©The Author(s) 2022.
World J Clin Cases. May 26, 2022; 10(15): 5103-5110
Published online May 26, 2022. doi: 10.12998/wjcc.v10.i15.5103
Published online May 26, 2022. doi: 10.12998/wjcc.v10.i15.5103
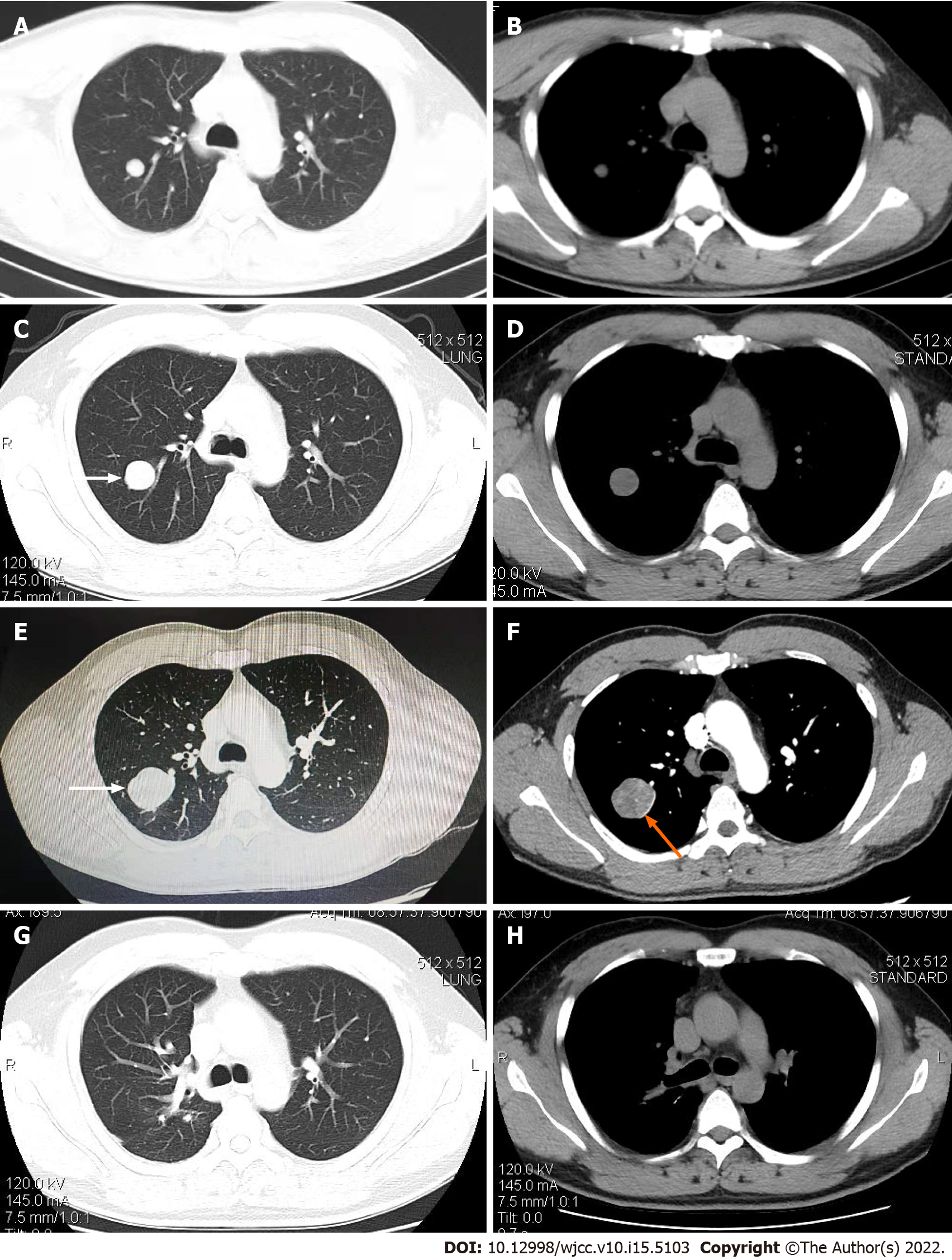
Figure 1 Computed tomography scans of the chest.
A and B: The shadow of the round nodules in the upper lobe of the right lung was detected in 2018, with a maximum diameter of about 14 mm and smooth edges; C and D: In 2019, the detected lesion had grown significantly larger, reaching a maximum diameter of approximately 30 mm, with smooth edges and shallow lobes (white arrows); E and F: By 2020, the lesion had grown to approximately 20 mm × 34 mm × 42 mm in size, with irregular density, smooth edges spotted with calcifications, slightly shallow lobes (white arrows), an uneven level of enhancement, and a ring-shaped enhanced image around the perimeter (orange arrow); G and H: From postoperative to 2021, no shadows with an abnormally high density were observed.
