Published online Jun 16, 2013. doi: 10.12998/wjcc.v1.i3.124
Revised: April 5, 2013
Accepted: May 9, 2013
Published online: June 16, 2013
Processing time: 161 Days and 9.3 Hours
Colonic lipomas are submucosal nonepithelial tumors covered by intact or eroded mucosa. In rare cases, alterations in the mucosa covering a lipoma include hyperplasia, adenoma, atrophy, ulceration, and necrosis. Here, we report a case of a colonic lipoma covered by hyperplastic epithelium in a 68-year-old woman. Based on the colonoscopy findings, a snare polypectomy was performed for a presumptive diagnosis of an epithelial lesion; however, the histological examination revealed a colonic submucosal lipoma with overlying hyperplastic epithelium.
Core tip: we report a rare case of a colonic lipoma with overlying hyperplastic epithelium. Removing an asymptomatic colonic lipoma is not necessary, as it may have no clinical significance. However, treatment plans for colonic lipomas might be reconsidered as transformation of the mucosa lining of a lipoma could occur in small and asymptomatic lesions.
- Citation: Yeom JO, Kim SY, Jang EC, Yu JY, Chang ED, Cho YS. Colonic lipoma covered by hyperplastic epithelium: Case report. World J Clin Cases 2013; 1(3): 124-127
- URL: https://www.wjgnet.com/2307-8960/full/v1/i3/124.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v1.i3.124
Lipomas are generally rare, but are the most common nonepithelial benign tumors of the gastrointestinal tract. Colonic lipomas are uncommon mesenchymal neoplasms, with a reported incidence of 0.2%-4.4%[1]. Colonic lipomas are usually asymptomatic and detected incidentally at colonoscopy, radiological investigation, surgery, or autopsy. The most common colonoscopic finding is a smooth, slightly yellow, spherical polyp, that is usually sessile and rarely pedunculated, with intact overlying mucosa[2]. In rare cases, the mucosa covering a lipoma shows alterations such as hyperplasia[3,4], atrophy[5], adenomatous changes[6,7], and necrosis and/or ulcerations[8-10]. We herein report a case of colonic lipoma covered with hyperplastic epithelium in a 68-year-old woman and review the literature pertaining to this condition.
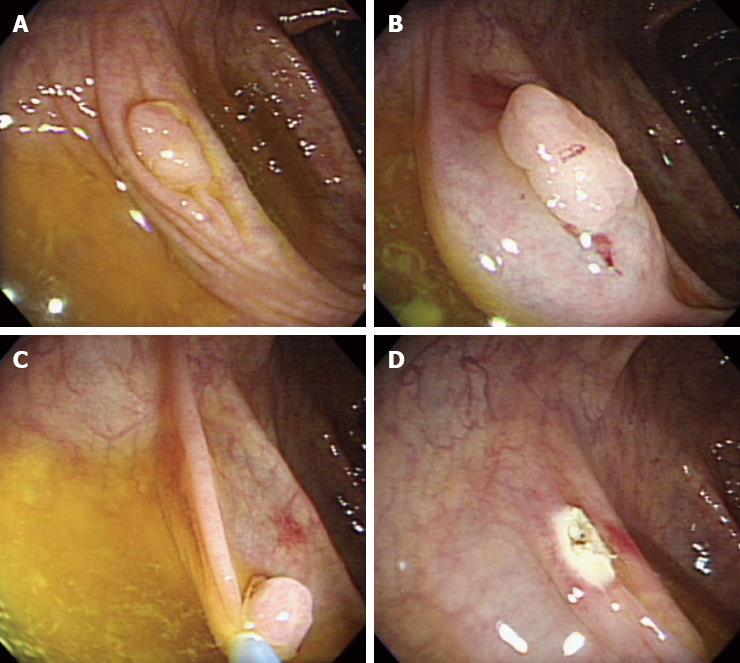
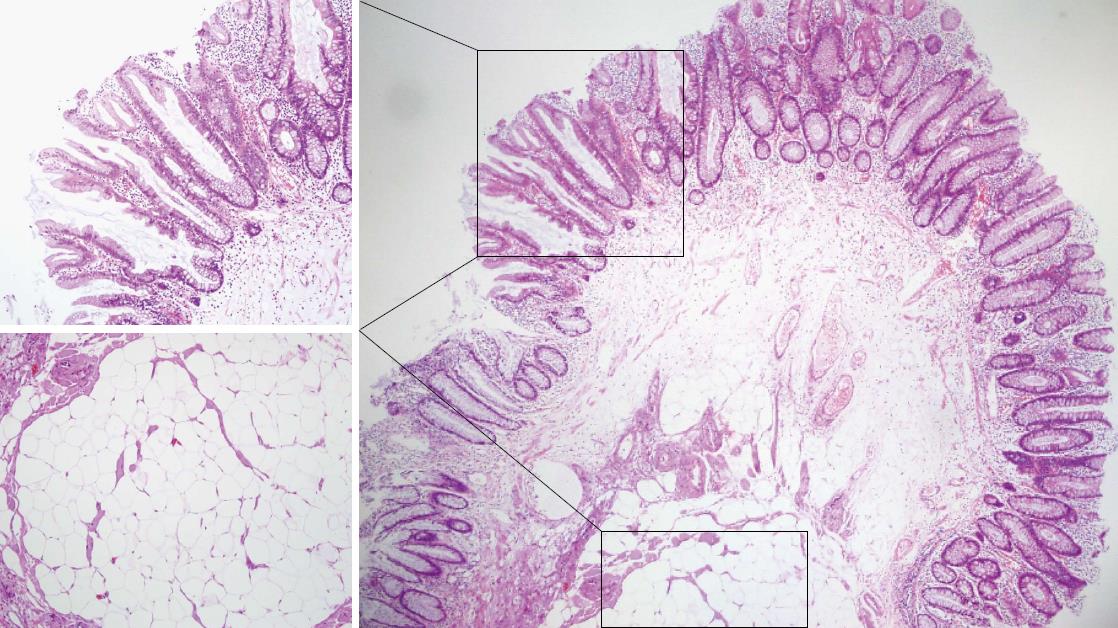
A 68-year-old woman with abdominal discomfort for several weeks was referred to our department by a private internist for further investigation of a 9 mm polyp in the ascending colon that was revealed during a barium enema for the evaluation of symptom. She denied constipation, diarrhea, hematochezia, or melena. Her physical examination and medical history were unremarkable. All laboratory examinations, including complete peripheral blood cell counts, blood biochemistry, and carcinoembryonic antigen levels were within normal ranges. Colonoscopy revealed a sessile polyp about 9 mm in diameter in the ascending colon (Figure 1). We resected the polyp using a endoscopic mucosal resection (EMR) after a saline solution injection. No procedural-related complications were observed. A histopathological examination revealed a tumor composed of adipose tissue covered by hyperplastic and serrated epithelium consisting of columnar and goblet cells (Figure 2). The patient has been followed closely and has shown no recurrence. A follow-up colonoscopy revealed no remarkable findings 6 mo after the EMR.
