Published online Apr 16, 2022. doi: 10.12998/wjcc.v10.i11.3547
Peer-review started: October 30, 2021
First decision: December 27, 2021
Revised: January 6, 2022
Accepted: February 27, 2022
Article in press: February 27, 2022
Published online: April 16, 2022
Processing time: 160 Days and 2.8 Hours
Simultaneous cerebral and myocardial infarction with arterial involvement has not been reported in hypereosinophilic syndrome (HES). Here, we report a patient with HES that was also associated with acute ischemic stroke, myocardial infarction, and arterial involvement of the left common carotid artery, vertebral arteries, posterior cerebral artery, and coronary artery.
A 64-year-old male patient was admitted with headache and right lower extremity weakness. Laboratory tests indicated eosinophilia. Brain magnetic resonance imaging (MRI) showed bilateral and multiple acute infarcts in the border zones. Electrocardiography revealed that T wave was inverted and that the concentration of troponin I was significantly elevated above normal levels. Cardiac echocardiography showed an ejection fraction of 69% with mitral and tricuspid mild regurgitation. Computed tomography angiography detected multiple and localized instances of mild stenosis in the left common carotid artery bifurcation, bilateral vertebral arteries (V5 segment), and the posterior cerebral artery (P2 segment). These were observed together with multiple non-calcified and mixed plaques as well as luminal stenosis in the left circumflex artery, left anterior descending artery, and right coronary artery. The patient was treated with oral methylprednisolone and clopidogrel, after which the absolute eosinophil count fell rapidly to a normal level. After one month, a second brain MRI showed a partial reduction in the size and number of the lesions.
HES can masquerade as ischemic stroke, myocardial infarction, and arterial vascular involvement. The patient reported here recovered very quickly when his eosinophil blood count returned to normal. Early diagnosis and rapid reduction of eosinophils may lead to a good prognosis.
Core Tip: Hypereosinophilic syndrome (HES) is characterized by unexplained eosinophilia in the blood and tissues. Neurologic and cardiac involvement in patients with HES is common and variable. Eosinophil-mediated arterial vascular involvement is a rare manifestation of HES. This rare case of HES was accompanied by acute ischemic stroke, myocardial infarction and arterial vascular involvement. Early diagnosis and rapid reduction of eosinophils may lead to a good prognosis.
- Citation: Sun RR, Chen TZ, Meng M. Hypereosinophilic syndrome presenting as acute ischemic stroke, myocardial infarction, and arterial involvement: A case report. World J Clin Cases 2022; 10(11): 3547-3552
- URL: https://www.wjgnet.com/2307-8960/full/v10/i11/3547.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i11.3547
Hypereosinophilic syndrome (HES) is characterized by unexplained eosinophilia in the blood and tissues, and is associated with a variety of clinical manifestations[1]. It has long been thought that HES is associated with multiple organ dysfunctions, ranging from minor skin involvement to serious and even life-threatening cardiovascular, hematologic, and neurologic manifestations[2]. Neurologic involvement in patients with HES is common and highly variable, and includes the occurrence of peripheral neuropathy, encephalopathy, and stroke[3]. Cardiac involvement may lead to the development of thrombi, resulting a transient ischemic attack or embolic stroke with associated sequelae[4]. However, eosinophil-mediated arterial vascular involvement is a rare manifestation of HES. Most HES patients present with organ involvement showed normal cranial computed tomography angiogram (CTA) or magnetic resonance angiography[3,5,6]. Here, we report a rare case of HES accompanied by the simultaneous occurrence of acute ischemic stroke and myocardial infarction (MI), as well as arterial vascular involvement of the left common carotid artery, vertebral arteries, posterior cerebral artery, and coronary artery.
A 64-year-old male patient without any cerebrovascular risk factors was admitted to our hospital with a headache and right lower extremity weakness that lasted for two days.
The patient had a history of toothache, smoking, and alcohol consumption.
