Published online Dec 16, 2013. doi: 10.12998/wjcc.v1.i9.285
Revised: November 5, 2013
Accepted: November 18, 2013
Published online: December 16, 2013
Processing time: 89 Days and 17.7 Hours
Typically situated posterolateral in the spinal canal, intraspinal facet cysts often cause radicular symptoms. Rarely, the midline location of these synovial or ganglion cysts may cause thecal sac compression leading to neurogenic claudication or cauda equina syndrome. This article summarizes the clinical presentation, radiographic appearance, and management of three intraspinal, midline facet cysts. Three patients with symptomatic midline intraspinal facet cysts were retrospectively reviewed. Documented clinical visits, operative notes, histopathology reports, and imaging findings were investigated for each patient. One patient presented with neurogenic claudication while two patients developed partial, subacute cauda equina syndrome. All 3 patients initially responded favorably to lumbar decompression and midline cyst resection; however, one patient required surgical stabilization 8 mo later. Following the three case presentations, we performed a thorough literature search in order to identify articles describing intraspinal cystic lesions in lateral or midline locations. Midline intraspinal facet cysts represent an uncommon cause of lumbar stenosis and thecal sac compression. Such entities should enter the differential diagnosis of midline posterior cystic lesions. Midline cysts causing thecal sac compression respond favorably to lumbar surgical decompression and cyst resection. Though laminectomy is a commonly performed operation, stabilization may be required in cases of spondylolisthesis or instability.
Core tip: Midline, intraspinal cysts arise from facet joint degeneration. The lesions represent an important and often over-looked cause of back pain and other neurological symptoms. Radiographic identification of the fluid-filled sacs is particularly important in the setting of cauda equina syndrome, in which immediate surgical intervention is required in order to address the compressive lesion. Although the treatment of choice is a spinal decompression and resection, posterior fusions may prevent cyst recurrence.
- Citation: Pindrik J, Macki M, Bydon M, Maleki Z, Bydon A. Midline synovial and ganglion cysts causing neurogenic claudication. World J Clin Cases 2013; 1(9): 285-289
- URL: https://www.wjgnet.com/2307-8960/full/v1/i9/285.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v1.i9.285
Intraspinal facet cysts, also known as synovial and/or ganglion cysts, typically reside adjacent to the facet joints and may cause radicular symptoms due to nerve root compression and foraminal compromise. Representing a zygapophyseal joint, facet joints lie enclosed within a capsule lined by synovial epithelium[1]. Breakdown of this articular lining or encapsulated accumulation of fluid outside of the facet joint may lead to pathologic cyst formation. Synovial and ganglion cysts typically occur in the lower lumbar region, frequently the site of degenerative changes and dynamic instability[1-5]. They are found in the postero-lateral region of the canal, consistent with their source of pathology. Lined with cuboidal epithelium and filled with synovial fluid, synovial cysts frequently retain communication with their facet joint of origin[4,6]. In contrast, ganglion cysts lack synovial lining and structural communication to facet joints[3,6]. Ganglion cysts contain a collagenous or fibrous wall encircling gelatinous or myxoid substance[4,7-9]. Clinically, however, both terms are used interchangeably to describe intraspinal facet cysts or juxtafacet cysts[2-4,7,9]. This article presents 3 unique cases of midline intraspinal facet cysts causing significant lumbar stenosis and symptomatic thecal sac compression.
Three patients with symptomatic midline intraspinal facet cysts were reviewed. Clinical visits, operative notes, histopathology reports, and imaging findings were investigated for each patient. A thorough literature search was used to identify case reports or series describing intraspinal cystic lesions.
A 65-year-old woman presented with a 1-mo history of bilateral buttock pain and lower extremity weakness. The patient had full strength in her upper extremities and 4/5 strength in her proximal lower extremities. Magnetic resonance imaging (MRI) showed a grade 1 anterior listhesis of L4 on L5 as well as a well-circumscribed midline synovial cyst posterior to the thecal sac at the L4-L5 level; the hyperintense lesion on T2 weighted sequences measured approximately 8 mm × 8 mm × 10 mm. Differential diagnosis includes perineural (Tarlov) cysts, arachnoid cysts, and migrated disc fragment. The patient underwent bilateral laminectomies at L4-L5, bilateral foraminotomies, medial facetectomies, and cyst resection. Smaller cysts were encountered at the bilateral L4-L5 and the right L5-S1 facet joints. Histologic sections of the excised midline cyst revealed fragments of dense connective tissue with overlying synovium. The patient had an uncomplicated post-operative course and remained asymptomatic at 15-mo follow up.
