©The Author(s) 2021.
World J Clin Cases. Oct 26, 2021; 9(30): 9244-9254
Published online Oct 26, 2021. doi: 10.12998/wjcc.v9.i30.9244
Published online Oct 26, 2021. doi: 10.12998/wjcc.v9.i30.9244
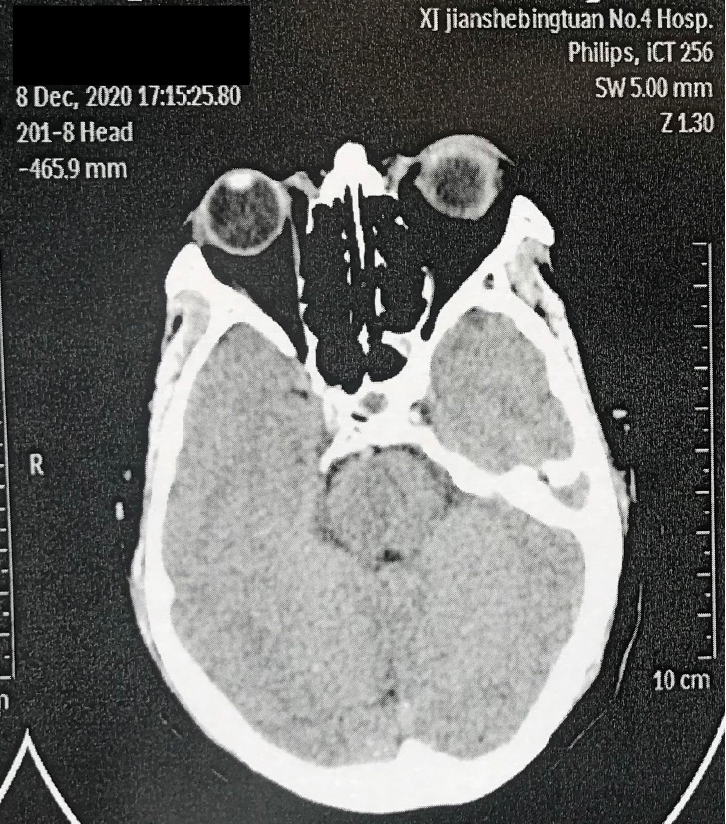
Figure 1 Computed X-ray tomography examination in the previous hospital.
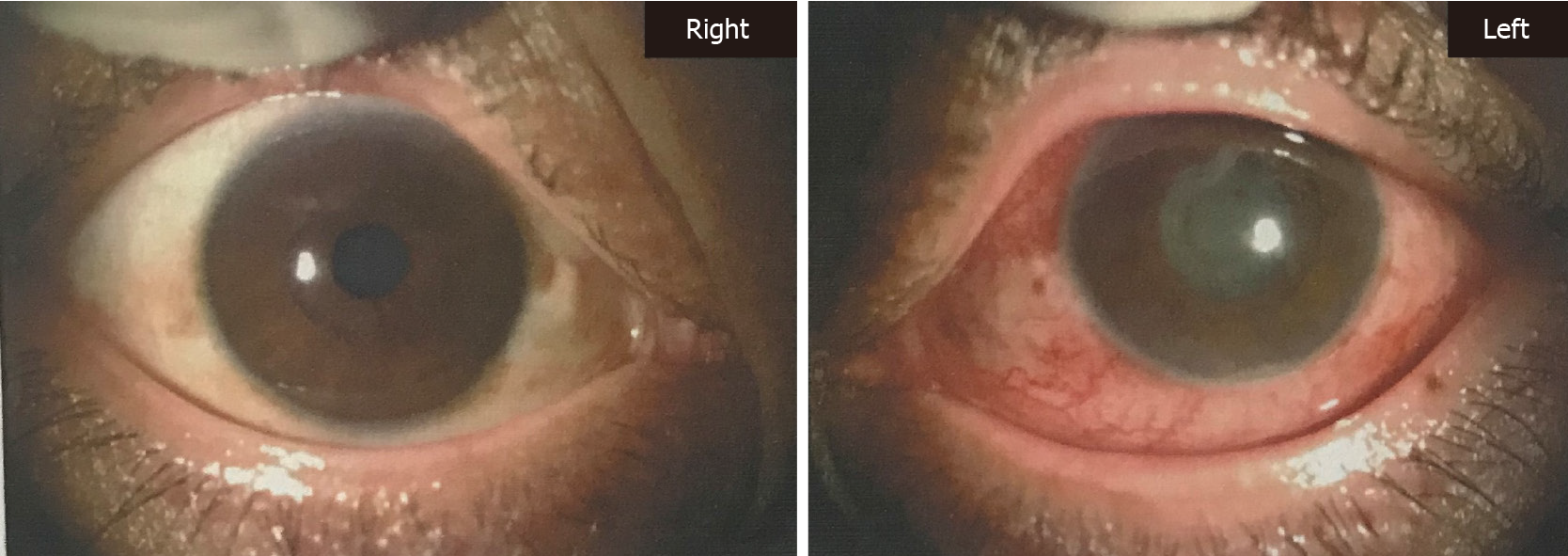
Figure 2 Anterior eye segment photography (left).