Until hospitalization, the patient was not burdened with any significant cardiovascular comorbidity.
The patient had no pertinent family history of heart disease or other illnesses.
The results of a physical examination showed right lower extremity weakness (4-/5 strength) and dystaxia.
Routine laboratory tests revealed significant leucocytosis (12.36 × 109/L) and an elevated eosinophil count (6.89 × 109/L, 55.7% of leukocytes) in the peripheral blood. The results of a blood clotting test, urine and stool routine examination, virus screening, liver and renal function examination, and immunological function examination were normal. The antinuclear antibodies, anti-neutrophil cytoplasmic antibodies, and tumor markers were also negative. Molecular genetic analysis of fusion gene mutation (Fip1-like 1-platelet-derived growth factor receptor alpha) was also negative. Bone marrow aspirate results were compatible with HES, showing no sign of myelodysplasia, hemoparasite, or atypical cells. Cerebrospinal fluid analysis revealed that the levels of white blood cells, proteins, and glucose were normal. Acid-fast staining and India ink staining of cerebrospinal fluid were negative. Electrocardiography (ECG) revealed that the T wave was inverted and the concentration of troponin I (0.644 ng/mL) was significantly elevated. The clinical history and examination results of this patient showed no sign of parasitic infection, neoplasm, vasculitis, or allergy.
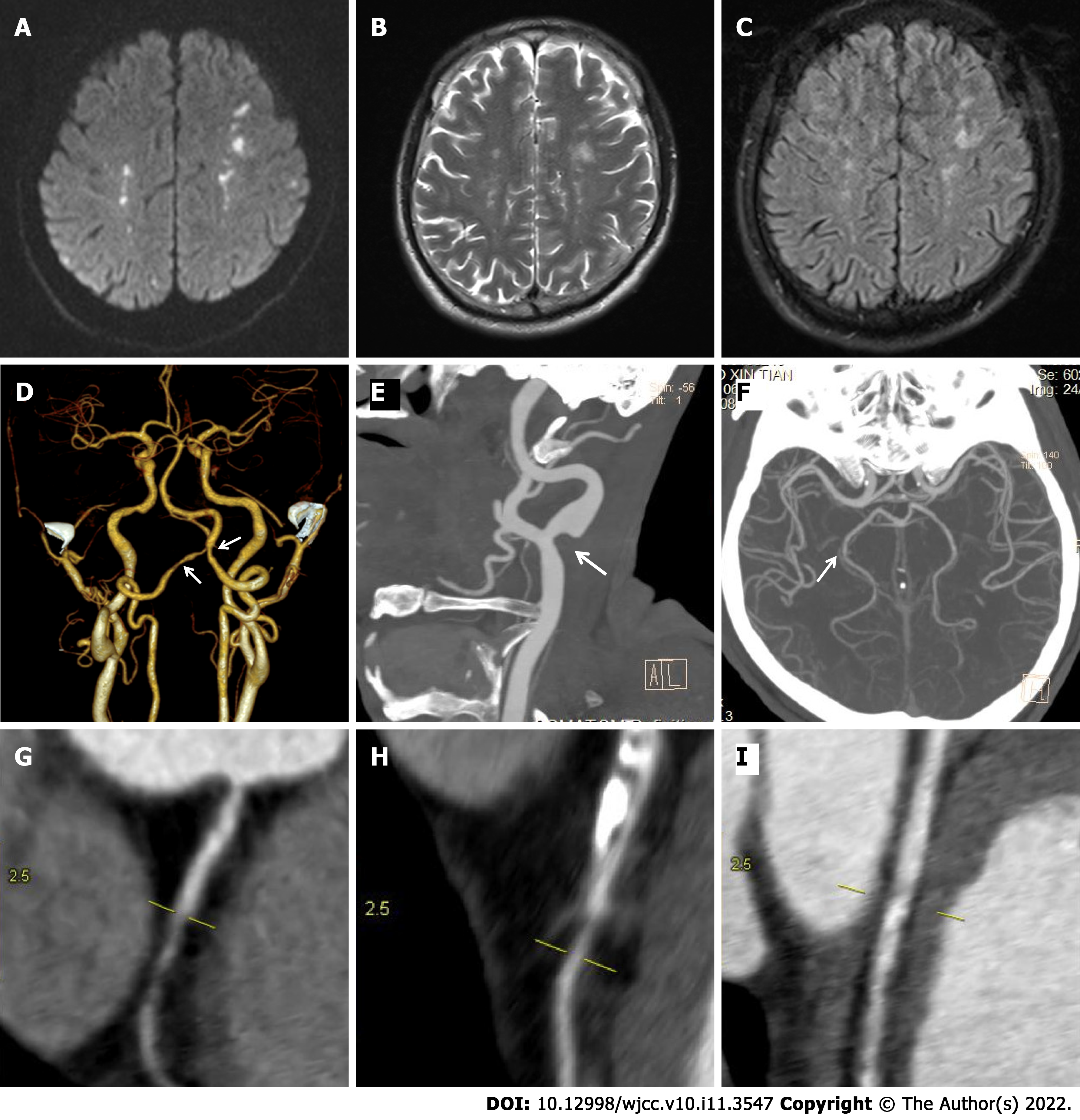
A CT scan of the chest was normal. Abdominal ultrasound revealed multiple hepatic cysts. Brain magnetic resonance imaging (MRI) detected bilateral and multiple acute infarcts in the border zones, which were located in the cortical and subcortical areas (Figure 1A-C). CTA of the head and neck revealed multiple and localized mild instances of stenosis in the left common carotid artery bifurcation, bilateral vertebral arteries (V5 segment), and posterior cerebral artery (P2 segment) (Figure 1D-F). Cardiac echocardiography showed an ejection fraction of 69% with mitral and tricuspid mild regurgitation. Coronary CTA showed multiple non-calcified, mixed plaques and luminal stenoses in the left circumflex artery, left anterior descending artery, and right coronary artery (Figure 1G-I). The results of cardiac examination supported the diagnosis of non-ST-elevated MI.
