©The Author(s) 2019.
World J Clin Cases. Sep 6, 2019; 7(17): 2526-2535
Published online Sep 6, 2019. doi: 10.12998/wjcc.v7.i17.2526
Published online Sep 6, 2019. doi: 10.12998/wjcc.v7.i17.2526
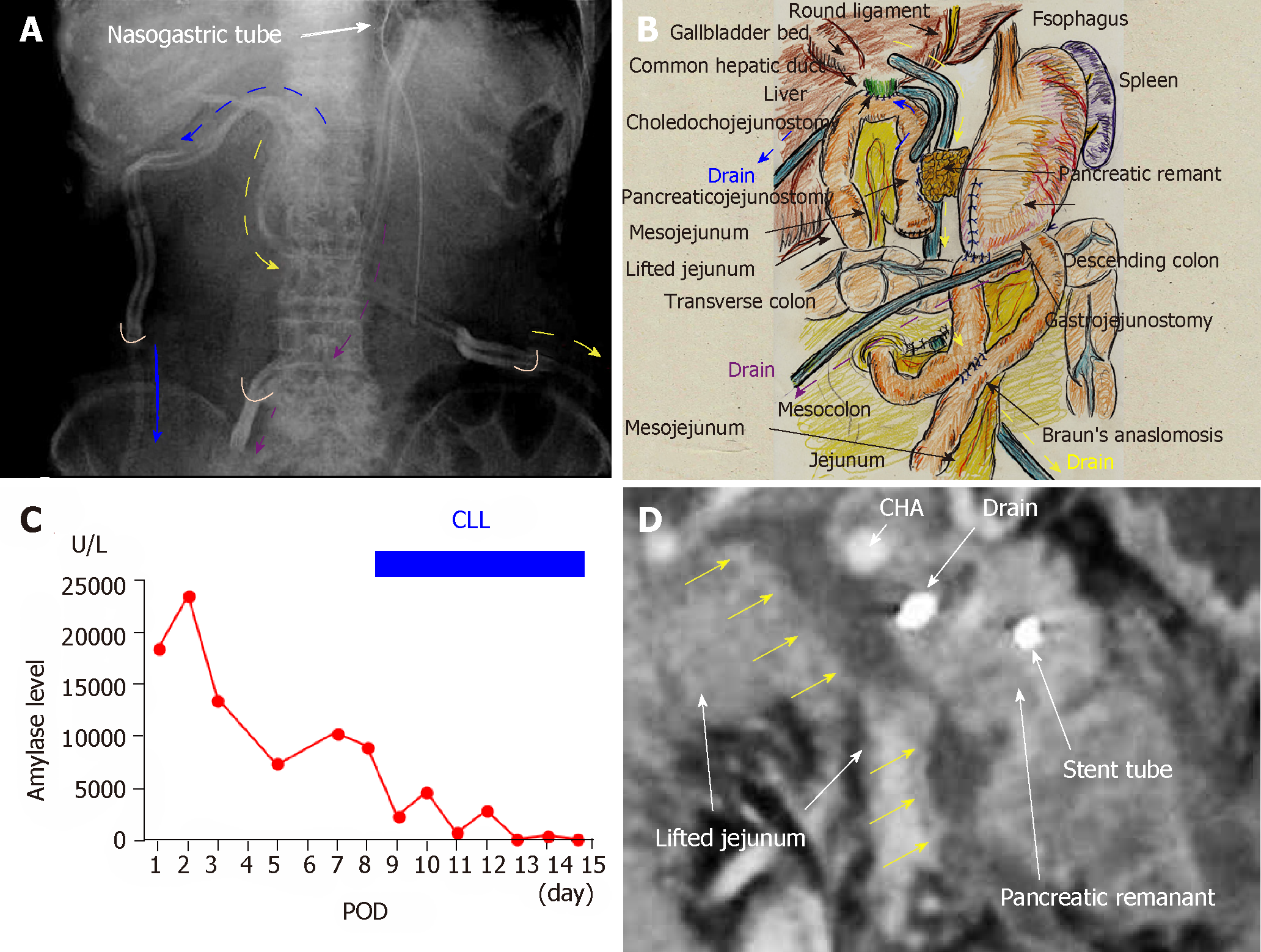
Figure 1 Case 1.
