Copyright
©The Author(s) 2024.
World J Clin Cases. Sep 16, 2024; 12(26): 5974-5982
Published online Sep 16, 2024. doi: 10.12998/wjcc.v12.i26.5974
Published online Sep 16, 2024. doi: 10.12998/wjcc.v12.i26.5974
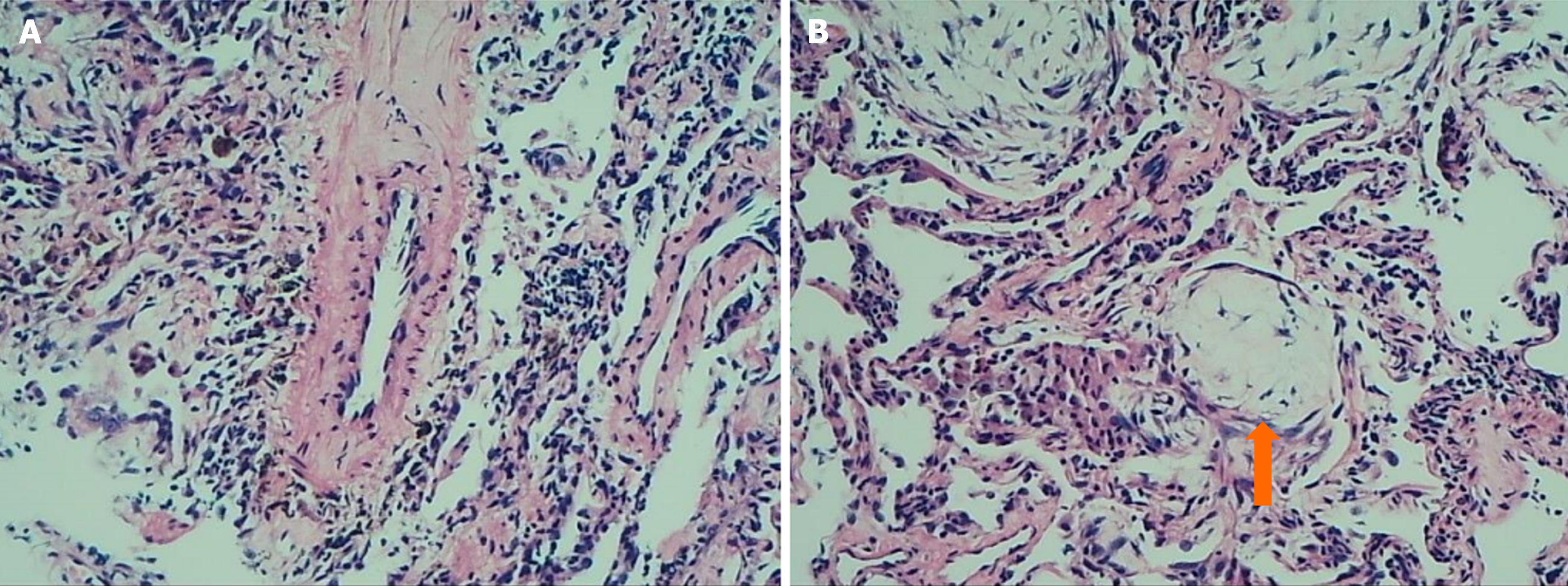
Figure 1
The lung biopsy showed alveolar atrophy, interstitial fibrosis, scattered inflammatory cell infiltration, and focal organizing pneumonia changes, and focal presence of Masson's bodies (indicated by arrows) (Hematoxylin-eosin staining × 100 magnification).
