©The Author(s) 2023.
World J Clin Cases. Feb 6, 2023; 11(4): 859-865
Published online Feb 6, 2023. doi: 10.12998/wjcc.v11.i4.859
Published online Feb 6, 2023. doi: 10.12998/wjcc.v11.i4.859
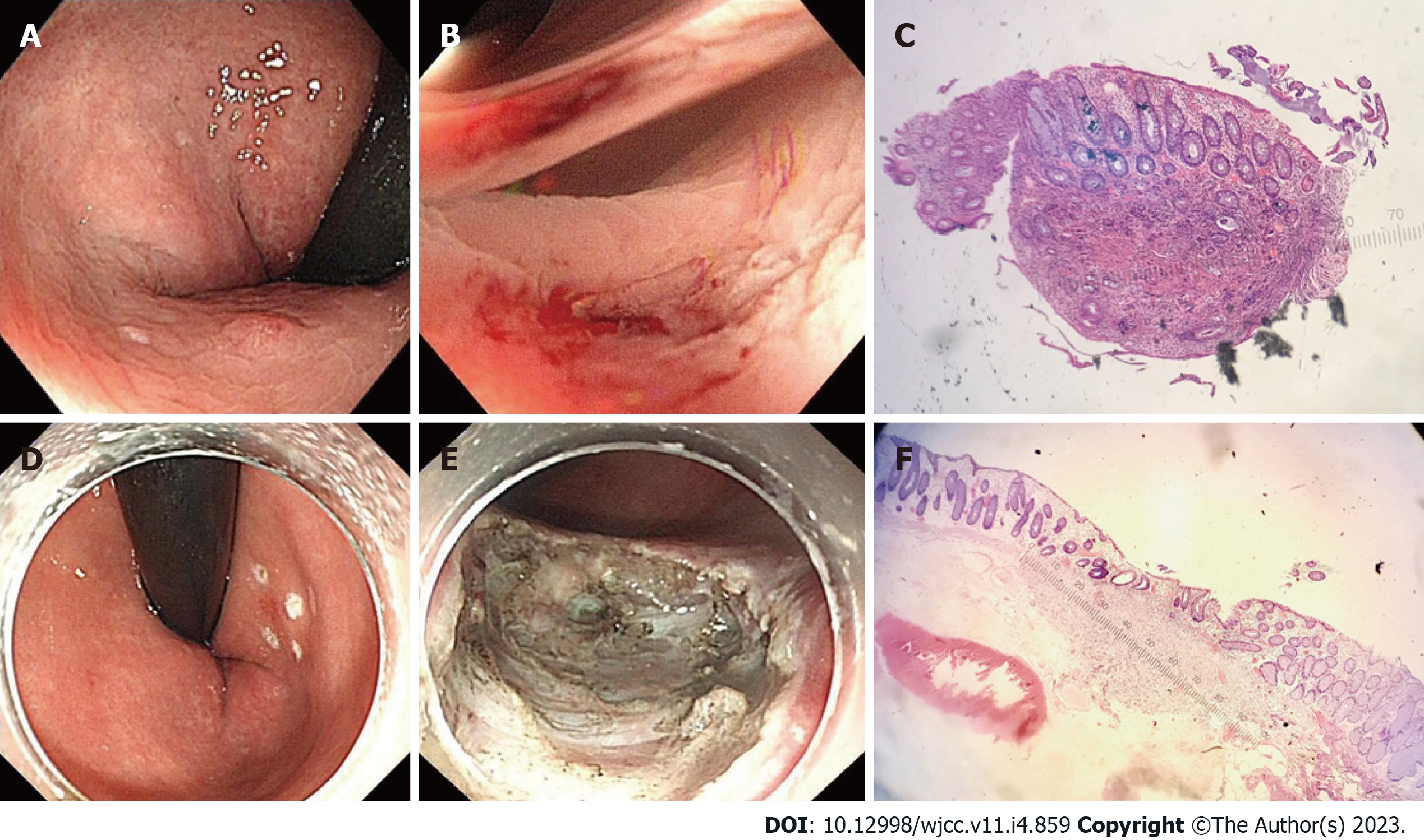
Figure 1 The endoscopic manifestation of the rectal neuroendocrine tumor.