A and B: We placed three drains near the anastomoses of the pancreaticojejunostomy (yellow arrows), choledochojejunostomy (blue arrows), and gastrojejunostomy (purple arrows). For the pancreaticojejunostomy, we ran two drains intentionally through the ventral and dorsal sides (yellow and blue arrows, respectively); C: Pancreatic leakage began early postoperatively, and peak amylase level in the drainage discharge was 23480 U/L. High amylase levels in the drainage discharge were still seen on postoperative day (POD) 8 continuous local lavage (CLL) was initiated on POD 8, and saline volume was increased on POD 12. We continued CLL for 7 d, and amylase levels in the drainage discharge decreased dramatically during that time; D: Contrast computed tomography on POD 8 revealed intractable pancreatic fistula had led to an intraperitoneal abscess around the pancreaticojejunostomy (yellow arrows). CHA: Common hepatic artery; CLL: Continuous local lavage; POD: Postoperative day.
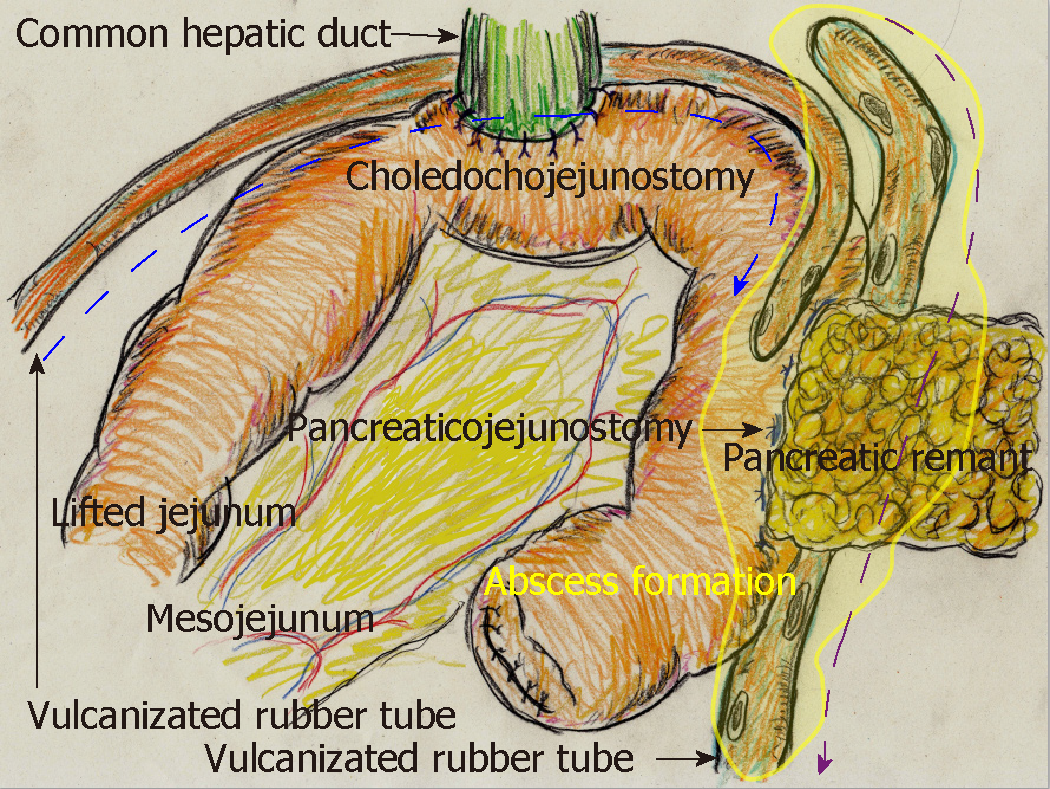
Figure 2 From the ventral tube to the pancreaticojejunostomy (blue arrow), saline was slowly and continuously irrigated into the abscess cavity (yellow area).
