©The Author(s) 2022.
World J Clin Cases. Aug 16, 2022; 10(23): 8406-8416
Published online Aug 16, 2022. doi: 10.12998/wjcc.v10.i23.8406
Published online Aug 16, 2022. doi: 10.12998/wjcc.v10.i23.8406
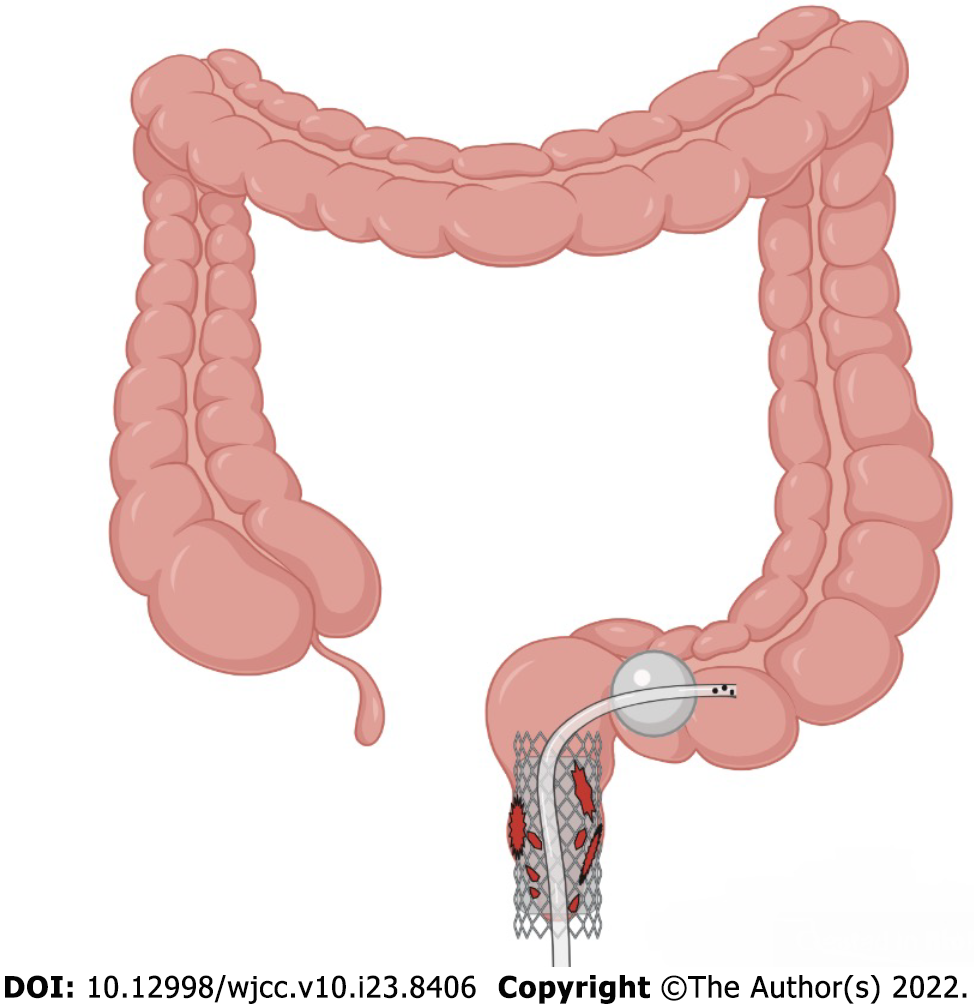
Figure 1 Schematic.
Self-expanding covered mental stent combined with transanal ileus drainage tube for the treatment of a complicated delayed rectal perforation.
