©The Author(s) 2023.
World J Clin Cases. Mar 6, 2023; 11(7): 1434-1441
Published online Mar 6, 2023. doi: 10.12998/wjcc.v11.i7.1434
Published online Mar 6, 2023. doi: 10.12998/wjcc.v11.i7.1434
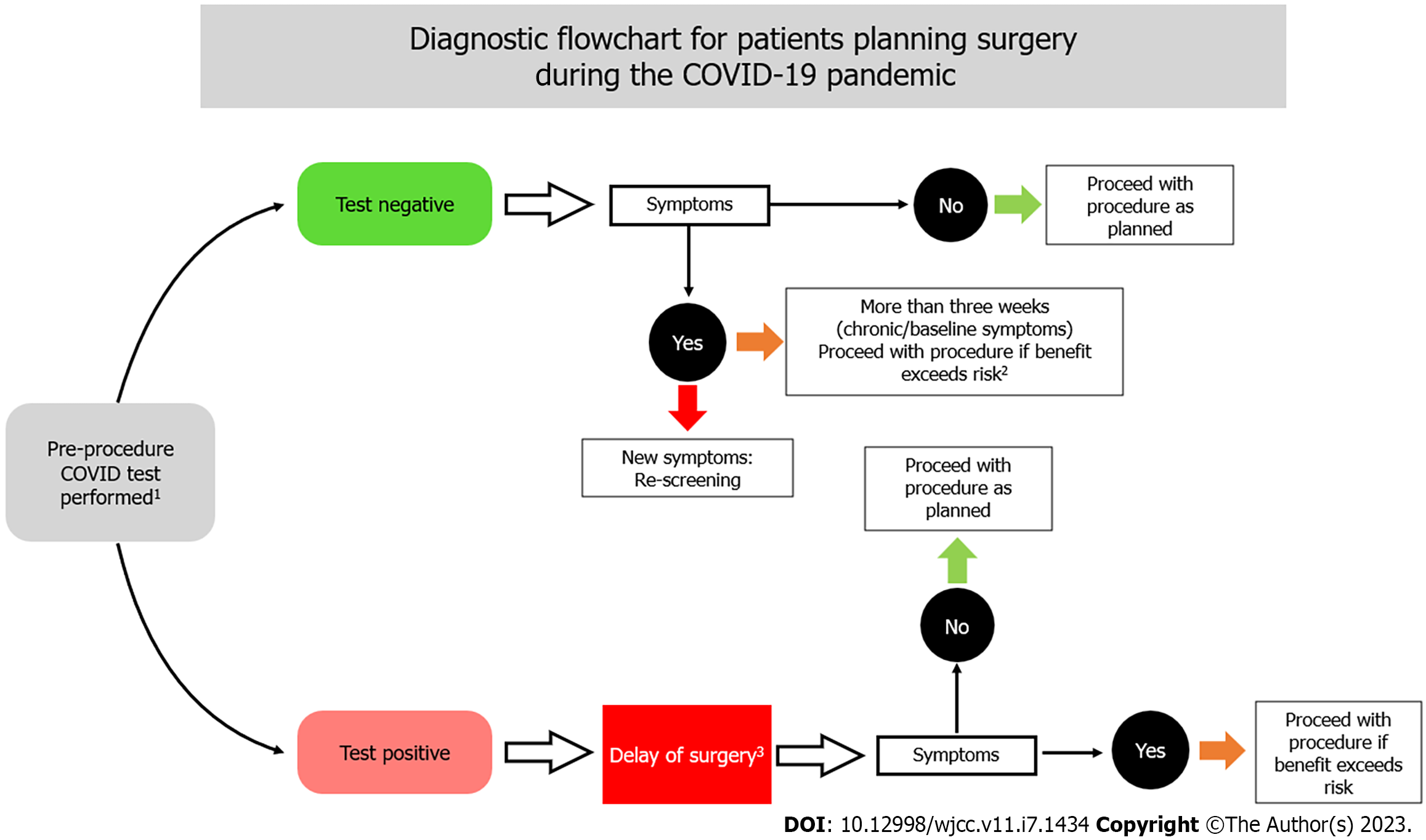
Figure 1 Diagnostic flowchart for patients planning surgery during the coronavirus disease 2019 pandemic.
1All coronavirus disease 2019 (COVID-19) positive or suspected patients requiring surgical intervention should be treated as positive cases until proven otherwise[17]. 2Patients with perioperative severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection are at increased risk of death and pulmonary complications after surgery[20]. 3There is to date only limited evidence on the optimal timing of surgery after SARS-CoV-2 infection[19]. A prospective cohort study found that surgery performed ≥ 4 wk after a positive SARS-CoV-2 swab result may be associated with a lower risks of pulmonary complications and postoperative mortality[21]. COVID-19: Coronavirus disease 2019.