In contrast, we used the dorsal tube to the pancreaticojejunostomy (purple arrow) only to drain the irrigated saline.
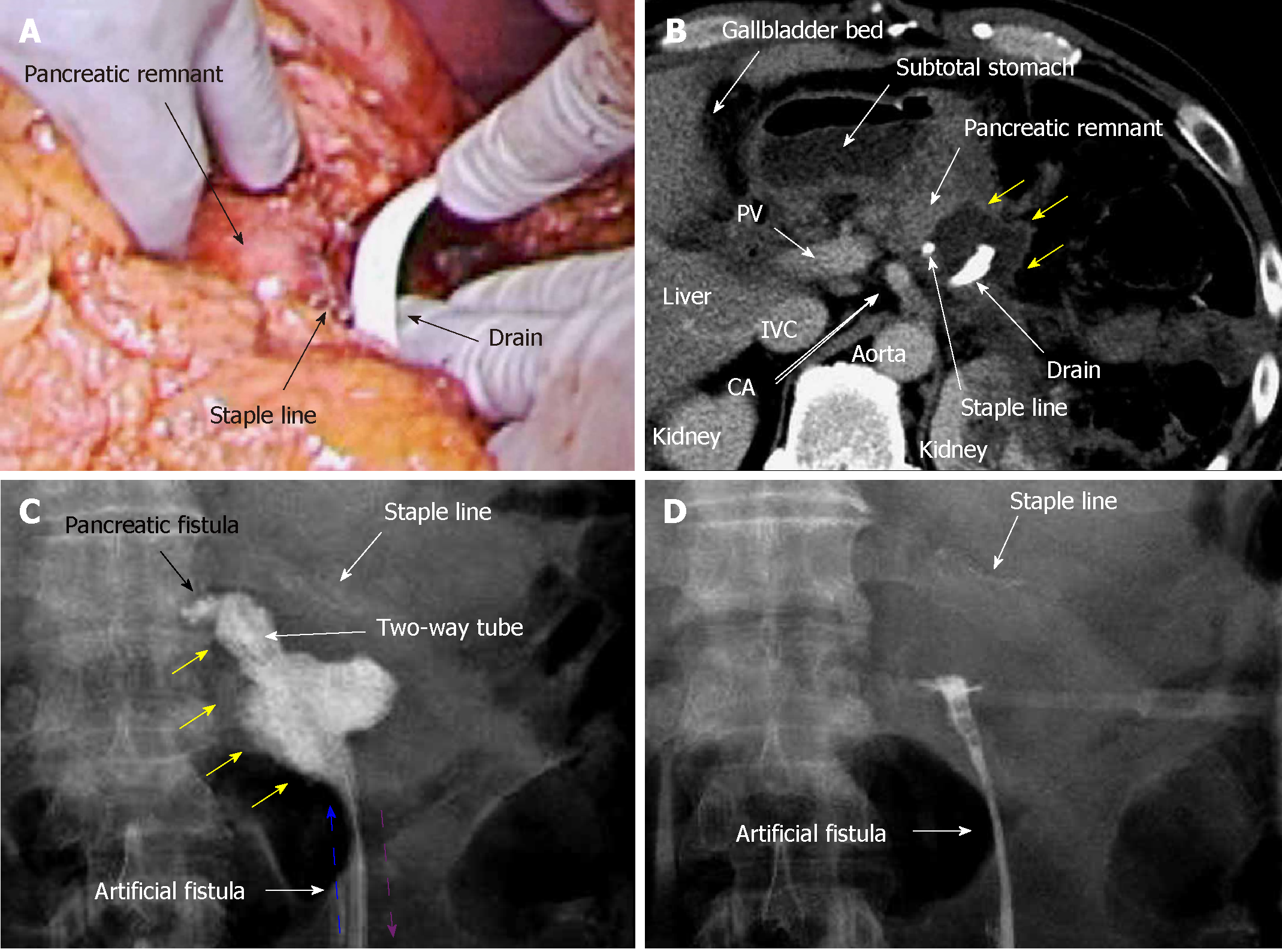
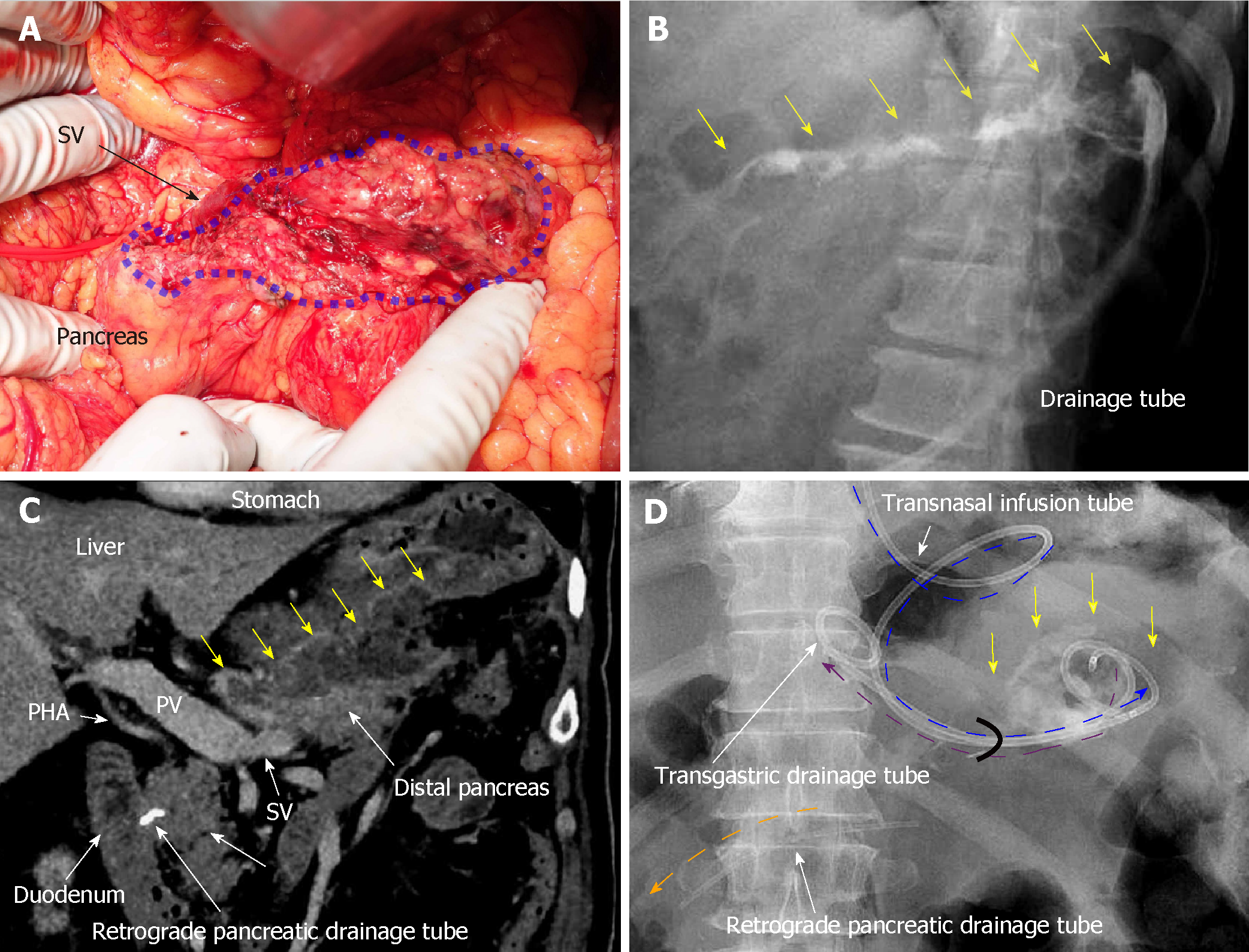
Figure 3 Case 2.