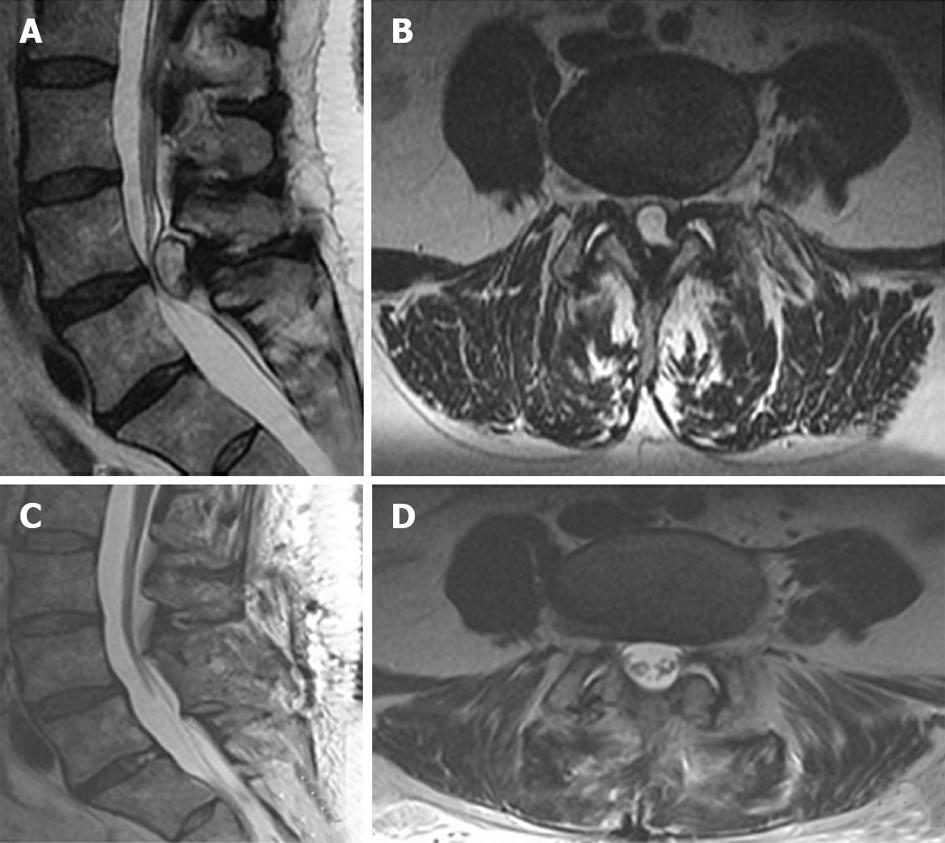
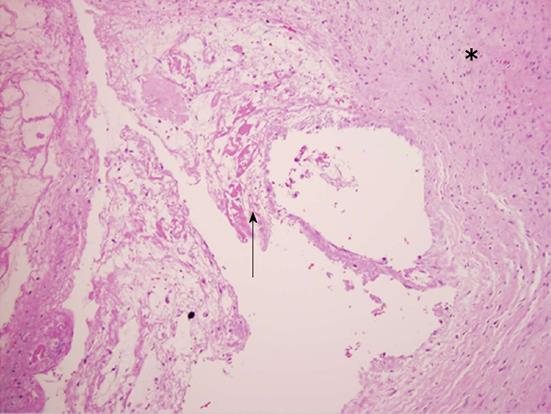
A 57-year-old woman presented with a 3-mo history of lower back, left lower extremity radiculopathy in the L5 and S1 distributions, and urinary incontinence. She exhibited full strength in the bilateral upper and lower extremities, with an unremarkable sensory exam. MRI revealed a large midline, well-circumscribed cystic lesion at the L4-L5 level, causing significant compression of the thecal sac and cauda equine; however, the images were unremarkable for spinal instability (Figure 1A and B). The patient underwent L4-L5 bilateral decompressive laminectomies with bilateral foraminotomies and cyst resection. Intraoperatively, a large intraspinal extradural cystic lesion appeared centrally, exerting significant compression on the thecal sac. While gross inspection revealed a cystic lesion containing clear viscous fluid, absence of epithelium lining the cystic cavity microscopic examination confirmed the final diagnosis of a ganglion cyst (Figure 2). The patient did well post-operatively. Imaging confirmed total cyst resection and adequate decompression of the thecal sac (Figure 1C and D). The patient reported improvement in all symptoms, including urinary incontinence, at her latest follow-up 17-mo post-operatively.