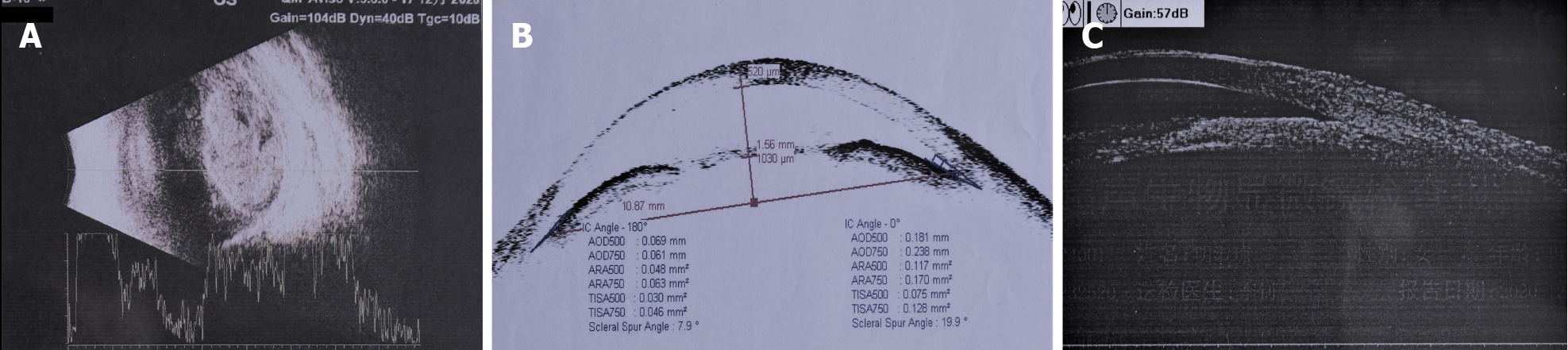
Figure 3 Ultrasonic biomicroscopy examination.
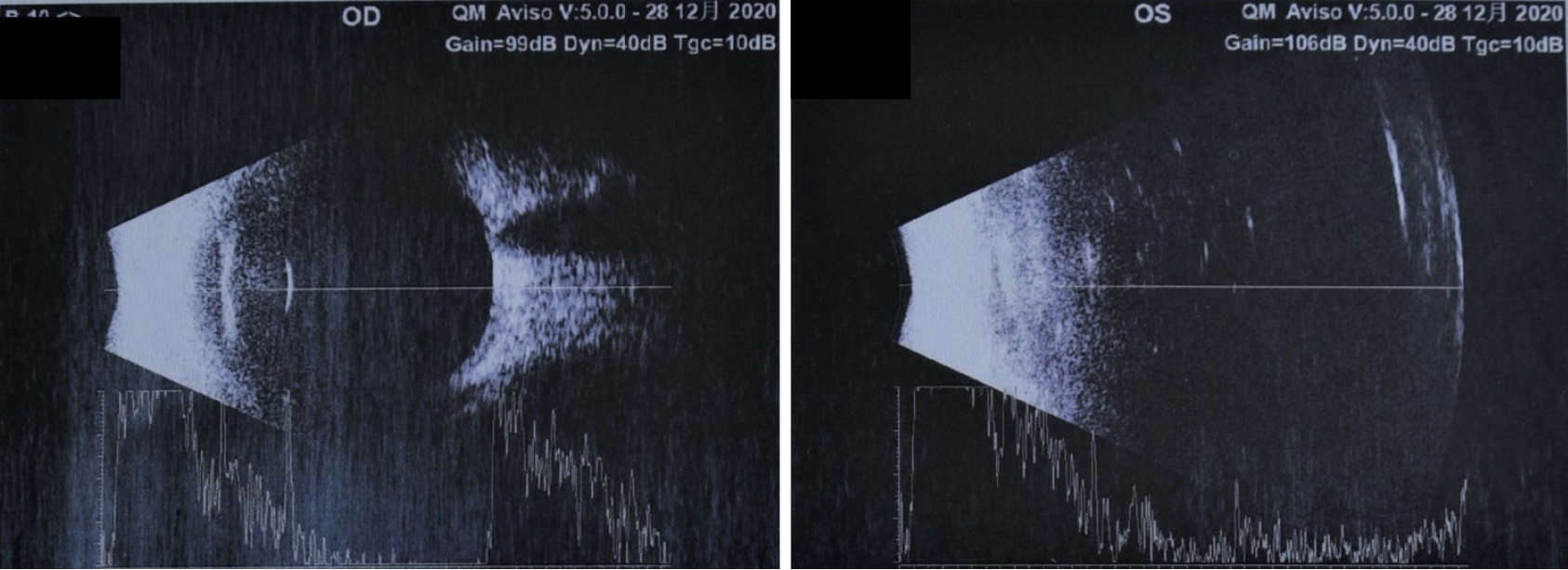
A: Ocular ultrasonography showing a normal optical axis in both eyes, vitreous opacity in the right eye, and vitreous turbidness in the left eye (potentially indicating hemorrhage); B: Anterior segment optical coherence tomography showing closure of the left eye from 7 to 10 o’clock, along with edema, and infiltration of the cornea; C: Ultrasonic biomicroscopy showing swelling of the iris root in both eyes, an expanded turbid anterior chamber in the left eye, shallow partial detachment of the ciliary body, and positive suprachoroidal effusion.
