Copyright
©The Author(s) 2023.
World J Clin Cases. Jan 26, 2023; 11(3): 576-597
Published online Jan 26, 2023. doi: 10.12998/wjcc.v11.i3.576
Published online Jan 26, 2023. doi: 10.12998/wjcc.v11.i3.576
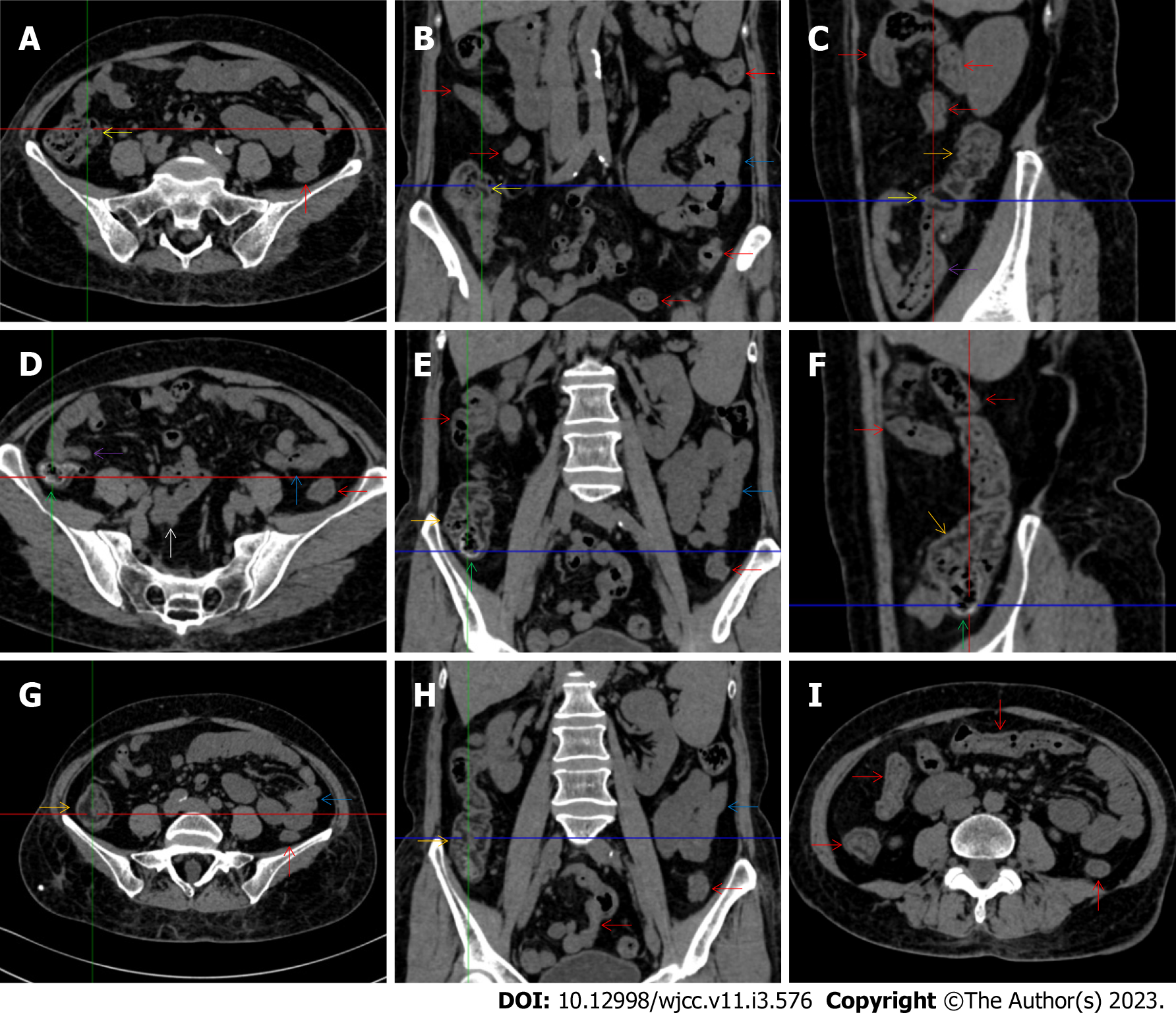
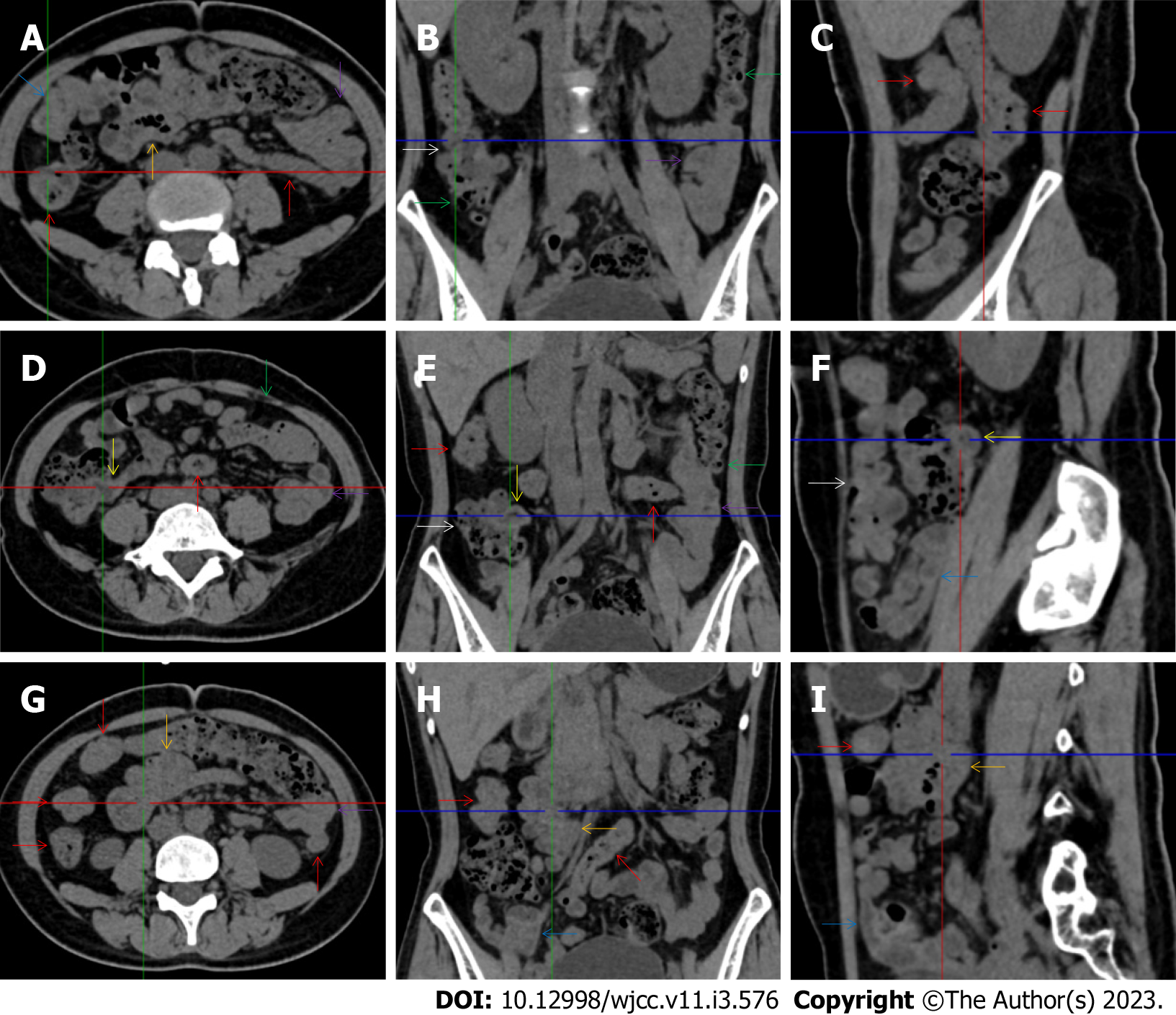
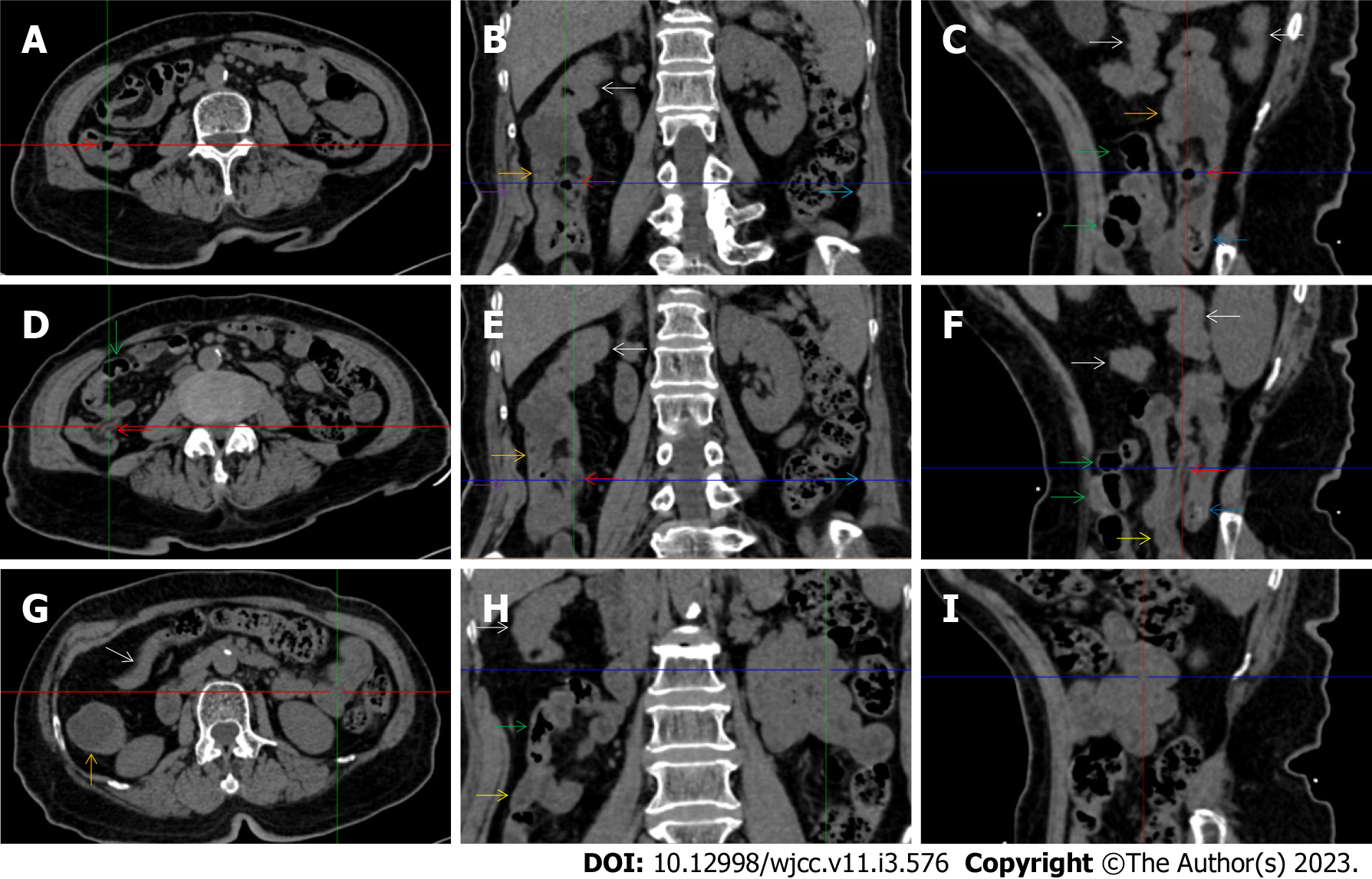
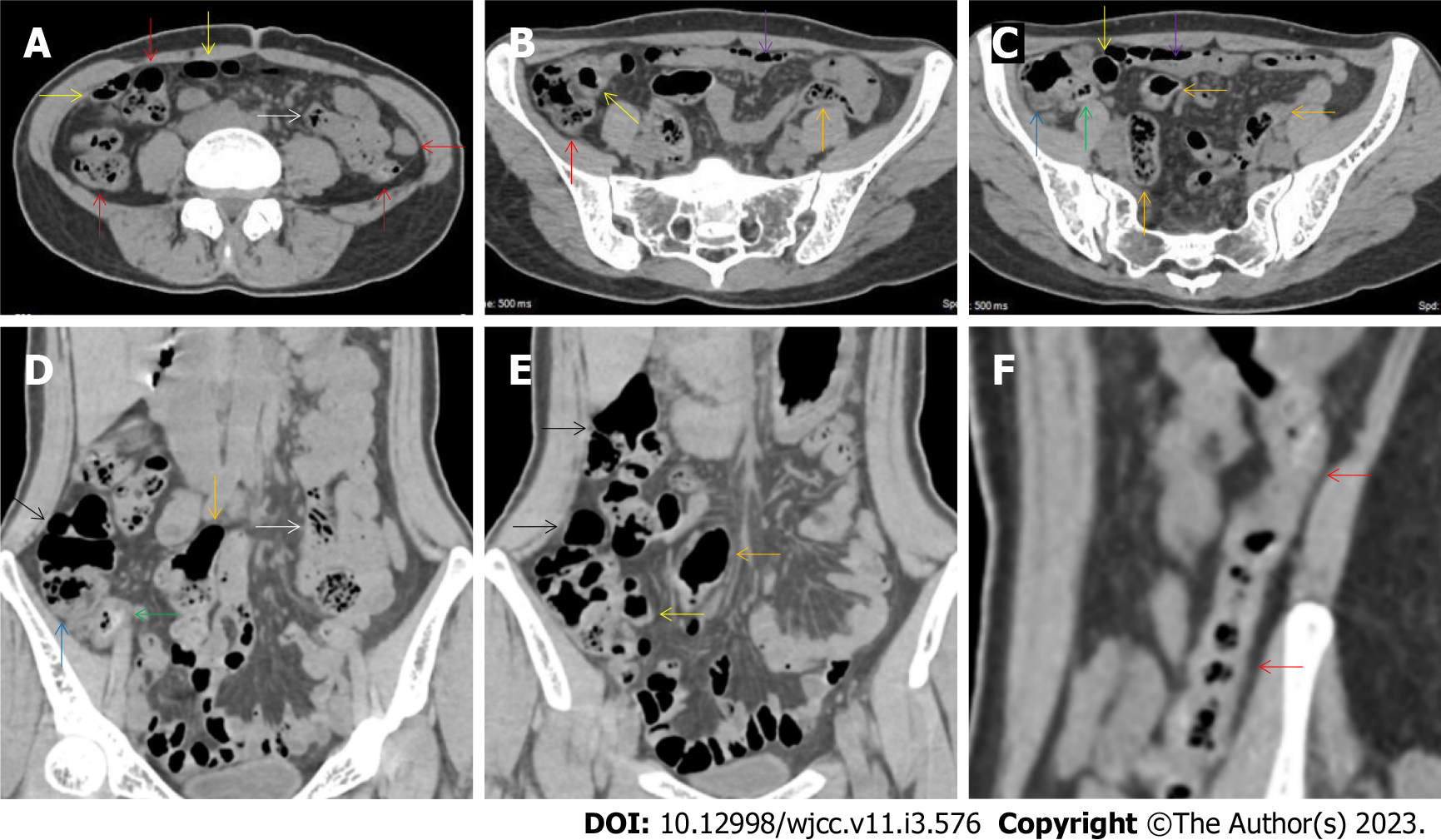
Figure 1 Characteristic images of case 4.
A-C: Characteristic images of the ileocecal region. The ileocecal valve (yellow arrows), the proximal ascending colon (orange arrows) and the terminal ileum (purple arrows) were significantly thickened and stratified by submucosal fat deposition, forming the so-called “fat holo sign”. From the distal ascending colon to the sigmoid colon (red arrows), the wall was thickened and stratified with “water holo sign”. The small intestine was heterogeneous in bowel wall texture, and gas-filled in some segments and liquid-filled in other segments, and a segment of adhesive bowel loop was found in the middle jejunum (blue arrows); D-F: Characteristic images of the asending