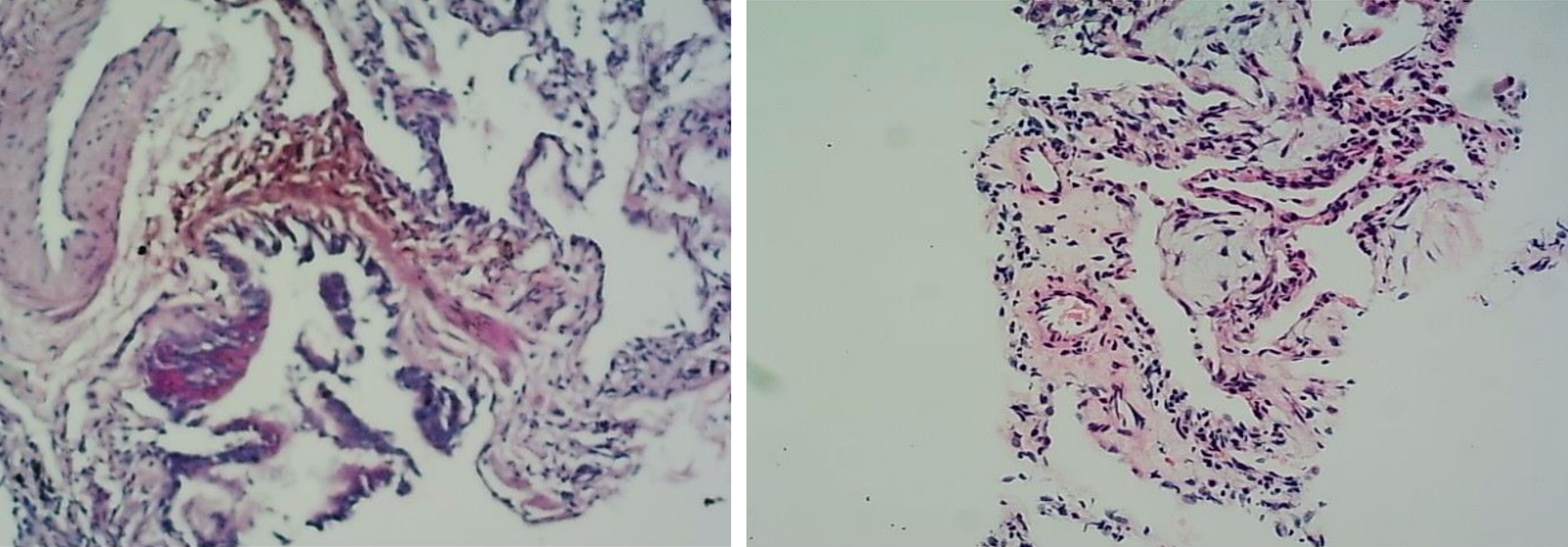
Figure 2
Special staining, including acid-fast, periodic acid shiff, and hexamine-silver, did not detect pathogenic bacteria (Hematoxylin-eosin staining × 100 magnification).
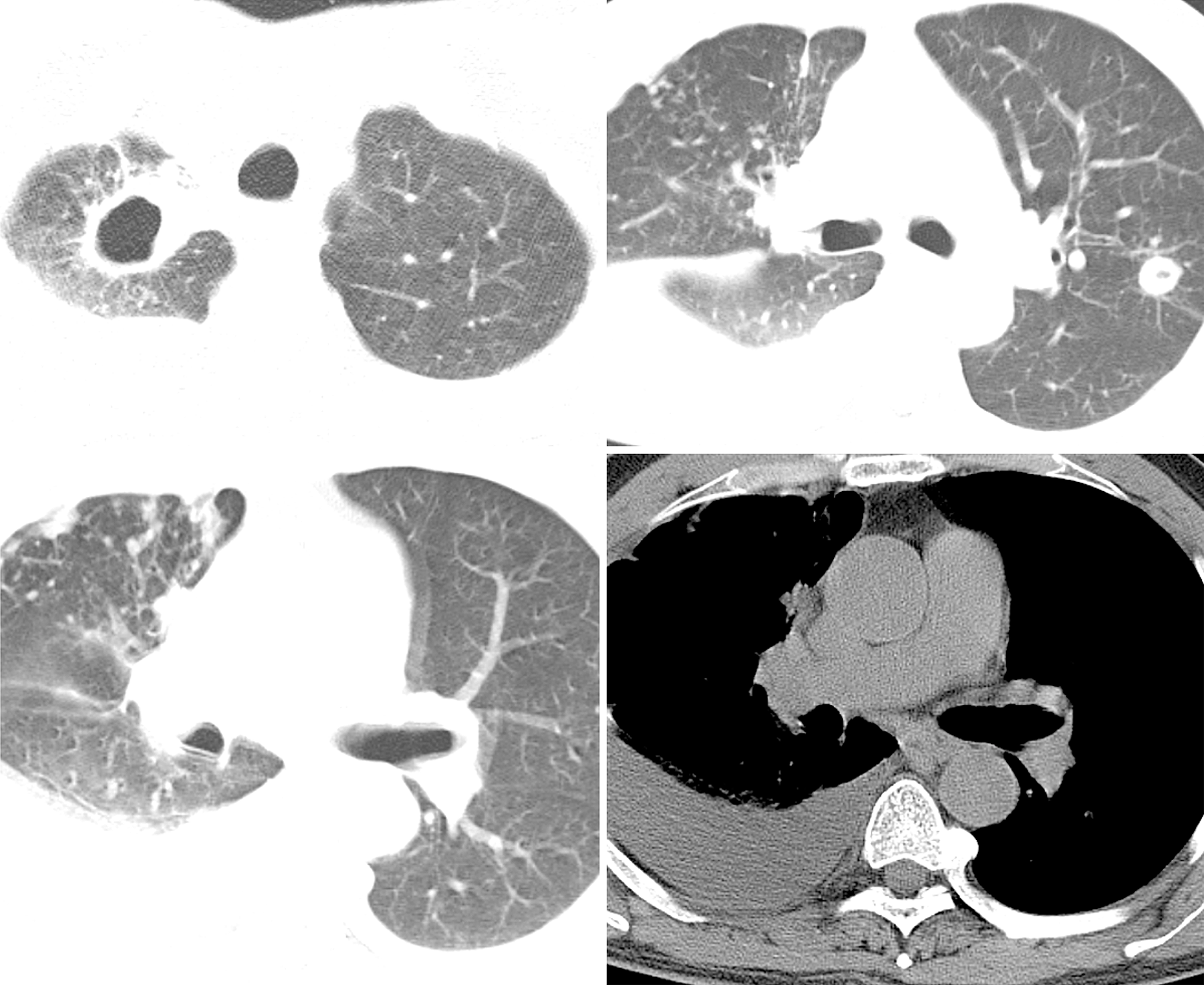
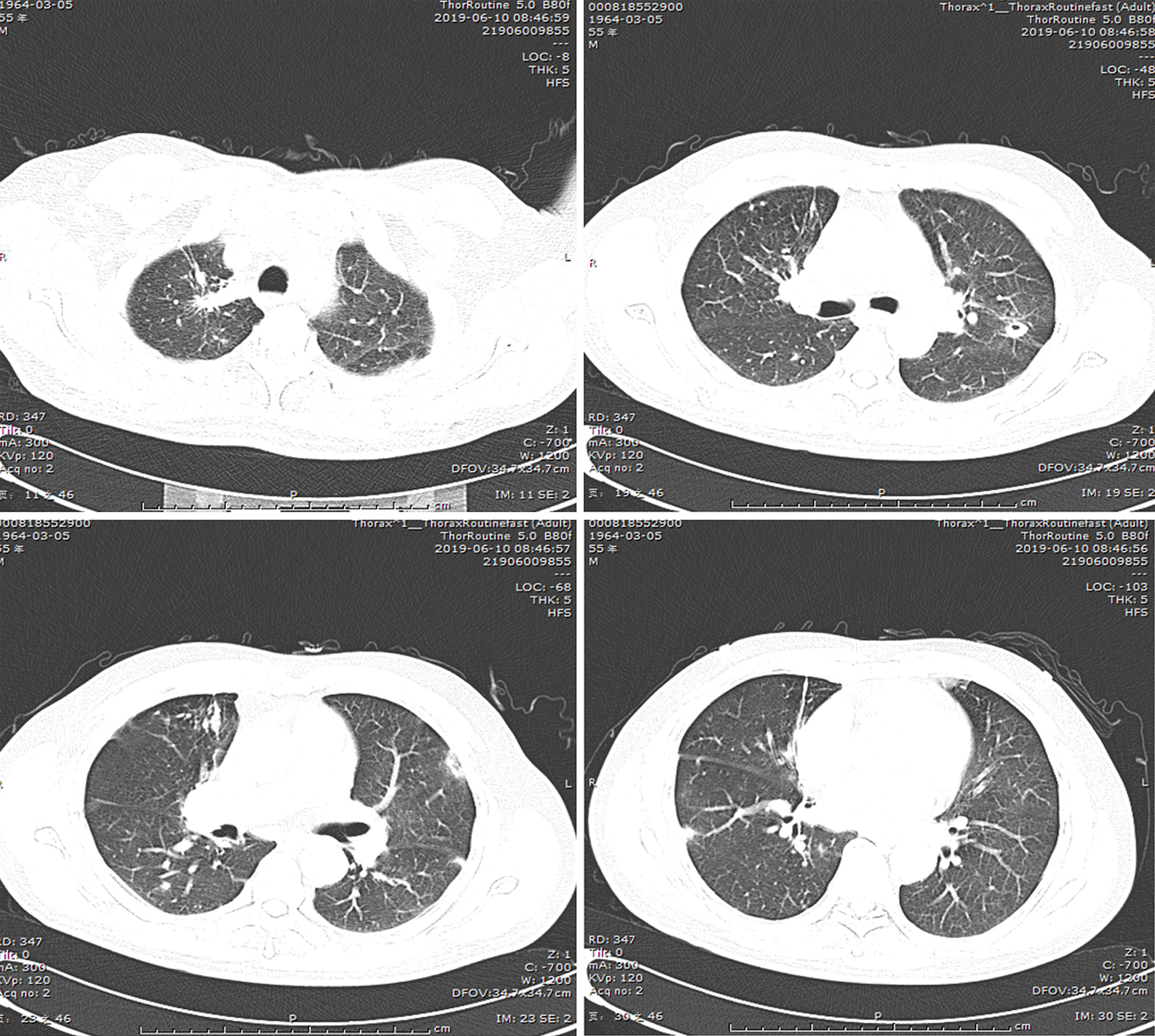
Figure 3 After admission, the computed tomography scan unveiled multiple nodules and cavities in both lungs, suggesting infection, particularly tuberculosis.
Right pleurisy and pleural effusion were noted.