Colonic lipomas are benign, slow growing tumors of mesenchymal origin that rarely cause symptoms and are usually detected incidentally[1,11]. The most common sites of colonic lipomas are the cecum, ascending colon, and sigmoid colon, in decreasing frequency. These benign tumors arise from the submucosal layer in approximately 90% of cases and from the subserosal or intermucosal layer in the remaining cases[2]. Pathologically, lipomas are composed of well-circumscribed, mature adipose tissue with varying amounts of fibrous stroma covered with intact colonic mucosa[1,2,11].
Diagnostic tools for colonic lipomas include colonoscopy, computed tomography, barium enema, and endoscopic ultrasonography. Among these, colonoscopy allows direct visualization of a colonic lipoma. Lipomas are seen as smooth, slightly yellow, rounded polyps with a thick stalk or broad-based attachment[2]. Characteristic features include the “tenting sign” (grasping the overlying mucosa), the “pillow sign” (pressing forceps against the lesion results in depression or pillowing of the mass), and the “naked fat sign” (extrusion of yellowish fat after biopsy)[1,2,11]. The current case did not show these three characteristic features of a lipoma but the morphology of an epithelial lesion such as hyperplastic polyp or sessile serrated adenoma. The resected specimen was a submucosal lipoma and the covering epithelium was hyperplastic, resembling a hyperplastic polyp. The epithelium was serrated and comprised of both columnar and goblet cells, but lacking atypia or mitotic activity. To the best of our knowledge the association of lipoma and hyperplastic polyp has been reported only once. Radhi et al[3] showed a large lipoma in the sigmoid colon with overlying hyperplastic epithelium that was detected during an operation in a patient with diverticulitis. It was unclear whether the co-occurrence of these entities was coincidental or correlated. Hyperplastic polyps have been considered non-neoplastic lesions without malignant potential for many years. However, recent studies have shown that some hyperplastic polyps possess molecular features similar to those of colorectal carcinomas[12,13]. Several subtypes of serrated polyps, such as sessile serrated adenomas, traditional serrated adenomas, and mixed polyps, have been proposed to be colorectal carcinoma precursors. In addition to hyperplastic changes of the epithelium lining in a lipoma, rare cases of adenomatous transformation have been reported[6,7]. It is speculated that chronic trauma due to the passage of stools may lead to hyperplasia and adenomatous transformation of overlying mucosa[7]. In rare cases, the colonoscopy may reveal ulcerations, a finding that may lead to a mistaken diagnosis of adenocarcinoma[8-10].