colon. The irregular contour and the fibrotic thickening of the mucosal folds made the colonic configuration rugged. The mucosa of the cecum and the appendiceal root was fibrously thickened (green arrows), and the appendix was gas-filled. Thickened omentum surrounded the ileocecal region and the ascending colon. A segment of adhesive bowel loop was found in the proximal ileum (a white arrow). The mucosa of the proximal ileum in the adhered bowel loop was fibrotically thickened, with mesenteric fat deposition and adjacent peritoneal thickening forming the so-called “abdominal cocoon”; G and H: Typical fat holo sign in the ascending colon. The “fat holo sign” was more typical in the middle ascending colon; I: Thickened and stratified larger intestine. From the distal ascending colon to the sigmoid colon (red arrows), the wall was thickened and stratified by edematous submucosal tissues, forming the so-called “water holo sign”. In some segments, the colon was emptied. Paracolonic fat stranding was present from the cecum to the sigmoid colon. The disproportionately less severe paracolonic fat stranding suggested that the edematous colon most likely occurred during an acute episode.
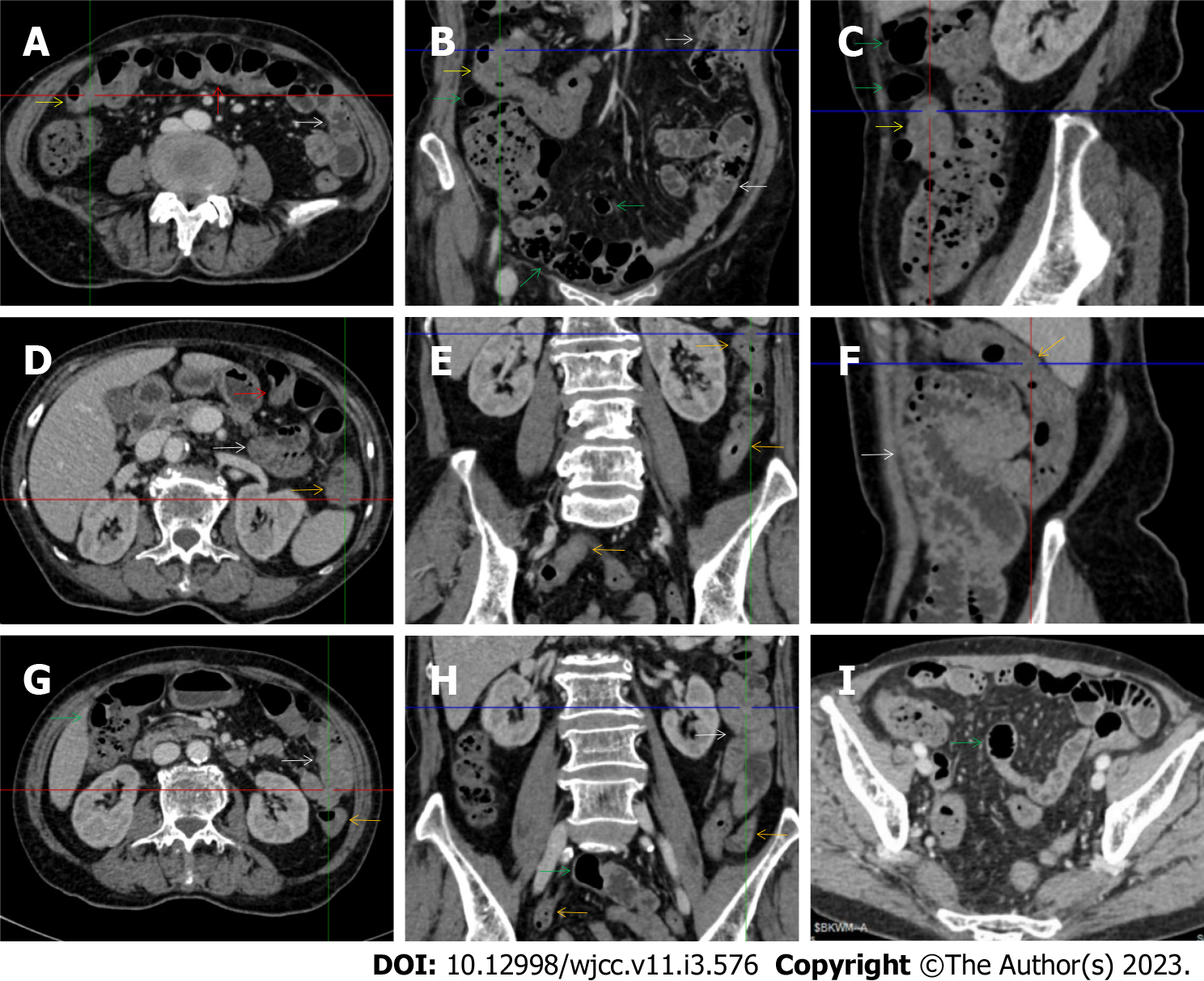
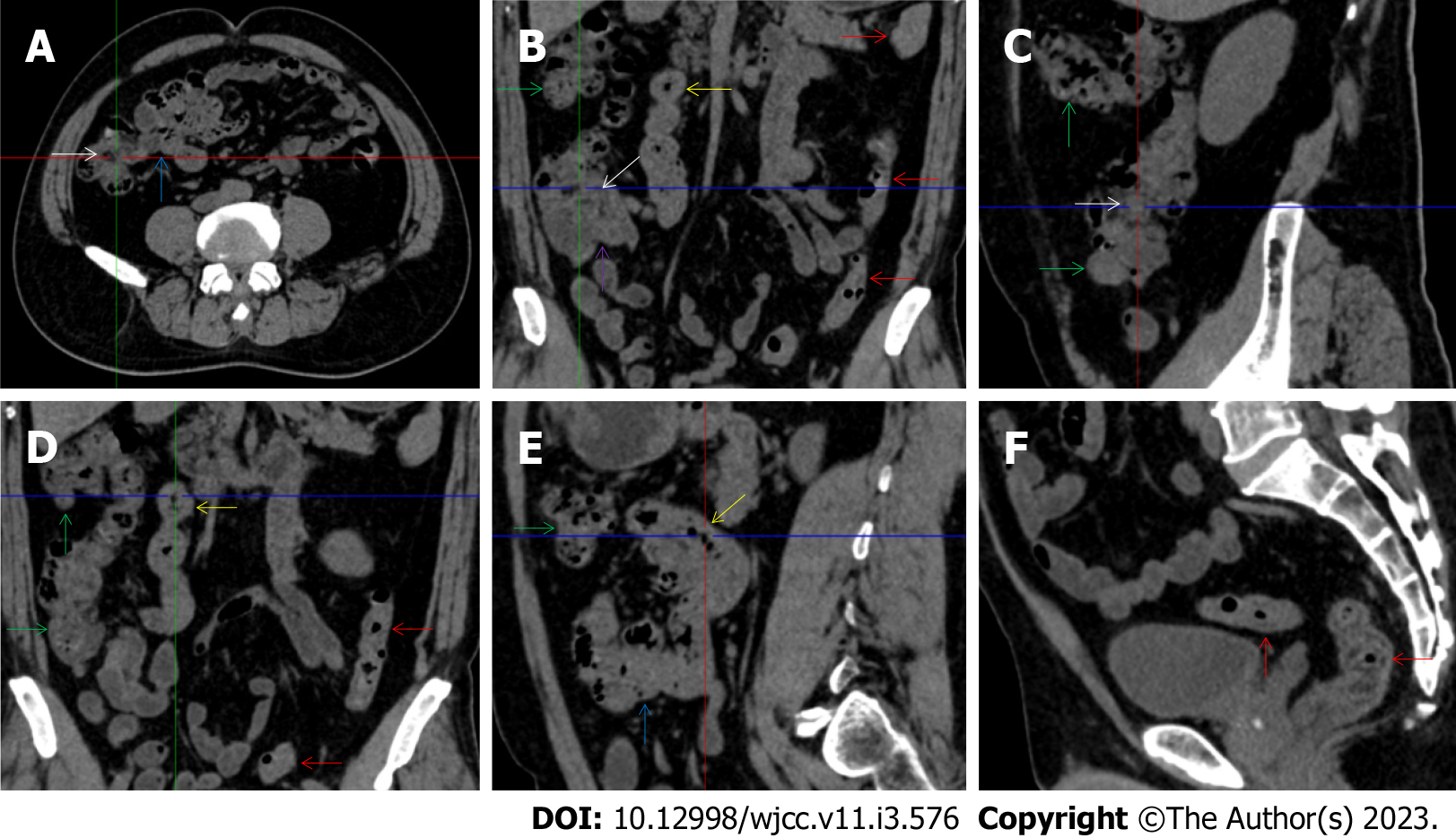
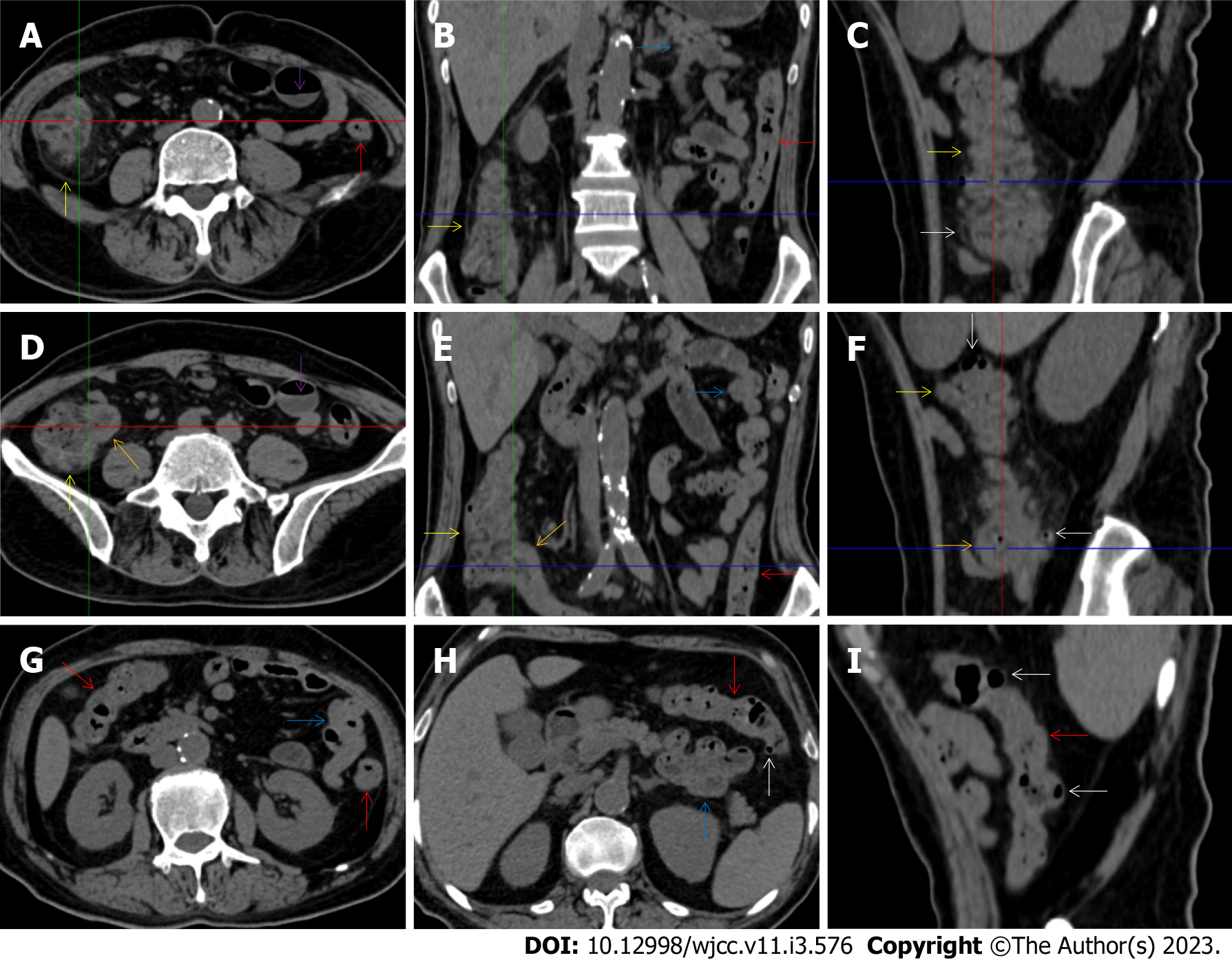
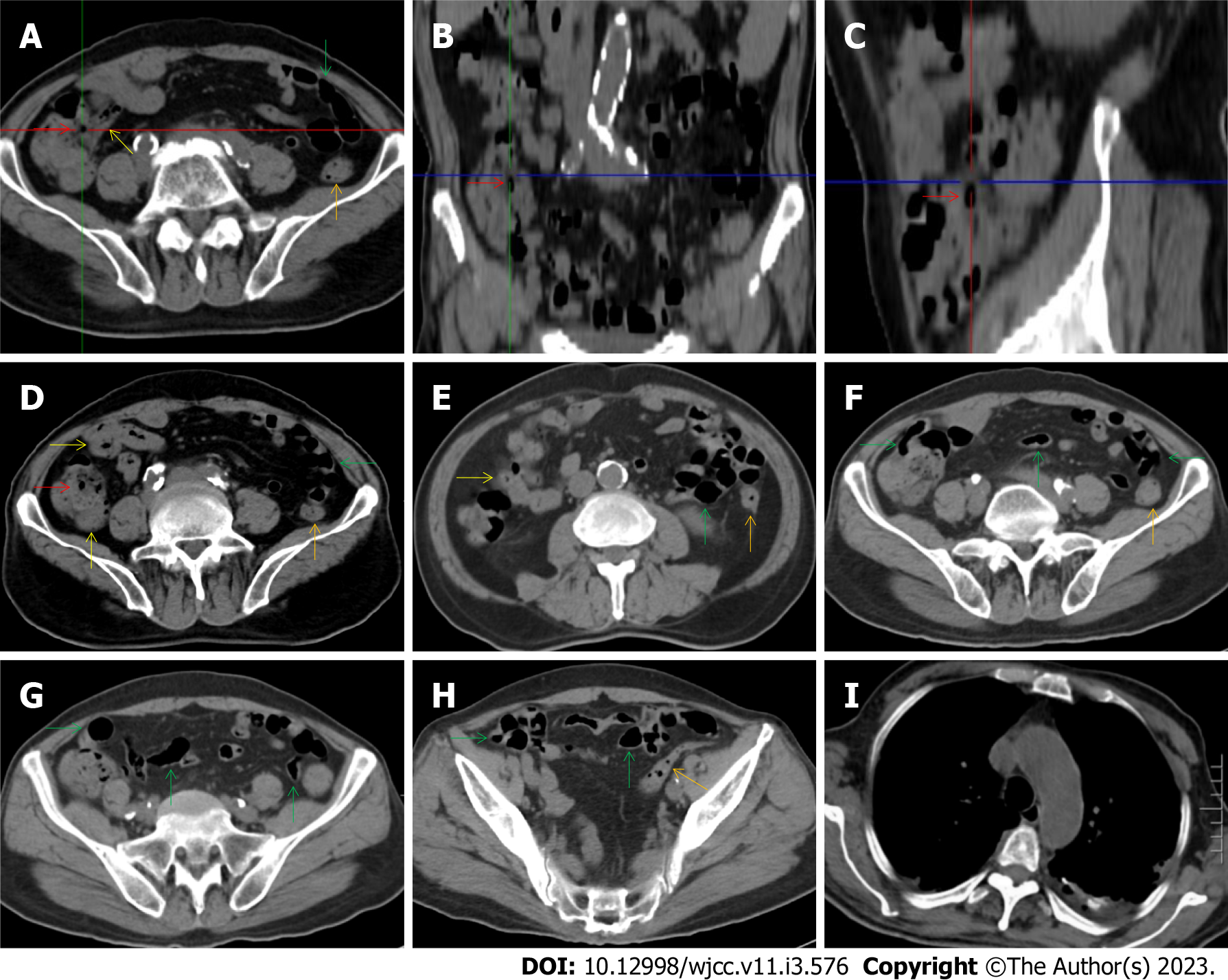
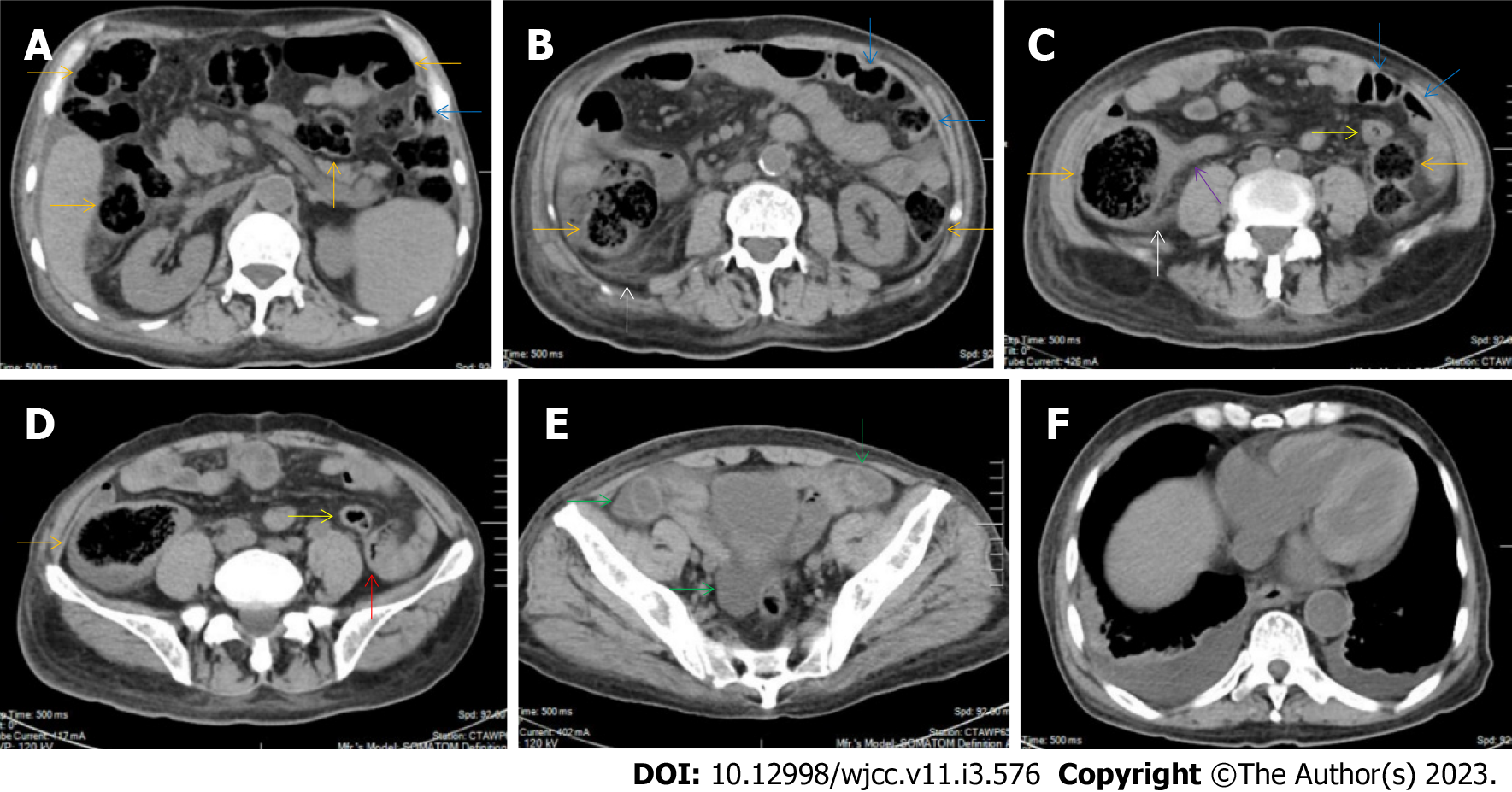
Figure 2 Characteristic images of case 3.
A-C: Characteristic images of the thickened transverse colon. The segmentally thickened, stratified (water holo sign) and emptied colon with paracolonic fat stranding was present in the hepatic flexure (yellow arrows) in which an inflamed polypoid lesion was found on endoscopic examination, followed by the asymmetrically thickened wall and gas-filled lumen of the transverse colon (red arrows) in which the colonic villi were absent; D-F: Characteristic images of the thickened descending colon. The wall of the descending and sigmoid colon was thickened and stratified with mesenteric fat stranding (orange arrows), with the most striking segment being in the splenic flexure; G and H: Characteristic images