©The Author(s) 2021.
World J Clin Cases. Dec 6, 2021; 9(34): 10738-10745
Published online Dec 6, 2021. doi: 10.12998/wjcc.v9.i34.10738
Published online Dec 6, 2021. doi: 10.12998/wjcc.v9.i34.10738
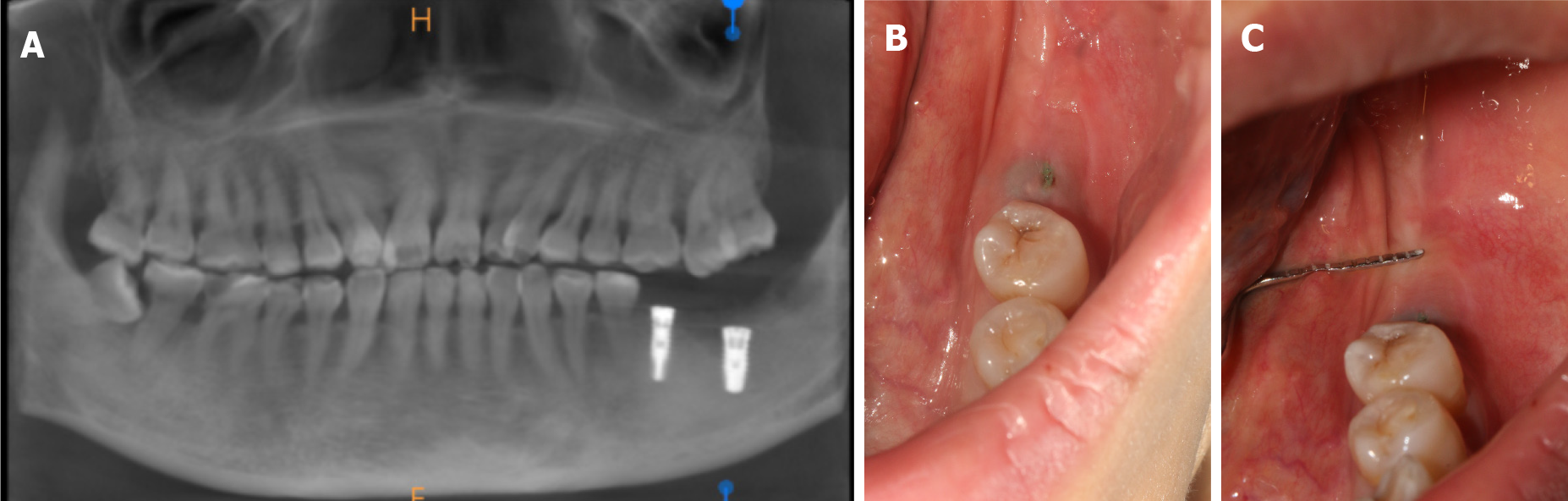
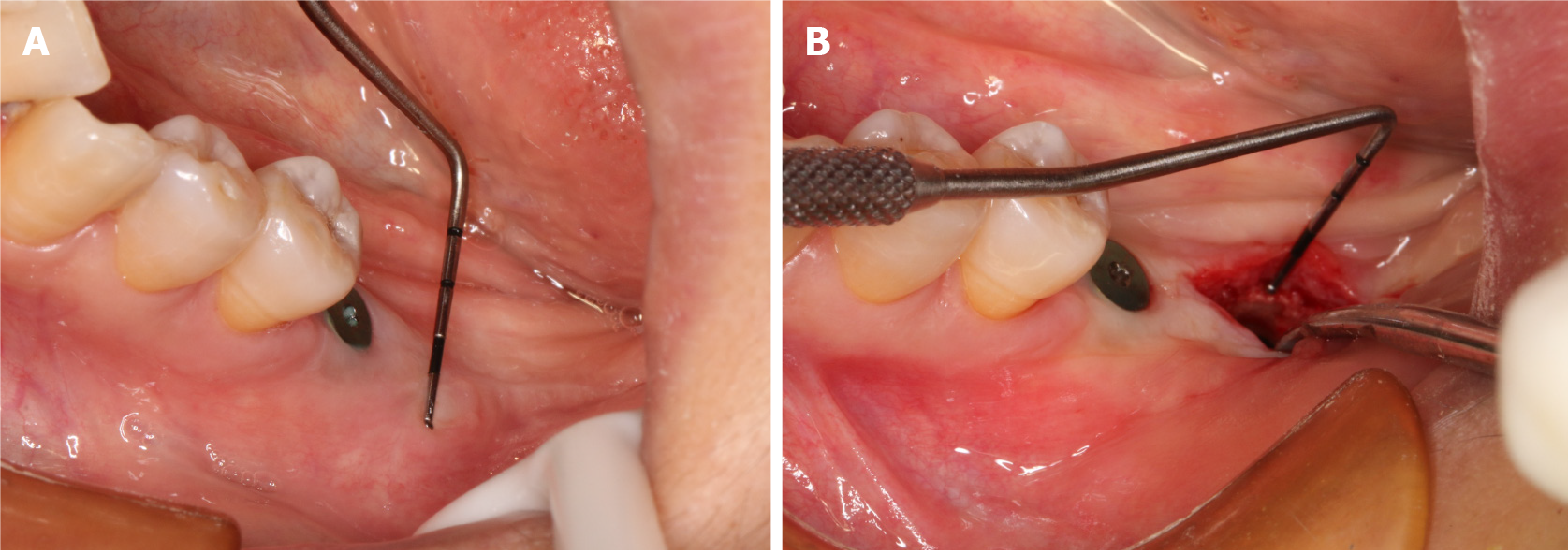
Figure 1 Three months after implant surgery.
