©The Author(s) 2022.
World J Clin Cases. Jun 16, 2022; 10(17): 5770-5775
Published online Jun 16, 2022. doi: 10.12998/wjcc.v10.i17.5770
Published online Jun 16, 2022. doi: 10.12998/wjcc.v10.i17.5770
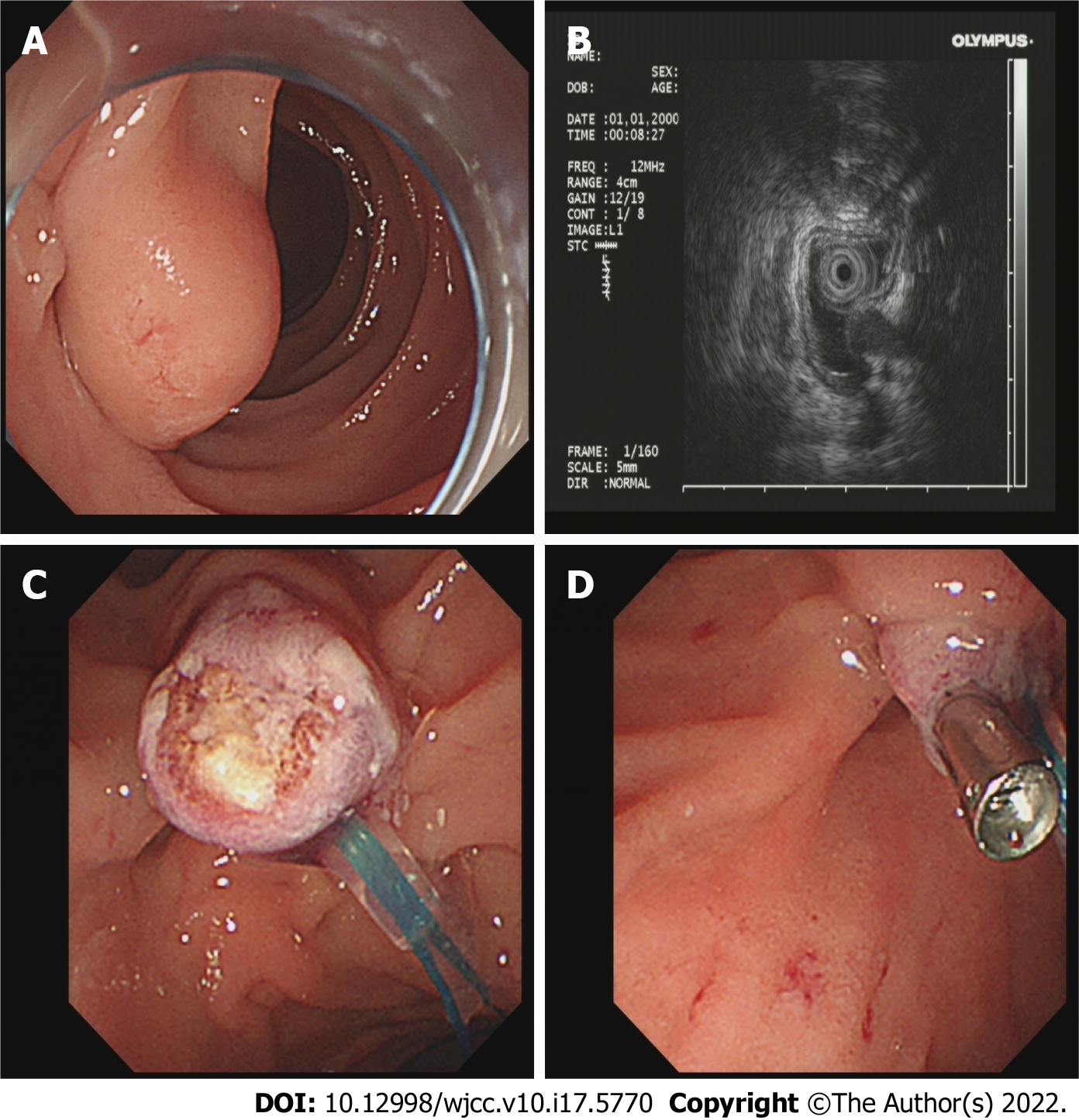
Figure 1 Endoscopic resection of the tumour.
A: Tumour in the descending part of the duodenum in the natural state; B: Using endoscopic ultrasonography to explore the tumour; C: Endoscopic electrocoagulation for resection of the tumour; D: A titanium clip was used to clamp the wound to stop the bleeding.