of an adhesive bowel loop. While the ileum was gas-filled and distended (green arrows), the adhesive jejunal loop (white arrows) was heterogeneous in bowel wall texture and liquid-filled with multiple gas-liquid levels and accrescent plica. Increased mesenteric fat and vasculature were adjacent to the adhered jejunal loop; I: Characteristic image of a balloon sign. Clustering and hypervascular mesenteric fat proliferation wrapped a segment of paper-thin ileum, forming the so-called “balloon sign”. Balloon sign was also present in the hepatic flexure.
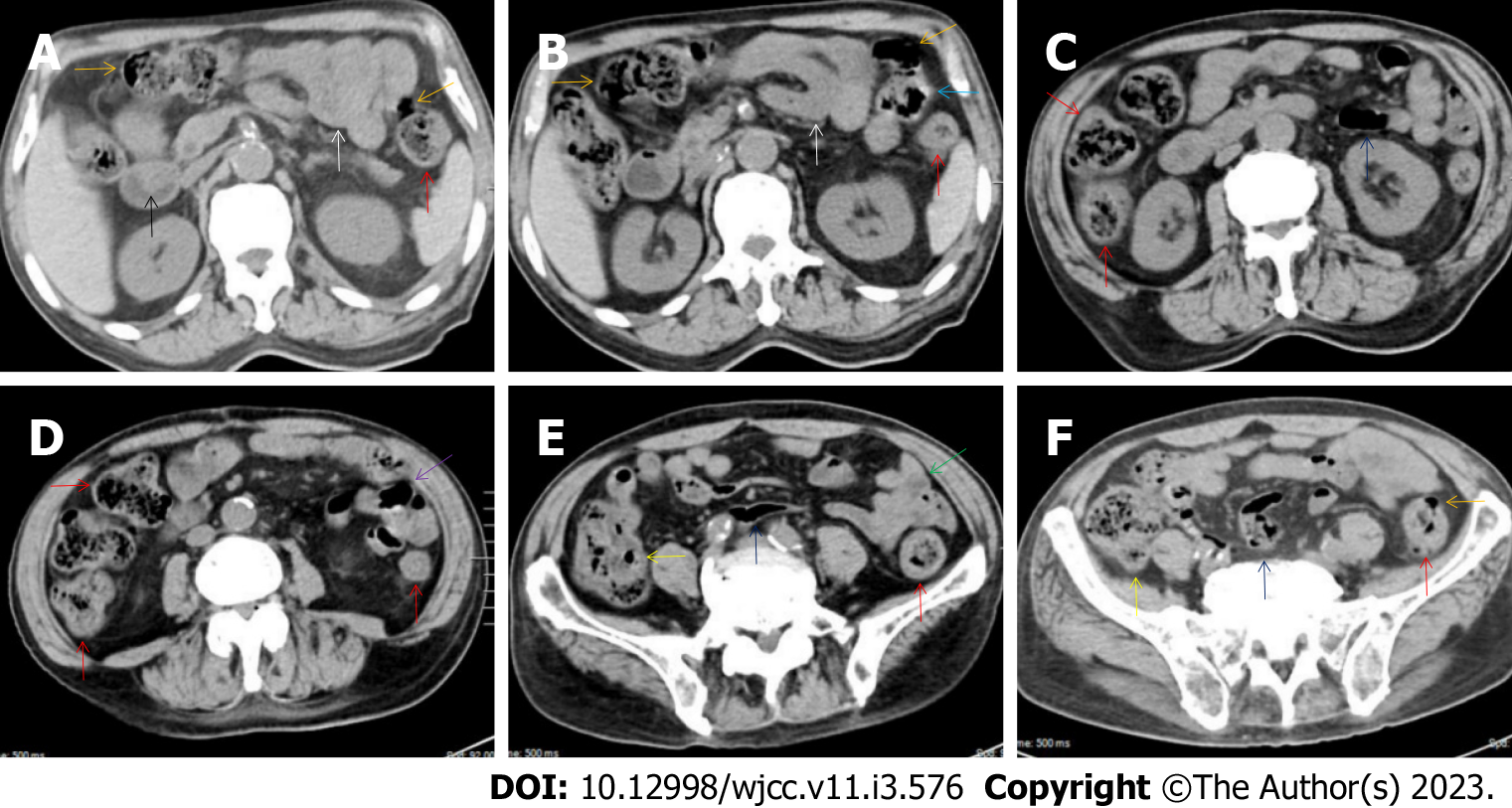
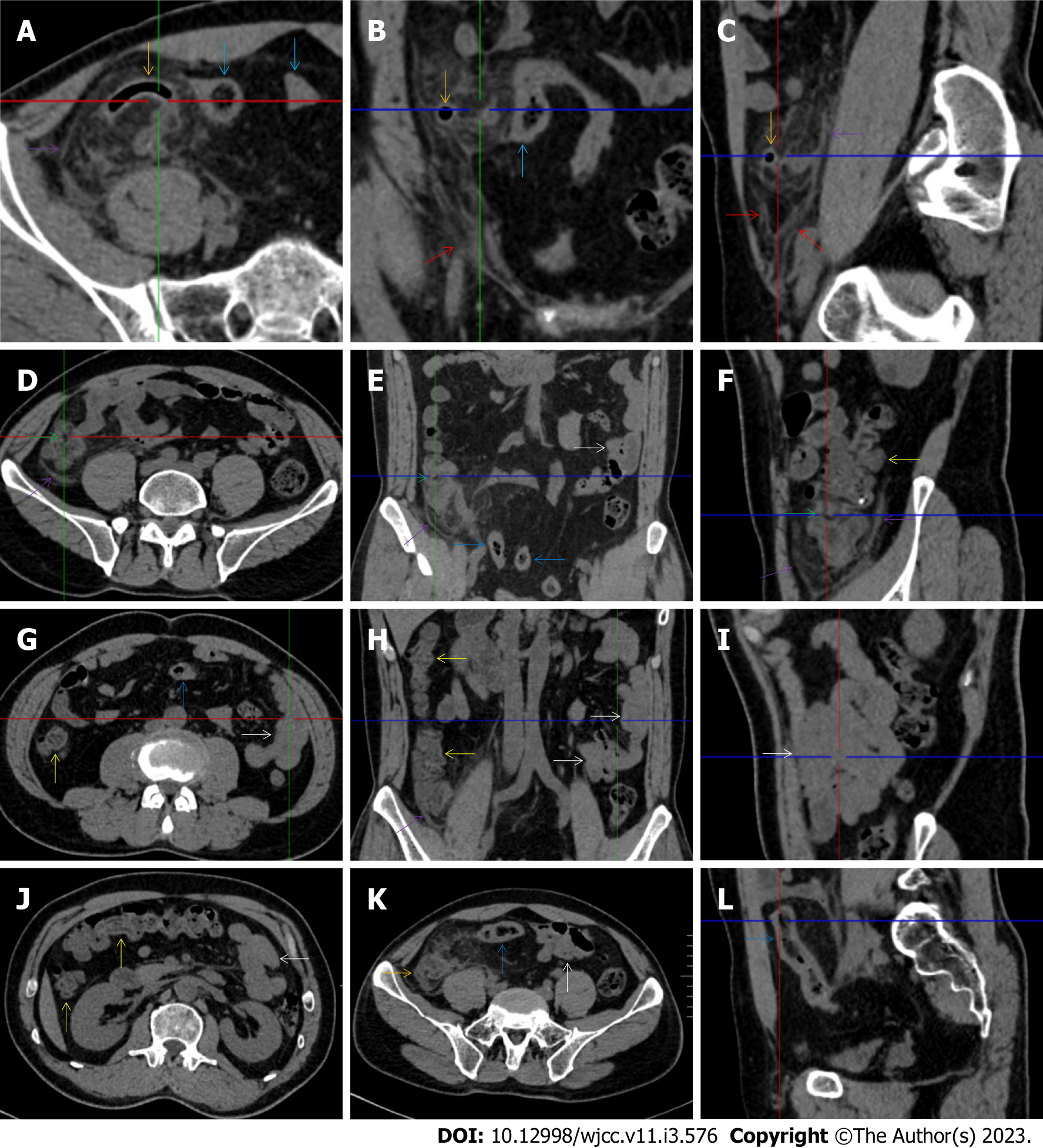
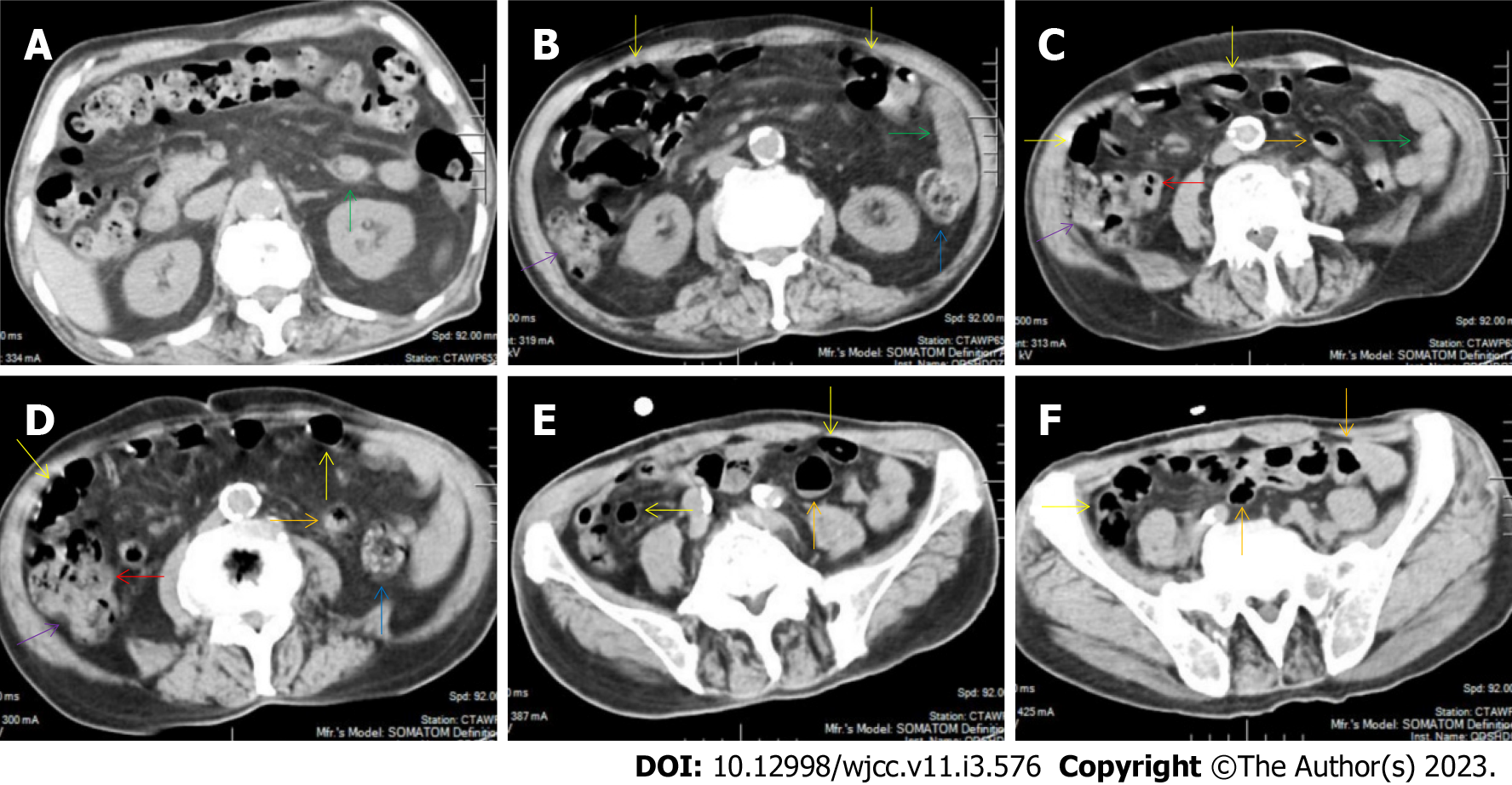
Figure 3 Characteristic images of case 6.
A and B: Characteristic images of the upper abdomen. Several inflamed diverticula (orange arrows) were present in the colonic segments. In the duodenum-jejunum junction (a blue arrow), the bowel wall was fibrotically thickened and the lumen was gas-filled. In the bulb part of the duodenum, a polypoid mass (a black arrow) protruded into the lumen. A