A: The cone-beam computer tomography showed that good osseointegration had formed between the implant and bone; B and C: Clinical examination and periodontal probe measurement showed that the width of the buccal keratinized gingiva of tooth #37 was 0.5 mm, 0.5 mm, 0 mm from mesial to distal, respectively.
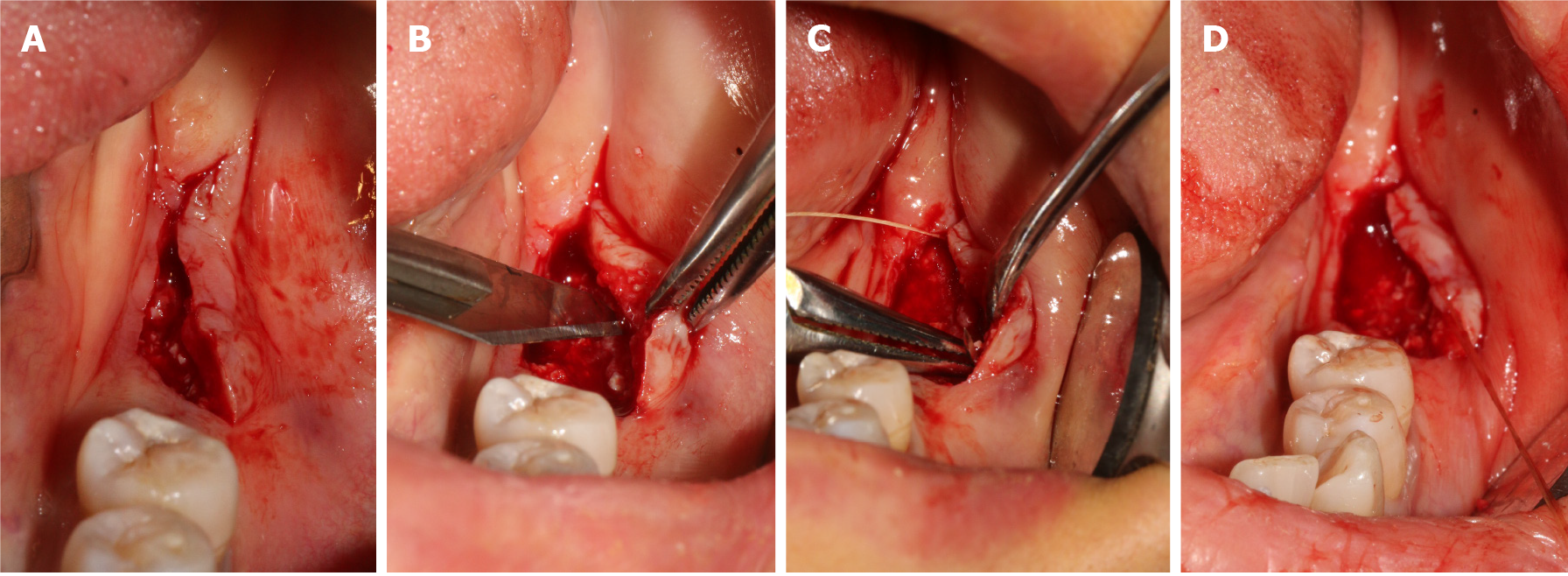
Figure 2 Surgery Process.