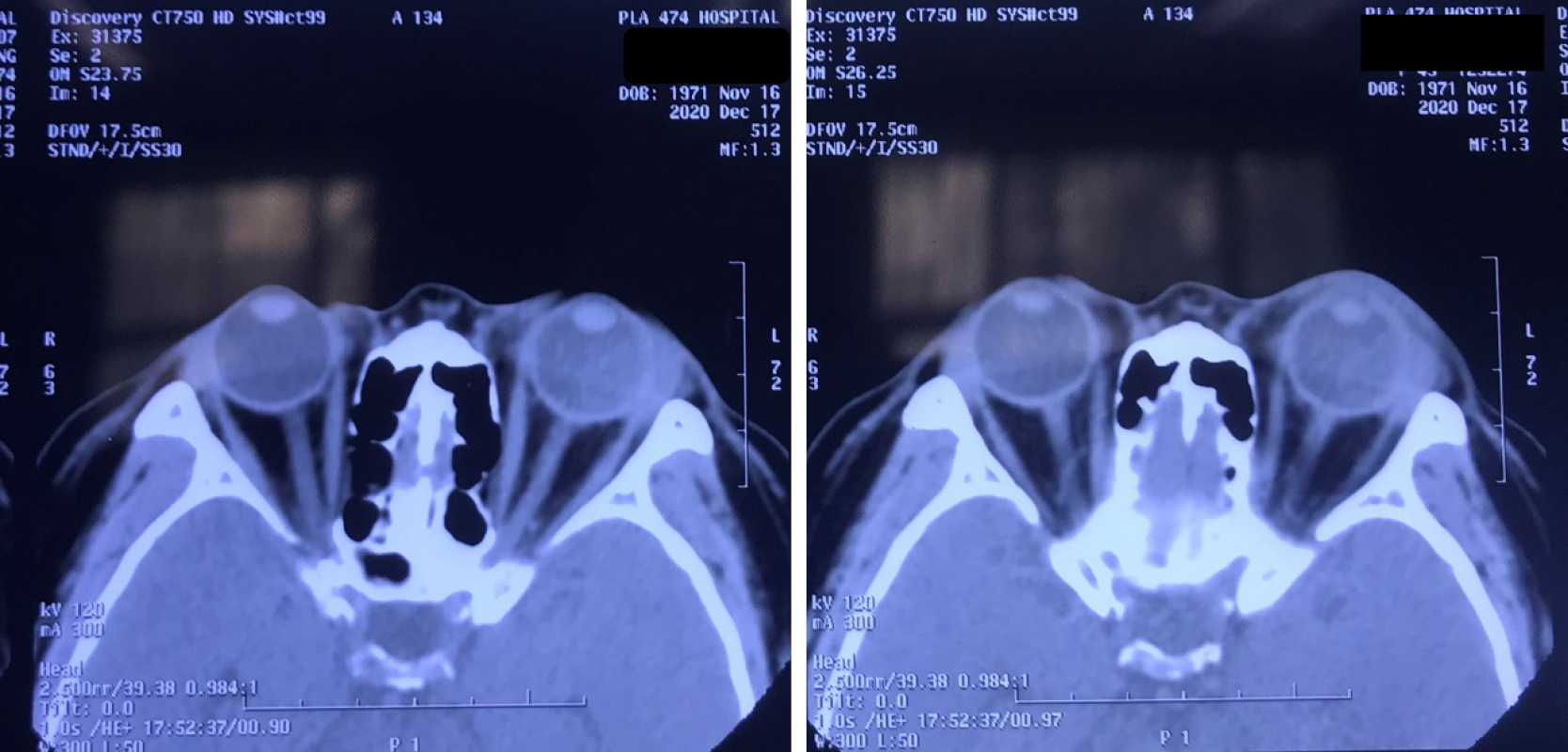
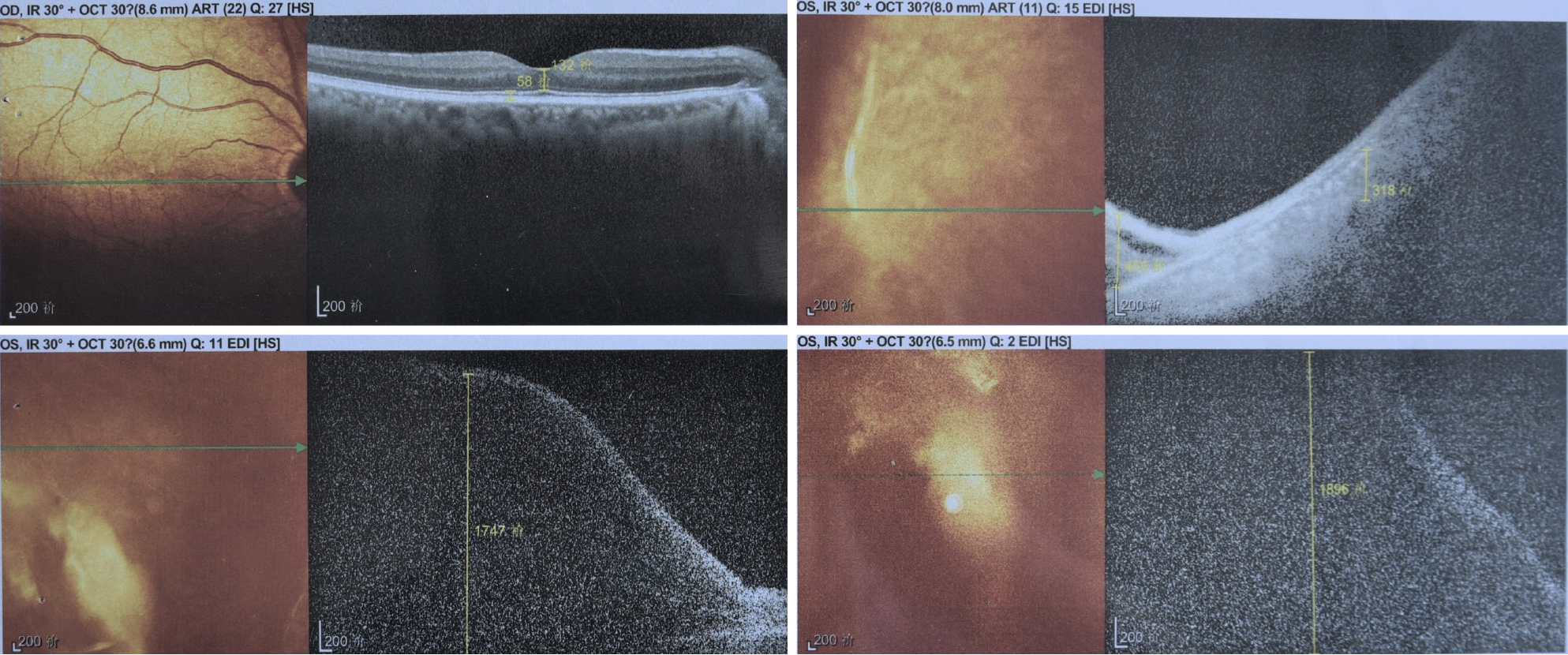
Figure 4 Computed X-ray tomography examination results.