A 70-year-old woman presented with a 1-mo history of bilateral buttock and lower extremity pain. The patient denied bowel or bladder incontinence. On examination, she was neurologically stable. MRI revealed multilevel lumbar spondylosis as well as a large multiseptated cystic lesion appearing centrally and dorsolaterally in the L4-L5 extra-dural space with subsequent severe canal stenosis, without foraminal compromise. The patient underwent with bilateral L3-L5 laminectomies, medial facetectomies, and cyst resection. Gross inspection of the excised midline lesion revealed a cystic structure. Histologic examination of specimen permanent sections was consistent with a ganglion cyst. The patient had an uncomplicated post-operative course. A post-operative MRI demonstrated complete removal of the ganglion cyst with posterior decompression from L3-L5. The patient remained well until 3 mo after surgery when she developed low back, right buttock, and right anterior thigh pain. Epidural and facet injections were tried without symptomatic relief. Given the findings of junctional stenosis at L2 and mechanical instability suggested by imaging and clinical evaluation, the patient underwent L2-L5 bilateral, instrumented fusion eight months later. At last follow-up, the patient was completely asymptomatic (total follow-up period: 15 mo).
Juxtafacet cysts may reside deep or superficial to the posterior elements of the vertebral canal, or have a bi-lobed architecture existing in both compartments[7]. Intraspinal facet cysts usually neighbor degenerated facet joints in the postero-lateral epidural space[1-3,5,7,10]. The cysts most frequently occur at L4-L5, the lumbar level characterized by greatest mobility and prevalence of degenerative disease[4,7,9,11-13].
Imaging characteristics of intraspinal facet cysts vary depending on cyst content. Computed tomography (CT) typically portrays a well circumscribed hypodense lesion with hyperdense rim due to calcification[9,10]. MRI typically shows hyperintense cystic extradural lesions. The cysts appear centrally iso- to hyperintense compared to cerebrospinal fluid (CSF) and iso- to hypointense compared to soft tissue on T1 weighted sequences[1,4,6,7,10,14]. Facet arthropathy and degenerative spondylosis frequently accompany juxtafacet cysts on CT or MRI[2,3,7,9,10].
Clinically indistinguishable, histopathologic analysis distinguishes synovial from ganglion cysts. The presence of cuboidal synovial epithelium encircling synovial fluid corroborates the diagnosis of a synovial cyst. In contrast, the absence of synovial epithelial lining or the presence of chronic fibrotic tissue along the cavity wall supports the diagnosis of a ganglion cyst[4,7,8,11].
Several mechanisms have been described to explain the development of juxtafacet cysts. Ganglion cysts most likely result from cystic or myxoid degeneration of connective tissue. The most likely mechanism of synovial cyst formation involves degenerative articular changes due to abnormal and increased motion at the facet joint[4,6,9,11]. Several studies have described associations between spinal instability or degenerative changes, reflected by lumbar spondylosis or spondylolisthesis, and intraspinal facet cysts[11,12]. Acquired defects in the joint capsule allow protrusion of synovial epithelium and cyst formation adjacent to the joint; hence, the communication between degenerated facet joints and synovial cysts found in many cases[4,9]. Furthermore, juxtafacet cysts occur most frequently at the level of greatest motion and prevalence of degenerative changes, L4-5, followed by L5-S1 and L3-4[4,9,11-13].
In the absence of neurologic deficits, symptomatic patients with intraspinal facet cysts may benefit from conservative management. Non-surgical treatments include activity restrictions, supportive bracing, oral analgesics or anti-inflammatories, physical therapy, and epidural or facet steroid injections[7,11,12]. Minimally invasive procedures include percutaneous injection or cyst aspiration[4,11,12]. However, failure of conservative measures has been widely documented by several clinical series[6,10-12]. Standard surgical techniques include hemilaminotomy or laminectomy, foraminotomy, medial facetectomy, and cyst excision[2,4,6,10-12].
