Published online Apr 6, 2022. doi: 10.12998/wjcc.v10.i10.3200
Peer-review started: November 6, 2021
First decision: December 27, 2021
Revised: January 5, 2022
Accepted: February 23, 2022
Article in press: February 23, 2022
Published online: April 6, 2022
Processing time: 143 Days and 10.2 Hours
General anesthesia in critically ill patients is associated with increased risk of complications. Nerve block anesthesia is an alternative, but could be challenging in cases with surgical field that involves multiple dermatomes.
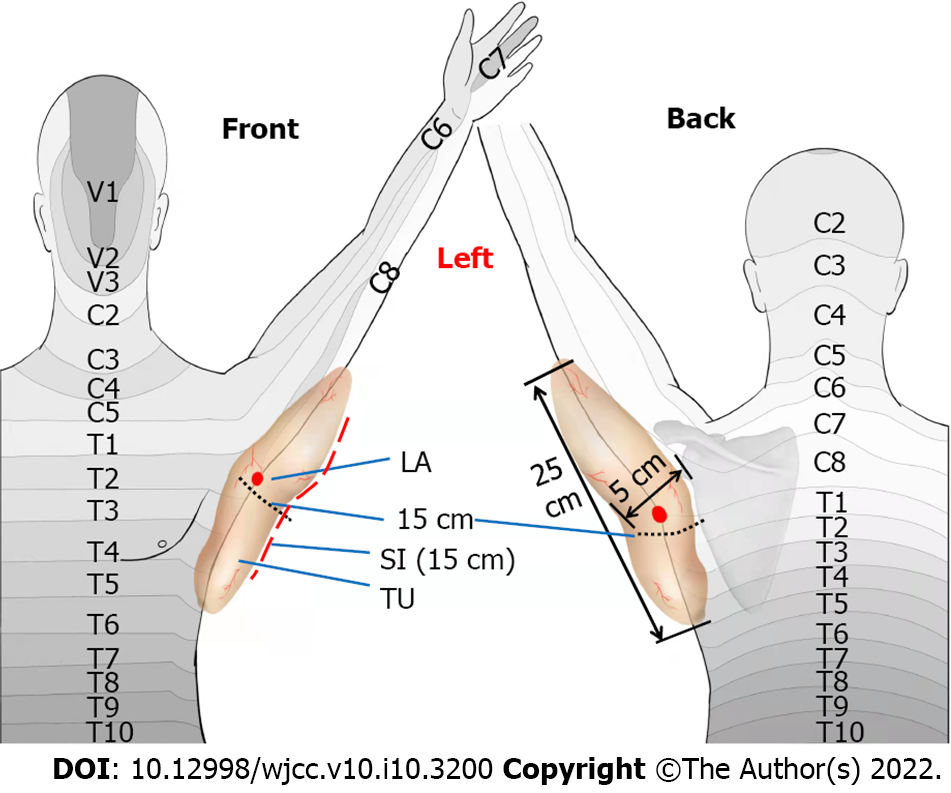
We report resection of a giant lipoma in the left shoulder and upper back under supraclavicular brachial plexus block plus T3-4 paravertebral block in an older patient with severe asthma. A 70-year-old patient presented with a slow-growing giant mass (25, 15 and 5 cm in length, width and depth, respectively) that extended from the lateral side of the left scapula to the axillary midline, and from the T5 thoracic vertebra intercostal to the mid-medial section of the left upper arm. He had sharp intermittent pain over the mass for the past 7 d. The patient also had severe bronchial asthma for the past 8 years. A pulmonary function test revealed only 20% of the predicted forced expiratory volume in 1 second (FEV1, 0.49 L). After controlling asthma with glucocorticoid, the tumor was resected under ultrasound-guided supraclavicular brachial plexus block and T3-4 paravertebral block. The surgery was completed without incident.
Ultrasound-guided regional nerve block is a viable alternative for patients with poor cardiopulmonary function undergoing shoulder, back and axillary surgery.
Core Tip: A giant lipoma that extended from the lateral side of the left scapula to the axillary midline, and from the fifth thoracic vertebra intercostal to the mid-medial section of the left upper arm was resected under ultrasound-guided brachial plexus block combined with thoracic paravertebral nerve block in an older patient with severe asthma. The patient recovered well after the operation. This anesthetic method could be a viable alternative to general anesthesia and epidural anesthesia in patients with poor cardiopulmonary function undergoing shoulder, back and axillary surgery.
