©The Author(s) 2022.
World J Clin Cases. Jun 16, 2022; 10(17): 5798-5804
Published online Jun 16, 2022. doi: 10.12998/wjcc.v10.i17.5798
Published online Jun 16, 2022. doi: 10.12998/wjcc.v10.i17.5798
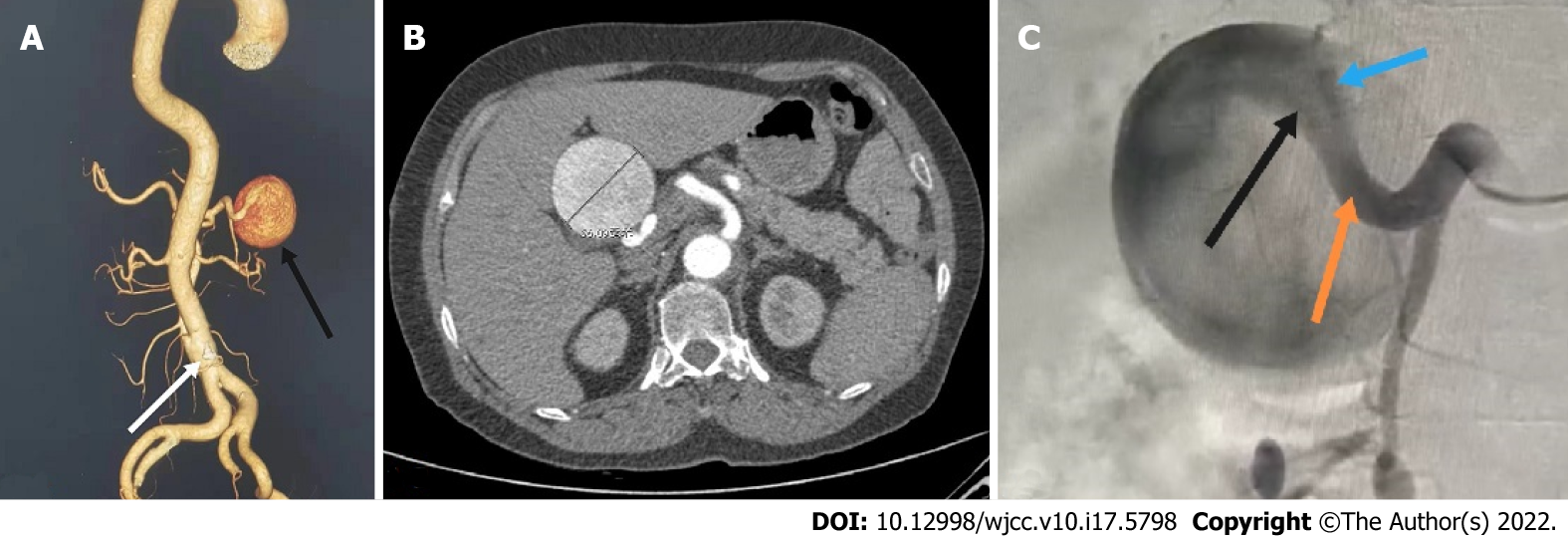
Figure 1 Computed tomography scan.
A: Abdominal computed tomography (CT) three-dimensional reconstruction showed a proper hepatic artery aneurysm (black arrow) and abdominal aortic dissection (white arrow); B: The patient's abdominal CT scan showed a huge proper hepatic artery aneurysm with a maximum diameter of approximately 56 mm; C: Abdominal aortography showed a huge proper hepatic aneurysm: A bit twisted, no collaterals, originated from the proper hepatic artery (orange arrow) and involving the bifurcation of the left (black arrow) and right hepatic arteries (blue arrow).