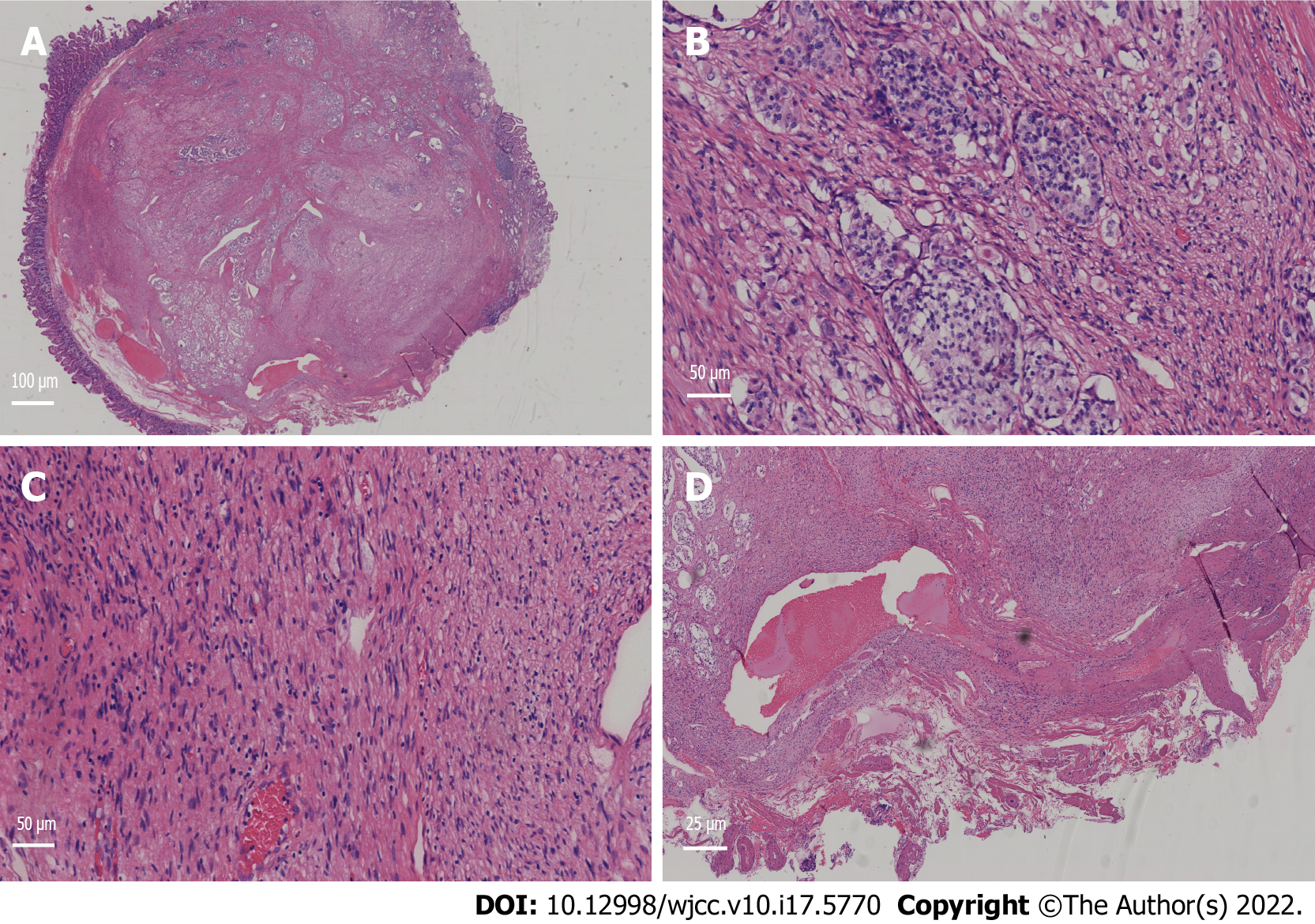
Figure 2 Pathological manifestation of the tumour under a light microscope.
A: Pathological tissue (Magnification: 100 ×). The lower right corner is the nesting tissue of the schwannoma, and the rest is the vesicle-like tissue of the neuroendocrine tumour; B: Neuroendocrine tumour tissue (Magnification: 200 ×); C: Schwannoma tissue (Magnification: 200 ×); D: The vertical incisal margin was negative, and there was no lymphatic vascular invasion (Magnification: 400 ×).
