Published online Dec 16, 2013. doi: 10.12998/wjcc.v1.i9.295
Revised: October 29, 2013
Accepted: November 18, 2013
Published online: December 16, 2013
Processing time: 86 Days and 20.9 Hours
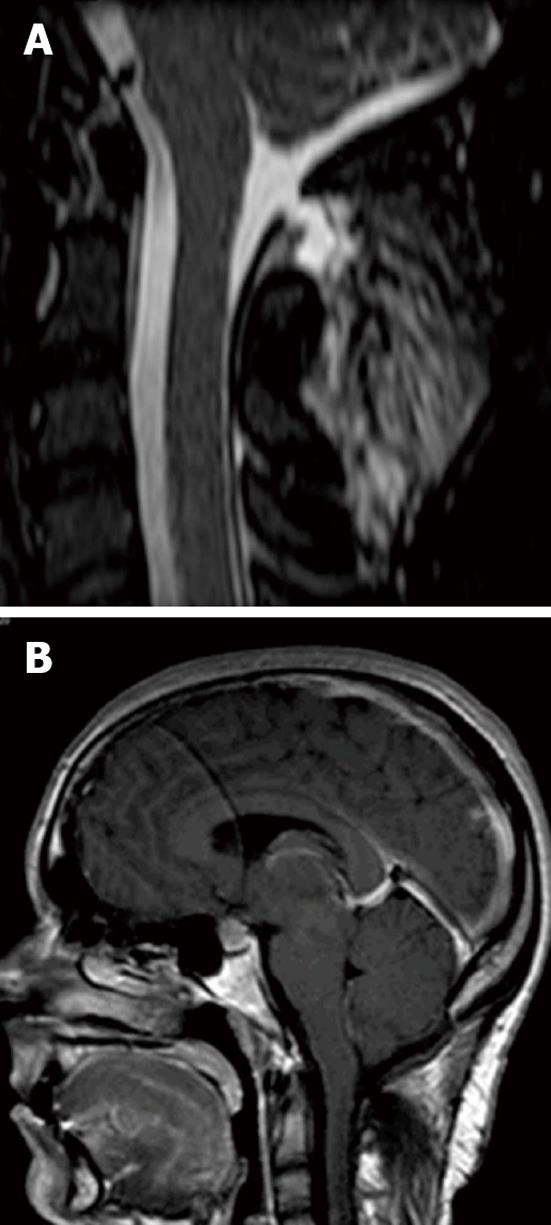
Intracranial hypotension syndrome (IHS) is a rare disorder characterized by a decrease in cerebrospinal fluid pressure to less than 60 mm H2O. The syndrome is associated with occipital headache radiating to the frontal and temporal zones. The current clinical case describes the manifestation of IHS in a twenty-five year old female with a history of suboccipital craniectomy due to Chiari I malformation nine years earlier. The patient was admitted to the hospital complaining about postural, mainly occipital, headache during the last three months, aggravated by being in an upright position. The magnetic resonance imaging (MRI) revealed engorgement of the dural venous sinuses, significant enlargement of the pituitary gland and download displacement or sagging of the brain with effacement of the perichiasmatic cisterns and the prepontine cistern, while the spinal T2W MRI revealed a 7 mm × 2.5 mm dural defect with an extradural cerebrospinal fluid collection at the dorsal soft tissues of the cervical spine. The previous imaging did not reveal subdural effusions.
Core tip: A 25-year-old female presented with a history of suboccipital craniectomy due to Chiari I malformation nine years earlier. The patient was admitted to the hospital with symptoms of postural, mainly occipital, headache during the last three months, aggravated by being in an upright position. The spinal T2W magnetic resonance imaging revealed a 7 mm × 2.5 mm dural defect with an extradural cerebrospinal fluid collection at the dorsal soft tissues of the cervical spine. The current clinical case indicates that a longer follow-up and increased alertness are required in a patient with a history of craniectomy due to Chiari I malformation.
- Citation: Barkoula D, Bontozoglou N, Gatzonis S, Sakas D. Intracranial hypotension syndrome in a patient due to suboccipital craniectomy secondary to Chiari type malformation. World J Clin Cases 2013; 1(9): 295-297
- URL: https://www.wjgnet.com/2307-8960/full/v1/i9/295.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v1.i9.295
Intracranial hypotension syndrome (IHS) is a rare disorder characterized by a decrease in cerebrospinal fluid pressure. IHS is associated with occipital headache similar to the orthostatic headache after lumbar puncture. They both radiate to the frontal and temporal zones and are aggravated in an upright position. HIS is also characterized by dural thickening and pachymeningeal contrast enhancement as a consequence of decreased cerebrospinal fluid (CSF) volume. Although spinal cerebrospinal fluid leaks may be the cause of this syndrome, only a few clinical or radiological cases have been reported.
