©The Author(s) 2018.
World J Clin Cases. Sep 6, 2018; 6(9): 284-290
Published online Sep 6, 2018. doi: 10.12998/wjcc.v6.i9.284
Published online Sep 6, 2018. doi: 10.12998/wjcc.v6.i9.284
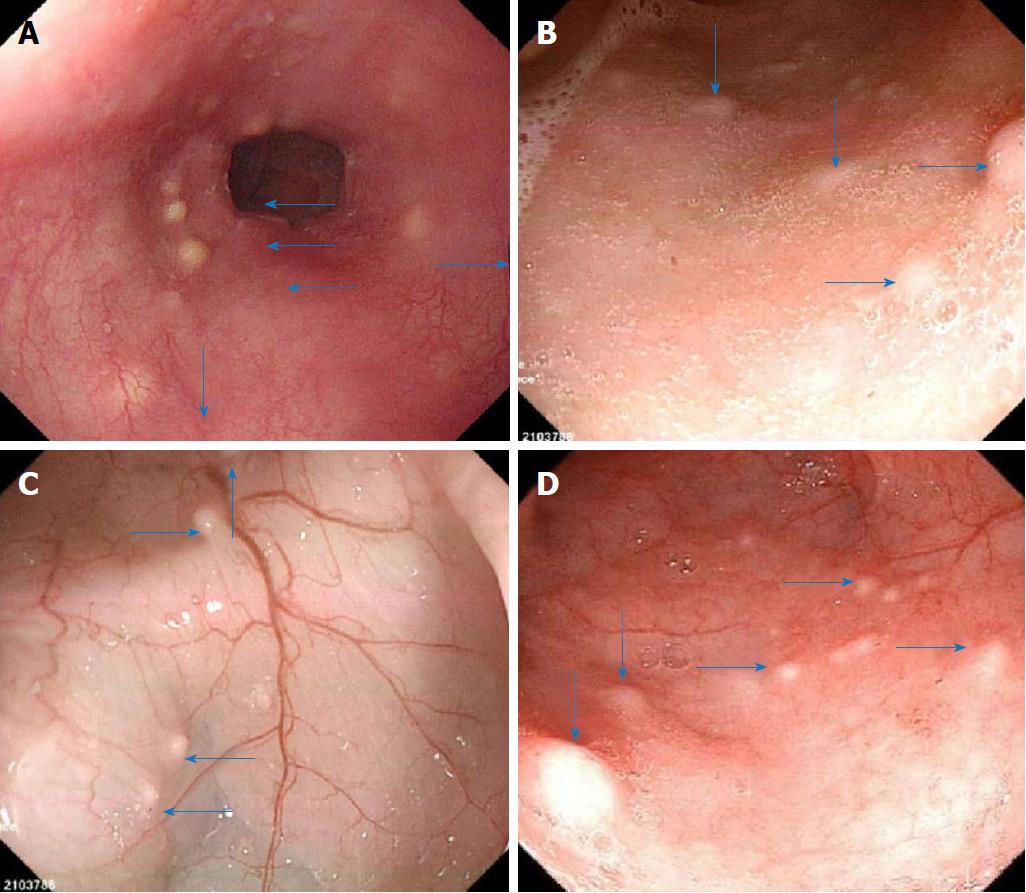
Figure 1 Representative images of enteroscopy at admission.
A: Nodular protuberances (arrows) in the esophagus; B: Nodular protuberances (arrows) in the ileum; C: Nodular protuberances (arrows) in the hepatic area of the colon; D: Nodular protuberances (arrows) in the rectum.