segment of adhesive jejunal loop was present in the proximal jejunum (white arrows); C and D: Characteristic images of the thickened colon. The wall from the cecum to the descending colon was significantly thickened with mural stratification, intramural gas and pericolonic fat stranding. A segment of adhesive bowel loop was present in the middle jejunum (a purple arrow) in which the bowel wall was asymmetrically thickened and the lumen was gas-filled with particularly prominent mesenteric fat stranding; E: Characteristic images of the ileocecal region. Stratified thickening of the ileocecal valve and the terminal ileum was gas-filled (yellow arrows). The third segments of adhesive bowel loop were present in the distal jejunum (a green arrow); F: Characteristic image of a balloon sign. The sigmoid colon was dilated and the wall was paper-thin (navy blue arrows), with clustering pericolonic fat stranding forming the so-called “balloon sign”.
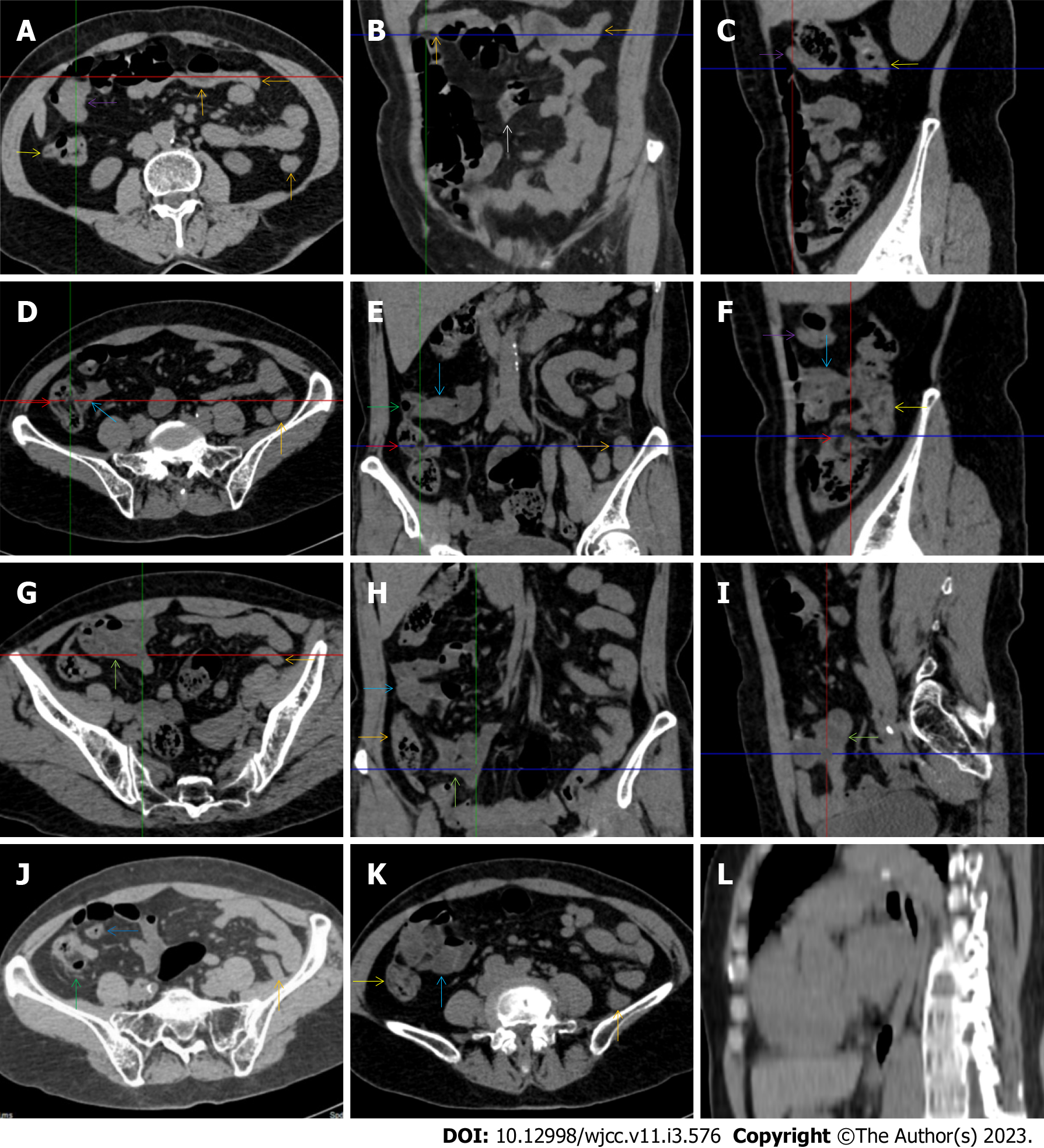
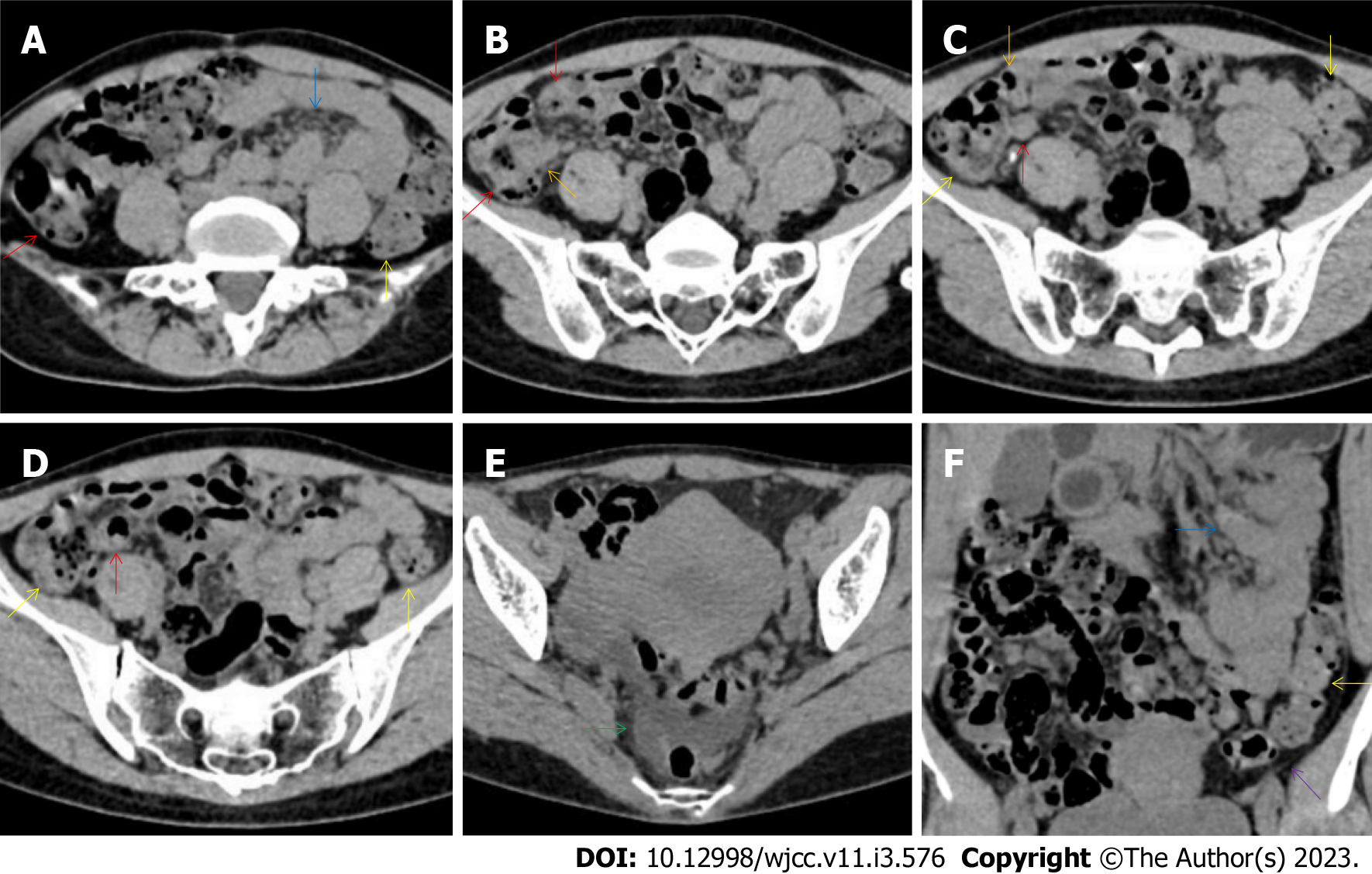
Figure 4 Characteristic images of case 9.
