©The Author(s) 2023.
World J Clin Cases. Mar 16, 2023; 11(8): 1878-1887
Published online Mar 16, 2023. doi: 10.12998/wjcc.v11.i8.1878
Published online Mar 16, 2023. doi: 10.12998/wjcc.v11.i8.1878
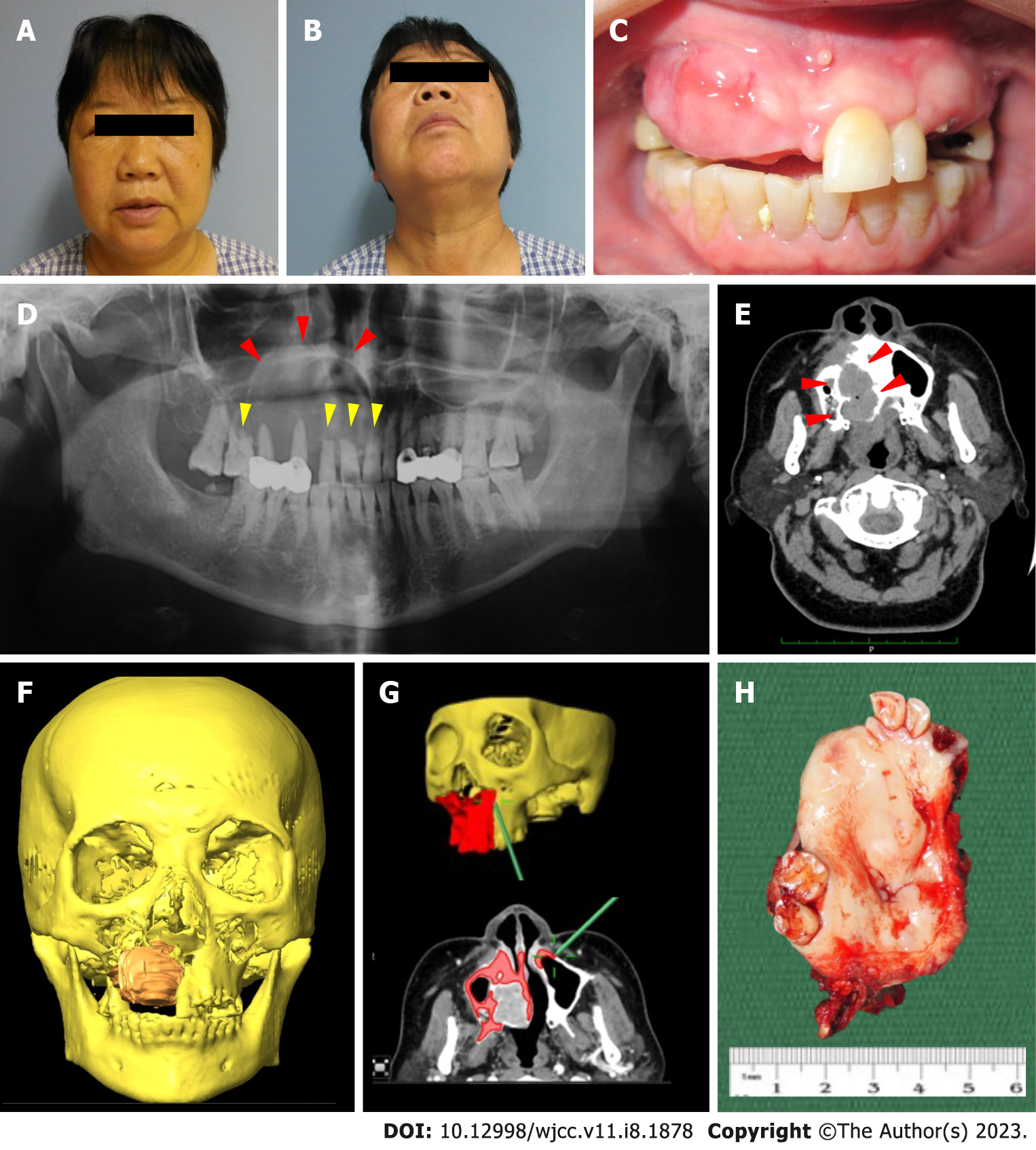
Figure 1 Clinical and radiological findings of the current case.