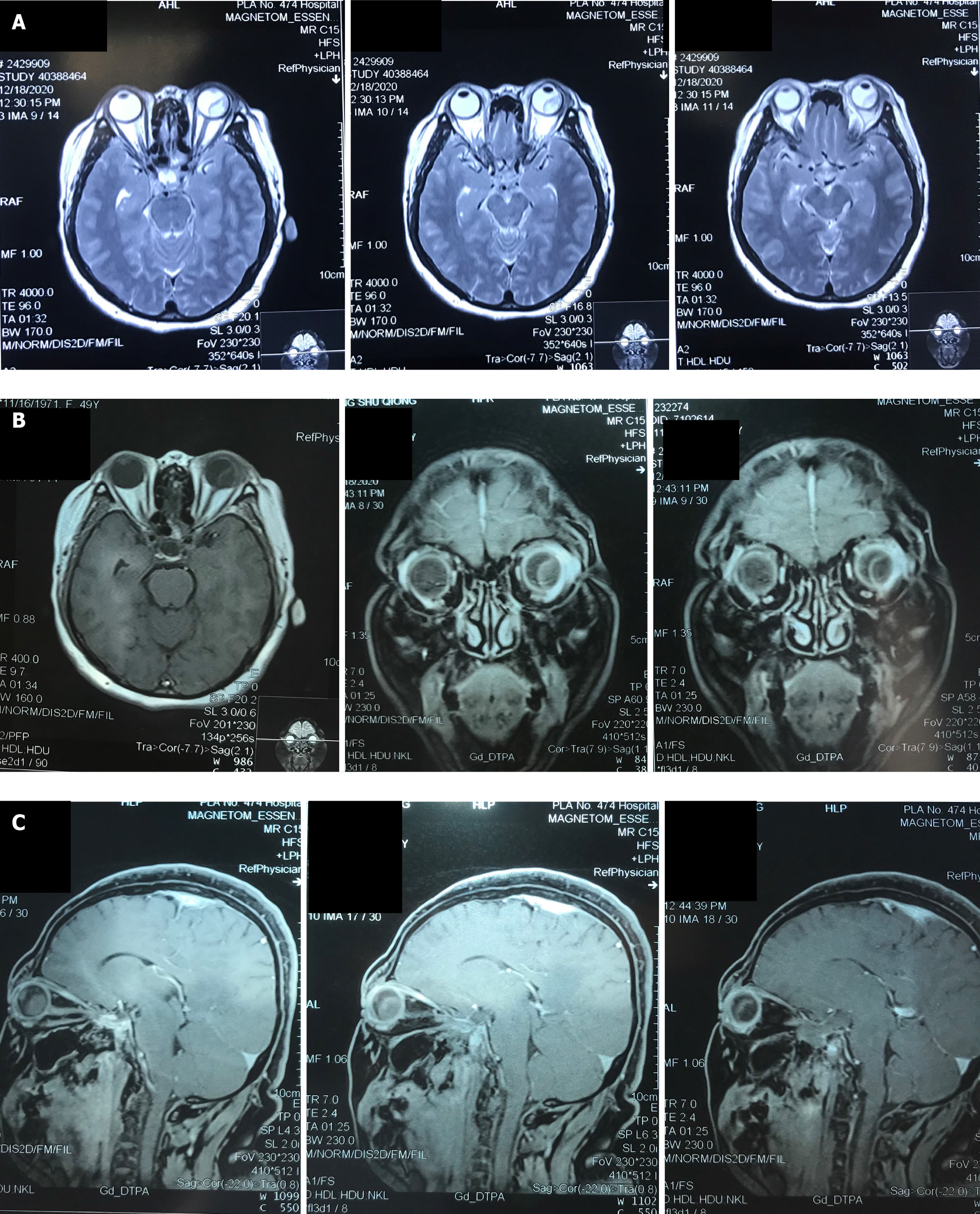
Figure 5 Magnetic resonance imaging examination results.
A: Coronal image; B: Sagittal image; C: Transverse image.
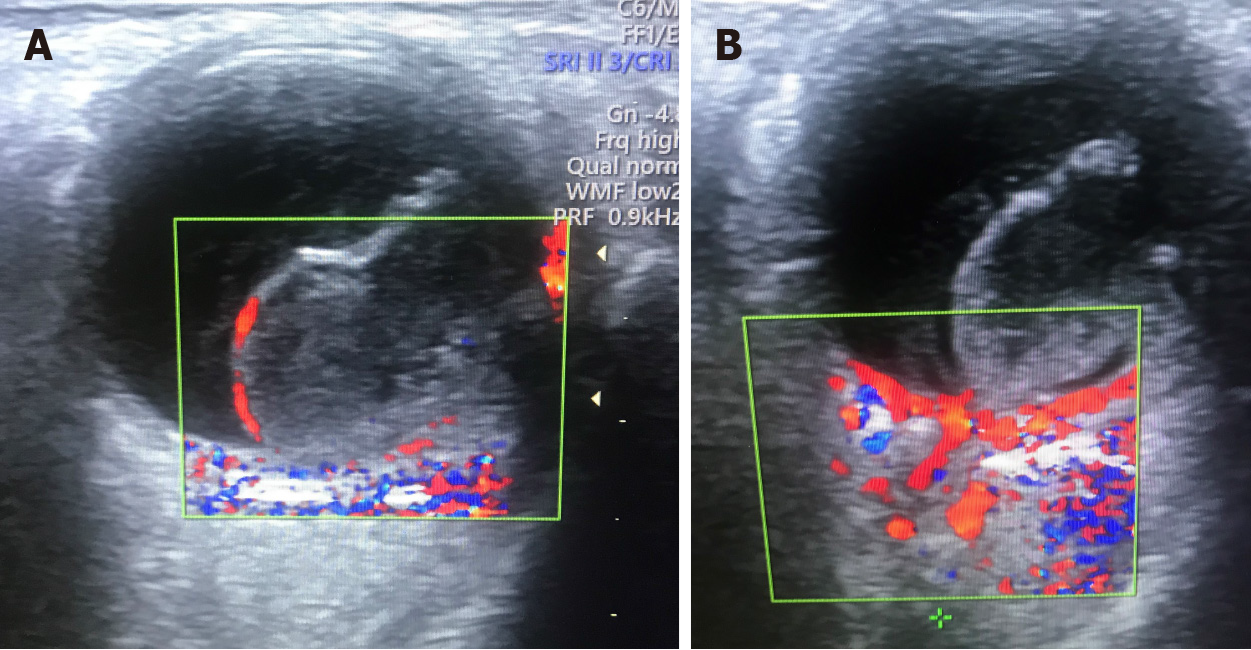
Figure 6 Color Doppler ultrasound examination of the left eye.