A-C: Characteristic images of an empty colon sign. The segmentally wall-thickened, stratified and emptied colon in the hepatic flexure (purple arrows) followed by the collapsed transverse (adjacent to the dilated ileum in which gas-liquid levels could be recognized) and descending colon (orange arrows), forming the so-called “empty colon sign”. A short segment of asymmetrically thickened wall was present in the proximal ileum (a white arrow), around which the hypervascular fat stranding was especially prominent, distal to which the ileal lumen was gas-filled, and proximal to which the ileal lumen was liquid-filled; D-F: Characteristic images of the ileocecal region. The ileocecal valve and the terminal ileum were thickened and stratified by submucosal fat deposition (red arrows). Omental thickening was especially prominent in the ileocecal region. The wall of the ascending colon was thickened and, in some segments, stratified with submucosal fat deposition, and in other segments, stratified with submucosal edematous tissue (yellow arrows). Several inflamed diverticula (green arrows) were present in the cecum and ascending colon. The distal ileum was strictured (blue arrows), proximal to which the ileal lumen was liquid-filled; G-I: Characteristic images of adhesive bowel loops. The fibrotic mucosa and liquid-filled lumen of the adhesive bowel loops were present in the proximal ileum (powder blue arrows) and distal ileum (jade-green arrows); J: Characteristic image of a balloon sign. A large cluster of circumferentially distributed hypervascular fat stranding wrapped a segment of the dilated lumen and paper-thin bowel wall of the sigmoid colon, forming the so-called “balloon sign”. An inflamed diverticula was present in the cecum, with strikingly thickened omentim (a green arrow); K: Characteristic image of an adhesive bowel loop in the proximal ileum. A segment of adhesive bowel loop in the proximal ileum, together with the fibrotically thickened peritoneum, formed the so-called “abdominal cocoon”; L: Characteristic image of esophagus. Hypertrophic lesions presented in two segments of the esophagus, together with the inflammatory lesions in the jejunum suggesting that the initiating factor in the upper gastrointestinal tract affected the functions of the downstream intestinal segments.
Figure 5 Characteristic images of case 15.
A-C: Characteristic images of the ascending colon. The ascending colon was rugged with omental thickening and paracolonic fat stranding, and the colonic wall was thickened with mural stratification and intramural gas (white arrows). From the hepatic flexure to the sigmoid colon (red arrows), the bowel wall was thickened and stratified with several inflamed diverticula (green arrows) in these colonic segments. Three segments of adhesive bowel loops were visualized: one in the distal ileum (blue arrows), the other two in the middle ileum (orange arrows) and the jejunum (purple arrows); D-F: Characteristic images of the ileocecal region. The ileocecal valve and the terminal ileal wall were fibrotically thickened (yellow arrows), proximal to which the ileal lumen was liquid-filled; G-I: Characteristic images of the adhesive bowel loops in the middle and distal ileum. The bowel loop in the middle ileum was adhered and clustered (orange arrows), with the bowel wall being highly heterogeneous in texture and the mucosa being hyperdense. The bowel loop in the distal ileum was adhered, the lumen was liquid-filled, and the bowel wall was fibrotically thickened, together with the fibrotically thickened peritoneum forming the so-called “abdominal cocoon” (blue arrows).
Figure 6 Characteristic images of case 2.
A-C: Characteristic images of the ileocecal region. The ileocecal valve and the terminal ileal wall were thickened and stratified (white arrows), the ileal mucosa was hyperdense and the ileal lumen was liquid-filled. The adhered and clustered distal ileum and cecum with the fibrotically thickened peritoneum (a purple arrow) formed the so-called “abdominal cocoon”; D and E: Characteristic images of the ascending colon and the adhesive bowel loops. In the ascending colon (green arrows), the wall was thickened and stratified with “water holo sign”, the mucosa was hyperdense and the configuration was rugged, with paracolonic fat stranding, omental thickening and subserosal pneumatoses. The wall of the descending and sigmoid colon (red arrows) was also thickened and stratified. In two segments of the adhesive bowel loop (blue arrows and yellow arrows), the bowel wall was heterogeneously thickened and the lumen was gas-filled, suggesting the presence of heterogeneity in small bowel wall texture; F: A particularly striking edematous segment was present in the rectum.
Figure 7 Characteristic images of case 1.
A-C: Characteristic images of the ileocecal region. A massive cluster of fat stranding that was wrapped by the strikingly thickened omentum (purple arrows) was centered on the homogeneously wall-thickened and gas-filled appendix (orange arrows), leading to the diagnosis of a chronic periappendiceal abscess. The periappendiceal inflammatory changes extended to the scrotum along the inguinal canal (red arrows). In the adjacent sigmoid colon, the wall was thickened and stratified with the water holo sign, and the lumen was gas-filled (blue arrows); D-F: Characteristic images of the ascending colon. The ileocecal valve was thickened and strictured (green arrows), proximal to which the ileal lumen was liquid-filled. Bowel wall thickening with irregular mucosal folds, emptied lumen, mural stratification (fat holo sign) and paracolonic fat stranding that was disproportionately less severe than the severity of the colonic wall thickening was present in the ascending colon (yellow arrows). In the descending colon, the wall was also fibrotically thickened; G-I: Characteristic images of an adhesive bowel segment. A segment of adhesive bowel loop with fibrotic bowel wall thickening, peritoneal thickening and hypervascular mesenteric fat stranding was present in the jejunum (white arrows), together with the segmentally gas-filled, segmentally liquid-filled jejunal lumen, suggesting the inflammatory involvement of the upper gastrointestinal tract; J: Characteristic image of the thickened transverse colon. Bowel wall thickening with emptied lumen, mural stratification (water holo sign) and paracolonic fat stranding that was disproportionately less severe than the severity of the colonic wall thickening was present in the transverse colon, suggesting the involvement of a transmural inflammatory condition; K and L: The thickened and stratified sigmoid colon. Of the sigmoid colon adjacent to the massive inflammatory lesion, the wall was thickened and stratified with the water holo sign, and the lumen was gas-filled.
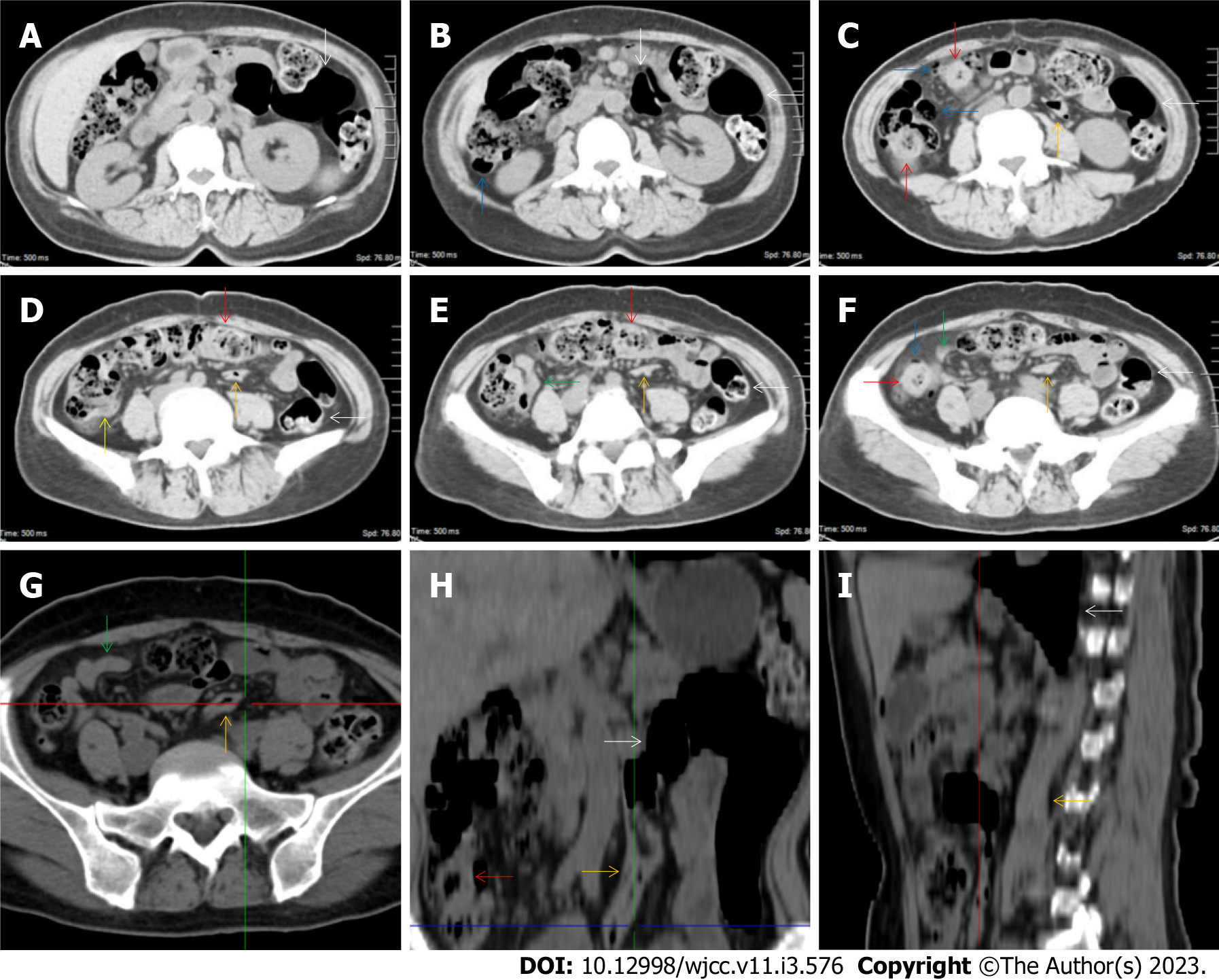
Figure 8 Characteristic images of case 7.