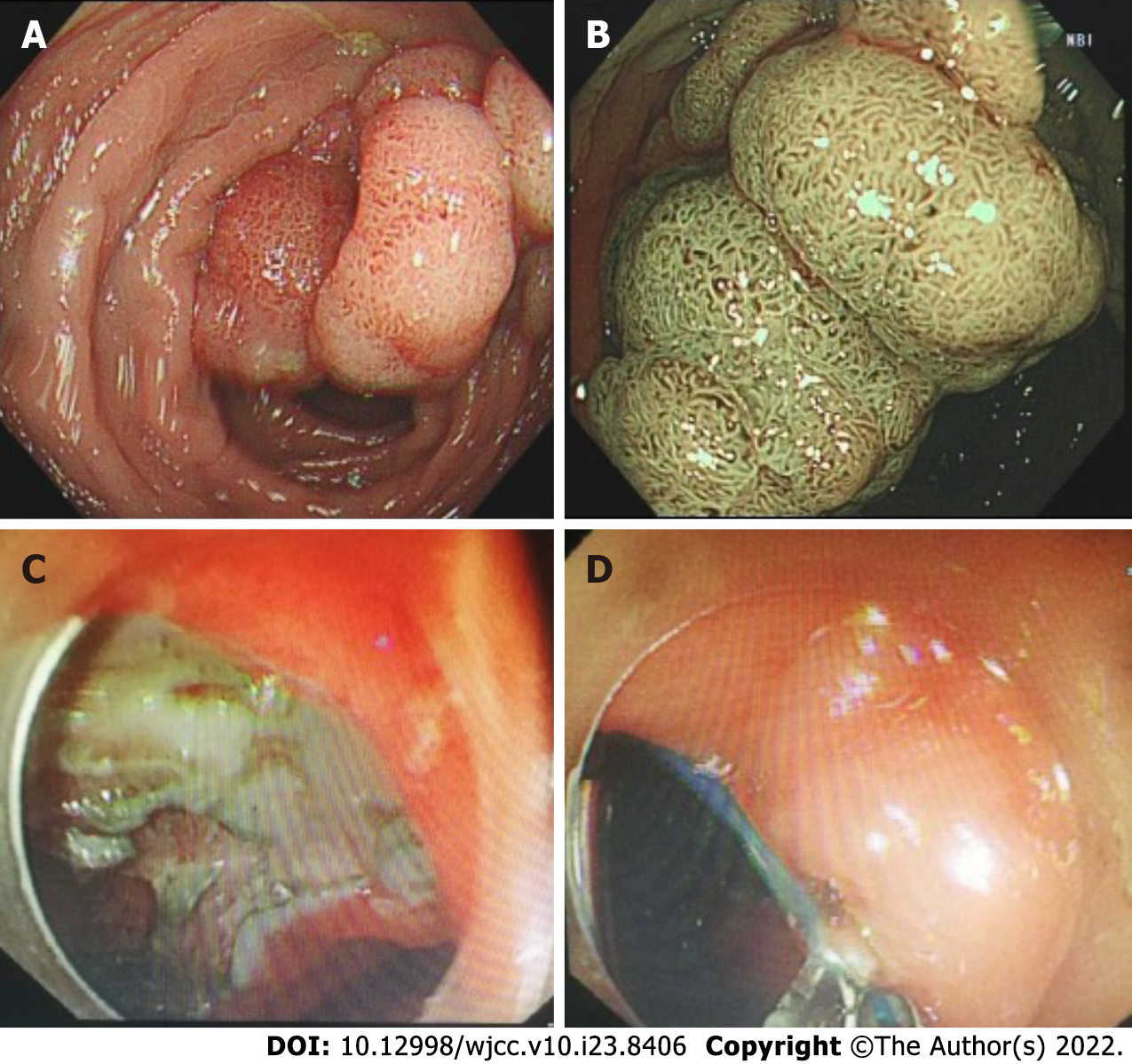
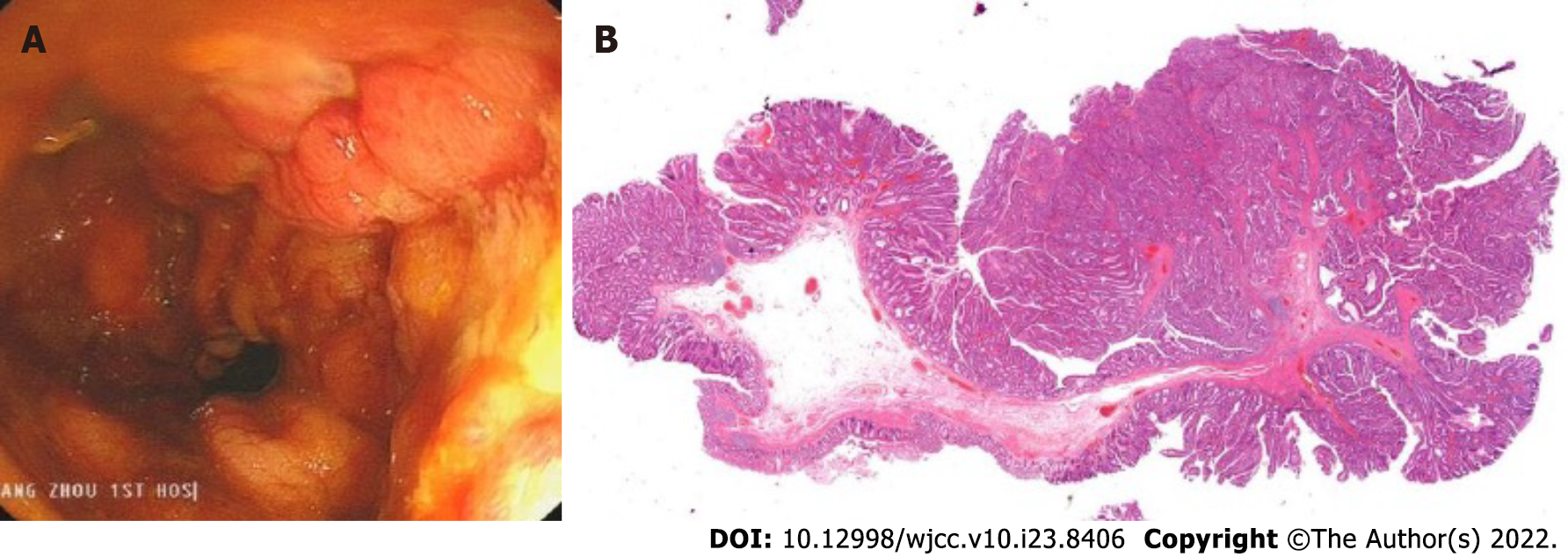
Figure 2 Tumor morphology and postoperative wound management.
A and B: Rectal laterally spreading tumor granular type (nodular mixed type), size of lesion 25 mm × 20 mm; C and D: Endoscopic submucosal dissection wound surface and purse-string suture.
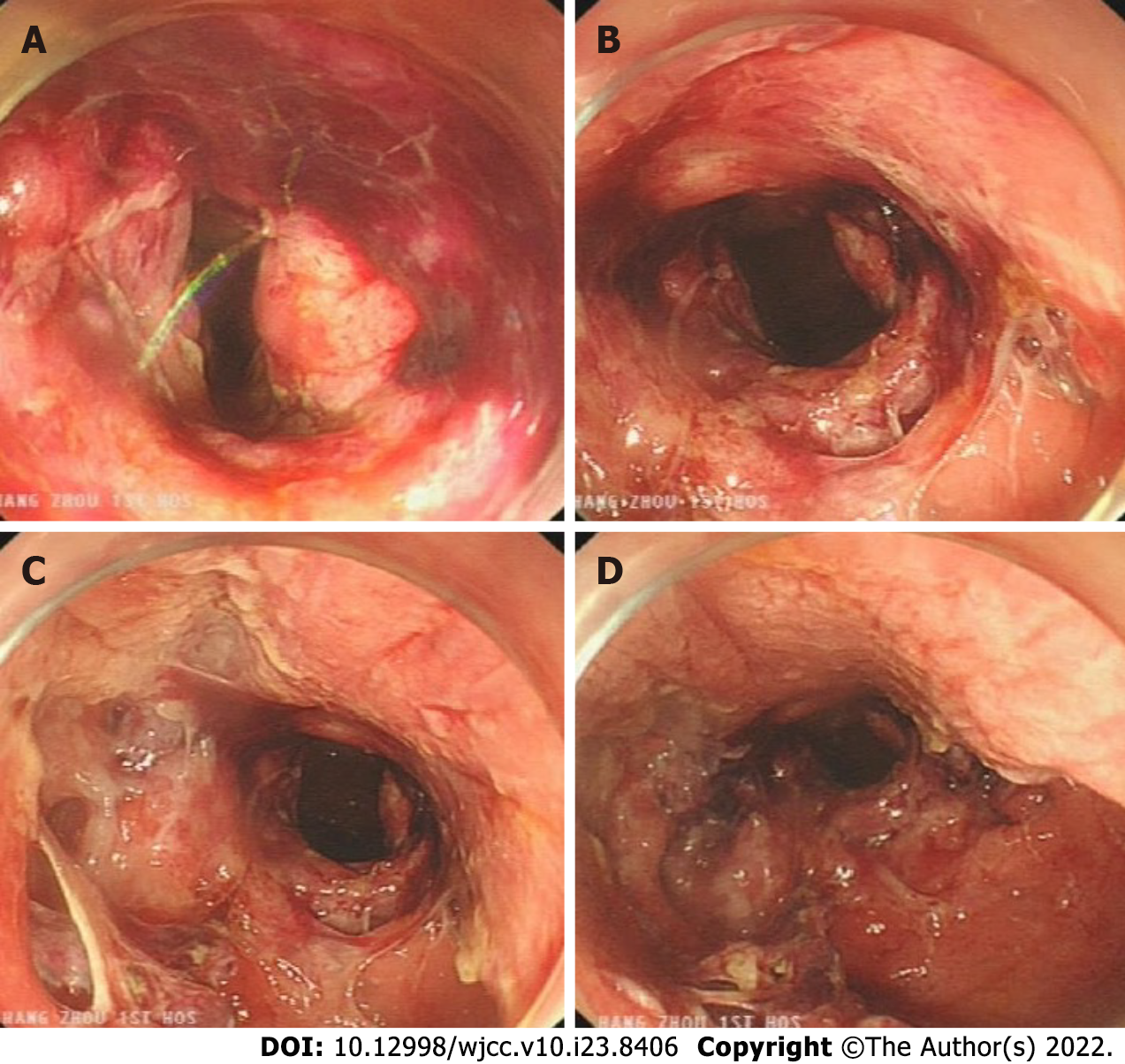
Figure 3 Complicated delayed rectal perforation.
A: Severe rectal injury, with a large amount of blood; B: The rectum is obviously perforated, and the surrounding wounds are reddened, bleeding and edematous; C: Multiple injuries to the mucosa around the perforation, and tearing of the rectal mucosa; D: A damaged internal anal sphincter.