A: Blood flow signals were seen in the entire periphery of the occupying lesion; B: There were no obvious blood flow signals in the solid portion in the middle of the lesion.
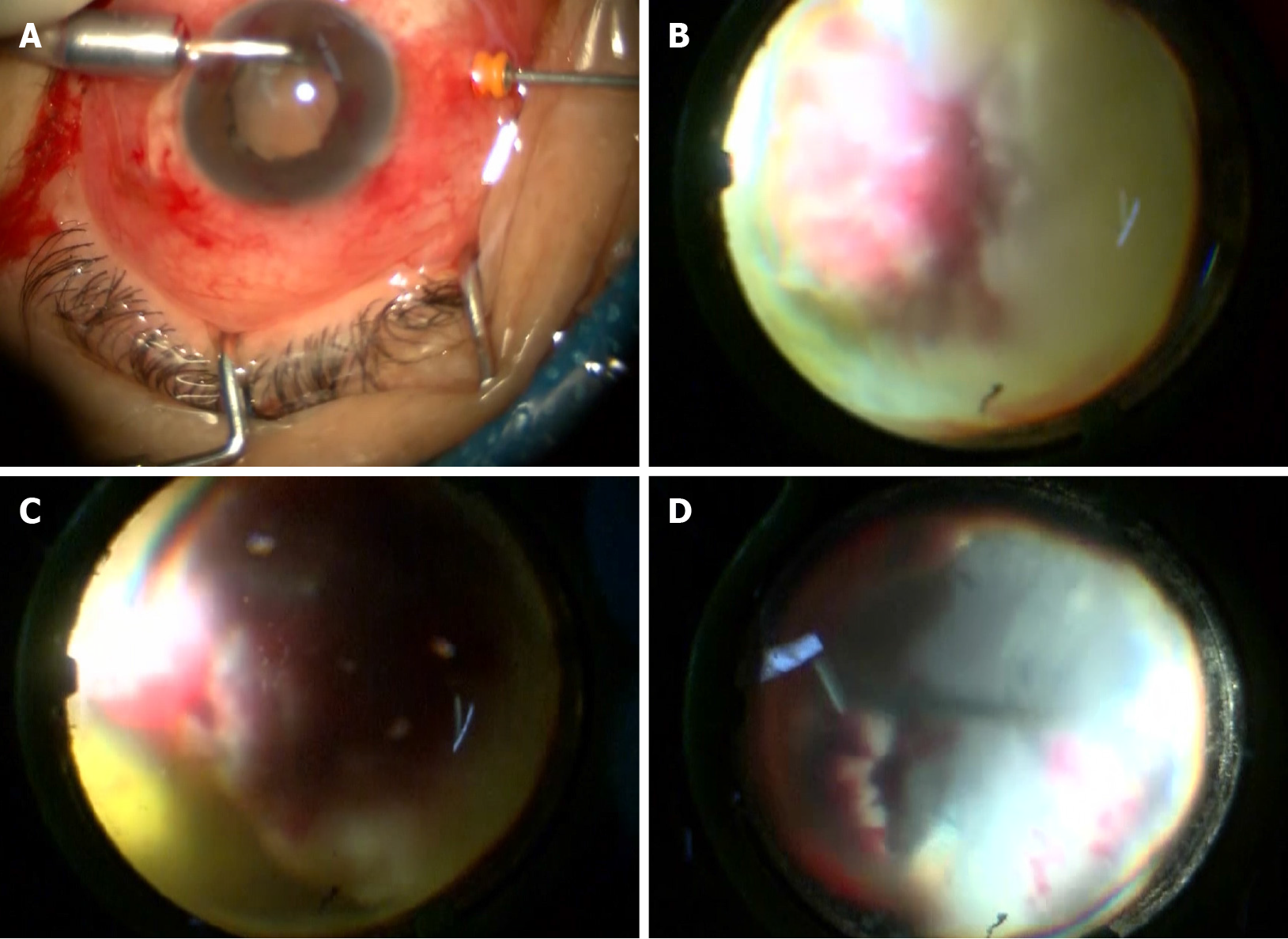
Figure 7 Imaging screenshots during surgery.