A-F: Characteristic images of the ileocecal region and the large colon. The ileocecal valve was thickened and stratified (yellow arrow). The distal ileum was thickened and strictured (green arrows) with a large cluster of misty exudative lesions surrounding the cecum and distal ileum, and the proximal small intestine was liquid-filled with multiple gas-liquid levels. From the cecum to the distal descending colon, the mucosa and the villi were hyperdense, with several focally wall-thickened and stratified colonic segments (red arrows) and several inflamed diverticula (blue arrows). An obstructively thickened segment of the sigmoid colon (orange arrows) with prominent paracolonic hypervascular fat stranding was distal to the remarkably distended lumen and paper-thin bowel wall of the sigmoid colon (white arrows); G-I: Reconstructed images of the obstructively thickened sigmoid colon. From the reconstructed images, the obstructively thickened segment of the sigmoid colon (orange arrows) and the proximal distended sigmoid colon (white arrows) were better visualized. The misty exudative lesions and the surrounded cecum and distal ileum were also better visualized (green arrows).
Figure 9 Characteristic images of case 13.
A-C: Characteristic images of the ileocecal valve and ascending colon. There was edematous fat deposition around the ileocecal valve and the terminal ileum, forming the so-called “fat holo sign”. A massive necrotic lesion in the colonic wall was adjacent to the edematous fat deposition, and the serosal colonic wall was hypertrophically thickened (orange arrows). The adjacent parietal peritoneum (purple arrows) and the left parietal peritoneum (navy blue arrows) were also hypertrophically thickened. The mucosa of the cecum was fibrotically thickened (blue arrow); D-F: Characteristic images of the distal ileum. Strictured thickening of the ileocecal valve and terminal ileum (red arrows) led to the distal ileum being liquid-filled. Proximal to the liquid-filled distal ileum (yellow arrows) was the asymmetrically wall-thickened and gas-filled ileum (green arrows). Heterogeneity of the small bowel wall was observed; G-I: Characteristic images of an “abdominal cocoon”. A segment of adhesive bowel loop was present in the middle jejunum, together with the fibrotically thickened bowel and peritoneal involvement forming the so-called “cauliflower sign”. Edematously thickened colonic wall and emptied colonic lumen were present from the proximal ascending colon to the hepatic flexure, followed by a segment of the collapsed transverse colon (white arrows), forming the so-called “empty colon sign”.
Figure 10 Characteristic images in case 11.
A-C: Characteristic images of the ascending colon. The ascending colon was rugged with fibrotically and irregularly thickened colonic mucosa, circumferentially distributed omental thickening and paracolonic fat stranding (yellow arrows), and other colonic segments were thickened and stratified with water holo sign (red arrows); D-F: Characteristic images of the ileocecal region. The ileocecal valve and the terminal ileal wall were strikingly thickened and stratified (orange arrows). Bowel wall thickening, mural stratification, heterogeneity in bowel wall texture and gas-liquid levels (purple arrows) were found in the small intestine; G-I: Stratified thickening of the large intestine. From the hepatic flexure to the sigmoid colon, the colonic wall was thickened and stratified with water holo sign (red arrows). Several inflamed diverticula was present in the colonic segments (white arrows). A segment of adhesive bowel loop was present in the middle jejunum (blue arrows), together with the peritoneal involvement forming the so-called “cauliflower sign”.
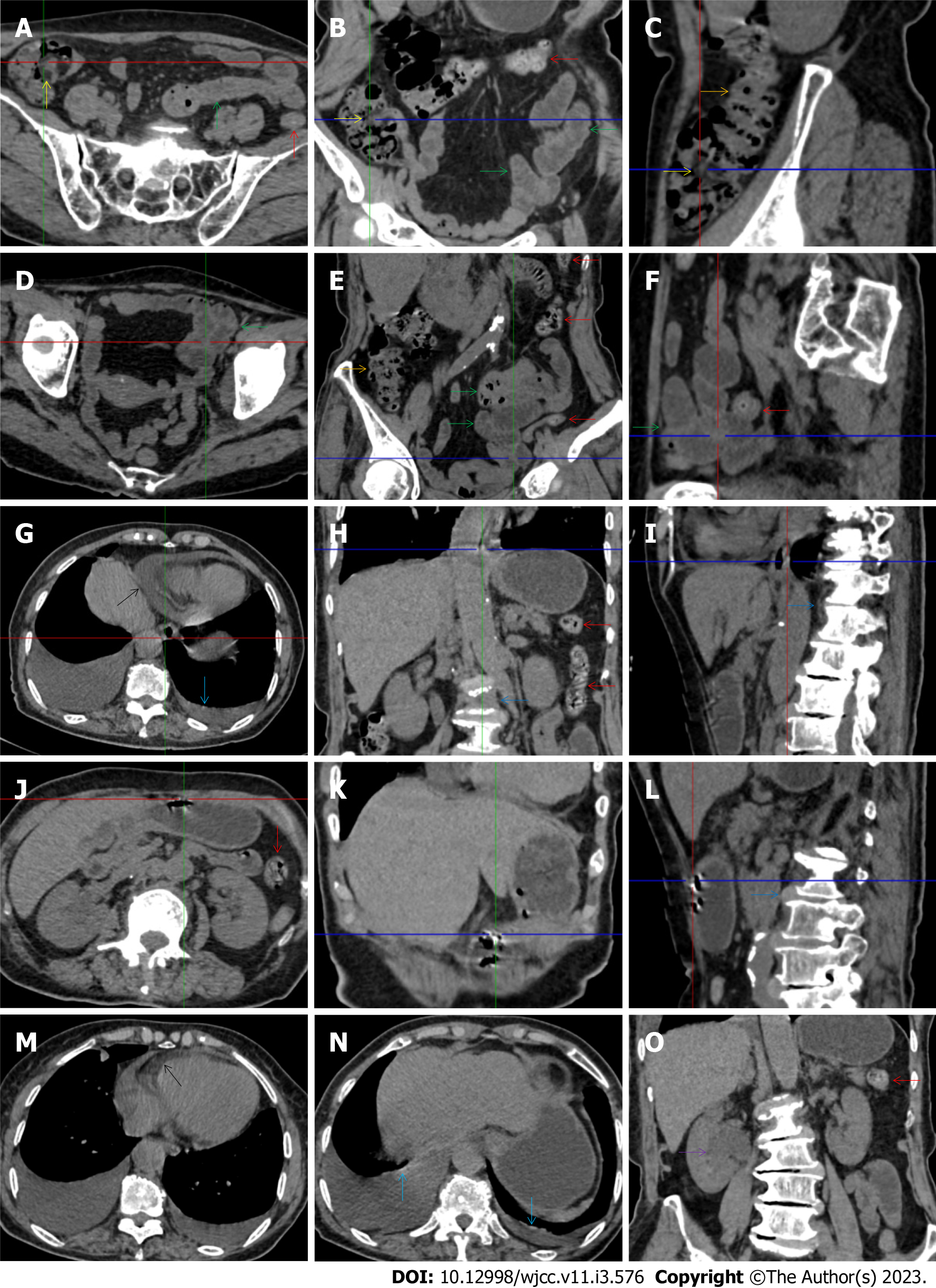
Figure 11 Characteristic images in case 17.
A-C: Characteristic images of the ileocecal region and the ascending colon. Circumferentially distributed fat deposition wrapped the ileocecal valve (yellow arrows), forming the so-called “fat holo sign”. The terminal ileum was thickened, and the strictured ileocecal valve and terminal ileum led to the small intestines being liquid-filled. Heterogeneity and hypertrophic lesions of the small intestines were easily recognized. The ascending colon was rugged with paracolonic fat stranding and peritoneal thickening, and the colonic wall was thickened and stratified with edematous submucosal tissue and intramural gas (orange arrows). From the transverse to the sigmoid colon (red arrows), the colonic wall was fibrotically thickened, with multiple inflamed diverticula in this colonic segment; D-F: Characteristic images of an adhered jejunal segment. A long segment of the adhered jejunal loop was present in the left iliac fossa and pelvic cavity (green arrows). In the adhesive jejunal loop, the lumen was gas-filled in the proximal segment and liquid-filled in the distal segment. Hypervascular mesenteric fat stranding and fibrotic peritoneal thickening were present in this bowel segment, forming the so-called “abdominal cocoon”. Fibrotic wall thickening was present in the entire jejunal segment and accrescent pili were visualized in the adhesive jejunal loop and the proximal jejunum; G-I: Erosive lesions in extraintestinal organs. Erosive lesions on the background of the calcified lesions were found in the esophagus. Hypertrophic lesions and seromembranous effusion were visualized in the pericardium (black arrows) and the pleura (light blue arrows). Exudative lesions were also present in the vertebral column (blue arrows); J-L: Erosive lesions in the stomach. Erosive lesions on the background of the calcified lesions were also found in the stomach; M-O: Exudative lesions in extraintestinal organ. Hypertrophic lesions and seromembranous effusion were visualized in the pericardium (black arrows) and the pleura (light blue arrows). Exudative lesions were also present in the renal pelvis and urinary tract (a purple arrow). These radiological features led to the diagnosis of reactive tuberculosis infections in the gastrointestinal tract, urinary tract, peritoneum, vertebral column, pleura and pericardium.
