Published online Apr 26, 2022. doi: 10.12998/wjcc.v10.i12.3893
Peer-review started: September 1, 2021
First decision: November 22, 2021
Revised: November 30, 2021
Accepted: March 7, 2022
Article in press: March 7, 2022
Published online: April 26, 2022
Processing time: 232 Days and 1.1 Hours
Pulmonary cryptococcosis (PC) is an opportunistic infectious disease of the respiratory system. Lung tissue biopsies, culture of respiratory samples (e.g., sputum, lung tissue, pleural fluid, and bronchoalveolar lavage fluid), and cryptococcal antigen (CrAg) testing are helpful for a definitive diagnosis. However, these tests are sometimes falsely negative. PC is often misdiagnosed or underdiagnosed owing to the absence of obvert symptoms, poor imaging specificity, and false-negative laboratory tests.
We report two female patients who underwent computed tomography-guided percutaneous needle pulmonary biopsy of a lung nodule for a confirmed diagnosis. In both patients, the CrAg test on the lung biopsy tissue homogenate was positive, while the serum CrAg test was negative. Combined with the lung tissue pathology, we made the diagnosis of PC. Antifungal therapy was effective in both patients.
Given the findings of our cases and the literature review, lung tissue homogenate CrAg testing can be helpful in improving the diagnosis of PC.
Core Tip: Pulmonary cryptococcosis (PC) is often misdiagnosed or underdiagnosed owing to the absence of obvert symptoms, poor imaging specificity, and false-negative laboratory tests. We presented two cases of PC wherein serum cryptococcal antigen (CrAg) tests were negative; however, CrAg tests using lung tissue homogenate were positive. Our report aims to highlight the dilemma in diagnosing PC, as well as a novel adjunct in the diagnostic work-up for PC–cryptococcal antigen tests on lung tissue homogenates.
- Citation: Wang WY, Zheng YL, Jiang LB. Cryptococcal antigen testing of lung tissue homogenate improves pulmonary cryptococcosis diagnosis: Two case reports. World J Clin Cases 2022; 10(12): 3893-3898
- URL: https://www.wjgnet.com/2307-8960/full/v10/i12/3893.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i12.3893
Cryptococcus neoformans, the aetiological cause of pulmonary cryptococcosis (PC), is globally prevalent and can cause a fatal, disseminated disease. As a potentially serious fungal infection, a timely and reliable diagnosis is very important for improving the prognosis of PC. The diagnosis of PC is based on a combination of clinical symptoms, radiological suspicion, and laboratory confirmation[1]. Culture, histopathology, and serology are the main laboratory methods used for confirmation[2]. However, PC may easily be misdiagnosed or underdiagnosed owing to the absence of clinical symptoms and false-negative laboratory results[2-6]. Cryptococcal antigen (CrAg) testing is convenient, inexpensive, and effective in diagnosing PC[5,7]. Serum, bronchoalveolar lavage fluid (BAFL), pleural effusion, percutaneous pulmonary aspirates, urine and cerebrospinal fluid have been used for CrAg testing[7-10], while lung tissue homogenate has not been reported thus far. The following cases highlight the usefulness and sensitivity of CrAg testing of lung tissue homogenate in the confirmation of PC.
Case 1: A 59-year-old female patient was admitted to the hospital for haemoptysis on August 21, 2017.
Case 2: A 57-year-old female patient complained of worsening cough for 4 mo and was admitted to the hospital on July 20, 2020.
Case 1: The patient complained of haemoptysis with no sputum. Chest computed tomography (CT) before admission revealed nodules in both lungs, and 7 d of antibacterial treatment was ineffective.
Case 2: The patient had a repeating cough with no fever or sputum.
Case 1: The patient had a 20-year history of immune thrombocytopenic purpura, 2-year history of secondary diabetes, and 1-month history of splenectomy. She had long-term steroid therapy indicated for systemic blood disease.
Case 2: The patient had no other medical history.
Both patients had no remarkable personal or family history.
Case 1: Initial medical examination showed a respiratory rate (RR) of 17 breaths/min, heart rate (HR) of 85 beats/min, temperature of 37.2 °C, and blood pressure (BP) of 102/65 mmHg. No rales were detected in either lung.
Case 2: Physical examination showed an RR of 18 breaths/min, HR of 89 beats/min, temperature of 37.2 °C and BP of 139/79 mmHg. Normal sounds were heard on auscultation of the lungs.