The patient was diagnosed with HES, accompanied with multiple cerebral infarctions and acute MI.
The patient was treated with oral methylprednisolone (1 mg/kg/d) and clopidogrel (75 mg/d) for 7 d, and responded well to the treatment. The absolute eosinophil count (0.18 × 109/L, 1.8% of leukocytes) fell to a normal level within 7 d.
The patient was discharged after two weeks and continued taking low-dose prednisone. The ECG at discharge showed a normal T wave. The troponin I was 0.455 ng/mL during hospitalization and 0.012 ng/mL at discharge. After one month, a second brain MRI showed a partial reduction in the size and number of the lesions (Figure 2A-C). After one year, another brain MRI showed cerebromalacia in multiple areas of the lesions (Figure 2D-F). The follow-up of this patient was satisfactory in that he remained asymptomatic while on low-dose prednisone.
HES comprises a group of disorders characterized by the abnormal accumulation of eosinophils in the peripheral tissues or blood, independent of known secondary causes of eosinophilia (e.g., parasitic infection)[4]. In 2010, new diagnostic criteria of HES were proposed: An absolute eosinophil count of more than 1500/mm3 on at least two occasions or marked blood eosinophilia and prominent tissue eosinophilia associated with symptoms; exclusion of secondary causes of eosinophilia, such as neoplasms, hypoadrenalism, chemical- or drug-induced eosinophilia, allergic diseases, and viral or parasitic infection. Advances in diagnostic and therapeutic approaches have prompted a re-evaluation of the definition and classification of HES[7]. More than half of the patients with HES in one study (27 of 52) had neurologic dysfunction[8]. Stroke represents the most devastating neurological consequence of HES, which is characterized by a distinct pattern of both internal and external border zone infarcts[2].