A: Deviated lingual linear incision; B: The buccal full-thickness flap was split to a semi-thick flap by a No. 15 blade; C and D: The semi-thick flap was positioned apically with 5-0 protein absorbable sutures.
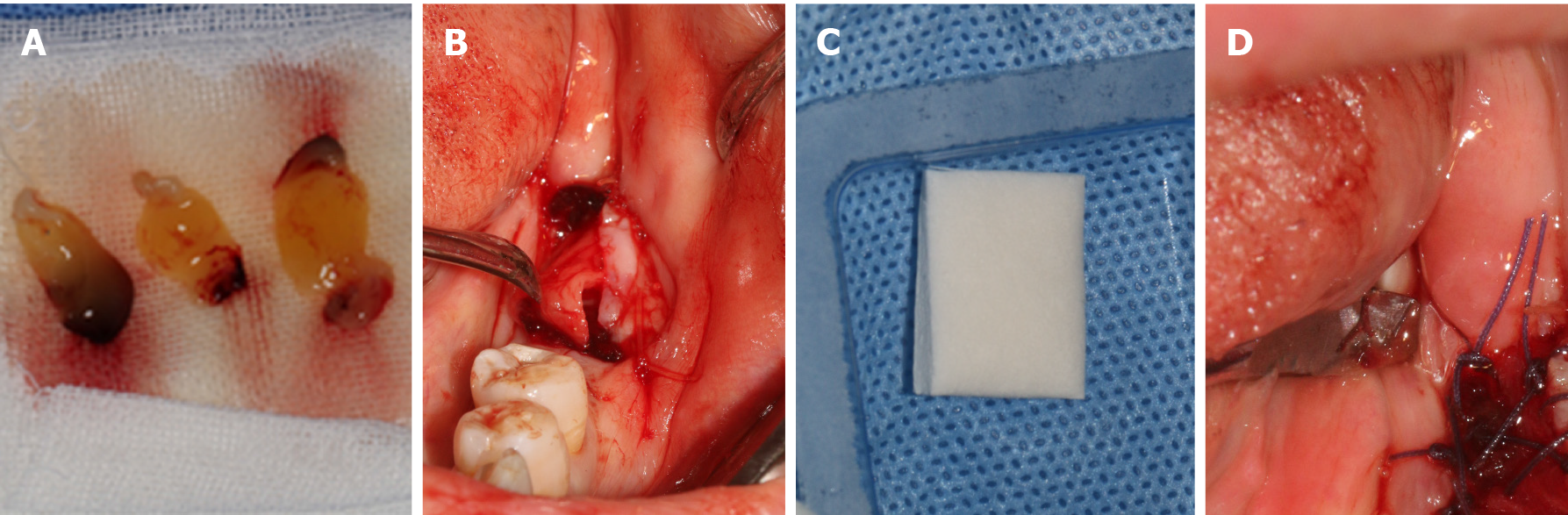
Figure 3 Graft materials implantation.