A: Placement of a perfusion system into the corneoscleral tunnel; B: The occupying lesion was found to occupy 75% of the vitreous cavity; C: The peripheral retina was necrotic and denatured; D: The entire white viscous tissue was completely removed, and the necrotic retina was cleaned up.
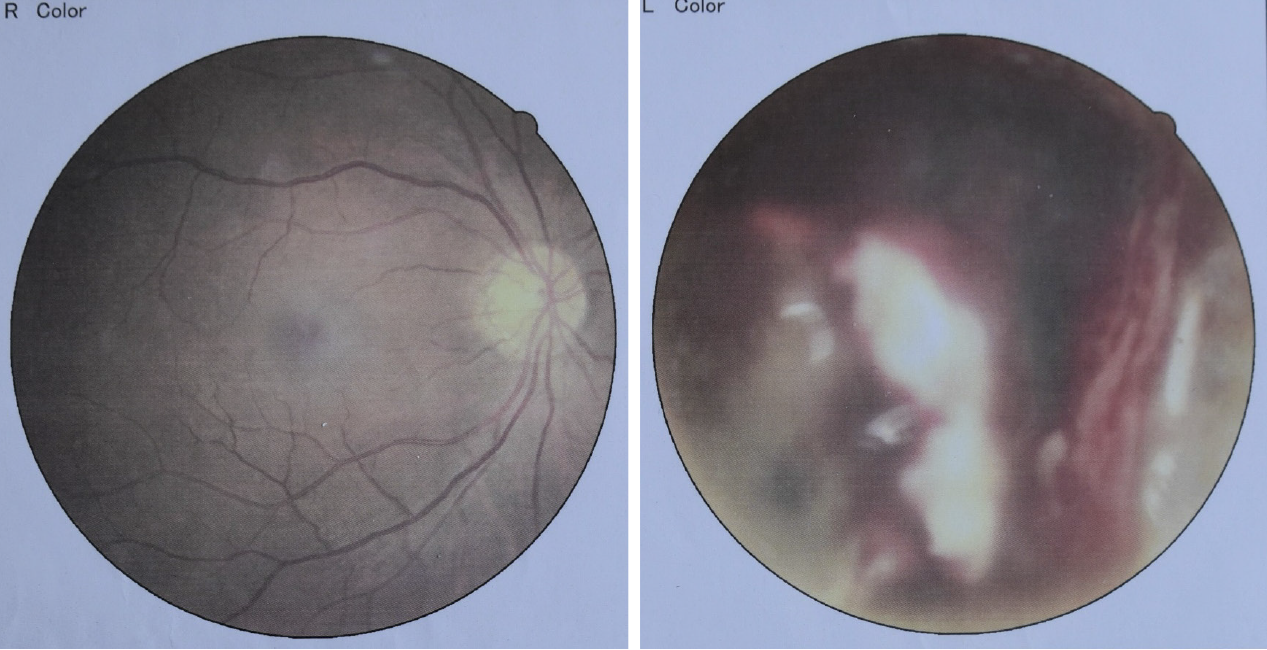
Figure 8 Fundus imaging photographs taken 3 d after surgery.
Figure 9 Optical coherence tomography imaging taken 3 d after surgery.
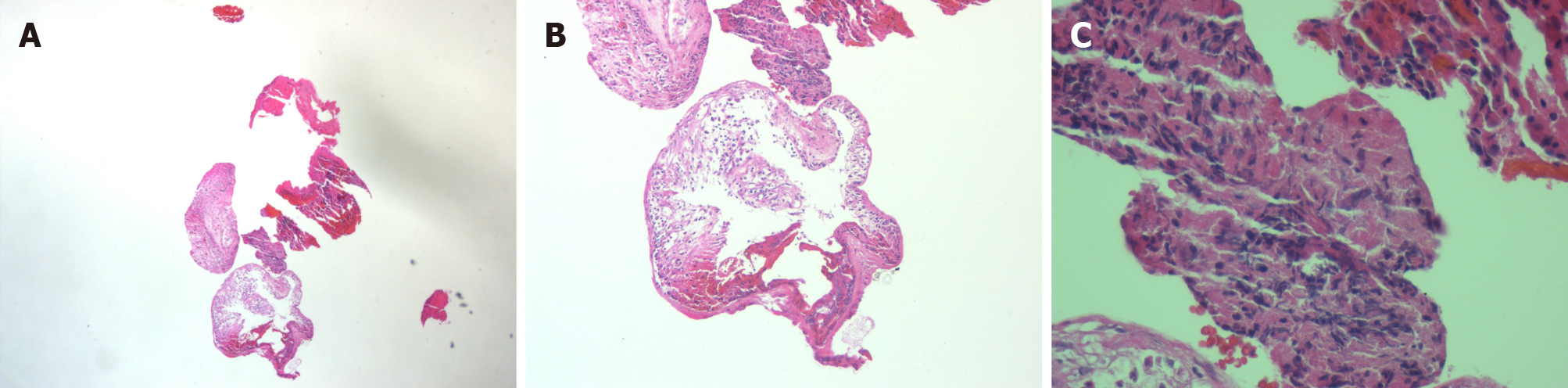
Figure 10 Pathological results derived from the removed lesion.