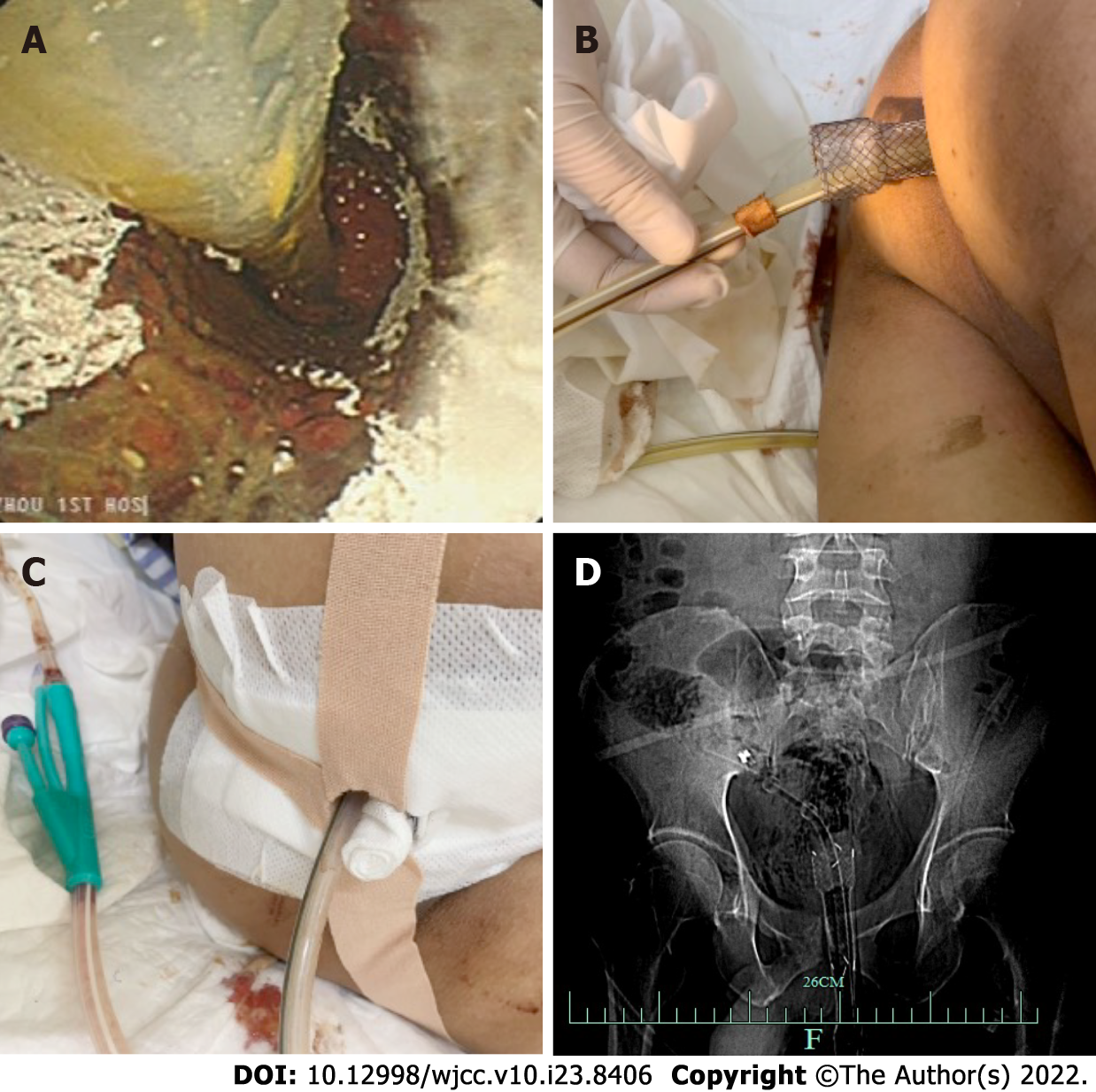
Figure 4 The self-expanding covered mental stent and transanal ileus drainage tube were inserted into the rectum.
A: Self-expanding covered mental stent and transanal ileus drainage tube (TIDT) into the rectum; B: The end part of the stent is retained outside the body; C: The stent and TIDT were fixed with medical adhesive tape; D: X-rays confirm the correct placement of the stent and TIDT in the body.
Figure 5 Routine management of self-expanding covered mental stent and transanal ileus drainage tube.
A: The status of the stents and transanal ileus drainage tube (TIDT) was observed daily; B: Continuous negative pressure drainage through TIDT; C: Keeping the perianal clean; D: The regular changing of the dressings to keep the stents and TIDT in a fixed state.
Figure 6 Removal of the metal stent and pathological findings.
A: After the metal stent was removed, it was observed that the wound began to heal, and the perforation and significant injury were no longer present; B: Tubular-villous adenoma with part of high-grade intraepithelial neoplasia (intramucosal carcinoma), infiltrating the muscularis mucosae, and with clean margin.
Figure 7 The pelvic free gas gradually decreased in the patient.
A: Day 2 computed tomography (CT), Metal tubular shadows were observed in the rectal lumen, and a lot of gas was observed around the intestinal canal; B: Day 5 CT: a lot of free air was trapped behind the peritoneum and in the pelvis, but this was slightly resolved on day 5, as compared the amount of air on Day 2 CT slice; C: Day 10 CT: The free air in the peritoneal cavity and behind the peritoneum was significantly reduced as compared with that on Day 5 CT slice; D: Day 17 CT: No clear manifestation of the original rectal stent was observed. A little amount of free air trapped in the pelvis was absorbed as compared with that on the Day 10 CT slice.