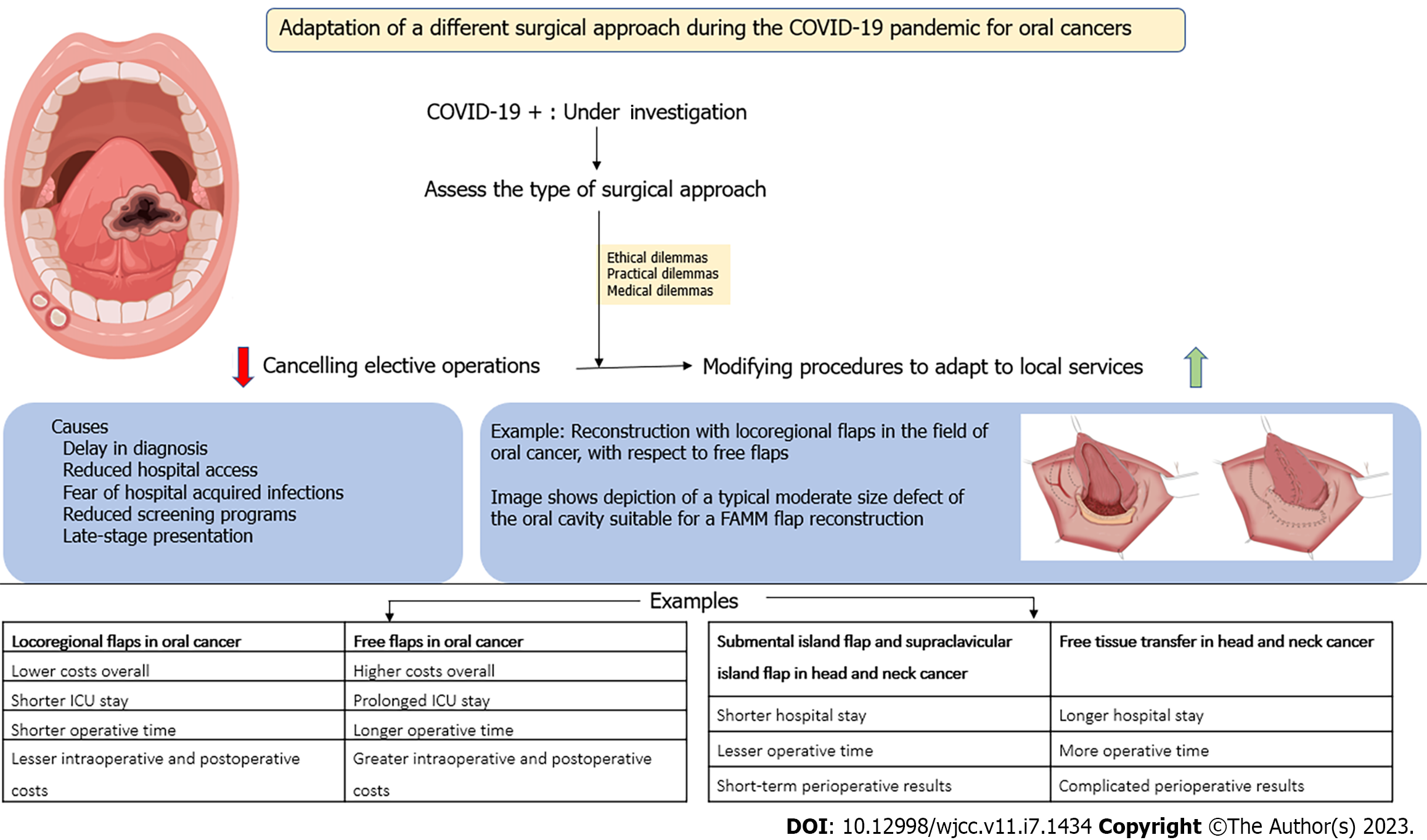
Figure 2 Schematic representation of changes in the choice of surgical techniques for the management of head and neck cancer during the coronavirus disease 2019 pandemic.
COVID-19: Coronavirus disease 2019; ICU: Intensive care unit; FAMM: The facial artery musculomucosal.
- Citation: Lizambri D, Giacalone A, Shah PA, Tovani-Palone MR. Reconstruction surgery in head and neck cancer patients amidst the COVID-19 pandemic: Current practice and lessons for the future. World J Clin Cases 2023; 11(7): 1434-1441
- URL: https://www.wjgnet.com/2307-8960/full/v11/i7/1434.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i7.1434