A: Magnification of 10 × 5; B: Magnification of 10 × 10; C: Magnification of 10 × 40.
Figure 11 Postoperative ultrasound results.
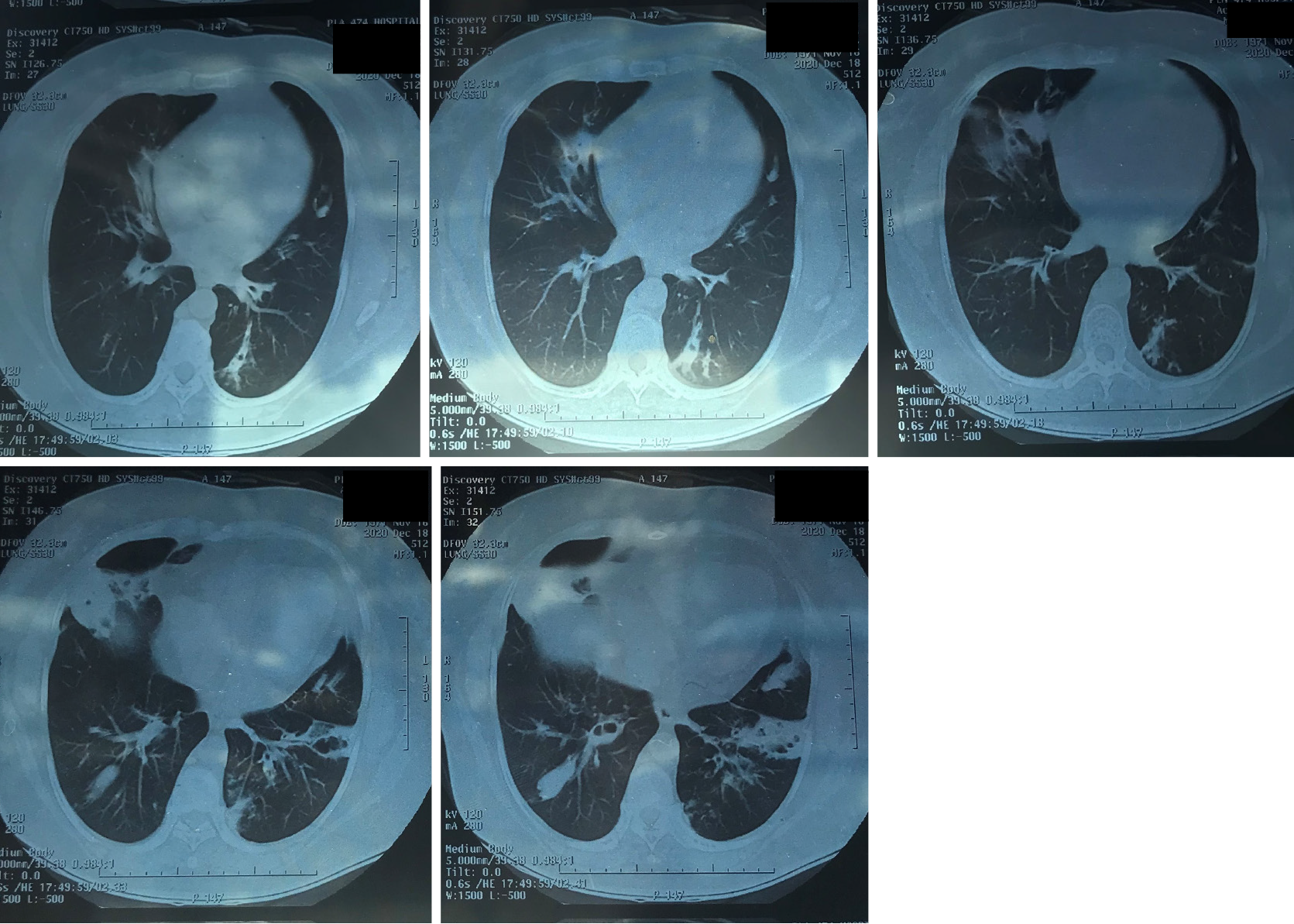
Figure 12 Retrospective lung computed X-ray tomography examination at admission.
- Citation: Li Z, Gao W, Tian YM, Xiao Y. Choroidal metastatic mucinous abscess caused by Pseudomonas aeruginosa: A case report. World J Clin Cases 2021; 9(30): 9244-9254
- URL: https://www.wjgnet.com/2307-8960/full/v9/i30/9244.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i30.9244