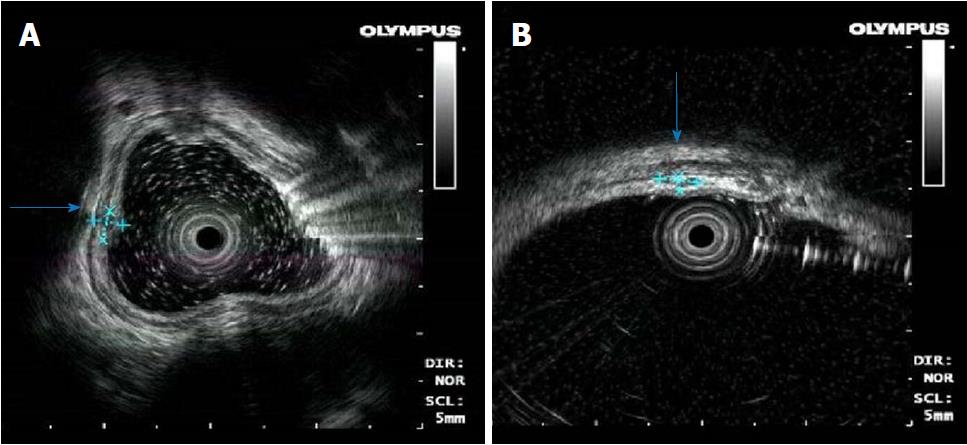
Figure 2 Images of endoscopic ultrasonography.
A: Nodular protuberances in the esophagus stemming from hypoechoic lesions of the submucosa, and the layer of origin was clear; B: Nodular protuberances in the colon stemming from the submucosa, partially invading the intrinsic myometrium with a hypoechoic structure, which is partially hypoechoic fusion and inhomogeneous echo.
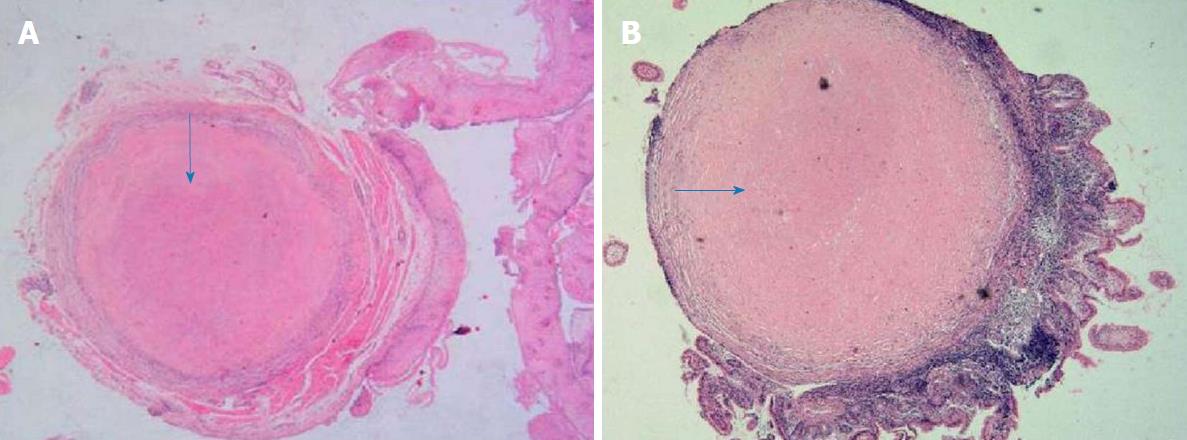
Figure 3 Pathological examination with hematoxylin and eosin staining.
A: The central portion of an esophagus biopsy sample containing a homogeneous powder and dyed structure (arrows), which is surrounded by inflammatory cells and fibrous tissues (magnification 10 × 4); B: The biopsy sample of ileum containing multiple homogeneous powder dyeing (arrow) without structural small nodules in the submucosal layer (MAGNIFICATION 10 × 4).