In the patient reported here, eosinophilic involvement resulted in multiple cerebral infarctions and acute MI. Acute cerebral infarctions in the border zones were the first presenting symptom in this case. Meanwhile, the patient suffered from ischemic ECG changes, troponin I elevation, and mild valve regurgitation in echocardiography, which supported the diagnosis of MI. As a rare complication of HES, MI occurs as the result of endomyocardial fibrosis[9]. CTA of the head and neck, as well as the coronary artery showed multiple arterial stenoses in this case. Single arterial stenosis or occlusion has been only occasionally reported in patients with HES. Chang et al[10] reported a 43-year-old male patient with HES presenting with ischemic stroke and segmental stenosis of the right posterior cerebral artery resulting from direct eosinophilic toxicity. Li et al[11] described a middle-aged woman with idiopathic HES presenting with bilateral middle cerebral artery occlusion and progressive multiple cerebral infarction. Our patient suffered from multiple arterial vascular damage involving the left common carotid artery, vertebral arteries, posterior cerebral artery, and coronary artery. Eosinophilic toxicity to the vascular wall, via either arterial or venous vessels, was considered the pathological consequence of eosinophil accumulation[10]. Eosinophils have direct cytotoxic activity through the local release of toxic substances, including pro-inflammatory cytokines, reactive oxygen species, enzymes, arachidonic acid-derived factors, and cationic proteins[10,12].
The mechanism of eosinophilia-associated stroke remains unknown. The major etiology is cardiac embolism. More than half of cases with HES show a sign of cardiac involvement in echocardiography, which is a common source of thromboembolism with thrombi formation in damaged endocardium[13,14]. With the development of thromboembolism, patients with HES may experience a transient ischemic attack or embolic stroke as the initial presenting symptom[15]. Eosinophilia may damage the myocardium and endocardium, and therefore contribute to cardiac embolism by releasing eosinophilic granule contents, such as eosinophilic cationic protein and major basic protein[14]. Generally, eosinophilic myocarditis can be divided into three stages, which may occur simultaneously: (1) Acute necrosis/myocarditis stage-eosinophilic infiltration of the myocardium associated with myocardial necrosis due to the release of toxic cationic proteins from degranulated eosinophils; (2) thrombosis stage-thrombosis at both ventricles where the ventricular outflow tract and subvalvular regions are associated with a significant risk of embolic complications; and (3) fibrotic stage-fibrosis replaces the thrombus formed on denuded myocardium and often requires surgical intervention[9,16]. The clinical records and laboratory tests of this case indicated that eosinophilia-induced cardioembolism and vascular wall damage may have been the main cause of cerebral infarction. Unfortunately, cardiac MRI and endocardial biopsy were not performed. Despite advances in noninvasive imaging methods (e.g., echocardiography and cardiac MRI), endomyocardial biopsy remains the gold standard for the diagnosis of HES, especially in patients at the early stages of myocardial infiltration.
Corticosteroids are the most widely used medication to reduce eosinophil levels in patients with HES. If the patient presents with significant end-organ damage, corticosteroid treatment should be initiated immediately. An antiplatelet agent was used to reduce the risk of embolization in this case, however, the use of antiplatelet agents or anticoagulants alone is not recommended. The rapid reduction of eosinophil count is essential for preventing thromboembolic events and end-organ damage in patients at risk.
