©The Author(s) 2020.
World J Clin Cases. Jan 26, 2020; 8(2): 451-463
Published online Jan 26, 2020. doi: 10.12998/wjcc.v8.i2.451
Published online Jan 26, 2020. doi: 10.12998/wjcc.v8.i2.451
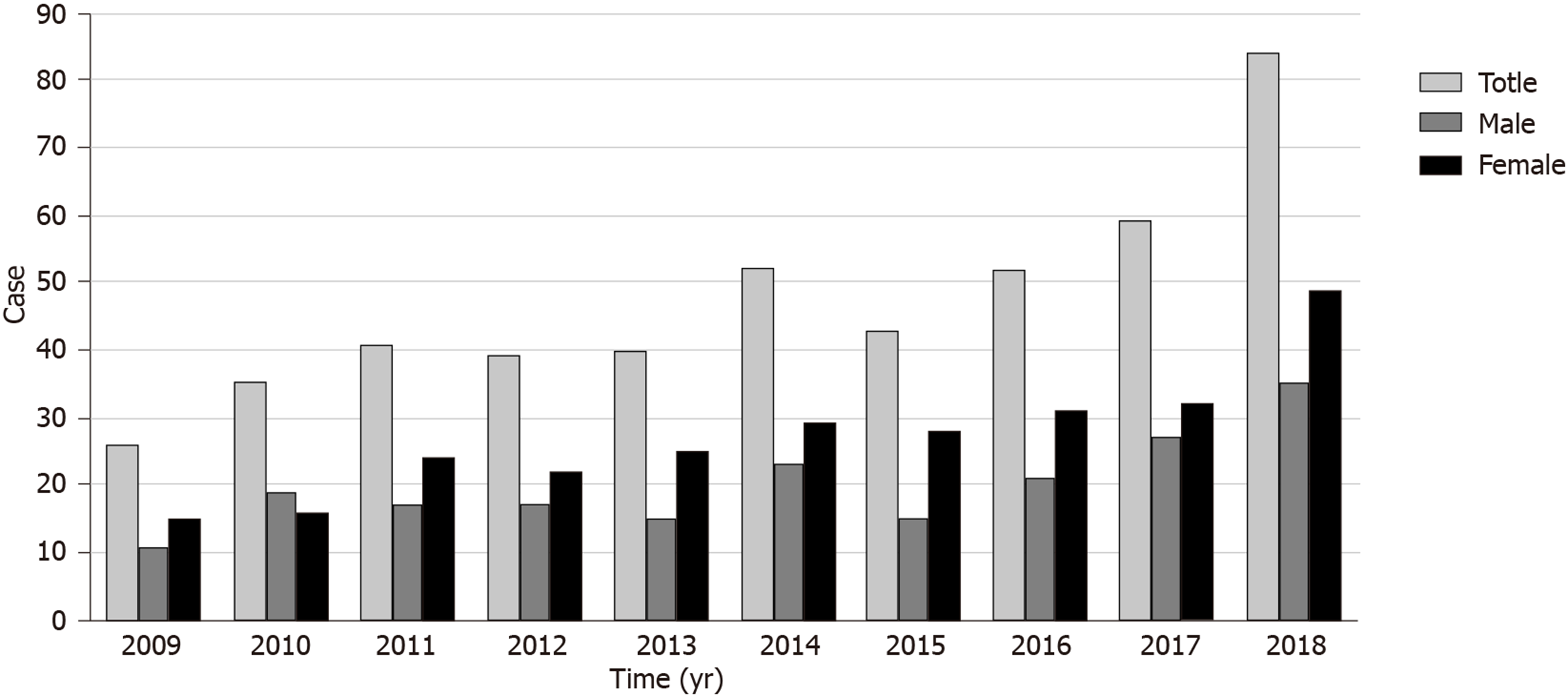
Figure 1 Annual changes in the number of fungal rhinosinusitis patients from 2009 to 2018.