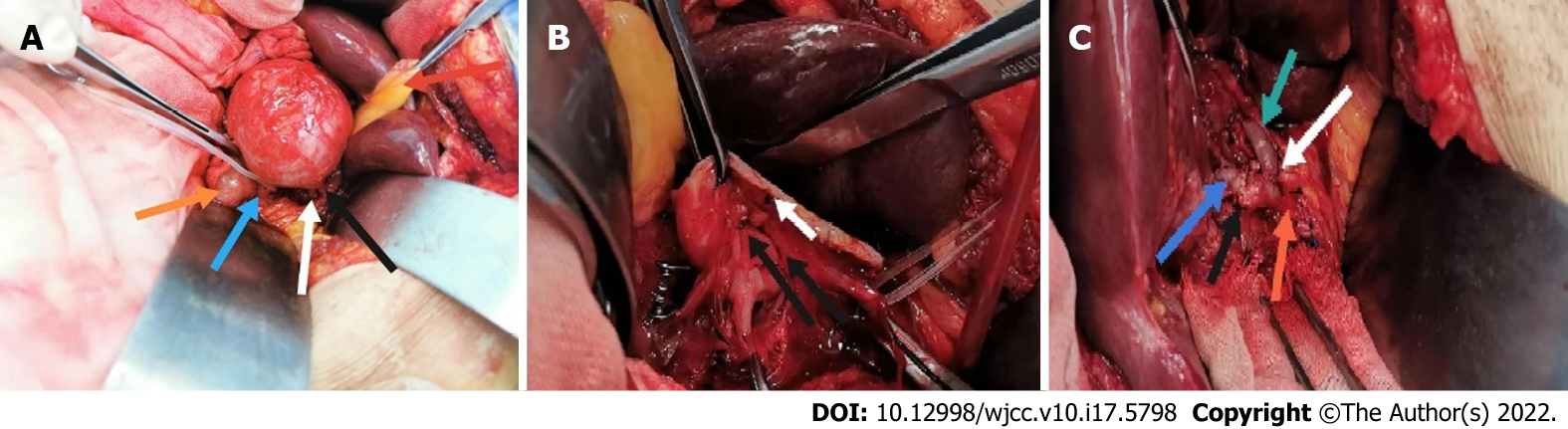
Figure 2 Open repair was performed six days later.
A: This is a general view of the isolated hepatic aneurysm. The red arrow indicates the gallbladder; the yellow arrow the descending duodenum; the green arrow the proper hepatic artery; the white arrow the right hepatic artery and the black arrow the left hepatic artery; B: This is a general view of the cut aneurysm. The white arrow indicates the aneurysm break and the black arrow the mural thrombus; C: The general view of the proper hepatic artery (red arrow) after suturing with the left (dark green arrow) and right hepatic arteries (light green arrow), respectively. The black arrow indicates the end-to-end anastomosis of the proper hepatic artery and the right hepatic artery while the white arrow indicates the end to side anastomosis of the proper hepatic artery and the left hepatic artery.
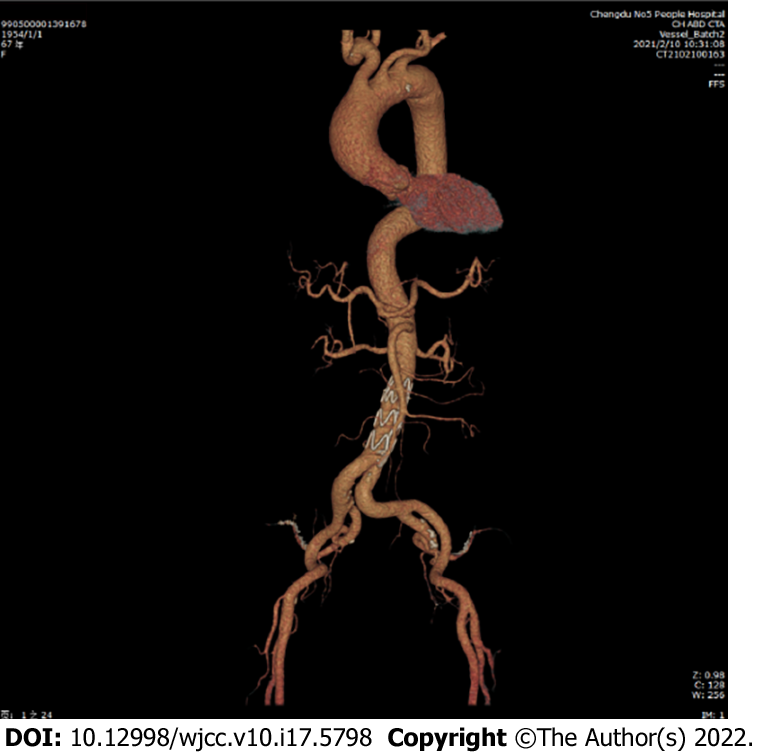
Figure 3 The patient was reexamined 3 mo after surgery and showed no complications.
The anastomotic end of the proper hepatic artery was unobstructed. The abdominal aortic dissection was well isolated.
- Citation: Wen X, Yao ZY, Zhang Q, Wei W, Chen XY, Huang B. Surgical repair of an emergent giant hepatic aneurysm with an abdominal aortic dissection: A case report. World J Clin Cases 2022; 10(17): 5798-5804
- URL: https://www.wjgnet.com/2307-8960/full/v10/i17/5798.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i17.5798