Both can achieve a satisfactory accuracy in implant surgeries. Block et al[15] reported similar accuracies between dynamic and static navigation. Mediavilla Guzmán et al[16] reported no significant difference between dynamic and static navigation at the coronal and apical levels, but a significantly smaller angular deviation was observed in the dynamic system. In the present case, the deviations at the implant shoulder of teeth 36 and 37 were 0.831 mm and 0.682 mm, respectively; 0.574 mm and 0.867 mm at the implant apical level, respectively; and angular deviations of 3.118° and 2.317°, respectively. The results were consistent with preliminary studies on the accuracy of dynamic navigation surgeries[8,15,17].
Compared to static navigation, dynamic navigation has many advantages. First, 3D-printed surgical guide plates are not needed, thus reducing expenses and surgical time[18]. Second, no special drills are required. Third, it has a lower requirement regarding an open bite. Fourth, the risk of overheating is decreased due to sufficient irrigation. Finally, it allows for real-time feedback on the preparation and insertion on the implant in 3D[10].
Although a CADNS offers significant advantages, there are some disadvantages. One limitation is the huge initial investment in equipment (CBCT equipment, intraoral scan equipment, and dynamic navigation equipment) and training. Learning to use new software and adapting to virtual image-guided operation may also require effort. Many researchers believe that there is a learning curve to achieve proficiency in this technique. A study showed that dentists become statistically equivalent and proficient after 20 implant placements[15]. As for this case, there is a disadvantage of the CADNS-guided trans-IAN technique that it is not always possible to place an implant that provide an ideal prosthetic position.
CADNS can ensure the accuracy and safety of implant placement and avoid the risk of damaging the IAN. Therefore, CADNS-guided trans-IAN placement could be a recommended technique for patients with an extremely insufficient RBH but sufficient buccal bone width in the posterior mandibular area.
| 1. | Esposito M, Grusovin MG, Felice P, Karatzopoulos G, Worthington HV, Coulthard P. Interventions for replacing missing teeth: horizontal and vertical bone augmentation techniques for dental implant treatment. Cochrane Database Syst Rev. 2009;CD003607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 97] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 2. | Jung RE, Al-Nawas B, Araujo M, Avila-Ortiz G, Barter S, Brodala N, Chappuis V, Chen B, De Souza A, Almeida RF, Fickl S, Finelle G, Ganeles J, Gholami H, Hammerle C, Jensen S, Jokstad A, Katsuyama H, Kleinheinz J, Kunavisarut C, Mardas N, Monje A, Papaspyridakos P, Payer M, Schiegnitz E, Smeets R, Stefanini M, Ten Bruggenkate C, Vazouras K, Weber HP, Weingart D, Windisch P. Group 1 ITI Consensus Report: The influence of implant length and design and medications on clinical and patient-reported outcomes. Clin Oral Implants Res. 2018;29 Suppl 16:69-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 138] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 3. | Markose J, Eshwar S, Srinivas S, Jain V. Clinical outcomes of ultrashort sloping shoulder implant design: A survival analysis. Clin Implant Dent Relat Res. 2018;20:646-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Felice P, Barausse C, Barone A, Zucchelli G, Piattelli M, Pistilli R, Ippolito DR, Simion M. Interpositional Augmentation Technique in the Treatment of Posterior Mandibular Atrophies: A Retrospective Study Comparing 129 Autogenous and Heterologous Bone Blocks with 2 to 7 Years Follow-Up. Int J Periodontics Restorative Dent. 2017;37:469-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 5. | Vetromilla BM, Moura LB, Sonego CL, Torriani MA, Chagas OL Jr. Complications associated with inferior alveolar nerve repositioning for dental implant placement: a systematic review. Int J Oral Maxillofac Surg. 2014;43:1360-1366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Todisco M. Early loading of implants in vertically augmented bone with non-resorbable membranes and deproteinised anorganic bovine bone. An uncontrolled prospective cohort study. Eur J Oral Implantol. 2010;3:47-58. [PubMed] |
| 7. | Zhao K, Wang F, Huang W, Wu Y. Clinical Outcomes of Vertical Distraction Osteogenesis for Dental Implantation: A Systematic Review and Meta-Analysis. Int J Oral Maxillofac Implants. 2018;33:549-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Edelmann C, Wetzel M, Knipper A, Luthardt RG, Schnutenhaus S. Accuracy of Computer-Assisted Dynamic Navigation in Implant Placement with a Fully Digital Approach: A Prospective Clinical Trial. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 9. | Wei SM, Zhu Y, Wei JX, Zhang CN, Shi JY, Lai HC. Accuracy of dynamic navigation in implant surgery: A systematic review and meta-analysis. Clin Oral Implants Res. 2021;32:383-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 111] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 10. | Cecchetti F, Di Girolamo M, Ippolito DG, Baggi L. Computer-guided implant surgery: analysis of dynamic navigation systems and digital accuracy. J Biol Regul Homeost Agents. 2020;34:9-17. DENTAL SUPPLEMENT. [PubMed] |
| 11. | O'Meara S. Commentary on Vermeulen H, Ubbink DT, Schreuder SM and Lubbers MJ (2007) Inter- and intra-observer (dis)agreement among nurses and doctors to classify colour and exudation of open surgical wounds according to the Red-Yellow-Black scheme. Journal of Clinical Nursing16, 1270-1277 and Sugama J, Matsui Y, Sanada H, Konya C, Okuwa M and Kitagawa A (2007) A study of the efficiency and convenience of an advanced portable wound measurement system (VISITRAK). Journal of Clinical Nursing 16, 1265-1269. J Clin Nurs. 2008;17:1677-1679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D; CARE Group. The CARE guidelines: consensus-based clinical case report guideline development. J Diet Suppl. 2013;10:381-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 61] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 13. | Papaspyridakos P, Chen CJ, Singh M, Weber HP, Gallucci GO. Success criteria in implant dentistry: a systematic review. J Dent Res. 2012;91:242-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 483] [Cited by in RCA: 427] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 14. | Merli M, Moscatelli M, Pagliaro U, Mariotti G, Merli I, Nieri M. Implant prosthetic rehabilitation in partially edentulous patients with bone atrophy. An umbrella review based on systematic reviews of randomised controlled trials. Eur J Oral Implantol. 2018;11:261-280. [PubMed] |
| 15. | Block MS, Emery RW, Lank K, Ryan J. Implant Placement Accuracy Using Dynamic Navigation. Int J Oral Maxillofac Implants. 2017;32:92-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 105] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 16. | Mediavilla Guzmán A, Riad Deglow E, Zubizarreta-Macho Á, Agustín-Panadero R, Hernández Montero S. Accuracy of Computer-Aided Dynamic Navigation Compared to Computer-Aided Static Navigation for Dental Implant Placement: An In Vitro Study. J Clin Med. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 69] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 17. | Block MS, Emery RW, Cullum DR, Sheikh A. Implant Placement Is More Accurate Using Dynamic Navigation. J Oral Maxillofac Surg. 2017;75:1377-1386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 150] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 18. | Van Assche N, Vercruyssen M, Coucke W, Teughels W, Jacobs R, Quirynen M. Accuracy of computer-aided implant placement. Clin Oral Implants Res. 2012;23 Suppl 6:112-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 204] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chrcanovic BR, Sweden; Ghimire R, Nepal S-Editor: Wang JL L-Editor: A P-Editor: Wang JL