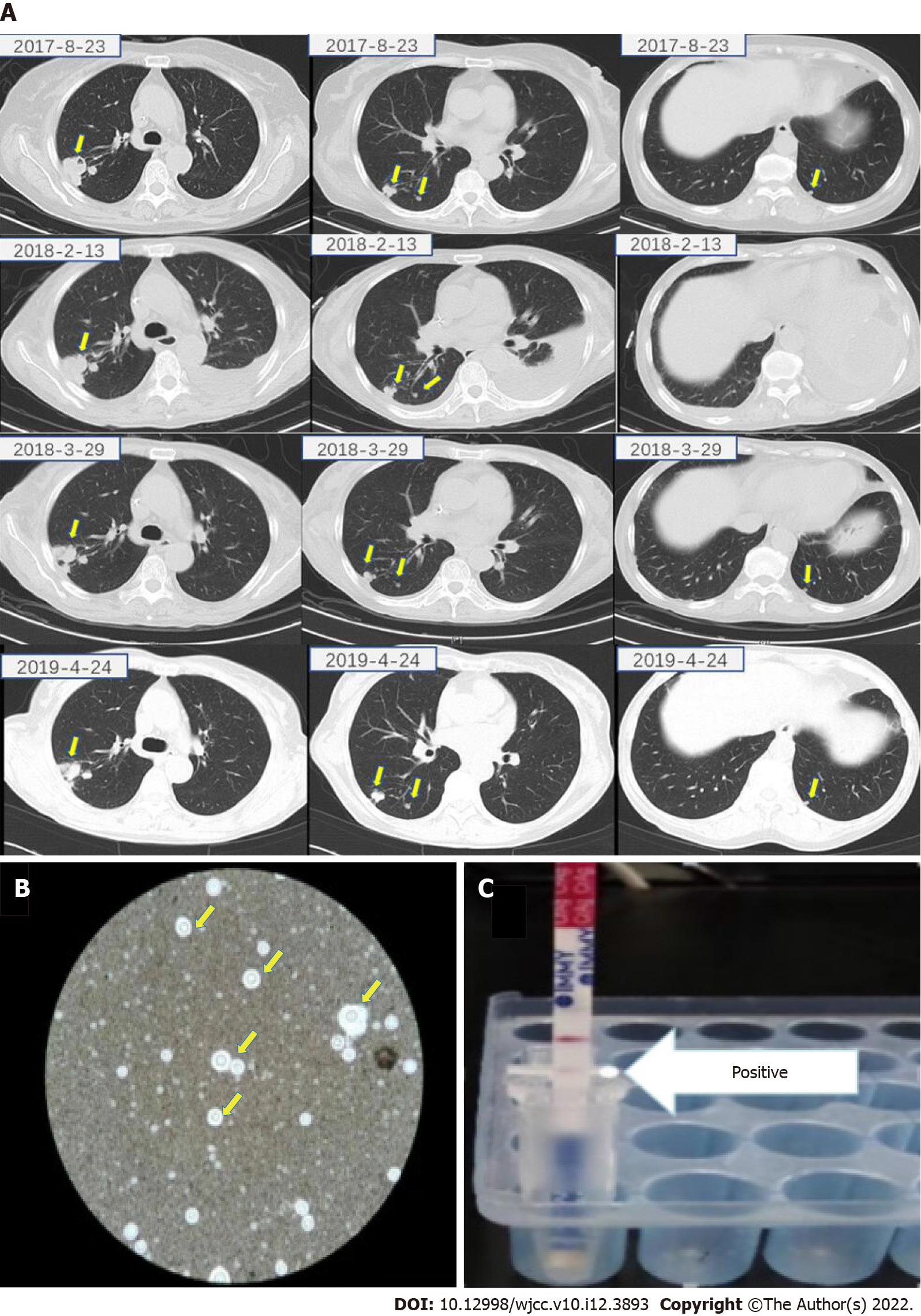
Case 1: The patient was HIV-negative. A CT-guided transthoracic needle lung biopsy (TNLB) of a nodule in the right lung was sent for evaluation 3 d after admission (Figure 1A). Her serum CrAg test was negative, while her lung biopsy revealed Cryptococcus neoformans infection. Lumbar puncture ruled out Cryptococcus infection of the nervous system. Therefore, she was investigated for PC, and antifungal therapy (fluconazole: 400 mg once daily for 3 mo and then voriconazole 200 mg twice daily for 9 mo) was initiated; however, her lung lesions did not resolve. A follow-up CT-guided TNLB on September 21, 2018 was positive for Cryptococcus neoformans on ink staining (Figure 1B). At that time, CrAg testing of lung biopsy tissue homogenate was performed, which yielded a positive result (Figure 1C). Her serum CrAg test and lung tissue culture remained negative.