Although most lipomas require no treatment, a small subgroup requires surgical intervention, including those with suspected malignancy, symptomatic lipomas, surgical emergencies such as intussusception, and obstruction with ulceration and bleeding[1,2,11]. Colonic lipomas < 2 cm can be safely removed endoscopically, whereas larger lesions should be removed by segmental resection[1,2,14]. In the present case, the polyp was initially suspected as a small epithelial lesion based on the colonoscopic findings and was resected endoscopically.
In conclusion, we report a rare case of a colonic lipoma with overlying hyperplastic epithelium. Removing an asymptomatic colonic lipoma is not necessary, as it may have no clinical significance. However, treatment plans for colonic lipomas might be reconsidered as transformation of the mucosa lining of a lipoma could occur in small and asymptomatic lesions.
| 1. | Vecchio R, Ferrara M, Mosca F, Ignoto A, Latteri F. Lipomas of the large bowel. Eur J Surg. 1996;162:915-919. [PubMed] |
| 2. | Bardají M, Roset F, Camps R, Sant F, Fernández-Layos MJ. Symptomatic colonic lipoma: differential diagnosis of large bowel tumors. Int J Colorectal Dis. 1998;13:1-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 34] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Radhi JM, Haig TH. Lipoma of the colon with overlying hyperplastic epithelium. Can J Gastroenterol. 1997;11:694-695. [PubMed] |
| 4. | Franc-Law JM, Bégin LR, Vasilevsky CA, Gordon PH. The dramatic presentation of colonic lipomata: report of two cases and review of the literature. Am Surg. 2001;67:491-494. [PubMed] |
| 5. | Petrozza V, Passaro V, De Salazar C, Pulvirenti S, Riccardelli F, Magliocca FM. [An anatomicoclinical case of lipoma of the sigmoid]. Minerva Chir. 1994;49:89-94. [PubMed] |
| 6. | Lancet F, Alberti LE, Alberti-Flor JJ. Diminutive colon polyp coexisting with a large lipoma: an endoscopic ‘rarity’. Can J Gastroenterol. 2004;18:178. [PubMed] |
| 7. | Capra F, Zorcolo L, Scintu F, Mascia R, Casula G. Giant sigmoid lipoma covered by a villous adenoma. Int J Colorectal Dis. 2007;22:563-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Meghoo CA, Cook PR, McDonough CA, Bowser LK, Waddell BE. Large colonic lipoma with mucosal ulceration mimicking carcinoma. Gastrointest Endosc. 2003;58:468-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (1)] |
| 9. | Katsinelos P, Chatzimavroudis G, Zavos C, Pilpilidis I, Lazaraki G, Papaziogas B, Paroutoglou G, Kountouras J, Paikos D. Cecal lipoma with pseudomalignant features: a case report and review of the literature. World J Gastroenterol. 2007;13:2510-2513. [PubMed] |
| 10. | El-Khalil T, Mourad FH, Uthman S. Sigmoid lipoma mimicking carcinoma: case report with review of diagnosis and management. Gastrointest Endosc. 2000;51:495-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | McGrew W, Dunn GD. Colonic lipomas: clinical significance and management. South Med J. 1985;78:877-879. [PubMed] |
| 12. | Yano Y, Konishi K, Yamochi T, Katagiri A, Nozawa H, Suzuki H, Toyota M, Kubota Y, Muramoto T, Kobayashi Y. Clinicopathological and molecular features of colorectal serrated neoplasias with different mucosal crypt patterns. Am J Gastroenterol. 2011;106:1351-1358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Jass JR, Baker K, Zlobec I, Higuchi T, Barker M, Buchanan D, Young J. Advanced colorectal polyps with the molecular and morphological features of serrated polyps and adenomas: concept of a ‘fusion’ pathway to colorectal cancer. Histopathology. 2006;49:121-131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 187] [Cited by in RCA: 188] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 14. | Pfeil SA, Weaver MG, Abdul-Karim FW, Yang P. Colonic lipomas: outcome of endoscopic removal. Gastrointest Endosc. 1990;36:435-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 71] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
P- Reviewers Ng SSM, Soetikno R, Triantopoulou C S- Editor Zhai HH L- Editor A E- Editor Ma S