- Citation: Liu Q, Zhong Q, Zhou NN, Ye L. Giant tumor resection under ultrasound-guided nerve block in a patient with severe asthma: A case report. World J Clin Cases 2022; 10(10): 3200-3205
- URL: https://www.wjgnet.com/2307-8960/full/v10/i10/3200.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i10.3200
General anesthesia is associated with a variety of complications, including respiratory depression, deep venous thrombosis, pulmonary embolism, postoperative hemorrhagic shock, pneumonia, and renal failure. Pulmonary complications represent a particular challenge in patients with existing pulmonary disease[1]. Regional anesthesia promotes postoperative recovery, and has been associated with reduced risk of postoperative complications[2]. Nerve block anesthesia could provide sufficient anesthesia if the surgery is confined to the area innervated by the target nerve, but has been limited by inaccuracy and local complications. Ultrasound guidance ensures accurate delivery of the anesthetic agent to the target area and improves the safety of nerve block anesthesia[3,4]. Brachial plexus block is primarily used in surgery of the upper limbs, whereas thoracic paravertebral block is used in thoracic surgery[5-7]. Here, we report combined use of brachial plexus block and thoracic paravertebral block to resect a giant lipoma (25, 15 and 5 cm in length, width and depth, respectively) that involved both the left shoulder and upper back in a patient with severe asthma.
A 70-year-old man (170 cm; 60 kg; body mass index 20.8 kg/m2) presented with sharp, acupuncture-like intermittent pain for 7 d. The pain occurred at a frequency of five or six episodes per day, with each lasting for 1-2 min. The pain intensity was 3 on the visual analog scale (VAS). The patient disclosed a giant mass in the left shoulder and upper back. The mass had been growing at a slow pace for 10 years.
The patient had severe bronchial asthma for 8 years (3 attacks per day on average), and used salbutamol aerosol to control symptoms.
The patient had no other significant medical history.
Family history was unremarkable.
Body examination confirmed the giant mass (25, 15 and 5 cm in length, width and depth, respectively) that extended from the lateral side of the left scapula to the axillary midline, and from the fifth thoracic vertebra (T5) intercostal to the mid-medial section of the left upper arm. The mass was not tender.
To prepare for surgery, a pulmonary function test was conducted. Forced expiratory volume in 1 second (FEV1) was 0.49 L (about 20% of the predicted value), and FEV1/forced vital capacity (FEV1/FVC) was 54% of predicted value. The preoperative erythrocyte sedimentation rate was 20 mm/h; the percentage of neutrophils was 74.4%. Partial oxygen pressure, oxygen saturation and partial carbon dioxide pressure were 78 mmHg, 94% and 44 mmHg, respectively.
Ultrasound examination as well as computed tomography report from a local hospital (images not available) suggested clear boundary to surrounding tissues.
The final diagnosis was benign tumor of the shoulder and back.
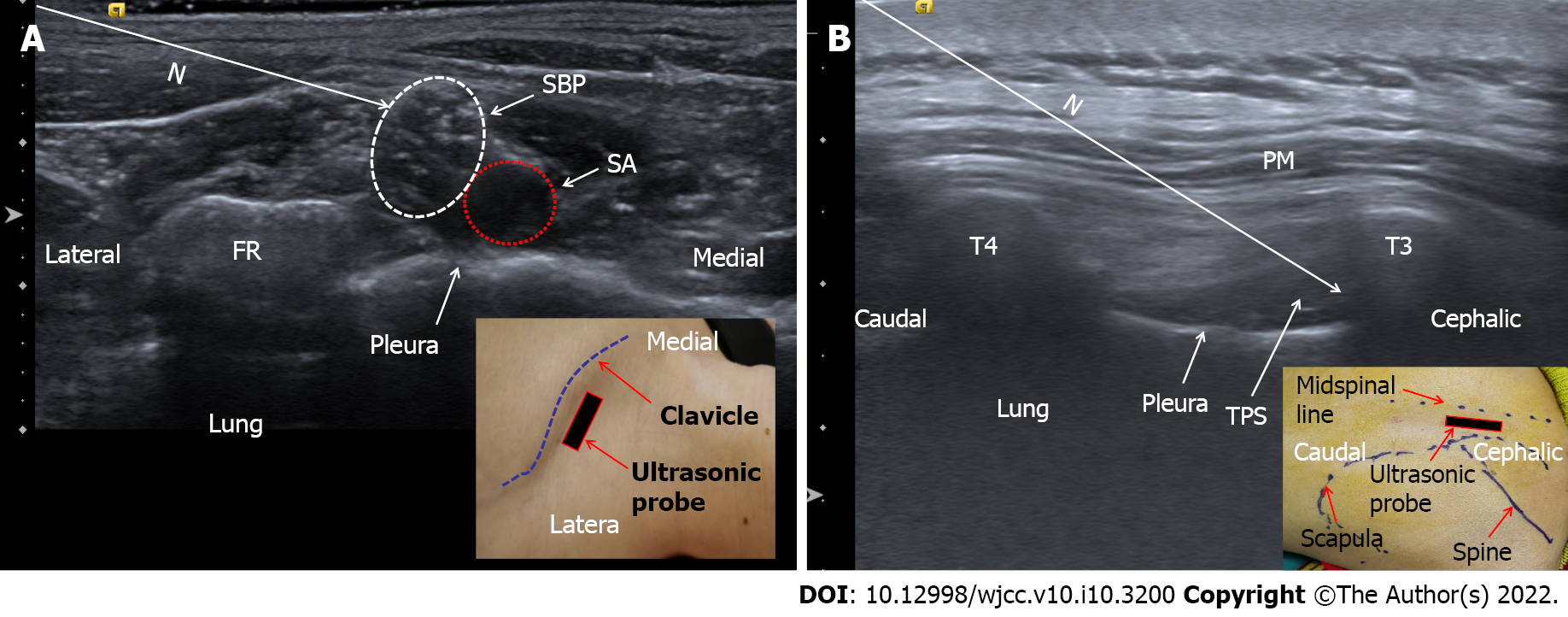