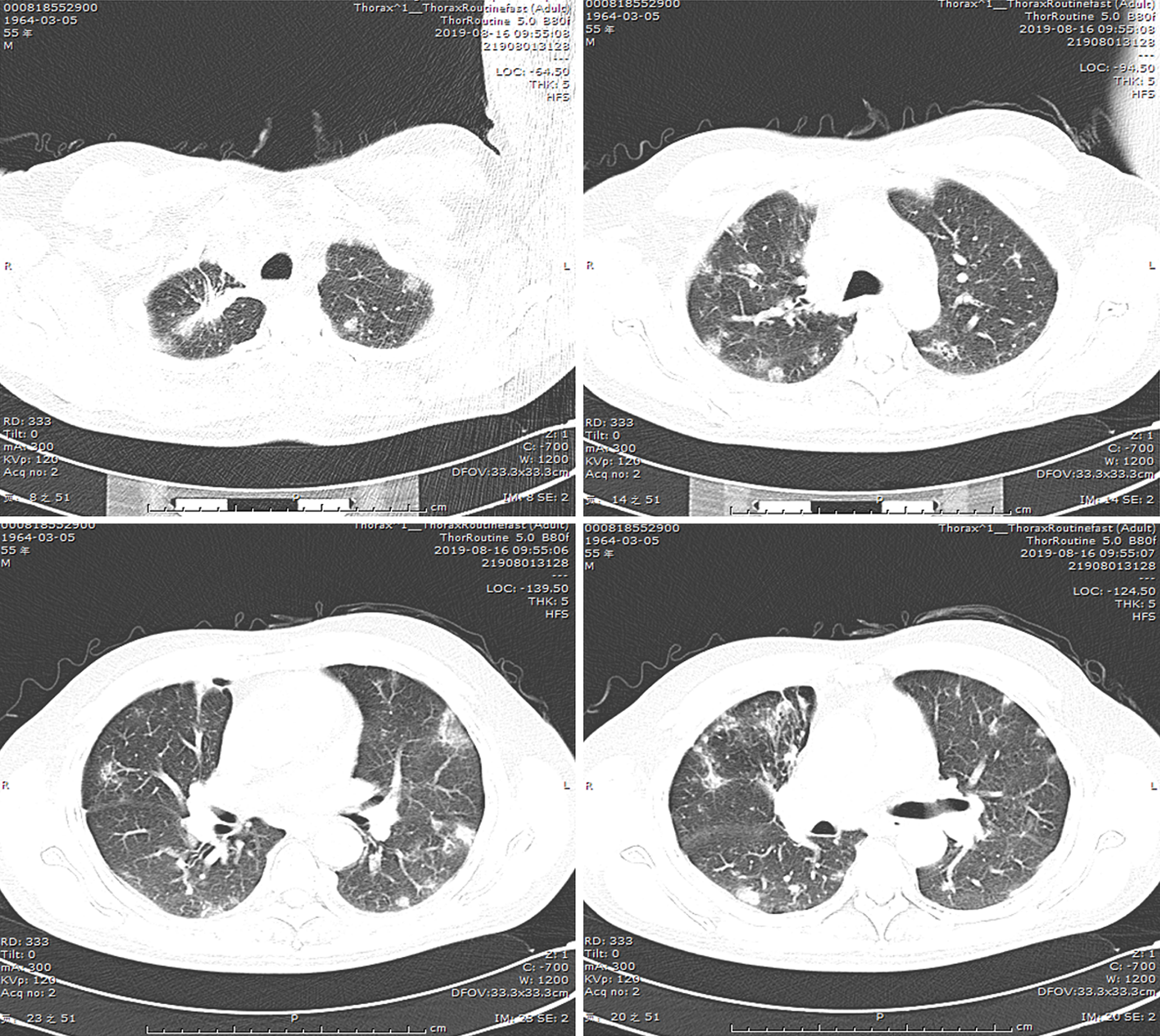
Figure 4
Following a 5-month course of anti-tuberculosis treatment, the subsequent computed tomography scan revealed complete closure of the cavity in the right upper lung, absorbtion of pleural effusion in the right hemithorax, and significant reduction in size of the cavity in the lower left lung.