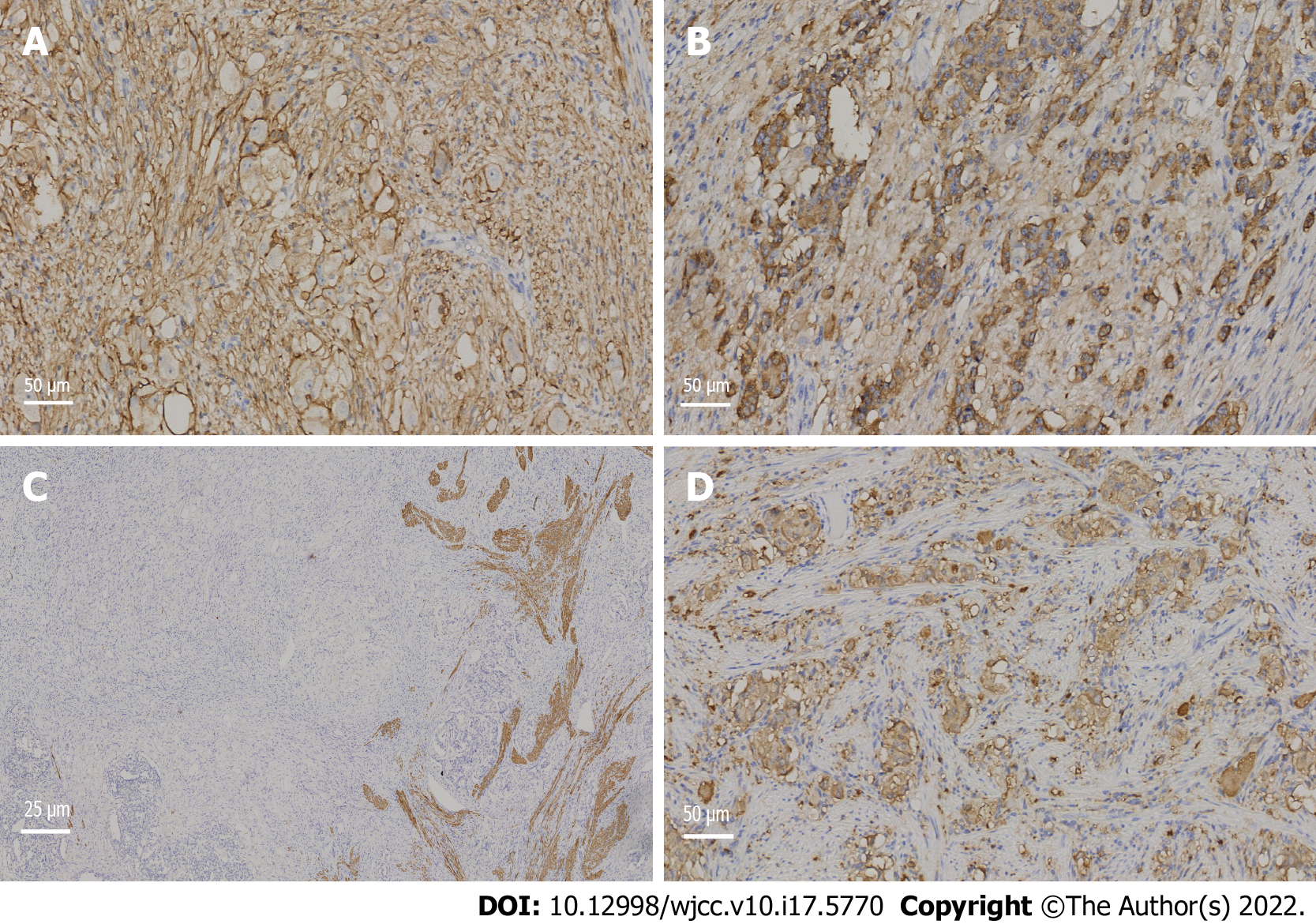
Figure 3 Immunohistochemical neuroendocrine tumour results.
A: CD56+ (Magnification: 200 ×); B: Chromogranin A+ (Magnification: 200 ×); C: Desmin+ (Magnification: 400 ×); D: Synaptophysin+ (Magnification: 200 ×).
Figure 4 Immunohistochemical results.
A: S100+ expression in schwannoma (Magnification: 200 ×); B: The antigen KI-67 index of the neuroendocrine tumour was approximately 1% (Magnification: 200 ×); C: The KI-67 index of the schwannoma was approximately 1% (Magnification: 200 ×).
- Citation: Zhang L, Zhang C, Feng SY, Ma PP, Zhang S, Wang QQ. Neuroendocrine tumour of the descending part of the duodenum complicated with schwannoma: A case report. World J Clin Cases 2022; 10(17): 5770-5775
- URL: https://www.wjgnet.com/2307-8960/full/v10/i17/5770.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i17.5770