Glucocorticoid treatment (budesonide inhalation twice daily) was initiated to control asthma to a reasonable condition. General anesthesia in this patient was risky. Thoracic epidural block was considered but not adopted considering the risk of hypotension as well as the technical difficulty[8]. Since the tumor was confined to the area of the seventh cervical vertebra (C7) to T5 (Figure 1), we decided to use a combination of brachial plexus block and thoracic paravertebral block[6,8]. Since the tumor occupied a wide range of area innervated by C7-T5 (Figure 1), surgery was conducted under brachial plexus block (0.4% ropivacaine 15 mL) plus thoracic paravertebral block (third-fourth thoracic vertebra, T3-4, 0.4% ropivacaine 15 mL) under ultrasound guidance using a 10-MHz linear array probe (Figure 2). Local infiltration anesthesia included 1% lidocaine (3 mL) for the block as well as the incision site (Figure 1).
The surgery was completed with no incidents. The pain intensity remained 2-3 on the 10-point VAS scale during the first 8 h after surgery. Postoperative pathological examination revealed lipoma. The patient developed mild pulmonary infection on the third day after the operation, but recovered after empirical antibiotic treatment.
Many types of brachial plexus block, including intermuscular sulcus block, supraclavicular brachial plexus block, infraclavicular brachial plexus block and axillary brachial plexus block, are available for surgery in the upper limbs depending on the specific location. Supraclavicular brachial block provides anesthesia from the distal end of the upper limb to the mid humerus, part of the area occupied by the tumor mass in the index patient. The incidence of pleural puncture and pneumothorax after paravertebral block is 1.1% and 0.5%, respectively. The incidence of pulmonary complications and hypotension, however, is lower than with epidural anesthesia. The incidence of permanent nerve injury is also lower after paravertebral block than epidural anesthesia[6,8]. Ultrasound-guided bronchial plexus block in combination with thoracic paravertebral block has been used for postoperative analgesia or auxiliary anesthesia in breast surgery[6,8,9]. The index patient had severe asthma. General anesthesia could induce asthma attack upon tracheal intubation due to high airway responsiveness[10,11]. In regional nerve block, the airway is not manipulated/stimulated, thus minimizing the risk asthma attack[11]. Previous studies have suggested, that in patients undergoing thoracotomy, paravertebral block is superior to thoracic epidural anesthesia[12]. In a recent case report, a giant tumor that involved both the chest wall and axillary envelope was resected under ultrasound-guided interscalene brachial plexus block and serratus anterior plane block[8]. Exact location and size of the tumor in the index case are different. In another case report, combination of block anesthesia was used a patient with tumor in the area innervated by both the brachial plexus and T1-5 intercostal nerves[13]. Such a combination of block anesthesia could in theory provide adequate anesthesia, but the possibility of incomplete block is high due to anatomical specificity[4]. In the index case, the patient required local infiltration anesthesia at the site of incision, suggesting that the nerve block was incomplete (Figure 1). Nonetheless, supraclavicular brachial plexus block plus T3-4 paravertebral block was the most appropriate combination based on the tumor location in our opinion.
In comparison to general anesthesia, nerve block anesthesia promotes postoperative recovery[14], and reduces the risk of pulmonary, circulatory and intestinal complications, especially for patients with preoperative cardiopulmonary problems. As such, combination of nerve block anesthesia could be appropriate in a much wider setting than in the index patient, for example, frail elderly patients with limited cardiopulmonary reserve.