A: Pancreatectomy was performed using a linear stapler, and we placed a drain near the staple line; B: Contrast computed tomography on postoperative day (POD) 9 revealed that intractable pancreatic fistula had led to an intraperitoneal abscess near the staple line (yellow arrows); C: Fistulography via the drain on POD 9 revealed intractable pancreatic fistula (black arrow) and the abscess cavity (yellow arrows). From POD 9, saline irrigation (blue arrow) was continuously injected into the abscess cavity via a two-way tube with the drainage route (purple arrow). Thereafter, amylase levels in the drainage discharge decreased immediately; D: Fistulography on POD 12 revealed that the abscess resolved after 4 d of continuous local lavage. CHA: Common hepatic artery; CLL: Continuous local lavage; IVC: Inferior vena cava; POD: Postoperative day.
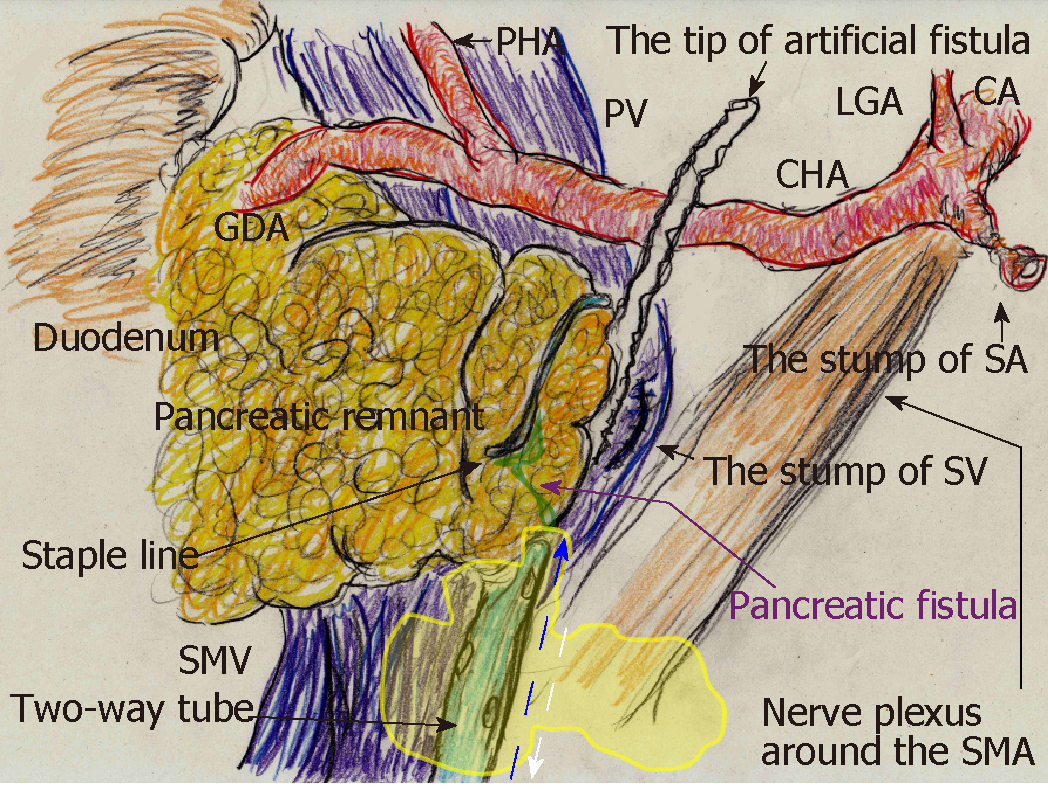
Figure 4 We replaced the drain passing almost through the abscess cavity (yellow area) with a two-way tube.