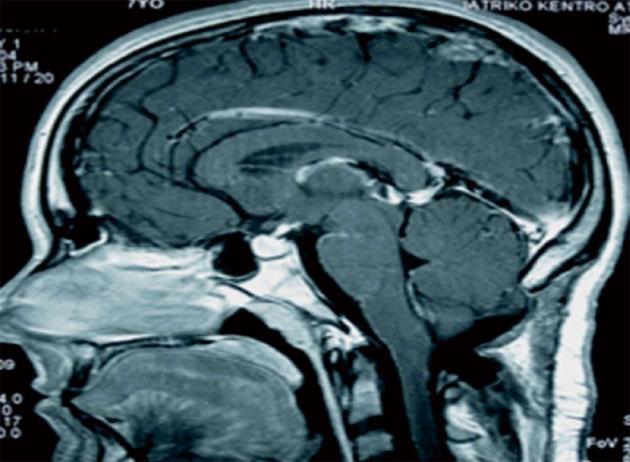
A 25-year-old female presented with a history of suboccipital craniectomy due to Chiari I malformation 9 years earlier. The patient was admitted to the hospital complaining about postural, mainly occipital, headache during the last three months. The headache was aggravated by being in an upright position. The magnetic resonance imaging (MRI) revealed mild engorgement of the dural venous sinuses, significant enlargement of the pituitary gland and download displacement or sagging of the brain with effacement of the perichiasmatic cisterns and the prepontine cistern (Figure 1B), while the spinal T2W MRI revealed a 7 mm × 2.5 mm dural defect with an extradural CSF collection at the dorsal soft tissues of the cervical spine (Figure 1A). The postoperative MRI nine years earlier revealed significant engorgement of the dural venous sinuses and mild enlargement of the pituitary gland without signs of download displacement or sagging of the brain (Figure 2). Even although the previous imaging did not reveal subdural effusions, the postoperative MRI revealed signs of intracranial hypotension syndrome soon after the suboccipital craniectomy. Nevertheless, the typical clinical symptoms of IHS only manifested three months before the admission of the patient. During the postoperative follow-up, the patient complained of intermittent occipital headaches, mostly explained by the Chiari malformation.
IHS is a rare disorder with a prevalence of about 1 per 50000 population[1]. The latest studies indicate that the estimated incidence is higher because the disorder remains under recognized[2]. This rare syndrome is characterized by a decrease in cerebrospinal fluid pressure to less than 60 mm H2O. IHS is associated with occipital headache radiating to the frontal and temporal zones, dural thickening and pachymeningeal contrast enhancement as a consequence of decreased CSF volume. The 5 characteristic imaging features of spontaneous intracranial hypotension visible on MRI are: (1) subdural fluid collections; (2) enhancement of the pachymeninges; (3) engorgement of venous structures; (4) pituitary hyperemia; and (5) sagging of the brain (mnemonic: SEEPS)[3]. Headache due to IHS is similar to the orthostatic headache after lumbar puncture. They both are aggravated in an upright position. ISH is highly related to a spontaneous CSF leak. In most cases, spinal cerebrospinal fluid leaks are related to the pathogenic mechanism of the syndrome. Nevertheless, they have rarely been demonstrated radiographically or surgically[1]. Some of the spontaneous CSF leaks are related to weakness of the meningeal sac, likely in connection with a connective tissue abnormality[4]. In clinical practice, the 2004 International Classification of Headache Disorders criteria cannot satisfy 100% of patients with HIS because of the variability of clinical and radiological manifestations[5]. Furthermore, although both intracranial hypotension syndrome and Chiari I malformation have been well described, their simultaneous presence has rarely been reported[6]. The current case indicates that even although the patient’s postoperative MRI revealed signs of IHS, the clinical features were intermittent and did not meet the IHS criteria. Therefore, a patient with a history of Chiari I malformation and intermittent occipital headache after craniectomy requires increased alertness and a longer follow-up.
A 25-year-old female presented with a history of suboccipital craniectomy due to Chiari I malformation nine years earlier.
The patient was admitted to the hospital complaining of postural, mainly occipital, headache during the last three months. The headache was aggravated in an upright position.
The magnetic resonance imaging (MRI) revealed engorgement of the dural venous sinuses, significant enlargement of the pituitary gland and download displacement or sagging of the brain with effacement of the perichiasmatic cisterns and the prepontine cistern, while the spinal T2W MRI revealed a 7 mm × 2.5 mm dural defect with an extradural cerebrospinal fluid collection at the dorsal soft tissues of the cervical spine.
The spinal T2W magnetic resonance imaging revealed a 7 mm × 2.5 mm dural defect with an extradural cerebrospinal fluid collection at the dorsal soft tissues of the cervical spine.
Latest studies indicate that the estimated incidence is higher because the disorder remains under recognized.
A patient with a history of Chiari I malformation and intermittent occipital headache after craniectomy requires increased alertness and a longer follow- up.
This clinical association is very rare and a larger number of patients are needed in order to have a wide clinical picture.
| 1. | Schievink WI, Meyer FB, Atkinson JL, Mokri B. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. J Neurosurg. 1996;84:598-605. [PubMed] |
| 2. | Anderson J, Corkill R. Spontaneous intracranial hypotension: clinical features in eight cases. J Neurol Neurosurg Psychiatry. 2013;84:e2. |
| 3. | Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA. 2006;295:2286-2296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 667] [Cited by in RCA: 727] [Article Influence: 36.4] [Reference Citation Analysis (0)] |
| 4. | Mokri B. Spontaneous intracranial hypotension. Curr Pain Headache Rep. 2001;5:284-291. [PubMed] |
| 5. | Schievink WI, Dodick DW, Mokri B, Silberstein S, Bousser MG, Goadsby PJ. Diagnostic criteria for headache due to spontaneous intracranial hypotension: a perspective. Headache. 2011;51:1442-1444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 98] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 6. | Atkinson JL, Weinshenker BG, Miller GM, Piepgras DG, Mokri B. Acquired Chiari I malformation secondary to spontaneous spinal cerebrospinal fluid leakage and chronic intracranial hypotension syndrome in seven cases. J Neurosurg. 1998;88:237-242. [PubMed] |
P- Reviewers: Juan DS, Rodrigues MG S- Editor: Zhai HH L- Editor: Roemmele A E- Editor: Yan JL