A and B: A thorough extra-oral and intra-oral examination was performed. The patient presented with a right facial swelling without overlying skin changes. The swelling was diffuse, firm, and non-tender, causing obliteration of the right nasolabial fold. Mouth opening was not restricted and there was no palpable cervical lymphadenopathy. There were no neurosensory changes to the right infraorbital region; C: Intra-oral examination showed an irregular mass at the anterior maxilla extending from the tooth 11 to 15 region and palatally crossing the midline into the left palate. There was no obliteration of the buccal sulcus. The swelling was firm and nontender, with a non-ulcerated overlying mucosa. The adjacent teeth showed no marked increase in mobility and no fluid discharge was noted on palpation of the swelling; D: The initial dental panoramic tomogram showed a radiolucent lesion of the right maxilla extending into the right maxillary sinus (red arrows) with marked root resorption (yellow arrows); E: Computed tomography scan with contrast showed an infiltrating lesion on the right maxilla with obvious bony destruction involving the right hard palate and right inferior turbinate (red arrows); F: Tumor mapping showing an expansile mass perforating both the buccal and palatal bone; G: The osteotomy lines were planned and confirmed using the intraoperative navigation system; H: Gross specimen of the lesion.
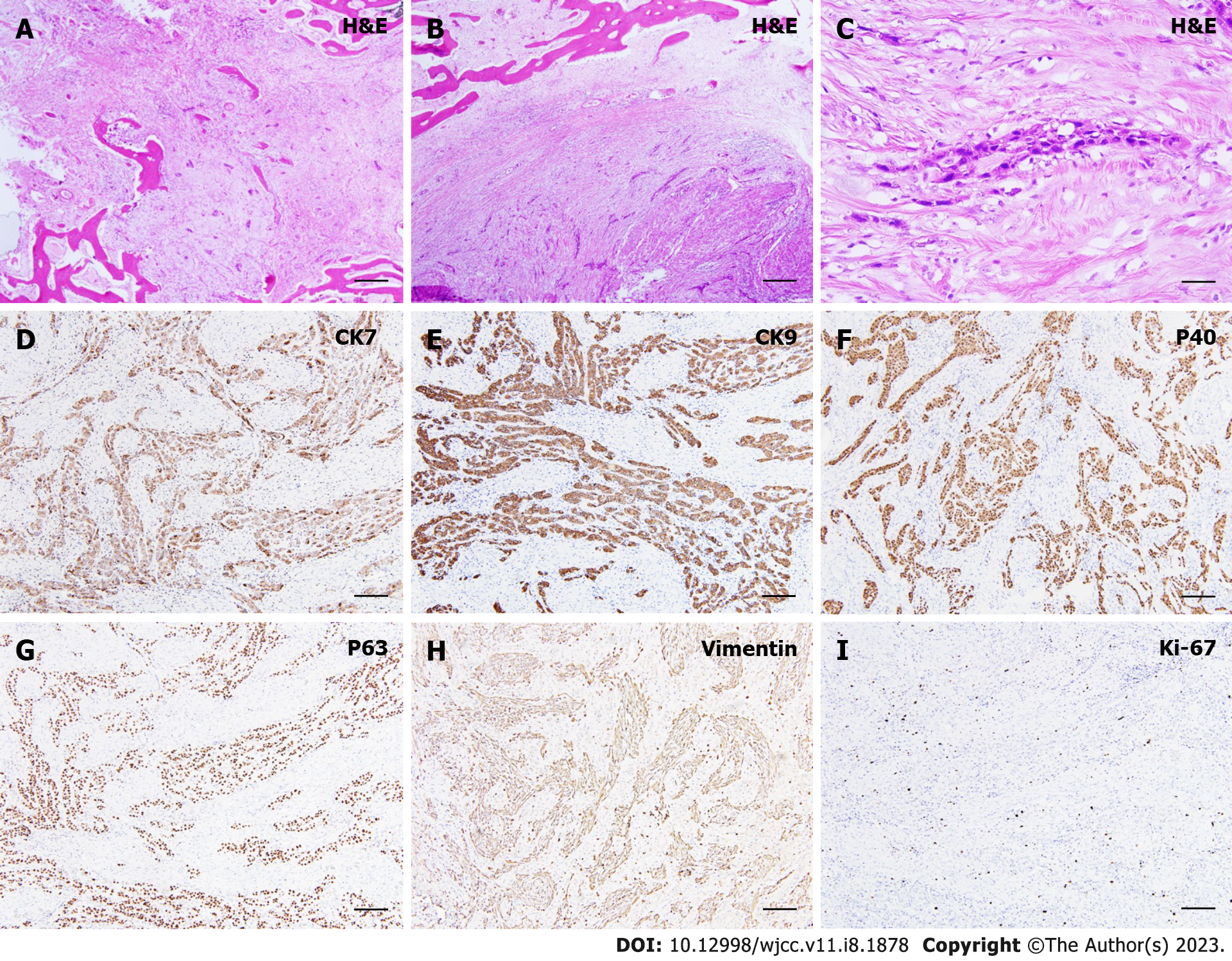
Figure 2 Histological findings of the present case.