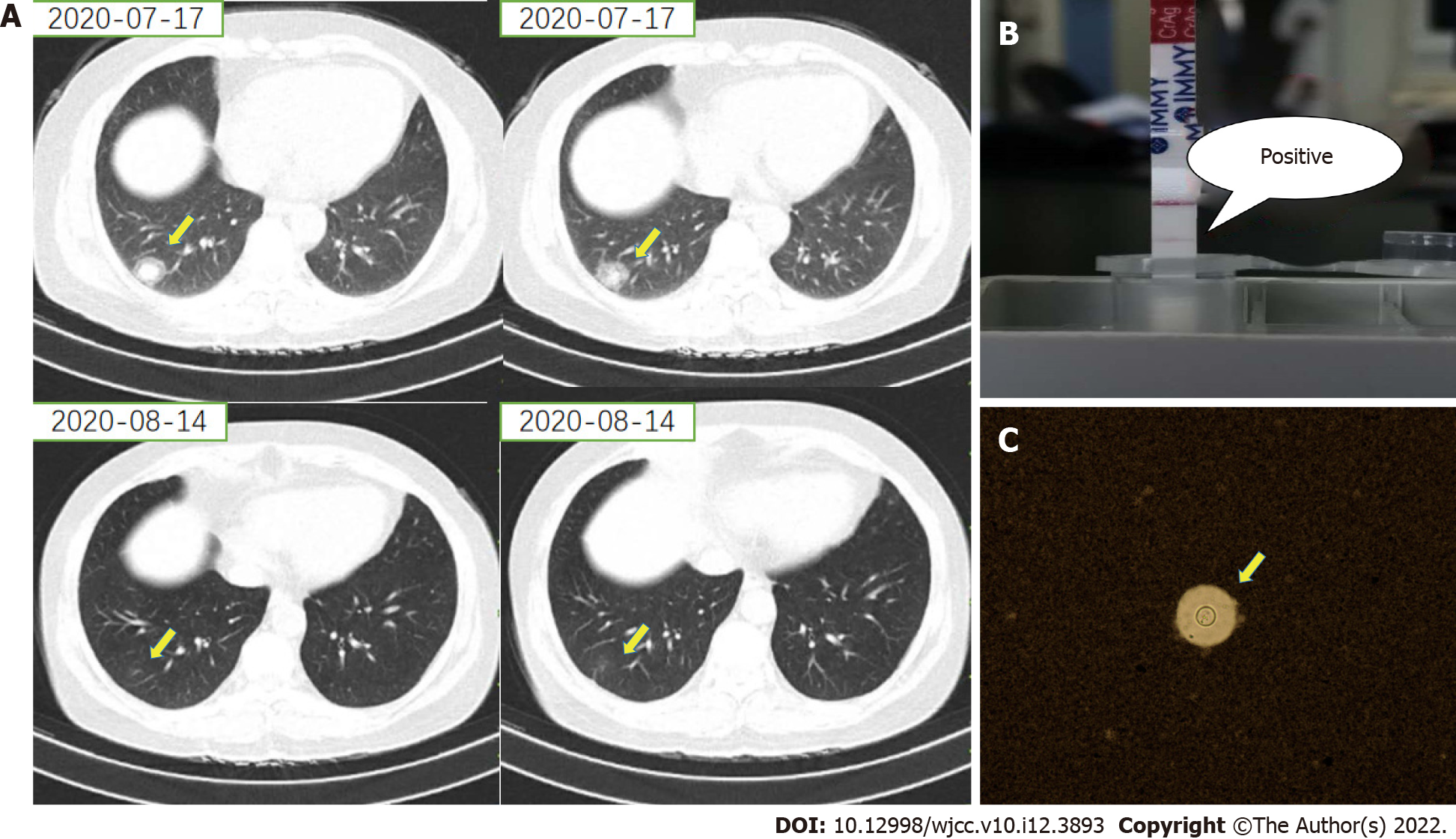
Case 2: The patient was HIV-negative. She underwent CT-guided TNLB of a nodule in the lower lobe of the right lung 2 d after admission (Figure 2A). CrAg testing using lung biopsy tissue homogenate was positive (Figure 2B). Ink staining of her lung biopsy specimen was positive for Cryptococcus neoformans (Figure 2C). Lumbar puncture ruled out Cryptococcus infection of the nervous system.