A: Platelet rich fibrin (PRF) was obtained by blood centrifugation from the patient; B: PRF was covered over the exposed wound; C: Mucograft® (Geistlich, Switzerland, 15 mm × 20 mm); D: Mucograft® was trimmed and added to cover the wound above the PRF by suture fixation.
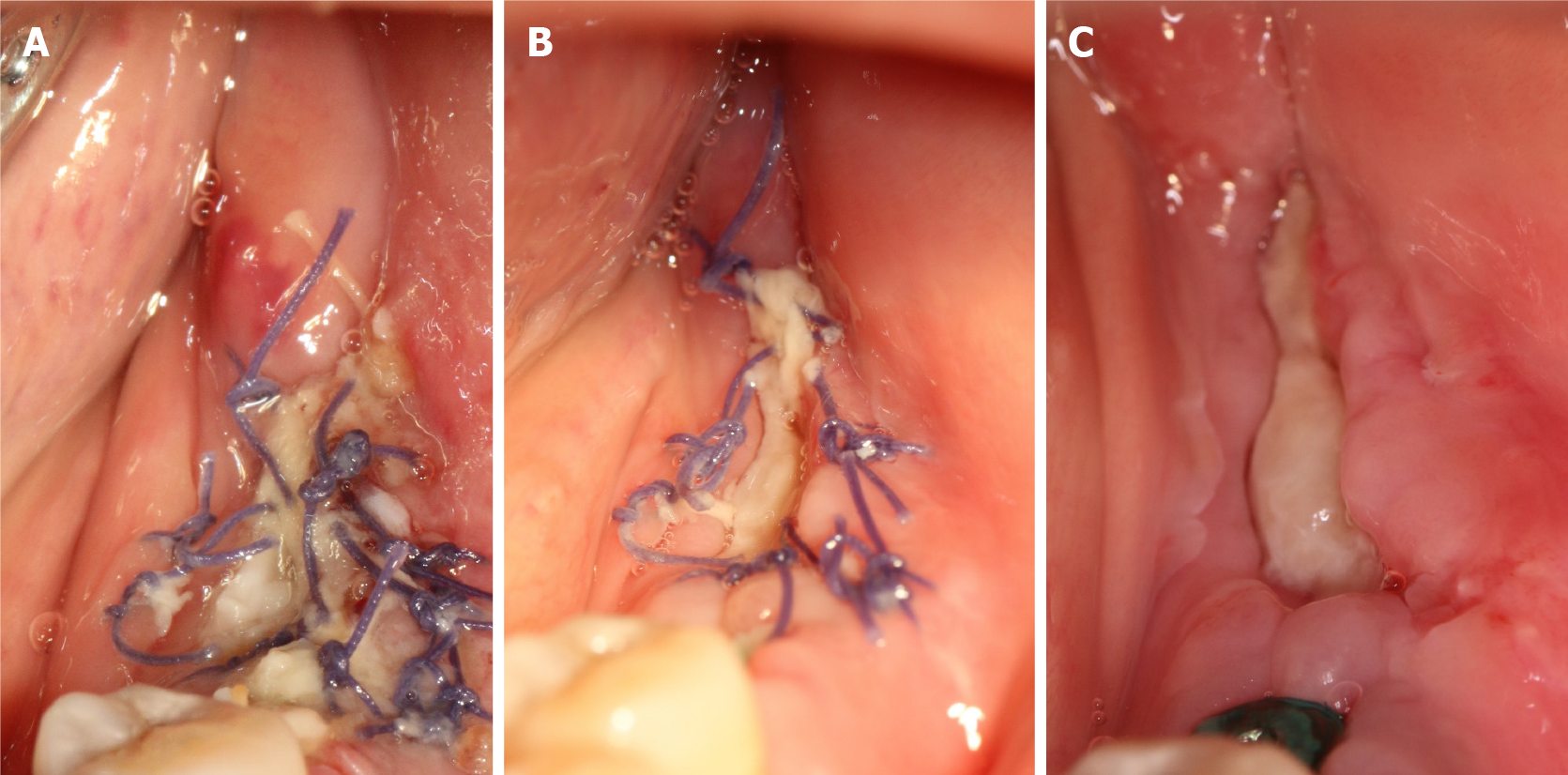
Figure 4 Healing process.