A-C: Rectal neuroendocrine tumor (rNET): under a white light endoscope, the surface is smooth, sessile, and the same color as the surrounding mucosa (A); after biopsy forceps (B); the first hematoxylin and eosin (H&E) stained pathological smear after the tumor was removed by biopsy forceps (C, × 40). Endoscopic submucosal dissection (ESD) remedial treatment; D-F: Under white light endoscope, before ESD (D); after additional ESD (E); HE stained pathological smears of specimens after ESD (F, × 40).
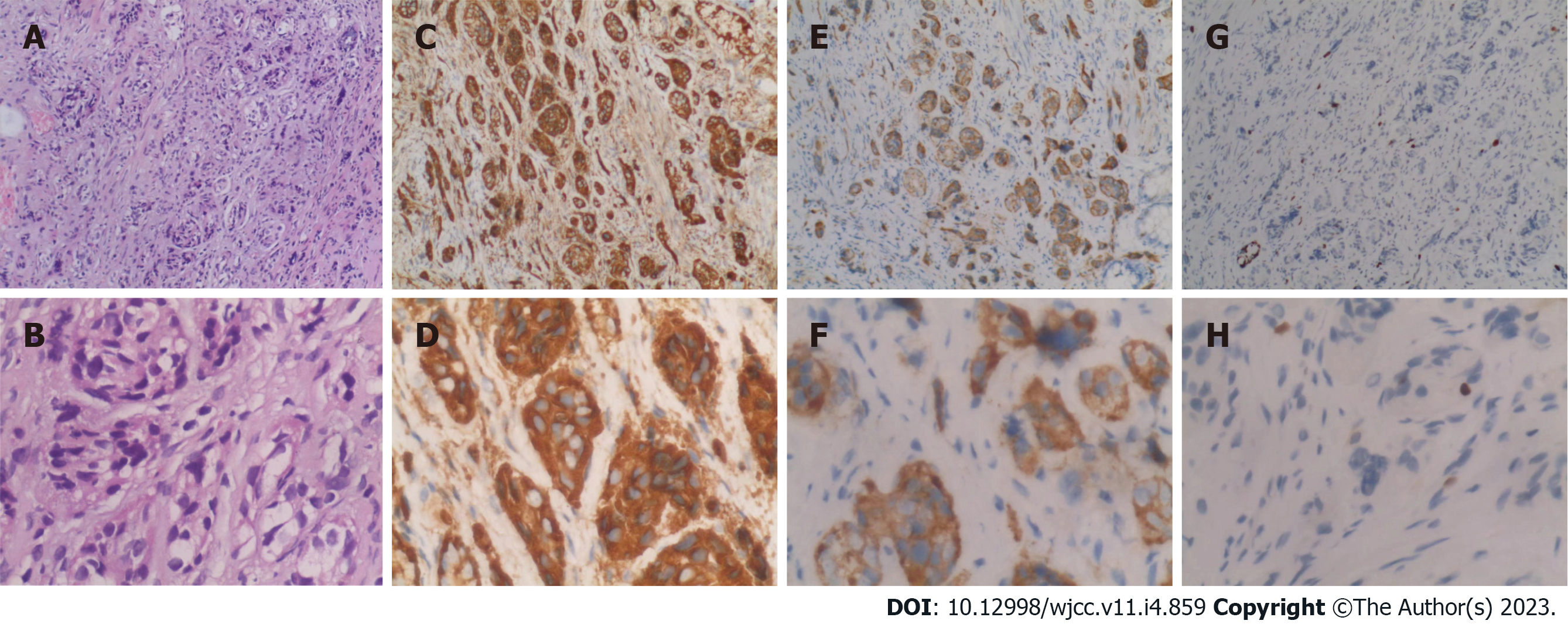
Figure 2 Pathological smears of tumor tissue after various immunohistochemical staining.