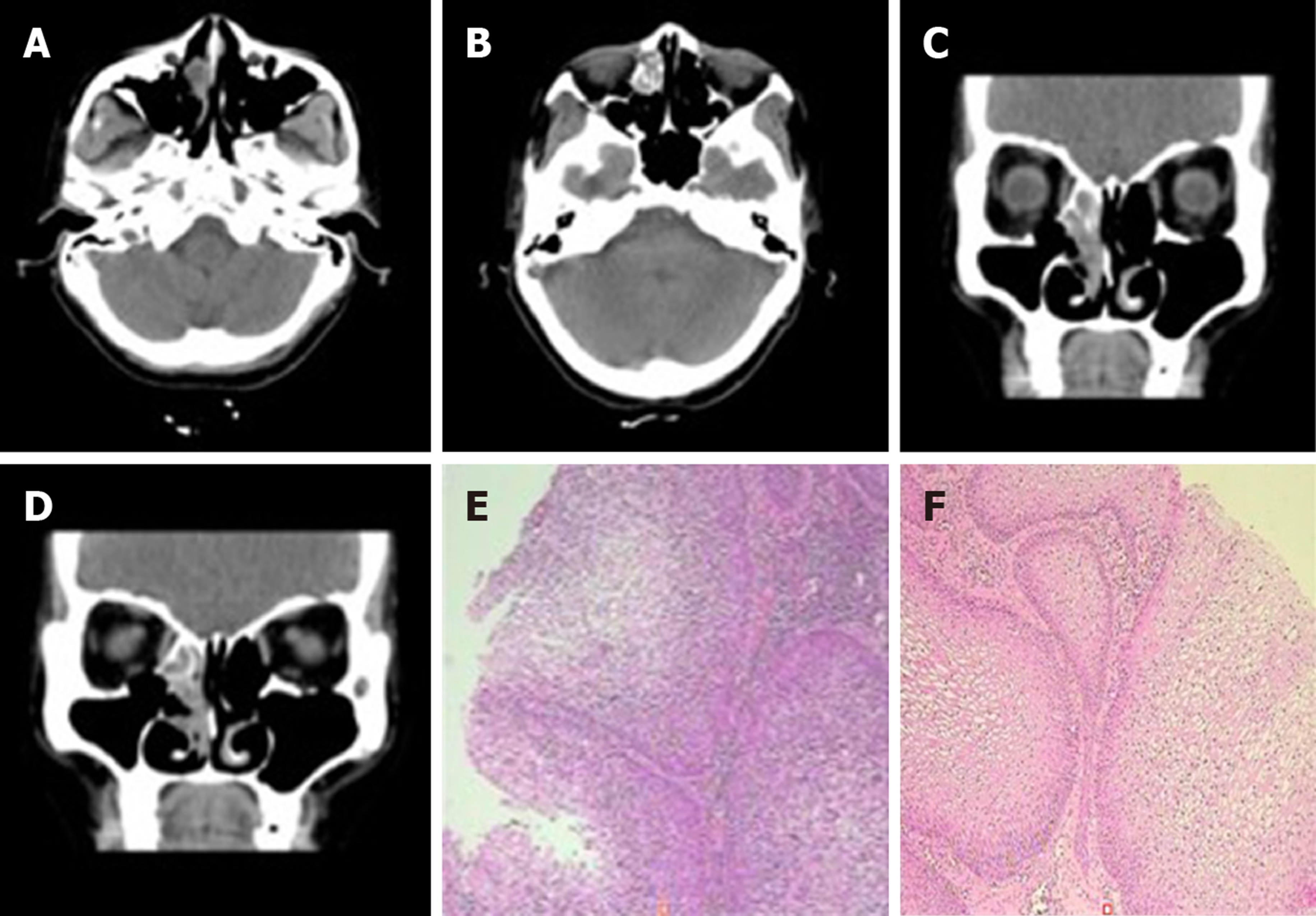
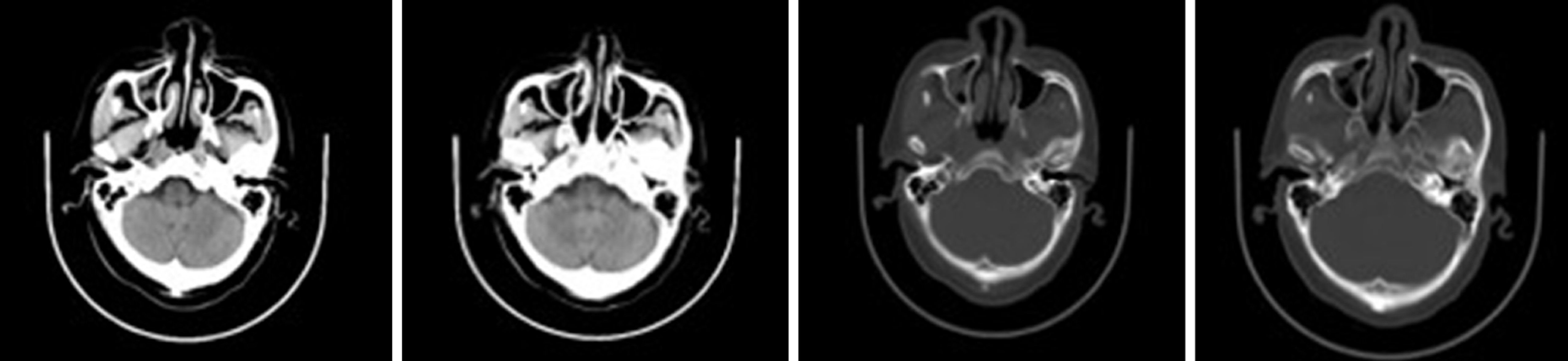
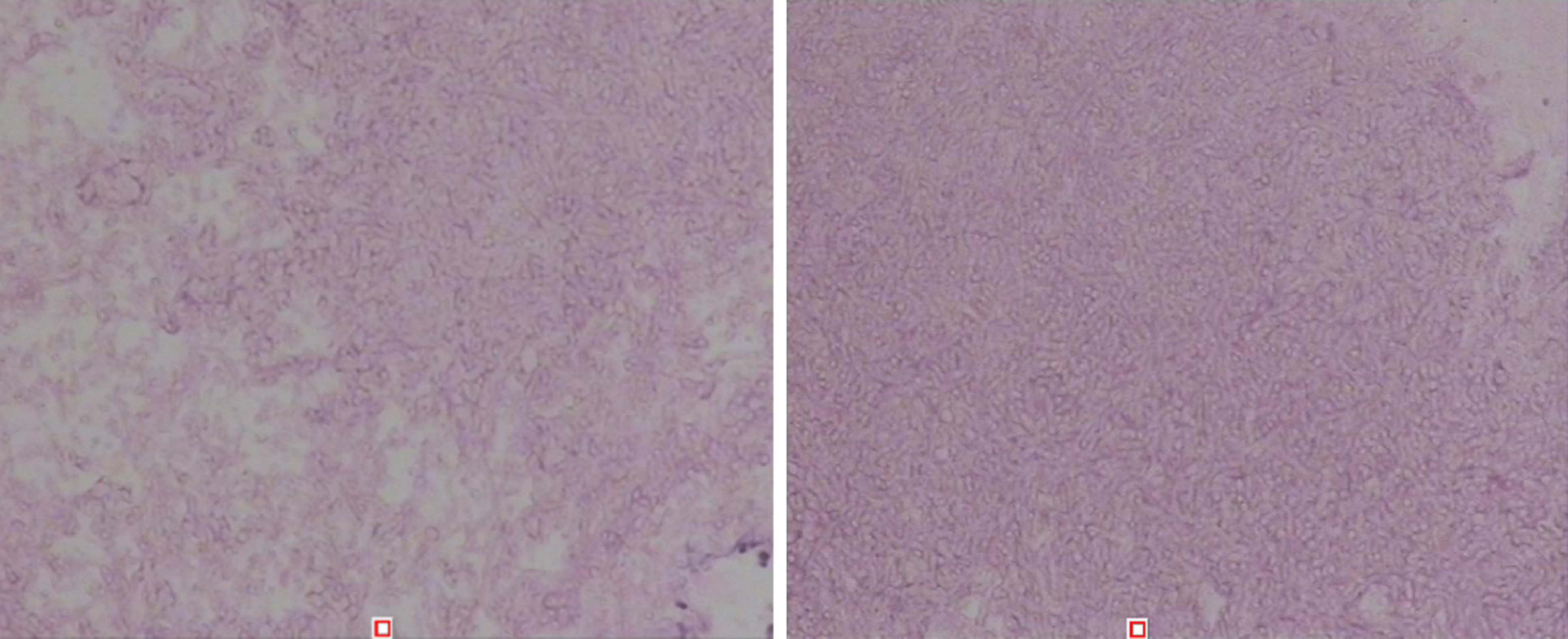
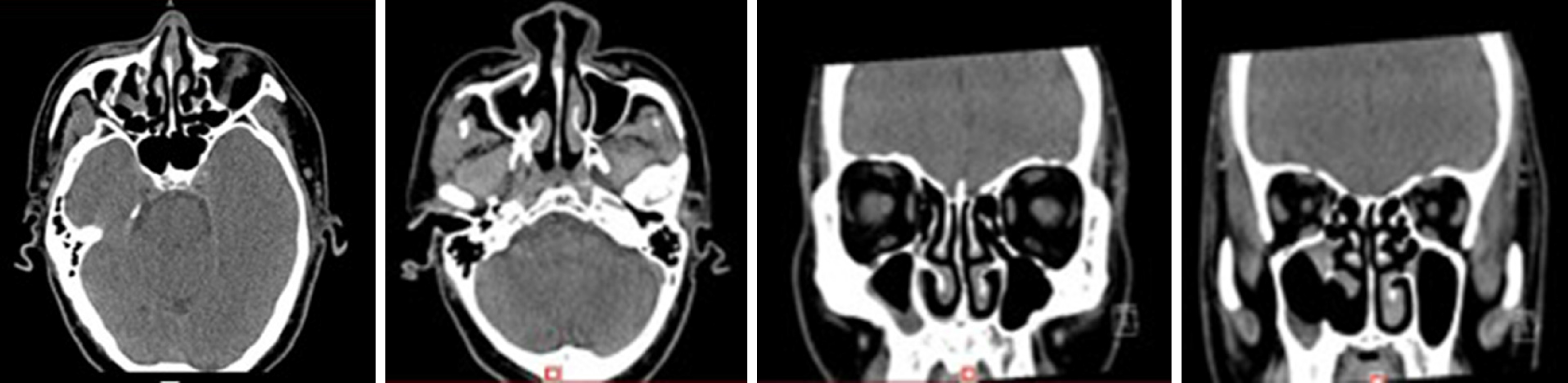
Figure 2 Computed tomography scan and histopathologic examination results of Case 1.
A-D: The first preoperative examination (February 4, 2016). Axial and sagittal paranasal sinus computed tomography scans showed dense shadows in the soft tissue of the right inferior nasal tract with small, low-density shadows, which were indistinct from the inferior turbinate and ethmoid sinus, and bone destruction in the ethmoid sinus; E and F: Histopathologic findings showed that the nasal mass was an inverted papilloma and that the maxillary sinus exhibited chronic inflammation of the mucous membrane.