Saline was continuously injected through the irrigation route (blue arrow), and this two-way tube followed the drainage route (white arrow). To effectively lavage the intractable pancreatic fistula and abscess cavity, the tip position of this tube was appropriately adjusted during fluoroscopic examination. CA: Celiac artery; CHA: Common hepatic artery; GDA: Gastroduodenal artery; LGA: Left gastric artery; PHA: Proper hepatic artery; PV: Portal vein; SA: Splenic artery; SMA: Superior mesenteric artery; SMV: Superior mesenteric vein; SV: Splenic vein.
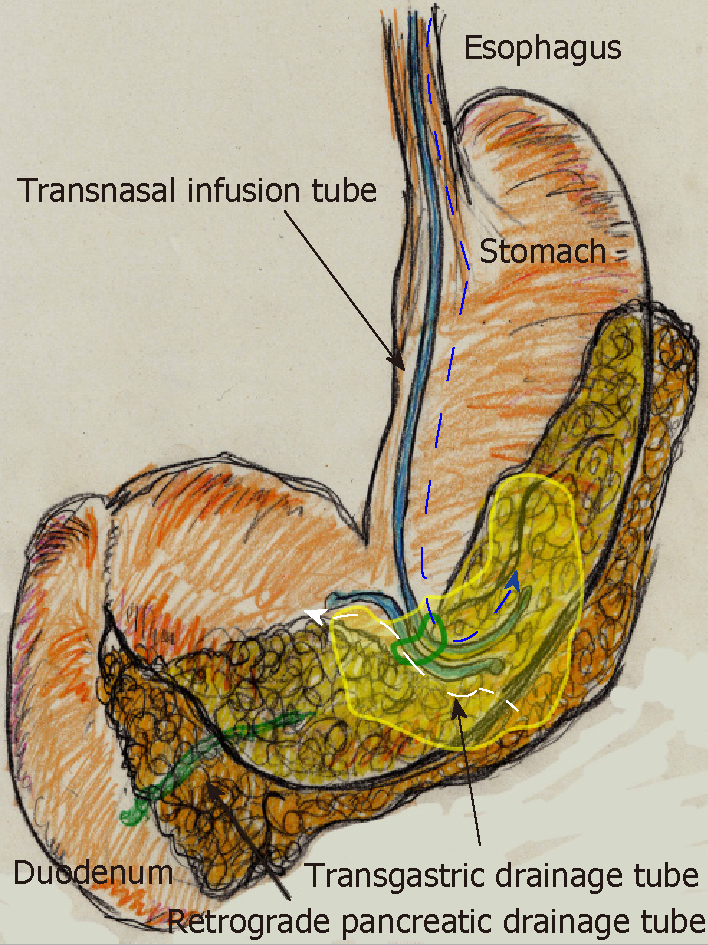
Figure 5 Case 3.
A: Pancreatic parenchyma was preserved with the splenic vein, although the pancreatic parenchyma was widely exposed secondary to the aneurysmectomy (blue area); B: Optimal tube drainage (i.e., intentional placement along the distal pancreas) could not be established because of difficulty using a percutaneous approach, and intractable pancreatic fistula along the distal pancreas (yellow arrows) was seen during fistulography on postoperative day (POD) 13; C: Intractable pancreatic fistula resulted in an abscess and localized peritonitis secondary to bacterial infection, and contrast computed tomography on POD 59 revealed an intraperitoneal abscess along the distal pancreas (yellow arrows); D: A retrograde pancreatic drainage tube (orange arrow) was placed endoscopically on POD 15. On POD 63, continuous local lavage (CLL) of the abscess cavity (yellow arrow) was initiated endoscopically via the transgastric route. Transnasal infusion was initiated and transgastric drainage tubes (purple and blue arrows) were placed endoscopically. From POD 63, saline irrigation was continuously injected via the transnasal infusion tube, and amylase levels in the lavaged fluid began to decrease immediately. Fistulography on POD 70 revealed resolution of the abscess after 1 wk of CLL. CLL: Continuous local lavage; PHA: Proper hepatic artery; POD: Postoperative day; PV: Portal vein; SV: Splenic vein.