A and B: Histological view focusing on small cords of epithelial cells of odontogenic origin immersed in a diffused sclerotic and collagenous stroma [hematoxylin and eosin (H&E), original magnification: × 20]; C: Evidence of vascular invasion (H&E, original magnification: × 20); D: Focal positivity in tumor cells to immunohistochemical staining for cytokeratin 7 (CK7) (original magnification: × 20); E: Immunohistochemistry for expression of CK19 demonstrating diffuse, uniform positivity in the neoplastic cells (original magnification: × 20); F: Immunohistochemistry demonstrating that the tumor cells expressed p40 (original magnification: × 20); G: Strong, diffuse positivity was seen for the expression of p63 (original magnification: × 20); H: The tumor cells were stained negative for vimentin (original magnification: × 20); I: Low proliferative activity (Ki-67) was seen (approximately 5%-10%) (original magnification: × 20). CK: Cytokeratin; H&E: Hematoxylin and eosin.
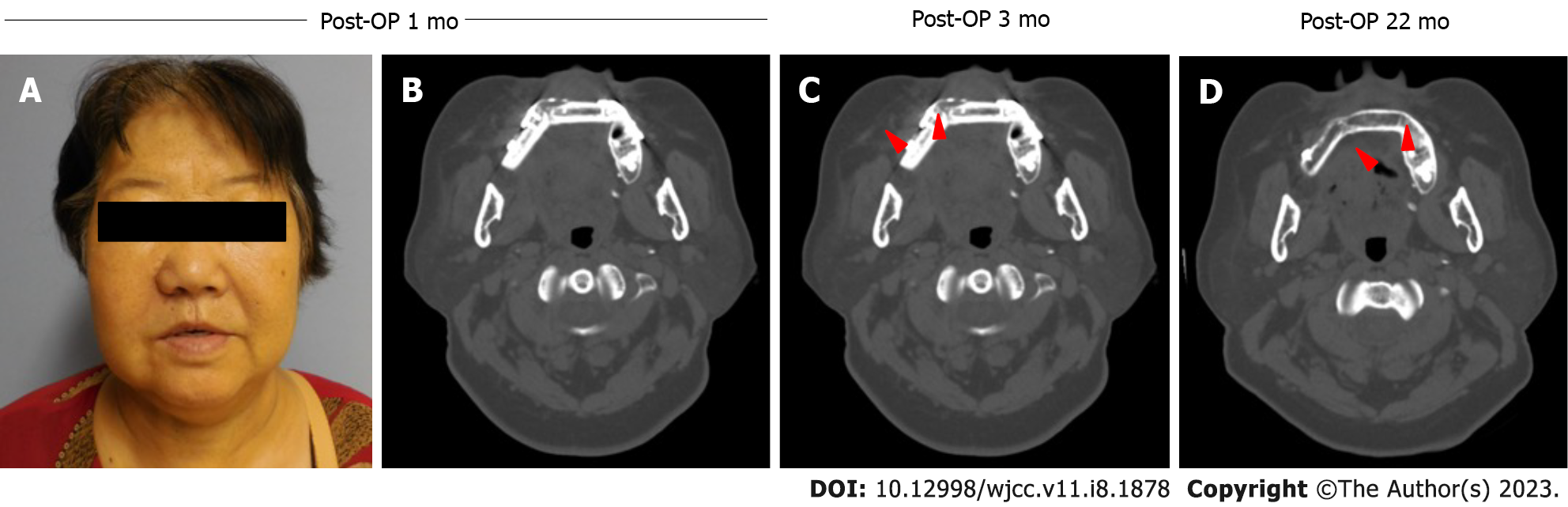
Figure 3 Post-operative clinical and radiological findings.
A and B: At postoperative 1-mo review, the patient was satisfied with her appearance and functions; C: The fibular segments appeared to be in the process of osseointegration at postoperative 3mo review (red arrows); D: No sign of recurrence observed at postoperative 22-mo review. Post-OP: Post-operative.
- Citation: Soh HY, Zhang WB, Yu Y, Zhang R, Chen Y, Gao Y, Peng X. Sclerosing odontogenic carcinoma of maxilla: A case report. World J Clin Cases 2023; 11(8): 1878-1887
- URL: https://www.wjgnet.com/2307-8960/full/v11/i8/1878.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i8.1878