The final diagnosis of both cases was PC.
Case 1: Antifungal therapy (fluconazole: 400 mg once daily for 3 mo and then voriconazole 200 mg twice daily for 9 mo) was initiated.
Case 2: Antifungal therapy (fluconazole: 400 mg once daily for 3 mo) was initiated.
Case 1: Antifungal therapy had to be discontinued because of hepatic impairment. The lung lesions were stable without apparent respiratory symptoms for one year after antifungal therapy was discontinued (Figure 1A).
Case 2: Imaging follow-up after 3 mo of antifungal therapy revealed very good resolution of the nodule in the right lung seen previously (Figure 2A).
Early diagnosis of PC is crucial for timely and effective treatment. The diagnosis is based on a combination of clinical symptoms (e.g., cough, expectoration, chest tightness, chest pain, fever, and dyspnoea), suspicious radiological findings, and laboratory confirmation[1]. PC may easily be misdiagnosed or underdiagnosed in the absence of clinical symptoms, especially for immunocompetent patients[6]. Clustered or solitary pulmonary nodules are the most commonly seen lung abnormalities in PC[11]. The radiographic similarities to pneumonia or neoplasms, however, can often confuse or delay the clinical diagnosis. Further diagnostic evaluation is often needed to rule out or confirm the diagnosis. The laboratory confirmation of PC is often the next step in evaluation and usually involves serology, histopathology, and/or mycological culture[2].
Lung tissue biopsies are an important method for a definitive diagnosis. Cryptococcus neoformans, an encapsulated organism, is a narrow-based budding yeast, as seen on histological staining with India ink, haematoxylin and eosin, Grocott-Gomori’s methenamine silver, or periodic acid-Schiff[1,12]. However, in several previous studies, Cryptococcus in some samples did not have a typical polysaccharide capsule[13]. In a previous study, the detection rate of Cryptococcus neoformans observed by electron microscopy was 89.5%[3]. Samples obtained by CT-guided percutaneous lung biopsy may therefore not be adequate for staining and present a further diagnostic dilemma in confirming cryptococcosis.
The culture of respiratory samples has a complementary role in confirming PC. However, Cryptococcus cultures often take several days to grow, and many factors may influence the culture results of lung tissue, such as the number of pathogens, previous antifungal agents administered and duration of culture. A study reported a diagnostic rate of 70.8% for lung tissue culture[5].
Serum CrAg testing is a convenient, sensitive and rapid method for diagnosing PC[5]. The overall sensitivity and specificity of CrAg testing in the diagnosis of cryptococcal infection were approximately 97.6% and 98.1%, respectively[7]. However, in the two presented cases, the serum CrAg tests were all falsely negative. A false-negative CrAg test result may be due to a prozone reaction due to high antigen titres, low fungal load, samples transported in inappropriate vials, the presence of immunocomplexes preventing the release of glucuronoxylomannan antigen, or hypocapsular or acapsular strains of Cryptococcus spp[14]. Patients with a single pulmonary nodule were less likely to have positive antigen testing than those with other radiographic presentations or concomitant extrapulmonary disease[4]. For cases with a single pulmonary nodule, cryptococcal capsular antigen possibly only exists in the nodule and is not released into the blood. This might be the reason why lung tissue homogenate CrAg testing is more sensitive than serum testing in these cases.
However, there is a limitation of CrAg testing invasion in lung tissue homogenates. Since there are only two cases, this detection methodology deserves further study in a large sample.
Due to the potential risk of further dissemination of Cryptococcus infection and the long duration of antifungal therapy, it is necessary to combine multiple methods to improve the diagnostic certainty. According to our cases, lung tissue homogenate CrAg testing may help enhance the accuracy of the diagnosis, especially for serologically negative patients.