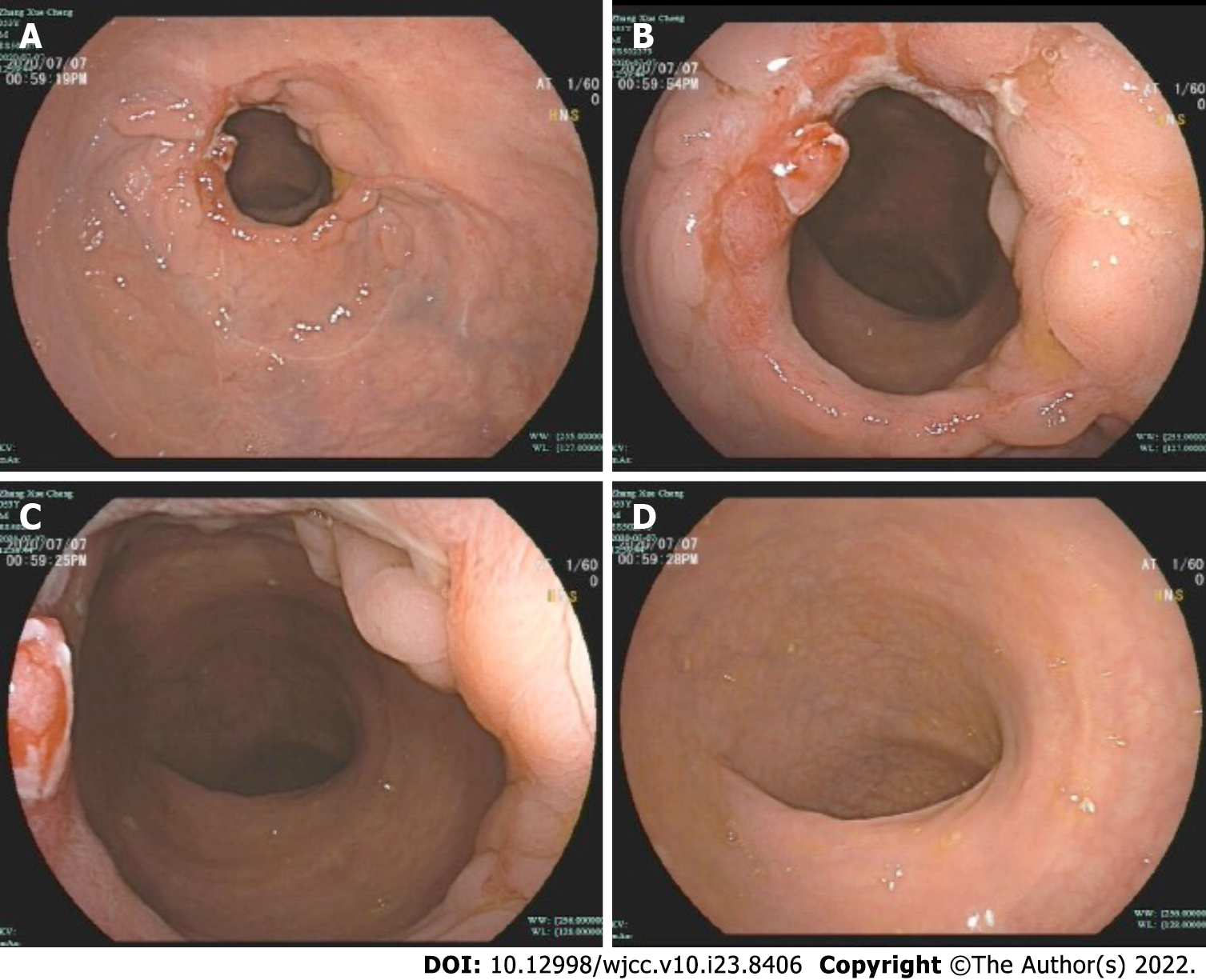
Figure 8 Follow-up after discharge (Day 42).
A: Observed from a distance, the wound surface was almost completely repaired; B: With close observation, some of the ulcers were still present; C: The rectum is slightly narrowed, but the endoscope can pass through; D: There was no obvious abnormalities in the distal intestinal mucosa.
- Citation: Cheng SL, Xie L, Wu HW, Zhang XF, Lou LL, Shen HZ. Metal stent combined with ileus drainage tube for the treatment of delayed rectal perforation: A case report. World J Clin Cases 2022; 10(23): 8406-8416
- URL: https://www.wjgnet.com/2307-8960/full/v10/i23/8406.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i23.8406