©The Author(s) 2022.
World J Clin Cases. May 26, 2022; 10(15): 4942-4948
Published online May 26, 2022. doi: 10.12998/wjcc.v10.i15.4942
Published online May 26, 2022. doi: 10.12998/wjcc.v10.i15.4942
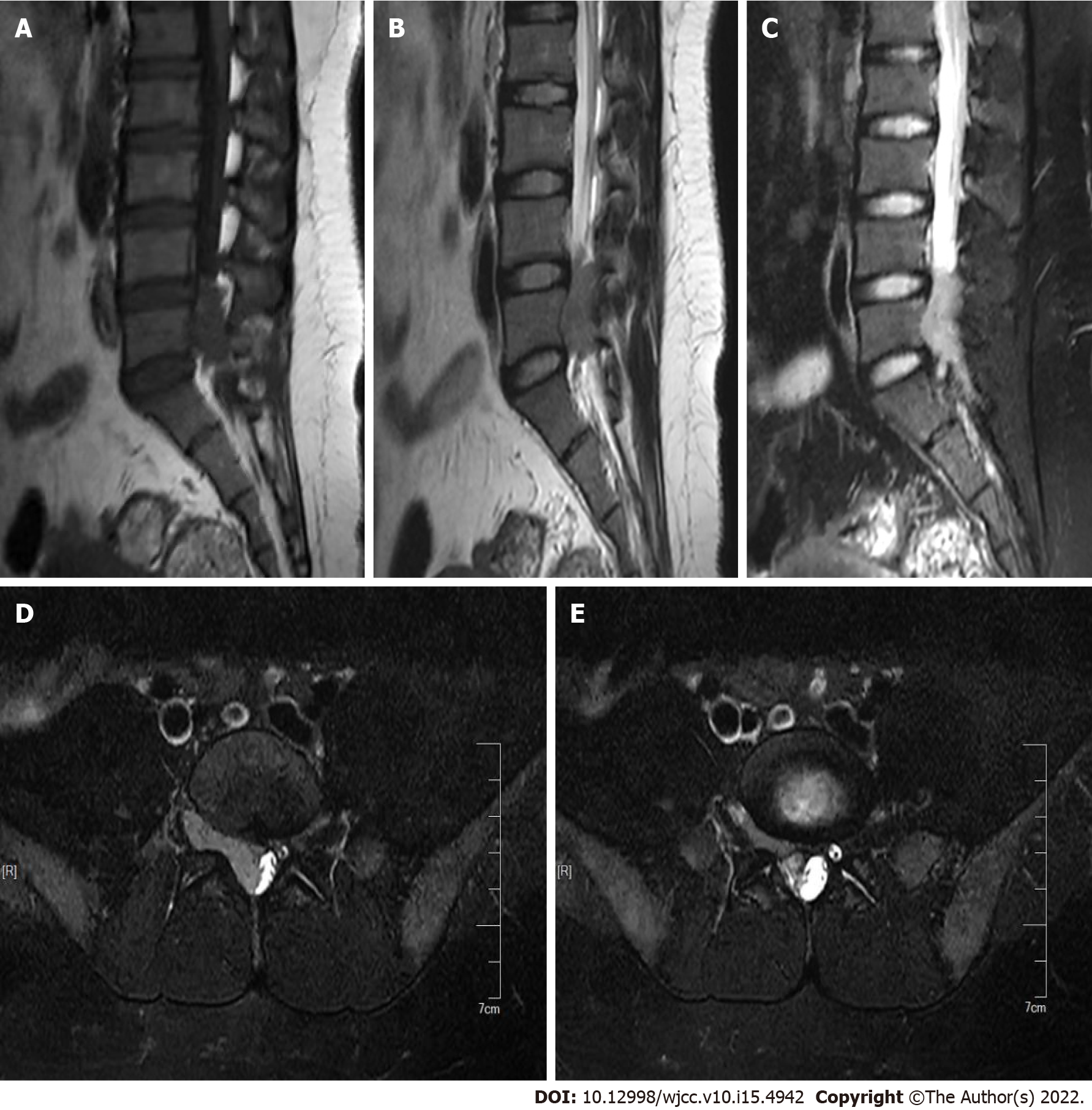
Figure 1 Preoperative magnetic resonance imaging examination.
A: Magnetic resonance imaging (MRI) shows low intensity on T1W1; B: MRI shows slightly high and slightly low intensities on T2W1, with a few small nodules of high intensity visible; C: MRI shows high intensity on STIR; D: With the mass extending into the intervertebral foramen in cross section; E: With the mass extending into the intervertebral foramen in cross section.