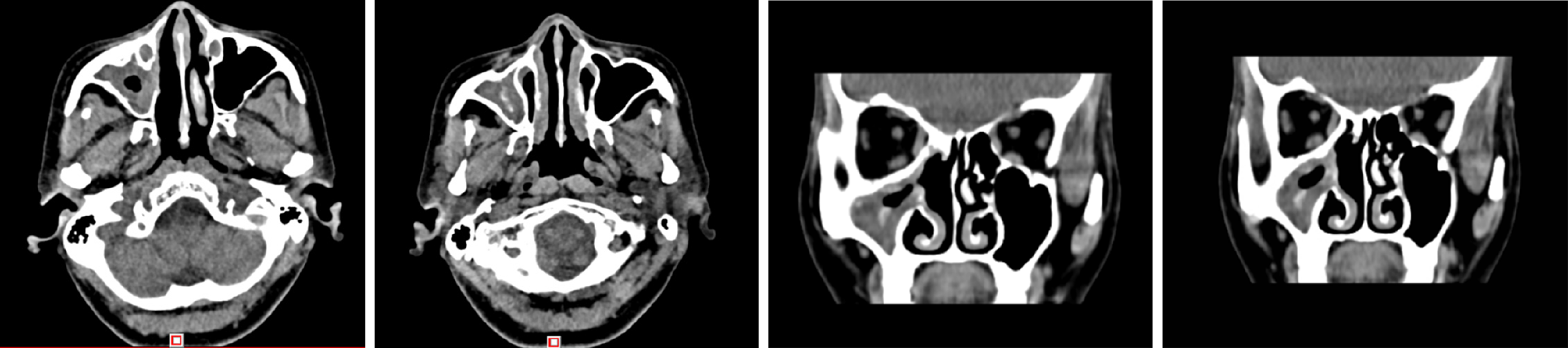
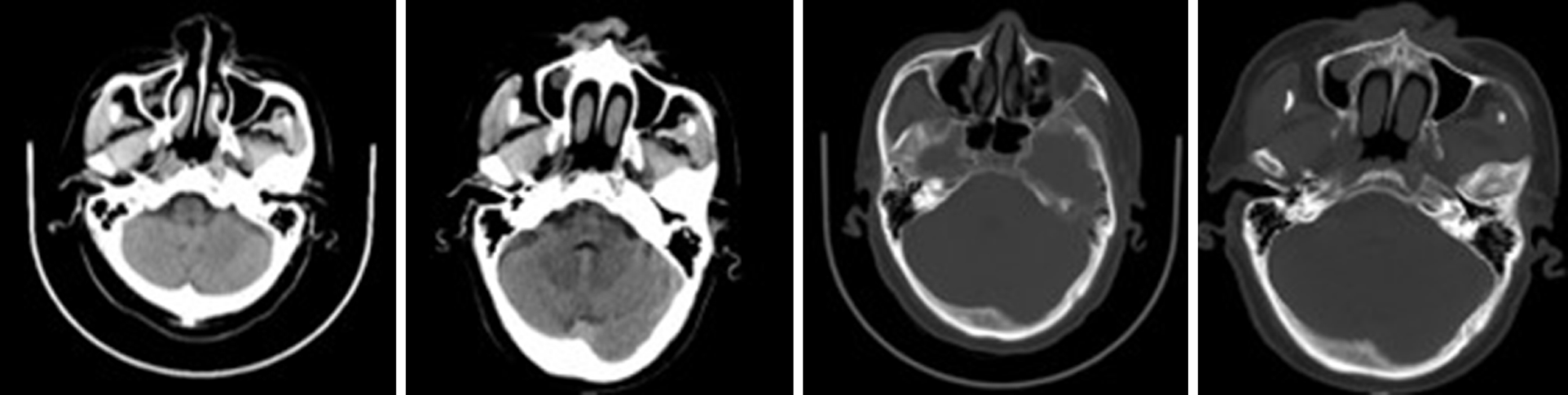
Figure 3 The second preoperative examination (October 19, 2017).
Axial and sagittal paranasal sinus computed tomography scans showed that most of the ethmoid plates in the right ethmoid sinus were missing. Patchy, dense shadows were visible in the right maxillary sinus, and strips of dense shadows were visible in the right maxillary sinus. No abnormal bone tissue was observed in the sinus wall.