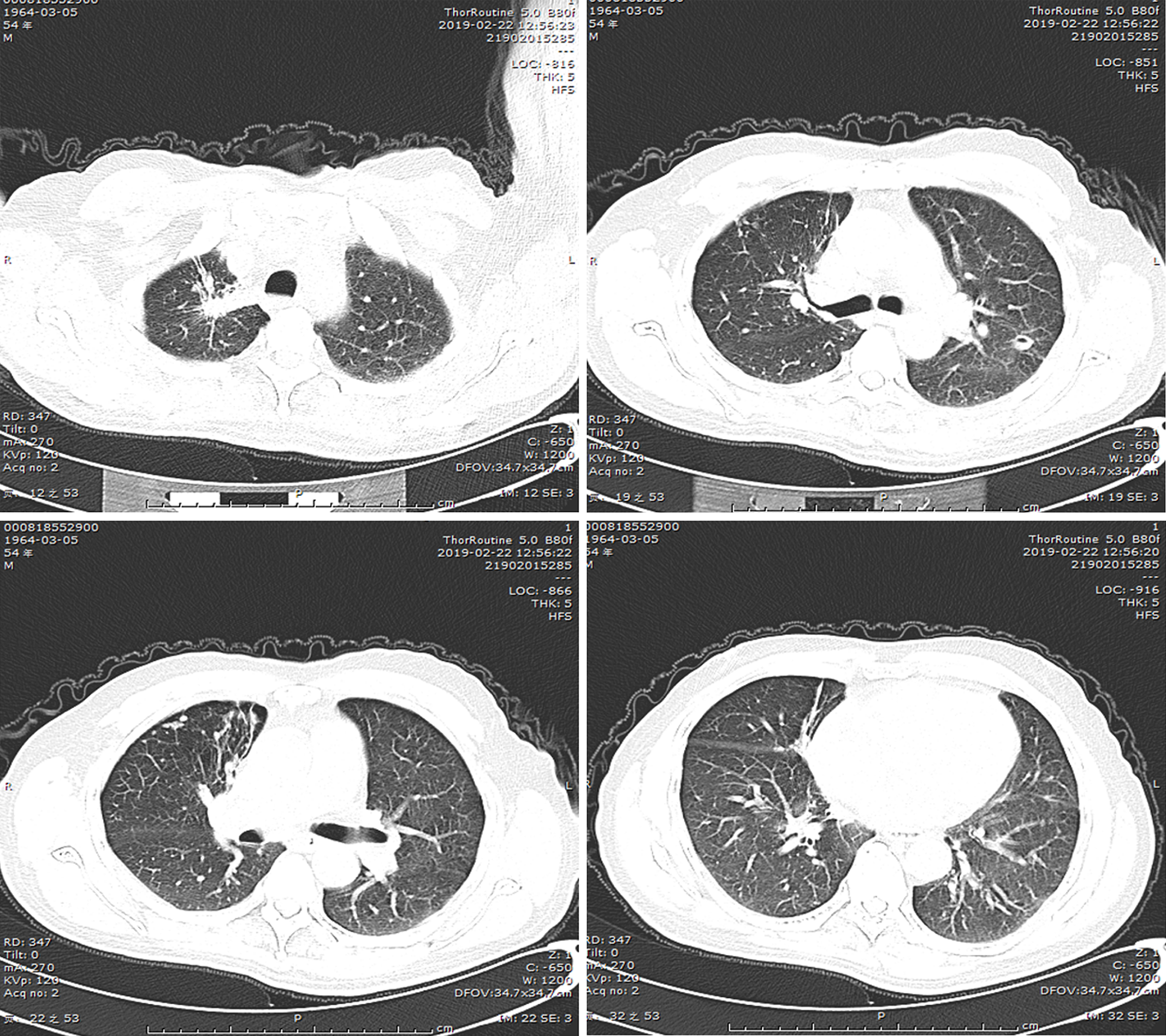
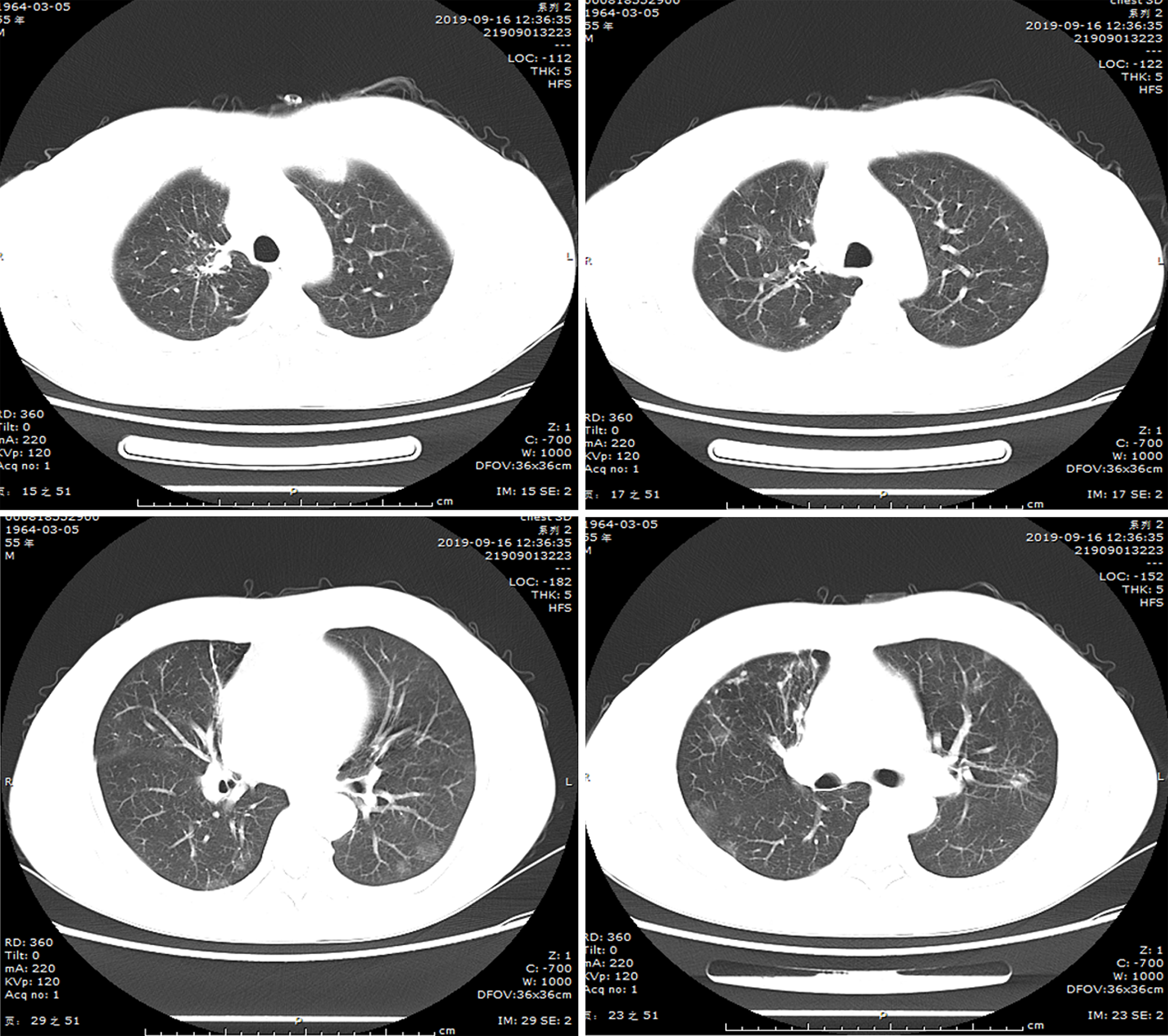
Figure 5
A follow-up lung computed tomography scan in June 2019 revealed new multifocal subpleural ground-glass opacities in both lungs.
Figure 6
On August 16, 2019, another lung computed tomography reexamination indicated a significant increase in ground-glass opacities in both lungs.
