Copyright
©The Author(s) 2020.
World J Clin Cases. Aug 26, 2020; 8(16): 3411-3430
Published online Aug 26, 2020. doi: 10.12998/wjcc.v8.i16.3411
Published online Aug 26, 2020. doi: 10.12998/wjcc.v8.i16.3411
Figure 1 Immunoglobulin G4-related disease pancreatitis.
A and B: Contrast enhanced computerized tomography scan showing diffuse pancreatic enlargement with a hypodense peripancreatic rim (arrows); C: Contrast enhanced computerized tomography showing decrease in pancreatic size but persistent delayed enhancement in the body of pancreas (arrow) 4 wk after steroid treatment.
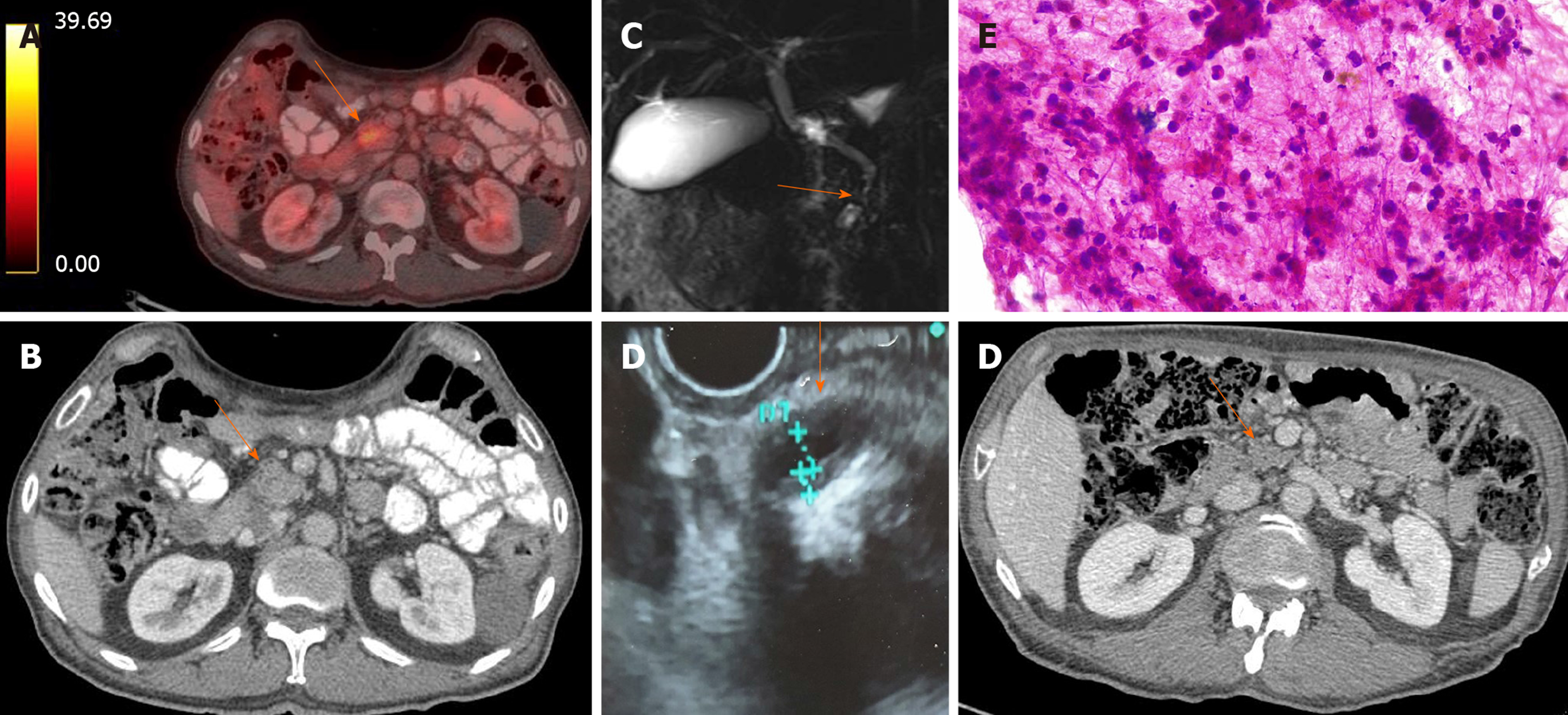
Figure 2 Idiopathic duct centric pancreatitis in a 70-year-old male with presenting with new onset diabetes mellitus patient and weight loss.
A and B: Positron emission tomography-computed tomography and simple computed tomography scan showing a heterogenous mass (arrows) in the head of the pancreas (max SUV 4.2); C: Magnetic resonance cholangiopancreatography showing a distal common bile duct common biliary duct stenosis with no proximal biliary or main pancreatic duct dilation; D: Endoscopic ultrasound showing a narrowed intrapancreatic common bile duct with symmetric hypoechoic thick walls; E: Micrography of cytology specimen from a pancreatic head mass obtained with endoscopic ultrasonography guided fine-needle aspiration, it shows a dense acute and chronic inflammatory infiltrate with numerous neutrophils in the background; F: Chest computed tomography (venous phase) showing atrophy and disappearance of the pancreatic mass in the head of the pancreas following 4 wk of steroid therapy (arrow).