In conclusion, neurologic and cardiac complications occurred almost simultaneously in this case. Thus, the early diagnosis and treatment of HES are crucial for the prevention of widespread cardioembolism and subsequent irreversible, life-threatening cerebrovascular complications. Long-term follow-up and ongoing surveillance are important for monitoring the progression of the disease. Clinicians should be cognizant of HES patients presenting with cerebral infarction in the border zone. Early diagnosis and prompt treatment with corticosteroids are required.
| 1. | Kahn JE, Groh M, Lefèvre G. (A Critical Appraisal of) Classification of Hypereosinophilic Disorders. Front Med (Lausanne). 2017;4:216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 55] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 2. | Rosenberg J, Aamodt W, Takvorian S, Mullen M. Clinical Reasoning: A young woman with symmetric weakness and behavioral disturbance. Neurology. 2018;90:e1442-e1447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Chen H, Raza HK, Jing J, Shen D, Xu P, Zhou S, Zu J, Yang X, Zhang W, Zhang S, Hua F, Cui G. Hypereosinophilic syndrome with central nervous system involvement: Two case reports and literature review. Brain Inj. 2017;31:1695-1700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
| 4. | Curtis C, Ogbogu P. Hypereosinophilic Syndrome. Clin Rev Allergy Immunol. 2016;50:240-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 129] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 5. | Psychogios K, Evmorfiadis I, Dragomanovits S, Stavridis A, Takis K, Kaklamanis L, Stathis P. ANCA-Negative Churg-Strauss Syndrome Presenting as Acute Multiple Cerebral Infarcts: A Case Report. J Stroke Cerebrovasc Dis. 2017;26:e47-e49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Rohmer J, Groh M, Samson M, London J, Jachiet M, Rouzaud D, Paule R, Suarez F, Lefèvre G, Cohen F, Lambotte O, Perlat A, Bielefeld P, Guillevin L, Kahn JE, Terrier B; French Vasculitis Study Group (FVSG). Distal ischemia as the initial presentation of hypereosinophilic syndrome-related arterial involvement: A case study and literature review. Autoimmun Rev. 2019;18:828-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Simon HU, Rothenberg ME, Bochner BS, Weller PF, Wardlaw AJ, Wechsler ME, Rosenwasser LJ, Roufosse F, Gleich GJ, Klion AD. Refining the definition of hypereosinophilic syndrome. J Allergy Clin Immunol. 2010;126:45-49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 256] [Cited by in RCA: 216] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 8. | Moore PM, Harley JB, Fauci AS. Neurologic dysfunction in the idiopathic hypereosinophilic syndrome. Ann Intern Med. 1985;102:109-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 152] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Ogbogu PU, Rosing DR, Horne MK 3rd. Cardiovascular manifestations of hypereosinophilic syndromes. Immunol Allergy Clin North Am. 2007;27:457-475. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 282] [Cited by in RCA: 275] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 10. | Chang WL, Lin HJ, Cheng HH. Hypereosinophilic syndrome with recurrent strokes: a case report. Acta Neurol Taiwan. 2008;17:184-188. [PubMed] |
| 11. | Li QF, Zhang Q, Huang YF, Zhang ZX. Acute progressive stroke with middle cerebral artery occlusion caused by idiopathic hypereosinophilic syndrome: a case report. BMC Neurol. 2020;20:361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Roufosse F, Cogan E, Goldman M. The hypereosinophilic syndrome revisited. Annu Rev Med. 2003;54:169-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 82] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Ommen SR, Seward JB, Tajik AJ. Clinical and echocardiographic features of hypereosinophilic syndromes. Am J Cardiol. 2000;86:110-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 129] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 14. | Rezaizadeh H, Sanchez-Ross M, Kaluski E, Klapholz M, Haider B, Gerula C. Acute eosinophilic myocarditis: diagnosis and treatment. Acute Card Care. 2010;12:31-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Spry CJ, Davies J, Tai PC, Olsen EG, Oakley CM, Goodwin JF. Clinical features of fifteen patients with the hypereosinophilic syndrome. Q J Med. 1983;52:1-22. [PubMed] |
| 16. | Cheung CC, Constantine M, Ahmadi A, Shiau C, Chen LYC. Eosinophilic Myocarditis. Am J Med Sci. 2017;354:486-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 63] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lakusic N, Croatia; Shariati MBH, Iran S-Editor: Chen YL L-Editor: A P-Editor: Chen YL