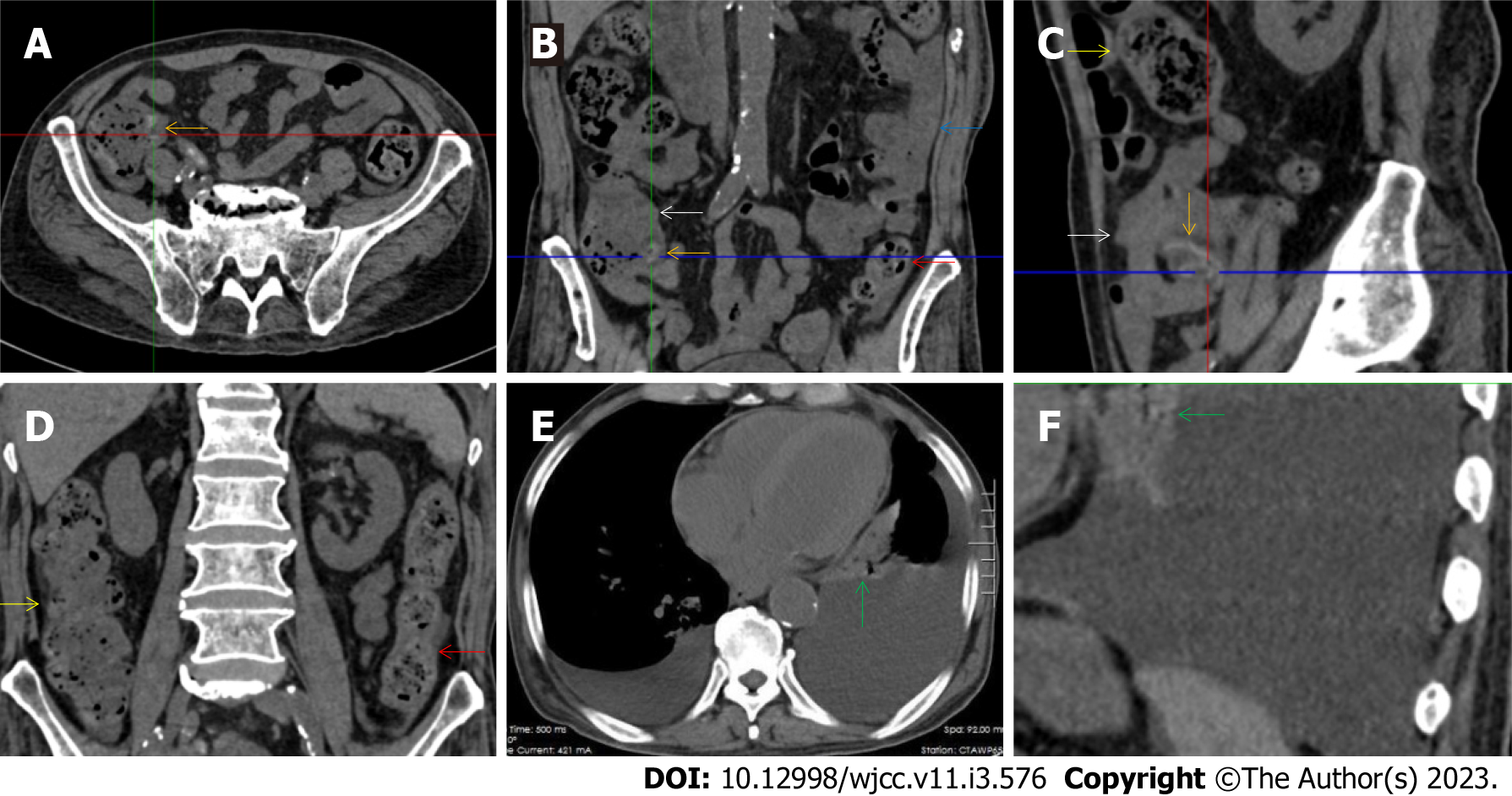
Figure 12 Characteristic images in case 16.
A-C: Characteristic images of the ileocecal region and the small intestine. The ileocecal valve was fibrotic and thickened with edematous fat deposition, forming the so-called “fat holo sign” (orange arrows), and the distal ileum was adhesive with mesenteric fat stranding and peritoneal thickening (white arrow), forming the so-called “abdominal cocoon”. Intestinal adhesion with bowel wall thickening, peritoneal involvement and mesenteric fat stranding was also found in the jejunum (blue arrow). Heterogeneity in the bowel wall texture was particularly prominent in the adhesive bowel segments; D: Characteristic image of the large intestine. The ascending colon was rugged and the colonic wall was thickened and stratified, with adjacent omental thickening (yellow arrows). The descending colonic wall were significantly thickened and stratified with mucosal hyperdensity and paracolonic fat stranding (red arrows); E and F: Characteristic images of the chest computed tomography (CT) scan. Chest CT revealed that the pleural effusion was predominantly in the left cavity and hypertrophic lesions involved both the left pleura and the pericardium (green arrows).
Figure 13 Characteristic images of case 14.
A-C: Characteristic images of the bowel inflammatory lesions. The ileocecal valve and the ileal wall were fibrotically thickened and the ileal lumen was gas-filled (yellow arrows), with a large cluster of hypervascular perienteric fat proliferation wrapping the wall-thickened and lumen-dilated ileum. The cecum (blue arrows) and appendix (green arrows) were also fibrotically thickened and stratified, with peripheral fat stranding. Gas-liquid levels were present in the lumen of the proximal ileum and distal jejunum (purple arrows). However, the adhesive jejunal loop was liquid-filled with prominent hypervascular mesenteric fat proliferation. In a segment of the jejunum (white arrows), the bowel wall was thickened, the lumen was gas-filled and the mesenteric fat stranding was especially prominent. Thickened peritoneum was adjacent to the adhesive jejunal loop, forming the so-call “abdominal cocoon” and the enlarged mesenteric vascularity formed the so-called “comb sign”. The ascending colon was dilated with a paper-thin bowel wall (black arrows), forming the so-called “balloon sign”. From the hepatic flexure to the distal descending colon (red arrows), the bowel was thickened and stratified (water holo sign), with paracolonic fat stranding and peritoneal thickening being particular prominent in the hepatic flexure. The sigmoid colon was fibrotically thickened and dilated (orange arrows); D and E: Characteristic images in coronally reconstructed images. The coronally reconstructed images better outlined the above-mentioned imaging features; F: Characteristic image of the descending colon in coronally reconstructed section. A coronally reconstructed image better outlined the thickened and stratified descending colon.
Figure 14 Characteristic images in case 8.
A-C: Characteristic images of the ileocecal region and the small intestine. The ileocecal valve (red arrows) was thickened, strictured and stratified. The distal ileum (yellow arrows) were significantly thickened with intramural gas and wrapped by prominent mesenteric fat stranding, which suggested the presence of aggravated inflammatory damage in the distal ileum and ileocecal region; D-H: Characteristic images of the small intestine. In the ileocecal region, the ileum adhered to the cecum, and the cecum was thickened and stratified. In other colonic segments (orange arrows), the bowel wall was also thickened and stratified, and the lumen was dilated in some segments and collapsed in other segments. From the jejunum to the proximal ileum (green arrows), the wall was fibrotic and thickened and the lumen was gas-filled. Several segments of adhesive bowel loop were present in the small bowel. Noticeably, panabdominal silt-like hypervascular fat deposition wrapped the adhesive and widened small bowel loop (creeping fat sign), which suggested the presence of chronic transmural inflammatory damage and a diagnosis of Crohn’s disease; I: Characteristic image of the chest computed tomography (CT) scan. Chest CT showed exudative lesions in the left pleura in the context of calcified lesions, indicating the reactivation of an old tuberculosis infection.
Figure 15 Characteristic images of case 10.
A and B: Characteristic images of the fat deposition. The most noticeable radiological finding was the panabdominal silt-like hypervascular fat deposition, leading to the widening of the bowel loop of the jejunum and the proximal ileum, forming the so-called “creeping fat sign”. The ileum was fibritically thickened and dilated, and the duodenum and the proximal jejunum were liquid-filled (green arrows); C and D: Characteristic images of the ileocecal region. The ileocecal valve and the terminal ileum were significantly thickened, stratified and strictured (red arrows), and proximal to the thickened terminal ileum, the ileal lumen was dilated and gas-filled and the mucosa was hyperdense (yellow arrows). The ascending colonic wall was also thickened (purple arrows). In a short segment of the descending colon (blue arrows), accrescent villi were especially prominent; E and F: Characteristic images of the small intestine. The proximal ileum and the distal jejunum (orange arrows) were thickened and gas-filled.
Figure 16 Characteristic images of case 12.
A-D: Characteristic images of the bowel inflammatory lesions. The ileocecal valve and the terminal ileal wall (red arrows) were thickened, stratified and strictured. Proximal to the strictured terminal ileum, the ileal lumen was dilated and gas-filled, and the mucosa was hyperdense. A large cluster of hypervasular mesenteric fat proliferation wrapped the dilated and gas-filled ileum. The jejunum was liquid-filled and the jejunual loop was adhesive. A cluster of hypervascular fat stranding wrapped a short segment of the jejunum (blue arrows), suggesting that the transmural inflammation was more serious in this jejunal segment. The colonic wall was also thickened and stratified, with intramural gas and subserosal pneumatosis (yellow arrows); E: Characteristic image of the pelvic liquid collection. Mild liquid collection was present in the pelvic cavity (a green arrow), together with the thickened peritoneum (a purple arrow) suggesting the presence of peritoneal involvement; F: Characteristic image in coronally reconstructed section. A coronally reconstructed image better outlined the above-mentioned imaging features.
Figure 17 Characteristic images of case 5.
A-D: Characteristic images of the bowel inflammatory lesions. From the cecum to the descending colon, the lumen was dilated, the mucosa was hyperdence and the wall was thickened and stratified in some segments (orange arrows), with striking mesenteric fat stranding. There was a hypertrophic lesion (a red arrow) in the terminal descending colon. The mucosa of the proximal sigmoid colon was hyperdense and the lumen was gas-filled (blue arrows), following which was a short segment of strictured sigmoid colon (yellow arrows). The ileocecal valve and the terminal ileum were thickened and strictured but without mural stratification (a purple arrow), proximal to which the small intestine was liquid-filled. In the ileocecal region, the colonic wall was thickened with smudgy peritoneal thickening (white arrows); E: Characteristic image of the pelvic liquid collection. Mild ascites was present in both the right and left iliac fossa (green arrows), together with a thickened peritoneum suggesting the presence of peritoneal involvement; F: Characteristic image of the chest computed tomography (CT) scan. Chest CT showed the presence of pleural effusion in the bilateral cavities and bilateral pleural hypertrophic thickening. Enlarged blood vessels extended to the hypertrophic lesions.
- Citation: Zhao XC, Xue CJ, Song H, Gao BH, Han FS, Xiao SX. Bowel inflammatory presentations on computed tomography in adult patients with severe aplastic anemia during flared inflammatory episodes. World J Clin Cases 2023; 11(3): 576-597
- URL: https://www.wjgnet.com/2307-8960/full/v11/i3/576.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i3.576