We acknowledge the contributions of Mr Jun-Min Cao and Mr Jian-Feng Wang for the research assistance.
| 1. | Setianingrum F, Rautemaa-Richardson R, Denning DW. Pulmonary cryptococcosis: A review of pathobiology and clinical aspects. Med Mycol. 2019;57:133-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 173] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 2. | Gazzoni AF, Severo CB, Salles EF, Severo LC. Histopathology, serology and cultures in the diagnosis of cryptococcosis. Rev Inst Med Trop Sao Paulo. 2009;51:255-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Zeng Y, Wu X, Yi X, Luo B, Zhu M, Rui W, Zhu X, Li X, Li H. Clinicopathologic and ultrastructural study of non-HIV-related primary pulmonary cryptococcosis in China: report of 43 cases. Ultrastruct Pathol. 2011;35:19-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Singh N, Alexander BD, Lortholary O, Dromer F, Gupta KL, John GT, del Busto R, Klintmalm GB, Somani J, Lyon GM, Pursell K, Stosor V, Muñoz P, Limaye AP, Kalil AC, Pruett TL, Garcia-Diaz J, Humar A, Houston S, House AA, Wray D, Orloff S, Dowdy LA, Fisher RA, Heitman J, Wagener MM, Husain S. Pulmonary cryptococcosis in solid organ transplant recipients: clinical relevance of serum cryptococcal antigen. Clin Infect Dis. 2008;46:e12-e18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 137] [Cited by in RCA: 110] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 5. | Zhou Y, Lin PC, Ye JR, Su SS, Dong L, Wu Q, Xu HY, Xie YP, Li YP. The performance of serum cryptococcal capsular polysaccharide antigen test, histopathology and culture of the lung tissue for diagnosis of pulmonary cryptococcosis in patients without HIV infection. Infect Drug Resist. 2018;11:2483-2490. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Xie X, Xu B, Yu C, Chen M, Yao D, Xu X, Cai X, Ding C, Wang L, Huang X. Clinical analysis of pulmonary cryptococcosis in non-HIV patients in south China. Int J Clin Exp Med. 2015;8:3114-3119. [PubMed] |
| 7. | Huang HR, Fan LC, Rajbanshi B, Xu JF. Evaluation of a new cryptococcal antigen lateral flow immunoassay in serum, cerebrospinal fluid and urine for the diagnosis of cryptococcosis: a meta-analysis and systematic review. PLoS One. 2015;10:e0127117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 8. | Zhang Y, Zhang SX, Trivedi J, Toll AD, Brahmer J, Hales R, Bonerigo S, Zeng M, Li H, Yung RC. Pleural fluid secondary to pulmonary cryptococcal infection: a case report and review of the literature. BMC Infect Dis. 2019;19:710. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Musabende M, Mukabatsinda C, Riviello ED, Ogbuagu O. Concurrent cryptococcal meningitis and disseminated tuberculosis occurring in an immunocompetent male. BMJ Case Rep. 2016;2016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Liaw YS, Yang PC, Yu CJ, Chang DB, Wang HJ, Lee LN, Kuo SH, Luh KT. Direct determination of cryptococcal antigen in transthoracic needle aspirate for diagnosis of pulmonary cryptococcosis. J Clin Microbiol. 1995;33:1588-1591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Hu Y, Ren SY, Xiao P, Yu FL, Liu WL. The clinical and radiological characteristics of pulmonary cryptococcosis in immunocompetent and immunocompromised patients. BMC Pulm Med. 2021;21:262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Guarner J, Brandt ME. Histopathologic diagnosis of fungal infections in the 21st century. Clin Microbiol Rev. 2011;24:247-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 465] [Cited by in RCA: 563] [Article Influence: 37.5] [Reference Citation Analysis (0)] |
| 13. | Casadevall A, Coelho C, Cordero RJB, Dragotakes Q, Jung E, Vij R, Wear MP. The capsule of Cryptococcus neoformans. Virulence. 2019;10:822-831. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 156] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 14. | Chastain DB, Guarner J, Franco-Paredes C. Cryptococcal antigen negative meningoencephalitis in HIV/AIDS. Diagn Microbiol Infect Dis. 2017;89:143-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Respiratory system
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Darbari A, India; Nabil A, Japan S-Editor: Liu JH L-Editor: A P-Editor: Liu JH