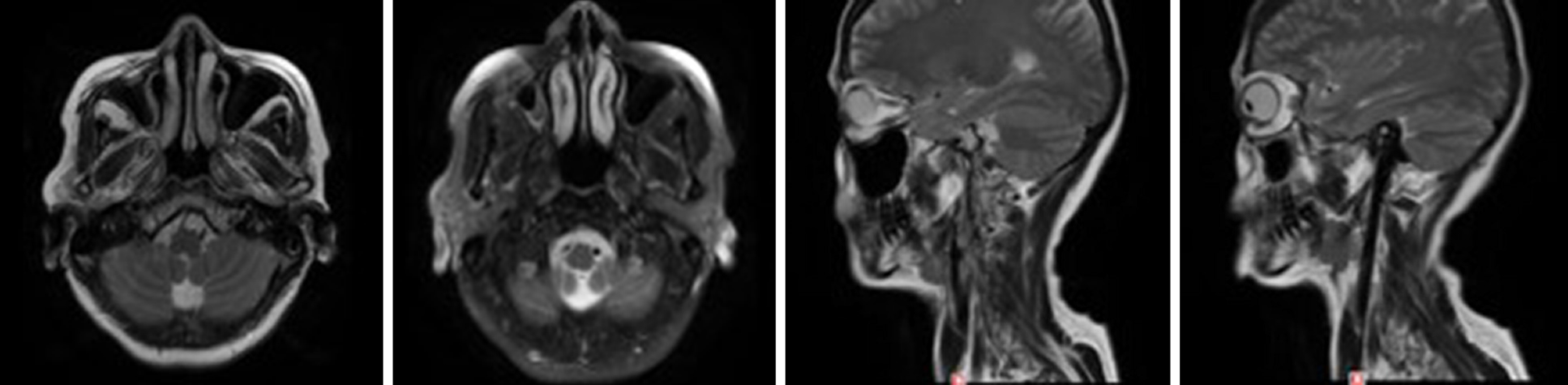
Figure 4 Postoperative re-examination (December 28, 2018).
Axial and sagittal magnetic resonance imaging of the right maxillofacial region showed that most of the ethmoid plates, and the middle turbinate and part of the upper turbinate of the right ethmoid sinus were absent, indicating postoperative changes. The opening of the right maxillary sinus was satisfactory, the mucosa was slightly thickened on the medial wall, and no abnormal signal or shadow was observed in the nasal cavity.
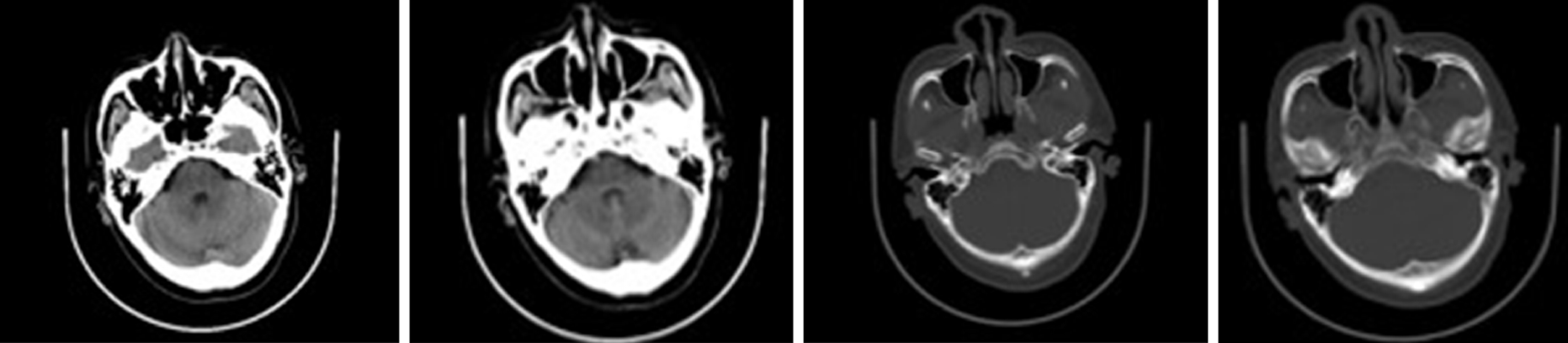
Figure 5 Physical examination (May 27, 2016).