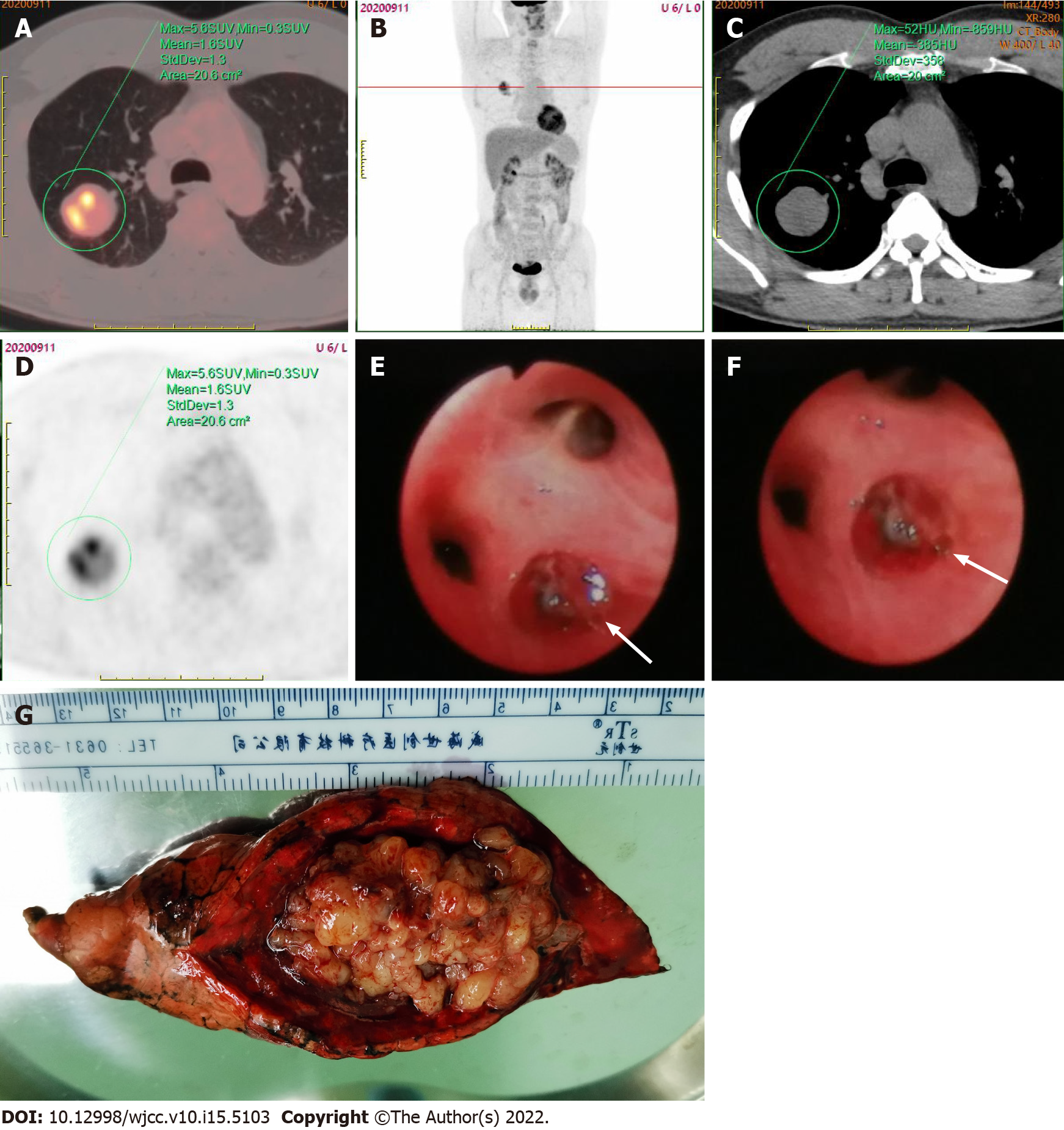
Figure 2 Positron emission tomography-computed tomography scan.
A-D: Showed a solitary round mass in the upper lobe of the right lung, with unevenly increased radioactivity uptake and an SUVmax of 5.6; E and F: Fiberoptic bronchoscopy revealed the presence of new organisms (white arrows) at the posterior opening of the upper right lobe, with a smooth capsule, surrounded by purulent secretions, and oozing a small amount of blood; G: The specimen obtained following the thoracoscopic resection of the posterior segment of the right upper lobe of the lung was grayish yellow in color, with some small round-like changes and a soft texture.