Ultrasound-guided brachial plexus block in combination with thoracic paravertebral block is a viable alternative for patients with poor cardiopulmonary function undergoing shoulder, back and axillary surgery.
The authors thank the index patient for agreeing to publish this report.
| 1. | Breivik H, Norum HM. [Regional analgesia--risks and benefits]. Tidsskr Nor Laegeforen. 2010;130:392-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Tziavrangos E, Schug SA. Regional anaesthesia and perioperative outcome. Curr Opin Anaesthesiol. 2006;19:521-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Re M, Blanco J, Gómez de Segura IA. Ultrasound-Guided Nerve Block Anesthesia. Vet Clin North Am Food Anim Pract. 2016;32:133-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Khanduri KC. Regional Anaesthesia Techniques for Orthopaedic Surgery. Med J Armed Forces India. 2008;64:108-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Ardon AE, Prasad A, McClain RL, Melton MS, Nielsen KC, Greengrass R. Regional Anesthesia for Ambulatory Anesthesiologists. Anesthesiol Clin. 2019;37:265-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Koyyalamudi VB, Arulkumar S, Yost BR, Fox CJ, Urman RD, Kaye AD. Supraclavicular and paravertebral blocks: Are we underutilizing these regional techniques in perioperative analgesia? Best Pract Res Clin Anaesthesiol. 2014;28:127-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | El-Boghdadly K, Wolmarans M, Stengel AD, Albrecht E, Chin KJ, Elsharkawy H, Kopp S, Mariano ER, Xu JL, Adhikary S, Altıparmak B, Barrington MJ, Bloc S, Blanco R, Boretsky K, Børglum J, Breebaart M, Burckett-St Laurent D, Capdevila X, Carvalho B, Chuan A, Coppens S, Costache I, Dam M, Egeler C, Fajardo M, Gadsden J, Gautier PE, Grant SA, Hadzic A, Hebbard P, Hernandez N, Hogg R, Holtz M, Johnson RL, Karmakar MK, Kessler P, Kwofie K, Lobo C, Ludwin D, MacFarlane A, McDonnell J, McLeod G, Merjavy P, Moran E, O'Donnell BD, Parras T, Pawa A, Perlas A, Rojas Gomez MF, Sala-Blanch X, Saporito A, Sinha SK, Soffin EM, Thottungal A, Tsui BCH, Tulgar S, Turbitt L, Uppal V, van Geffen GJ, Volk T, Elkassabany NM. Standardizing nomenclature in regional anesthesia: an ASRA-ESRA Delphi consensus study of abdominal wall, paraspinal, and chest wall blocks. Reg Anesth Pain Med. 2021;46:571-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 196] [Article Influence: 39.2] [Reference Citation Analysis (0)] |
| 8. | Guay Md J. Breast surgery without general anesthesia: is paravertebral blockade sufficient? Reg Anesth Pain Med. 2021;46:460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Woodworth GE, Ivie RMJ, Nelson SM, Walker CM, Maniker RB. Perioperative Breast Analgesia: A Qualitative Review of Anatomy and Regional Techniques. Reg Anesth Pain Med. 2017;42:609-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 192] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 10. | Kozian A, Schilling T, Hachenberg T. [Anesthetic management in bronchial asthma]. Anasthesiol Intensivmed Notfallmed Schmerzther. 2016;51:402-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Louie S, Morrissey BM, Kenyon NJ, Albertson TE, Avdalovic M. The critically ill asthmatic--from ICU to discharge. Clin Rev Allergy Immunol. 2012;43:30-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Yeung JH, Gates S, Naidu BV, Wilson MJ, Gao Smith F. Paravertebral block versus thoracic epidural for patients undergoing thoracotomy. Cochrane Database Syst Rev. 2016;2:CD009121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 154] [Cited by in RCA: 218] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 13. | Luo R, Gu Y, Deng X, Wu W, Yao Y. Giant axillary tumor resection using ultrasound-guided interscalene brachial plexus block and serratus anterior plane block. J Int Med Res. 2020;48:300060520954719. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Héroux J, Belley-Côté E, Echavé P, Loignon MJ, Bessette PO, Patenaude N, Baillargeon JP, D'Aragon F. Functional recovery with peripheral nerve block versus general anesthesia for upper limb surgery: a systematic review protocol. Syst Rev. 2019;8:273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Naganuma H, Oliver-Fornies P S-Editor: Chen YL L-Editor: Kerr C P-Editor: Chen YL