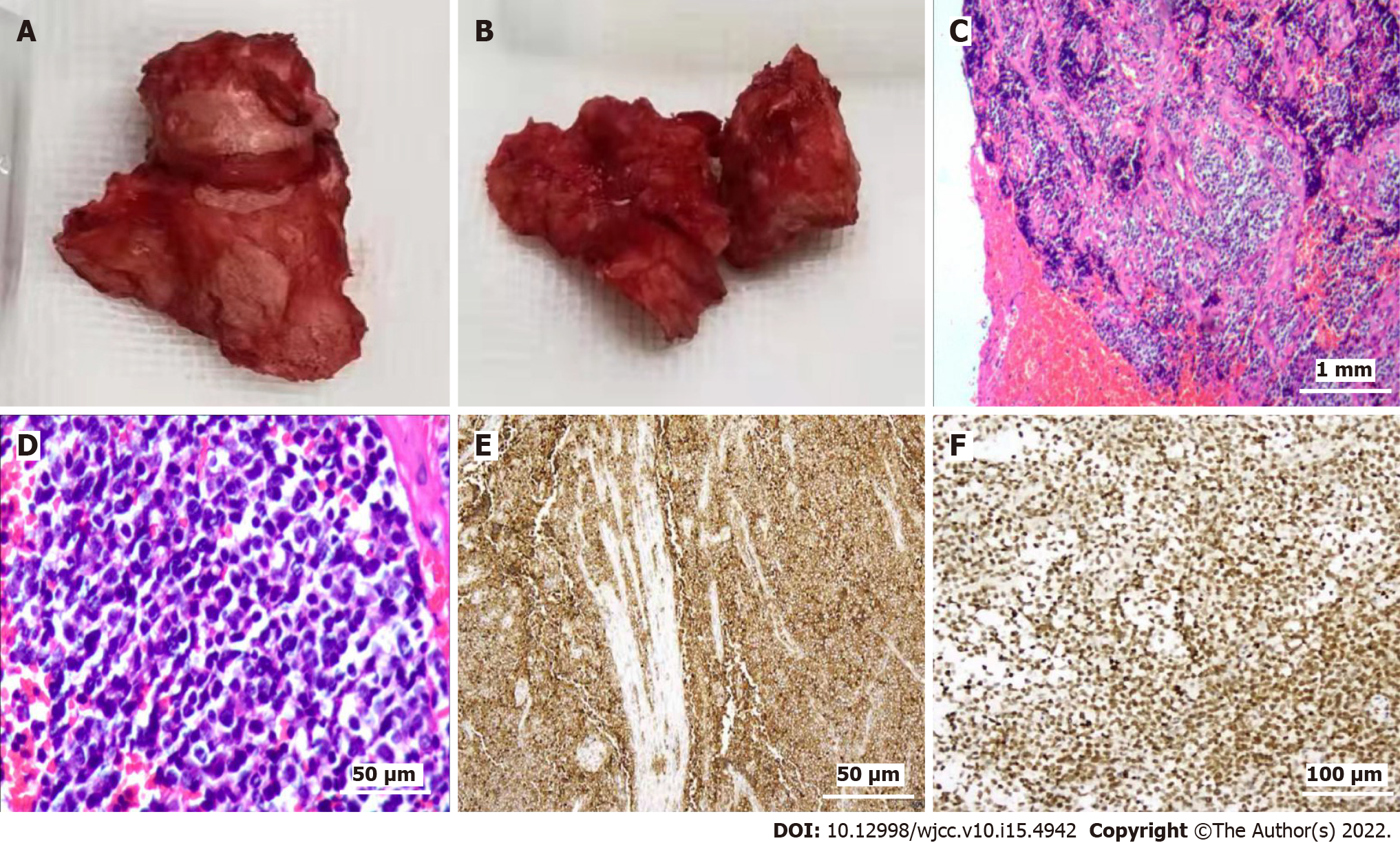
Figure 2 Tissue diagnosis and immunohistochemistry results.
A and B: Dark red, fish-like fleshy nerve root tumors were cut intraoperatively; C: Tumor boundaries were not clear, large areas of necrosis were visible, and tumor cells were segmented by fibrous tissue and exhibited a nest-like structure; D: Cells were round, nuclei were vacuolar, and cytoplasm was sparse; E and F: Mitotic observations were consistent with small round cell malignancy. Immunohistochemistry showed positivity for CD99 and S100.