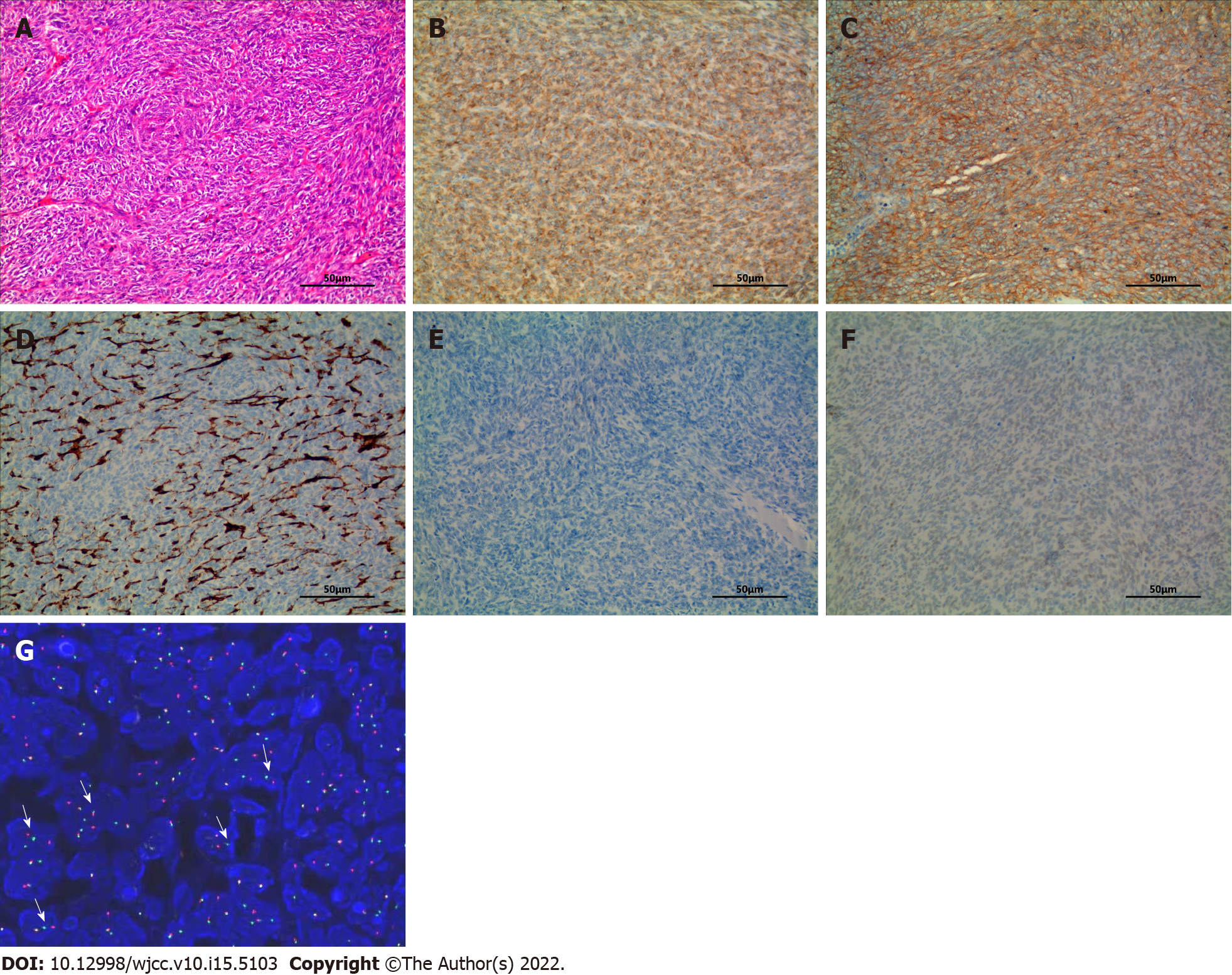
Figure 3 Hematoxylin and eosin staining.
A: Hematoxylin and eosin (H&E) staining of tissue sections of posterior segment of the right lung upper lobe obtained from surgery (H&E 200×). The tumor was composed of spindle cells, which were arranged in dense cellular sheets or vague fascicles, with a herringbone architectural pattern; B-F Immunohistochemistry (IHC) revealed the tumor cells were diffusely positive for BCL-2 (B) and CD99 (C), and negative for CD34 (D), EMA (E) and TLE1 (F). The blood vessels inside the tumor showed positive staining for CD99 (C) (IHC 200×); G: Fluorescence in situ hybridization analyses: Red and green signals show break-apart regions (white arrows), representing the splitting of SS18 (synovial sarcoma translocation, SYT).
- Citation: He WW, Huang ZX, Wang WJ, Li YL, Xia QY, Qiu YB, Shi Y, Sun HM. Solitary primary pulmonary synovial sarcoma: A case report. World J Clin Cases 2022; 10(15): 5103-5110
- URL: https://www.wjgnet.com/2307-8960/full/v10/i15/5103.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i15.5103