Published online May 16, 2013. doi: 10.12998/wjcc.v1.i2.82
Revised: March 7, 2013
Accepted: April 10, 2013
Published online: May 16, 2013
Processing time: 109 Days and 11.7 Hours
Although well recognized for tubo-ovarian abscesses, we report, in our best knowledge, the first case of a vaginal drain of a pelvic abscess due to colonic diverticulitis. A 78-year-old patient presented with abdominal and pelvic pain, fever (39.3 °C) and an elevated white blood cell count (18500/mL). After abdominopelvic computed tomography the patient was presumed to have a pelvic abscess, which developed as a complication of the sigmoid diverticulitis. Due to the numerous intervening structures that create obstacles to safe percutaneous access, we planned a trans-vaginal drain. A rapid recovery was obtained within 2 d from the procedure and, at present, the follow-up was uneventful after 18 mo. We believe that transvaginal drain of pelvic abscess could be a useful alternative, when percutaneous approach is not feasible.
Core tip: Large diverticular abscesses (> 3 cm) should be treated by antibiotics and percutaneous drain. Abscess deep in the pelvis pose a unique problem because numerous intervening structures create obstacles to safe percutaneous access. Transvaginal drain of pelvic abscess could be an useful alternative, when percutaneous approach is not feasible.
- Citation: Milone M, Sosa Fernandez ME, Venetucci P, Maietta P, Sosa Fernandez LM, Taffuri C, Milone F. A vaginal drain of a pelvic abscess due to colonic diverticulitis. World J Clin Cases 2013; 1(2): 82-83
- URL: https://www.wjgnet.com/2307-8960/full/v1/i2/82.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v1.i2.82
Although well recognized for tubo-ovarian abscesses[1,2], we report, in our best knowledge, the first case of a vaginal drain of a pelvic abscess due to colonic diverticulitis.
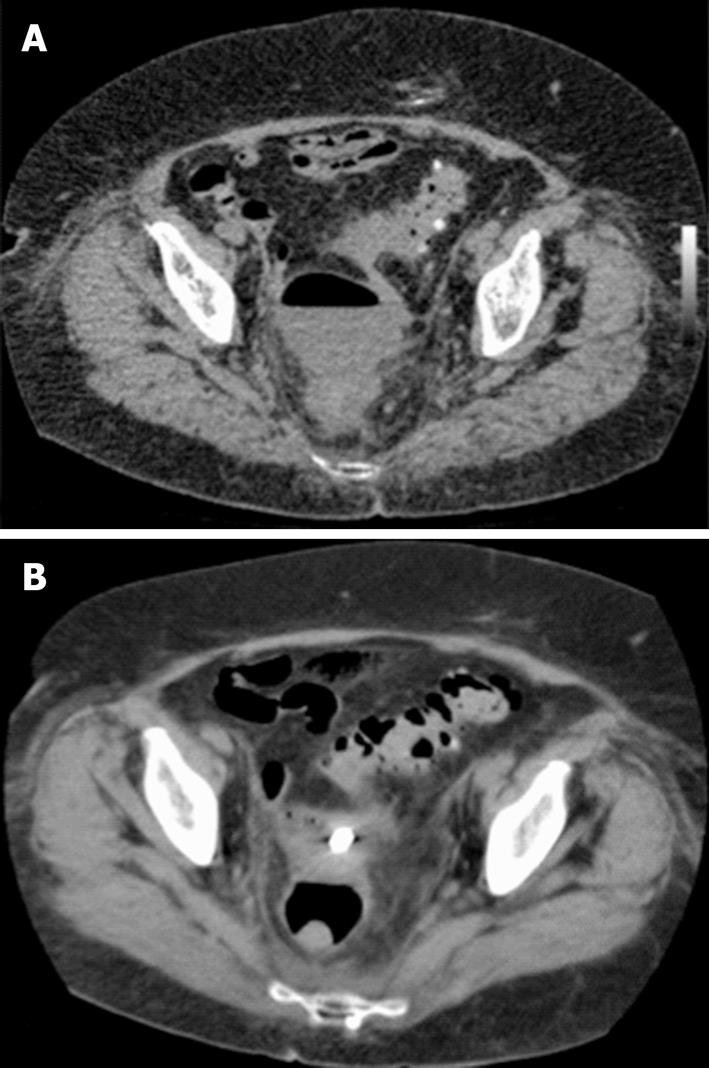
A 78-year-old patient presented with abdominal and pelvic pain. Physical examination demonstrated fever (39.3 °C) and mild tachycardia (120/min) with bilateral lower abdominal quadrant tenderness. Blood analysis revealed an elevated white blood cell count (18500/mL). The abdominopelvic computed tomography scan revealed a left sided collection with a prominent air-fluid level suggesting pelvic abscess, measuring 8 cm × 6 cm, close to the vagina. Multiple diverticula were identified and the sigmoid colon was lying around the collection with its borders that could not be distinguished from the abscess. The mesentery of the sigmoid colon was also found to be thickened due to inflammation (Figure 1).