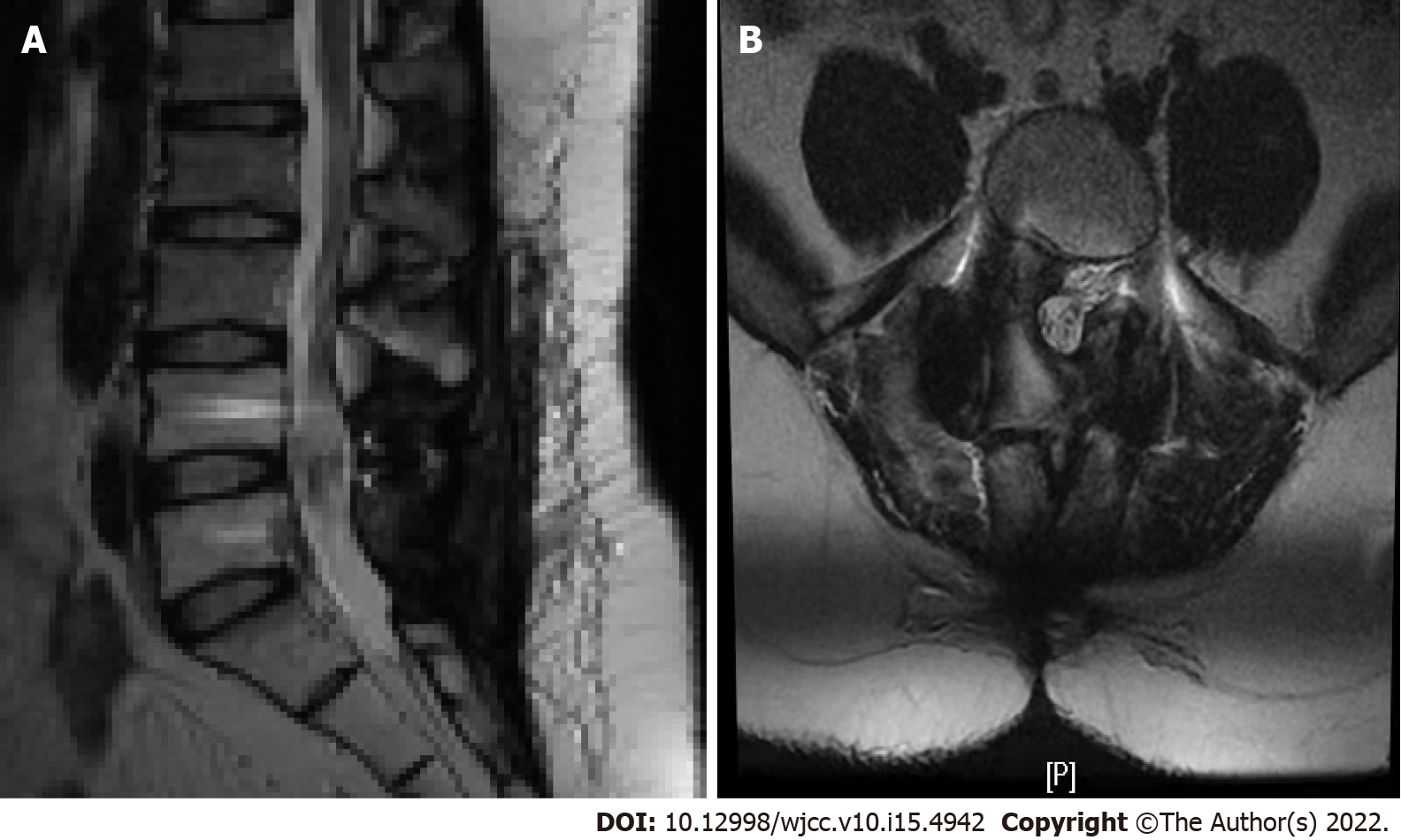
Figure 3 Magnetic resonance imaging examination after 1 year and 3 mo of follow-up.
A and B: Magnetic resonance imaging examination showed that the space occupying the spinal canal at the L4-5 level had been removed, and no obvious metabolic signs of recurrence were observed.
- Citation: Lei LH, Li F, Wu T. Primary extraskeletal Ewing’s sarcoma of the lumbar nerve root: A case report. World J Clin Cases 2022; 10(15): 4942-4948
- URL: https://www.wjgnet.com/2307-8960/full/v10/i15/4942.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i15.4942