An axial head computed tomography scan showed a round soft tissue shadow under the mucosa of the maxillary sinus on the right side with a clear boundary.
Figure 6 Physical examination (May 26, 2017).
An axial head computed tomography scan showed no abnormalities in the nasal cavity or sinuses.
Figure 7 Physical examination (May 31, 2018).
Compared to scans obtained on May 26, 2017, an axial head computed tomography scan showed new inflammation in the right maxillary sinus.
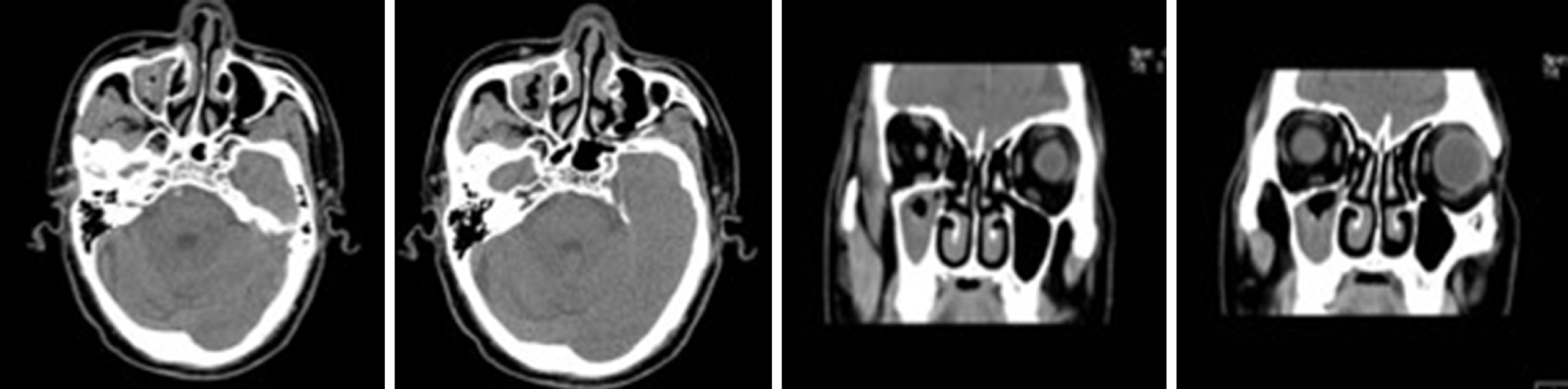
Figure 8 Preoperative examination (February 11, 2019).
An axial and sagittal paranasal sinus computed tomography scan showed an increased patchy, dense shadow in the right maxillary sinus and sinus wall bone integrity.
Figure 9 Postoperative pathological findings (right maxillary sinus mass) showing a large number of fungal mycetes when observed under a microscope, consistent with aspergillosis (February 14, 2019).
Specific staining results: PAS (+) and PASD (+).
Figure 10 Postoperative re-examination (June 6, 2019).
Axial and sagittal paranasal sinus computed tomography scans showed that the right lateral wall of the maxillary sinus was locally absent, and the mucosa in the sinus cavity was thickened. Other sinus cavities contained good air content and no abnormally dense shadow.
- Citation: Wang LL, Chen FJ, Yang LS, Li JE. Analysis of pathogenetic process of fungal rhinosinusitis: Report of two cases. World J Clin Cases 2020; 8(2): 451-463
- URL: https://www.wjgnet.com/2307-8960/full/v8/i2/451.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i2.451