A: 3 d; B: 7 d; C: 10 d.
Figure 5 After 4 wk, stage II surgery was performed.
A: The width of the buccal keratinized gingiva of tooth #37 is 4 mm; B: The thickness of mucosa is 4.5 mm.
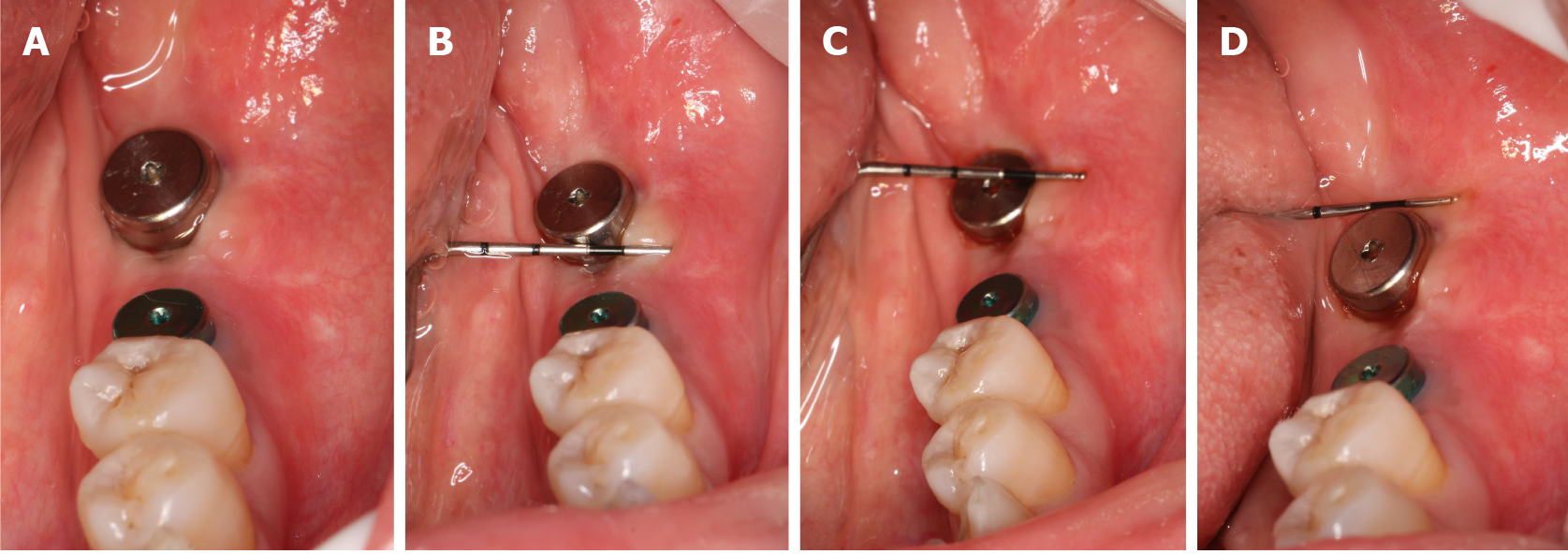
Figure 6 The keratinized gingiva.
A: The keratinized gingiva around the healing abutment was healthy, adequate and consistent with adjacent tissue; B: The mesial width of the buccal keratinized gingiva was 4 mm; C: The middle width of the buccal keratinized gingiva was 4 mm; D: The distal width of the buccal keratinized gingiva was 3 mm.
- Citation: Han CY, Wang DZ, Bai JF, Zhao LL, Song WZ. Peri-implant keratinized gingiva augmentation using xenogeneic collagen matrix and platelet-rich fibrin: A case report. World J Clin Cases 2021; 9(34): 10738-10745
- URL: https://www.wjgnet.com/2307-8960/full/v9/i34/10738.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i34.10738