The patient was presumed to have a pelvic abscess, which developed as a complication of the sigmoid diverticulitis, and, according to guidelines, we planned the drainage of the lesion[3]. However, due to the numerous intervening structures that create obstacles to safe percutaneous access, we planned a trans-vaginal drain.
The endovaginal ultrasound sonography (US) examination was performed using an end-fire endovaginal US probe with an attached needle guide. A puncture needle was introduced into the fluid collection under continuous US guidance and fluid from the cavity was aspirated with a syringe. A guidewire was introduced into the cavity via the puncture needle. Then a self-retaing pigtail catheter with a string lock was introduced over the guide wire into the cavity (Seldinger technique). The catheter was left in situ and irrigated three times per day.
A rapid recovery (normal temperature and leukocyte levels) was obtained within 2 d from the procedure (Figure 1). The catheter was removed after 2 wk, when the spontaneous output was clear and was less than 10 mL per day.
The short-term follow-up consisted of outpatient visits 7 to 10 d and 3 to 4 wk after operation. For long-term follow-up, a visit was scheduled and included an endovaginal US every 3 mo. At present the follow-up was uneventful after 18 mo.
Large diverticular abscesses (> 3 cm) should be treated by antibiotics and percutaneous drain. Percutaneous drain is the standard therapy in the absence of indications for immediate surgery[3]. However, abscess deep in the pelvis pose a unique problem because numerous intervening structures create obstacles for safe percutaneous access. These include pelvic bones, bowel, bladder, iliac vessels, and female reproductive organs. Alternative approaches to deep pelvic abscess include transvaginal, transrectal, transperineal and transgluteal punctures[4,5]. Transvaginal drainage has been described in several reports[1,2], but there has been no previous documentation of a vaginal drain of a pelvic abscess due to colonic diverticulitis.
In this case, rapid recovery was obtained with long-term disease-free survival, which is encouraging for its future use as an alternative drain of abscess due to diverticulitis.
Although further prospective studies evaluating the clinical usefulness of transvaginal drain of pelvic abscesses due to colonic diverticulitis are needed to give a definitive conclusion, we believe that transvaginal drain of pelvic abscess could be a useful alternative, when percutaneous approach is not feasible.
| 1. | Saokar A, Arellano RS, Gervais DA, Mueller PR, Hahn PF, Lee SI. Transvaginal drainage of pelvic fluid collections: results, expectations, and experience. AJR Am J Roentgenol. 2008;191:1352-1358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Gjelland K, Ekerhovd E, Granberg S. Transvaginal ultrasound-guided aspiration for treatment of tubo-ovarian abscess: a study of 302 cases. Am J Obstet Gynecol. 2005;193:1323-1330. [PubMed] |
| 3. | Andersen JC, Bundgaard L, Elbrønd H, Laurberg S, Walker LR, Støvring J. Danish national guidelines for treatment of diverticular disease. Dan Med J. 2012;59:C4453. [PubMed] |
| 4. | Levenson RB, Pearson KM, Saokar A, Lee SI, Mueller PR, Hahn PF. Image-guided drainage of tuboovarian abscesses of gastrointestinal or genitourinary origin: a retrospective analysis. J Vasc Interv Radiol. 2011;22:678-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
P- Reviewer Chong VH S- Editor Gou SX L- Editor A E- Editor Zheng XM