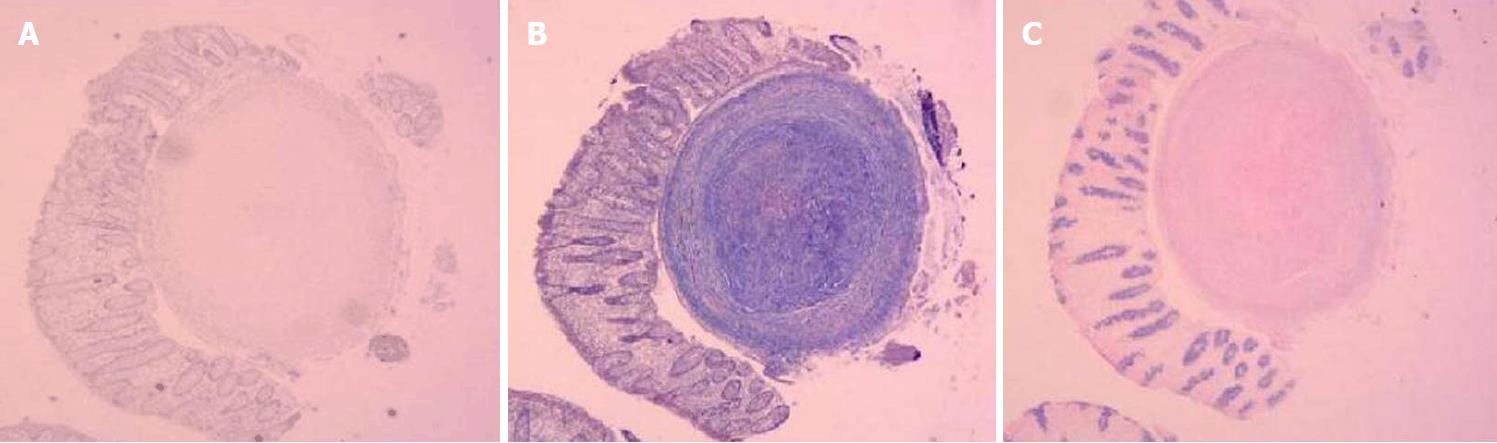
Figure 4 Positive staining of Esophagus biopsy sample.
A: With Congo red; B: With Masson blue; C: With Periodic Acid-Schiff.
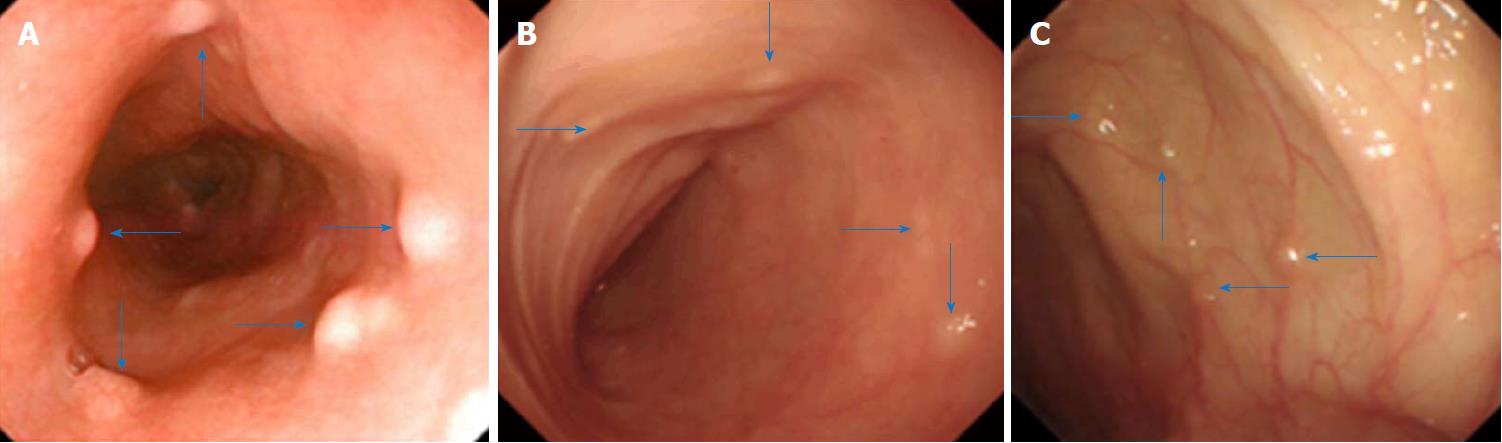
Figure 5 Representative images of enteroscopy three years after admission.
A: Nodular protuberances (arrows) in the esophagus; B: Nodular protuberances (arrows) in the ileum; C: Nodular protuberances (arrows) in the colon.
- Citation: Liu YP, Jiang WW, Chen GX, Li YQ. Case report and review of the literature of primary gastrointestinal amyloidosis diagnosed with enteroscopy and endoscopic ultrasonography. World J Clin Cases 2018; 6(9): 284-290
- URL: https://www.wjgnet.com/2307-8960/full/v6/i9/284.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i9.284