Figure 6 Continuous local lavage into the abscess cavity (yellow area) was instituted via transnasal continuous infusion (blue arrow) and endoscopic transgastric drainage (white arrow).
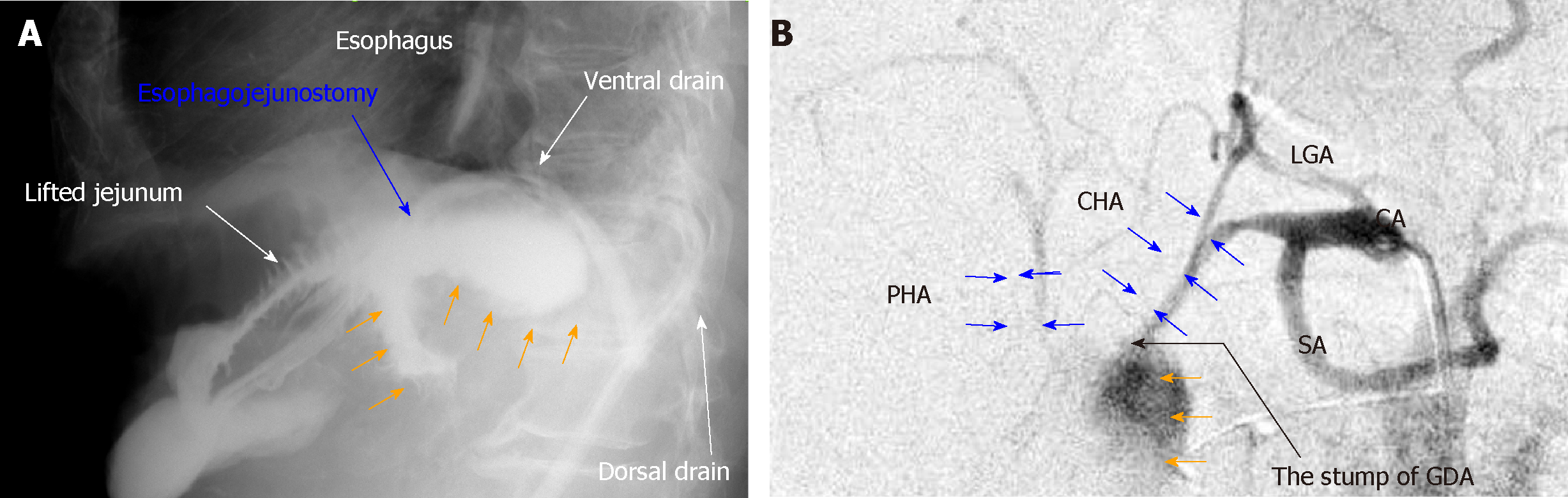
Figure 7 Typical findings of anastomotic leakage and arterial rupture associated with intractable pancreatic fistula.
A: Anastomotic leakage is a potentially fatal complication related to pancreatic juice leakage. Typical findings in postoperative examinations for digestive tract leakage secondary to anastomotic failure caused by intractable pancreatic fistula are shown; B: Arterial rupture of a pseudoaneurysm is a fatal complication related to pancreatic juice leakage. Typical angiographic findings for arterial pseudoaneurysm rupture caused by intractable pancreatic fistula are shown. CA: Celiac artery; CHA: Common hepatic artery; GDA: Gastroduodenal artery; LGA: Left gastric artery; PHA: Proper hepatic artery; POD: Postoperative day; SA: Splenic artery.
- Citation: Hori T, Ogawa K, Yamamoto H, Harada H, Matsumura K, Yamamoto M, Yamada M, Yazawa T, Kuriyama K, Tani M, Yasukawa D, Kamada Y, Aisu Y, Tani R, Aoyama R, Nakayama S, Sasaki Y, Nishimoto K, Zaima M. Impact of continuous local lavage on pancreatic juice-related postoperative complications: Three case reports. World J Clin Cases 2019; 7(17): 2526-2535
- URL: https://www.wjgnet.com/2307-8960/full/v7/i17/2526.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i17.2526