Most clinical series demonstrate moderate to high rates of successful outcomes in patients undergoing decompressive surgery with juxtafacet cyst resection[6,10,12]. Epstein reported good to excellent results in 58%-63% of patients undergoing decompressive surgery for synovial cysts and accompanying stenosis, with or without spondylolisthesis[10]. Most other clinical series report similar or even higher rates of favorable outcomes[10]. In their meta-analysis, Bydon et al[12] reported short-term post-operative resolution of back and lower extremity pain in above 90% of patients compiled. In prolonged follow-up, nearly 22% and 13% of patients reported recurrent back pain and radiculopathy, respectively. Delayed surgical complications include intraspinal facet cyst recurrence and the development or progression of spinal mechanical instability[11,12]. Static or dynamic imaging may reveal low grade spondylolisthesis or minimal instability in a minority of asymptomatic patients[6].
In the present case series, one patient demonstrated clinical and radiographic evidence of post-operative spinal instability and required an instrumented fusion at 8 mo follow-up. Such outcomes speak to the role of spinal fusion as an adjunct to decompression and cyst excision given the likely role of facet joint hypermobility and degeneration in the pathophysiology of synovial cyst formation[10-13]. While potentially improving mechanical back pain, concomitant spinal fusion may limit further destabilization and prevent cyst recurrence[6,11-13]. Although current studies reflect the predominance of decompression and cyst excision without fusion in the majority (> 80%) of surgical cases for synovial cysts[12], patients with clinical and radiographic evidence of post-operative spinal instability may benefit from concomitant surgical fixation and/or fusion[6,10-12]. Some authors suggest that radiographic indications for pre-operative spinal instability, such as spondylolisthesis, are the strongest predictor for post-operative instability, especially after spinal decompression[15-19]. However, patients without pre-operative spondyolisthesis may still develop post-operative spinal instability requiring a fusion, as demonstrated in case number three. Furthermore, same level cyst recurrence occurred in nearly 2% of patients, all following decompression and cyst resection alone. In contrast, cyst reformation did not occur in any patients following concomitant spinal fusion[12]. These findings stress the importance of considering concomitant spinal fusion with decompression and synovial cyst excision.
Lessons learned from this case series in that despite their rare occurrence, midline synovial and ganglion cysts should be considered in the differential diagnosis of centrally located posterior extradural cysts. When causing symptomatic lumbar stenosis and thecal sac compression, midline synovial and ganglion cysts may require decompressive laminectomy and resection to relieve patients’ symptoms and restore neurologic function. In the setting of baseline back pain or radiographically proven mechanical instability, concomitant spinal fusion may be considered. Following decompression and cyst excision alone, patients should be monitored closely for the progression or development of mechanical instability.
In this manuscript, we present a unique presentation of symptomatic, intraspinal cysts. Following the cyst recurrence, lumbar fusion may prevent long-term spinal instability or cyst recurrence. However, we do recognize that our manuscript is a limited case series of three patients. Larger cohorts are required to delineate the clinical outcomes in patients with midline synovial and ganglion cysts.
The authors thank the Johns Hopkins Hospital Department of Pathology for their assistance with collecting, preparing, and reviewing specimens sent from the operating room.
Three patients with symptomatic midline intraspinal facet cysts were retrospectively reviewed. Documented clinical visits, operative notes, histopathology reports, and imaging findings were investigated for each patient.
One patient presented with neurogenic claudication while two patients developed partial, subacute cauda equina syndrome.
All 3 patients initially responded favorably to lumbar decompression and midline cyst resection; however, one patient required surgical stabilization 8 mo later.
Radiographic identification of the fluid-filled sacs is particularly important in the setting of cauda equina syndrome, in which immediate surgical intervention is required in order to address the compressive lesion.
All 3 patients initially responded favorably to lumbar decompression and midline cyst resection; however, one patient required surgical stabilization 8 mo later.
Some authors suggest that radiographic indications for pre-operative spinal instability, such as spondylolisthesis, are the strongest predictor for post-operative instability, especially after spinal decompression
The authors present a unique presentation of symptomatic, intraspinal cysts. Following the cyst recurrence, lumbar fusion may prevent long-term spinal instability or cyst recurrence.
This manuscript illustrates a unique presentation, location, and management of intraspinal cysts. The article is well-written and does not require modifications.