A-H: HE (A, × 100; B, × 400); CgA (C, × 100; D, × 400); Syn (E, × 100; F, × 400); and ki67 (G, × 100; H, × 400).
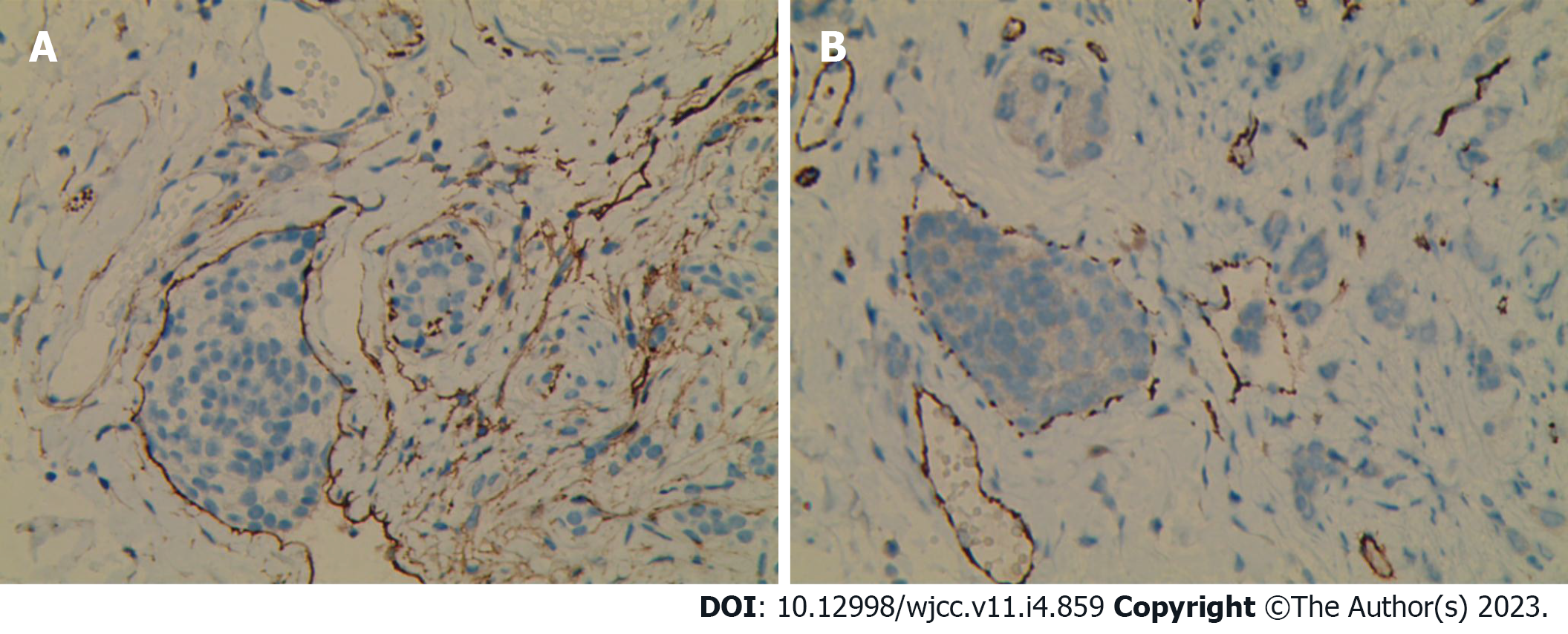
Figure 3 The tumor was found to have lymphatic invasion after staining with CD31 (A) and D2-40 (B).
A and B: × 200.
- Citation: Ran JX, Xu LB, Chen WW, Yang HY, Weng Y, Peng YM. Is lymphatic invasion of microrectal neuroendocrine tumors an incidental event?: A case report. World J Clin Cases 2023; 11(4): 859-865
- URL: https://www.wjgnet.com/2307-8960/full/v11/i4/859.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i4.859