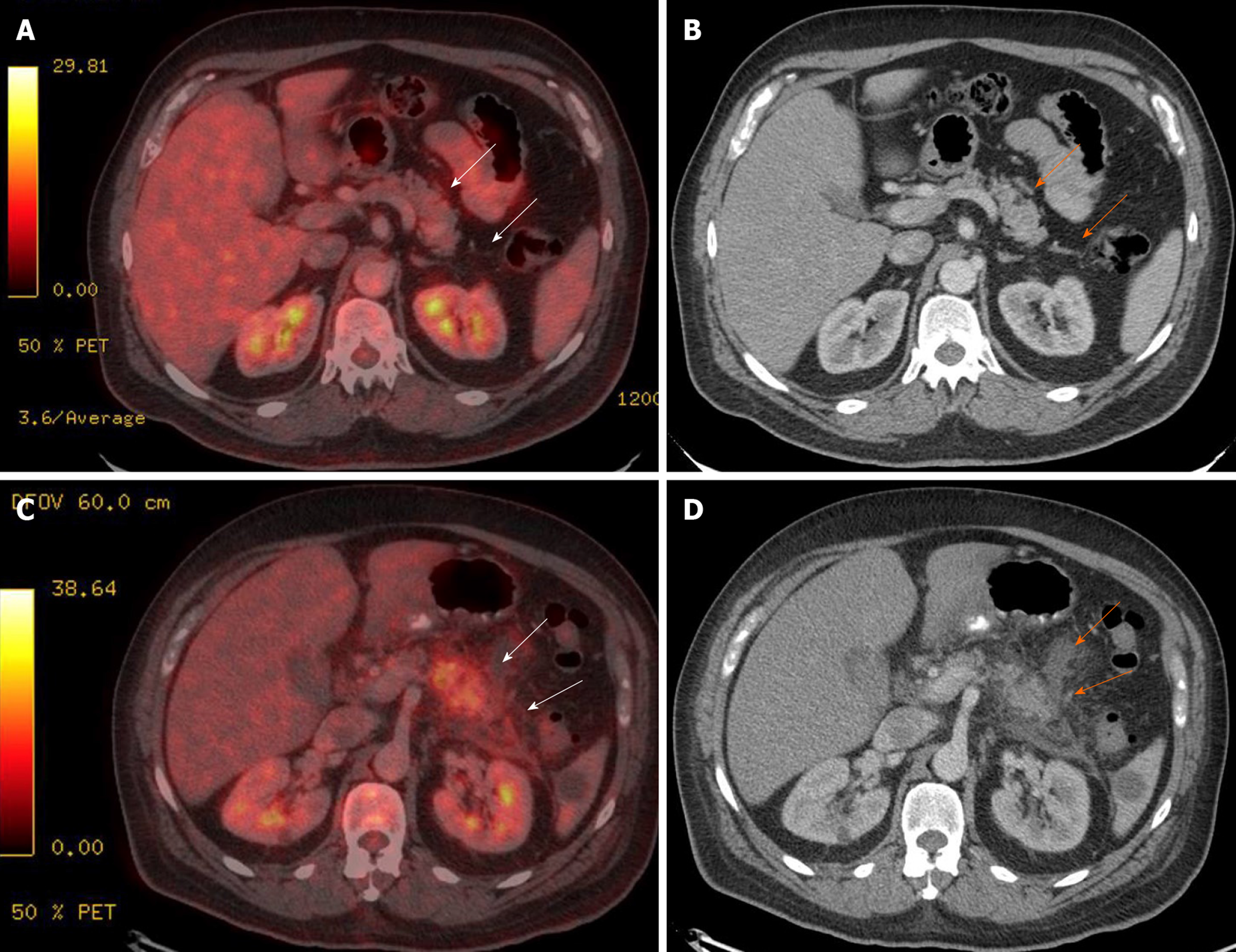
Figure 3 Immune checkpoint inhibitor-related acute pancreatitis in a patient receiving pembrolizumab for malignant melanoma.
A and B: Positron emission tomography-computed tomography and simple abdominal computed tomography at start of pembrolizumab showing normal pancreas and Peri pancreatic tissue (arrows); C and D: Positron emission tomography-computed tomography and simple abdominal computed tomography images 2 mo after starting pembrolizumab, showing increased activity at the tail of the pancreas (max SUV 8.2), Peri pancreatic fat stranding and Peri pancreatic fluid at the body and tail of pancreas (arrows).
- Citation: Pelaez-Luna M, Soriano-Rios A, Lira-Treviño AC, Uscanga-Domínguez L. Steroid-responsive pancreatitides. World J Clin Cases 2020; 8(16): 3411-3430
- URL: https://www.wjgnet.com/2307-8960/full/v8/i16/3411.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i16.3411