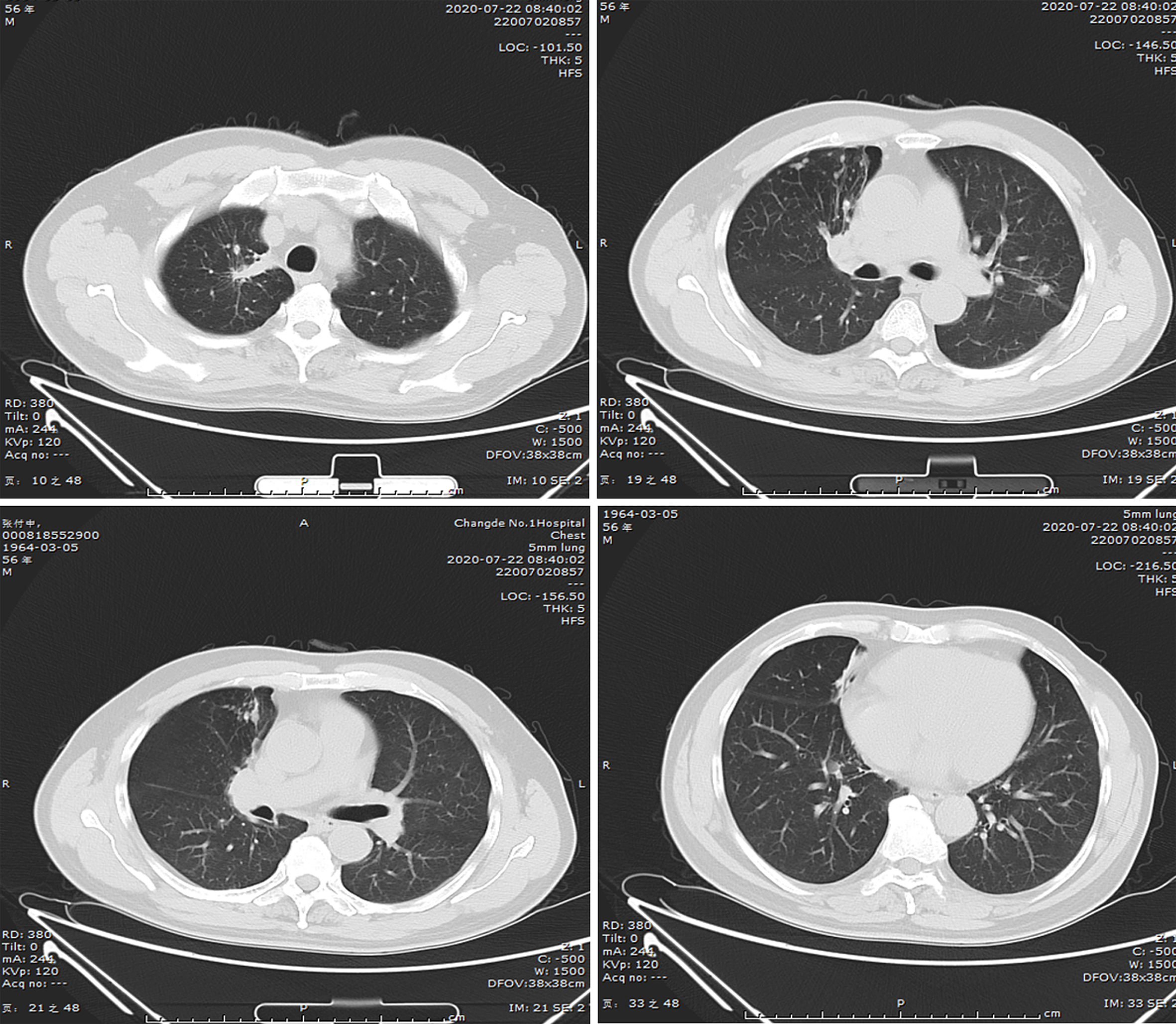
Figure 7
After undergoing hormone therapy, the follow-up examination revealed a significant improvement in the subpleural ground-glass opacities observed in both lungs.
Figure 8
No new lesions were detected on computed tomography follow-up one year after treatment discontinuation.
- Citation: Liu M, Dong XY, Ding ZX, Wang QH, Li DH. Organizing pneumonia secondary to pulmonary tuberculosis: A case report. World J Clin Cases 2024; 12(26): 5974-5982
- URL: https://www.wjgnet.com/2307-8960/full/v12/i26/5974.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i26.5974