| 1. | Gheyi VK, Uppot RN, Flores C, Koyfman YU. Unusual case of lumbar synovial cyst. Clin Imaging. 1999;23:394-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Indar R, Tsiridis E, Morgan M, Aldham CH, Hussein AA. Intraspinal lumbar synovial cysts: diagnosis and surgical management. Surgeon. 2004;2:141-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Howling SJ, Kessel D. Case report: acute radiculopathy due to a haemorrhagic lumbar synovial cyst. Clin Radiol. 1997;52:73-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Tatter SB, Cosgrove GR. Hemorrhage into a lumbar synovial cyst causing an acute cauda equina syndrome. Case report. J Neurosurg. 1994;81:449-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 67] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Nakayama S, Fujino H, Inomori S, Shuto T, Basugi N, Kuwabara T. [A case of a lumbar spinal synovial cyst located on the midline]. No Shinkei Geka. 1998;26:717-722. [PubMed] |
| 6. | Landi A, Marotta N, Tarantino R, Ruggeri AG, Cappelletti M, Ramieri A, Domenicucci M, Delfini R. Microsurgical excision without fusion as a safe option for resection of synovial cyst of the lumbar spine: long-term follow-up in mono-institutional experience. Neurosurg Rev. 2012;35:245-53; discussion 253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Hsu KY, Zucherman JF, Shea WJ, Jeffrey RA. Lumbar intraspinal synovial and ganglion cysts (facet cysts). Ten-year experience in evaluation and treatment. Spine (Phila Pa 1976). 1995;20:80-89. [PubMed] |
| 8. | Chan AP, Wong TC, Sieh KM, Leung SS, Cheung KY, Fung KY. Rare ligamentum flavum cyst causing incapacitating lumbar spinal stenosis: Experience with 3 Chinese patients. J Orthop Surg Res. 2010;5:81. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Wait SD, Jones FD, Lonser RR, Lee KS. Symptomatic epidural hematoma caused by lumbar synovial cyst rupture: report of two cases and review of the literature. Neurosurgery. 2005;56:E1157; discussion E1157. [PubMed] |
| 10. | Epstein NE. Lumbar laminectomy for the resection of synovial cysts and coexisting lumbar spinal stenosis or degenerative spondylolisthesis: an outcome study. Spine (Phila Pa 1976). 2004;29:1049-1555; discussion 1056. [PubMed] |
| 11. | Khan AM, Girardi F. Spinal lumbar synovial cysts. Diagnosis and management challenge. Eur Spine J. 2006;15:1176-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 92] [Article Influence: 4.6] [Reference Citation Analysis (1)] |
| 12. | Bydon A, Xu R, Parker SL, McGirt MJ, Bydon M, Gokaslan ZL, Witham TF. Recurrent back and leg pain and cyst reformation after surgical resection of spinal synovial cysts: systematic review of reported postoperative outcomes. Spine J. 2010;10:820-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 101] [Article Influence: 6.3] [Reference Citation Analysis (1)] |
| 13. | Xu R, McGirt MJ, Parker SL, Bydon M, Olivi A, Wolinsky JP, Witham TF, Gokaslan ZL, Bydon A. Factors associated with recurrent back pain and cyst recurrence after surgical resection of one hundred ninety-five spinal synovial cysts: analysis of one hundred sixty-seven consecutive cases. Spine (Phila Pa 1976). 2010;35:1044-1053. [PubMed] |
| 14. | Antonini A, Pilleri M, Padoan A, Landi A, Ferla S, Biundo R, D’Avella D. Successful subthalamic stimulation in genetic Parkinson’s disease caused by duplication of the α-synuclein gene. J Neurol. 2012;259:165-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Schnake KJ, Schaeren S, Jeanneret B. Dynamic stabilization in addition to decompression for lumbar spinal stenosis with degenerative spondylolisthesis. Spine (Phila Pa 1976). 2006;31:442-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 152] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 16. | Feffer HL, Wiesel SW, Cuckler JM, Rothman RH. Degenerative spondylolisthesis. To fuse or not to fuse. Spine (Phila Pa 1976). 1985;10:287-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 80] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Suk SI, Lee CK, Kim WJ, Lee JH, Cho KJ, Kim HG. Adding posterior lumbar interbody fusion to pedicle screw fixation and posterolateral fusion after decompression in spondylolytic spondylolisthesis. Spine (Phila Pa 1976). 1997;22:210-29; discussion 210-29;. [PubMed] |
| 18. | Schaeren S, Broger I, Jeanneret B. Minimum four-year follow-up of spinal stenosis with degenerative spondylolisthesis treated with decompression and dynamic stabilization. Spine (Phila Pa 1976). 2008;33:E636-E642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 131] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 19. | GILL GG, MANNING JG, WHITE HL. Surgical treatment of spondylolisthesis without spine fusion; excision of the loose lamina with decompression of the nerve roots. J Bone Joint Surg Am. 1955;37-A:493-520. [PubMed] |
P- Reviewer: Bydon A S- Editor: Zhai HH L- Editor: A E- Editor: Yan JL