Published online Dec 20, 2025. doi: 10.5662/wjm.v15.i4.105053
Revised: March 20, 2025
Accepted: April 3, 2025
Published online: December 20, 2025
Processing time: 207 Days and 0.4 Hours
Atrial fibrillation (AF) remains the most common cardiac arrhythmia. The safety of endoscopic retrograde cholangiopancreatography (ERCP) in patients with AF remains largely unknown.
To analyze the effect of AF on hospital outcomes in patients undergoing ERCP.
We performed a retrospective cohort study using the Nationwide Inpatient Sample database. Adult patients with AF who underwent an inpatient ERCP were identified, then stratified by timing of ERCP, via international classification of diseases-10 codes. The primary outcome was all-cause in-hospital mortality. Secondary outcomes, including resource utilization, were assessed. Statistical analysis was performed using STATA software.
Of the 433245 patients that underwent an ERCP, 49615 had a diagnosis of AF. Patients with AF had a significantly higher in-hospital mortality compared to those without AF [3.82% vs 1.13%, odds ratio (OR) = 1.93, P < 0.01]. AF was significantly associated with increased hospital stay (+1.71 days), hospital charges ($21210), shock (OR = 2.17), sepsis (OR = 1.34), intensive care unit admission (OR = 2.41), acute kidney injury (OR = 1.51), as well as a decreased likelihood of discharge to home (OR = 0.59), (all with P < 0.01). These results were consistent after propensity score matching. Upon subgroup analysis, patients with AF, whom underwent ERCP > 72 hours, had worse outcomes including higher in-hospital mortality (adjusted OR = 1.47, P < 0.01).
By way of this large, national analysis it appears AF is associated with sig
Core Tip: Atrial fibrillation (AF) significantly worsens hospital outcomes, including increased mortality, longer hospital stays, higher costs, and complications, in patients undergoing endoscopic retrograde cholangiopancreatography (ERCP). Delaying ERCP beyond 72 hours in patients with AF further exacerbates these risks. Prospective studies are needed to optimize management strategies for this high-risk population.
- Citation: Bangolo AI, Donepudi RC, Nagesh VK, Sandrugu J, Kianifar Aguilar I, Sarraf R, Suliman S, Wadhwani N, Espinoza CEA, Tran HHV, Levy C, Alqinai B, Rambaransingh A, Adibeig M, Ghosal A, Siddiqui G, Bhandari N, Kotnani S, Akrama AA, Thota A, Gill H, Aziz R, Lee CH, Abbisetty SD, Bhangu S, Randhawa K, Habib Z, Khan SA, Lee CYF, Sanoh M, Jacobson K, Lo A, Weissman S. Impact of atrial fibrillation in hospitalized patients undergoing endoscopic retrograde cholangiopancreatography: A nationwide analysis. World J Methodol 2025; 15(4): 105053
- URL: https://www.wjgnet.com/2222-0682/full/v15/i4/105053.htm
- DOI: https://dx.doi.org/10.5662/wjm.v15.i4.105053
Report on first endoscopic retrograde cholangiopancreatography (ERCP) was published in 1968[1]. With advancement in diagnostic imaging, the role of ERCP has been expanded to include both diagnostic and therapeutic domains. More than 50000 inpatient ERCP procedures are performed in the United States annually[2]. Common indications for ERCP include biliary pathologies (choledocholithiasis, benign and malignant stricture, sphincter of Oddi dysfunction), pancreatic diseases (recurrent acute pancreatitis, chronic pancreatitis, duct leaks, fluid collection, pancreatic cancer)[3].
Atrial fibrillation (AF) is the most common cardiac arrhythmia present in hospitalized patients, affecting nearly 1% of the United States population, and the prevalence is expected to increase 2.5-fold by 2050[4]. Patients with AF are usually on anticoagulants to reduce the risk of having a stroke—rendering it challenging to manage these patients when undergoing invasive medical procedures. As such, it can affect the decision on timing and planning of invasive pro
Data regarding the outcomes of patients with AF undergoing ERCP remains limited. Herein, we sought to analyze the effect AF has on hospitalization outcomes in patients undergoing ERCP.
In this retrospective cohort study, we used the Healthcare Cost and Utilization Project NIS database. NIS is the largest publicly available all-payer inpatient database in the United States. The NIS database contains data from 14.1 million hospital stays[8]. It contains de-identified clinical and nonclinical elements at both the patient-level and hospital-level. Institutional Review Board approval was not required for this study as it was performed using de-identified and publicly available data.
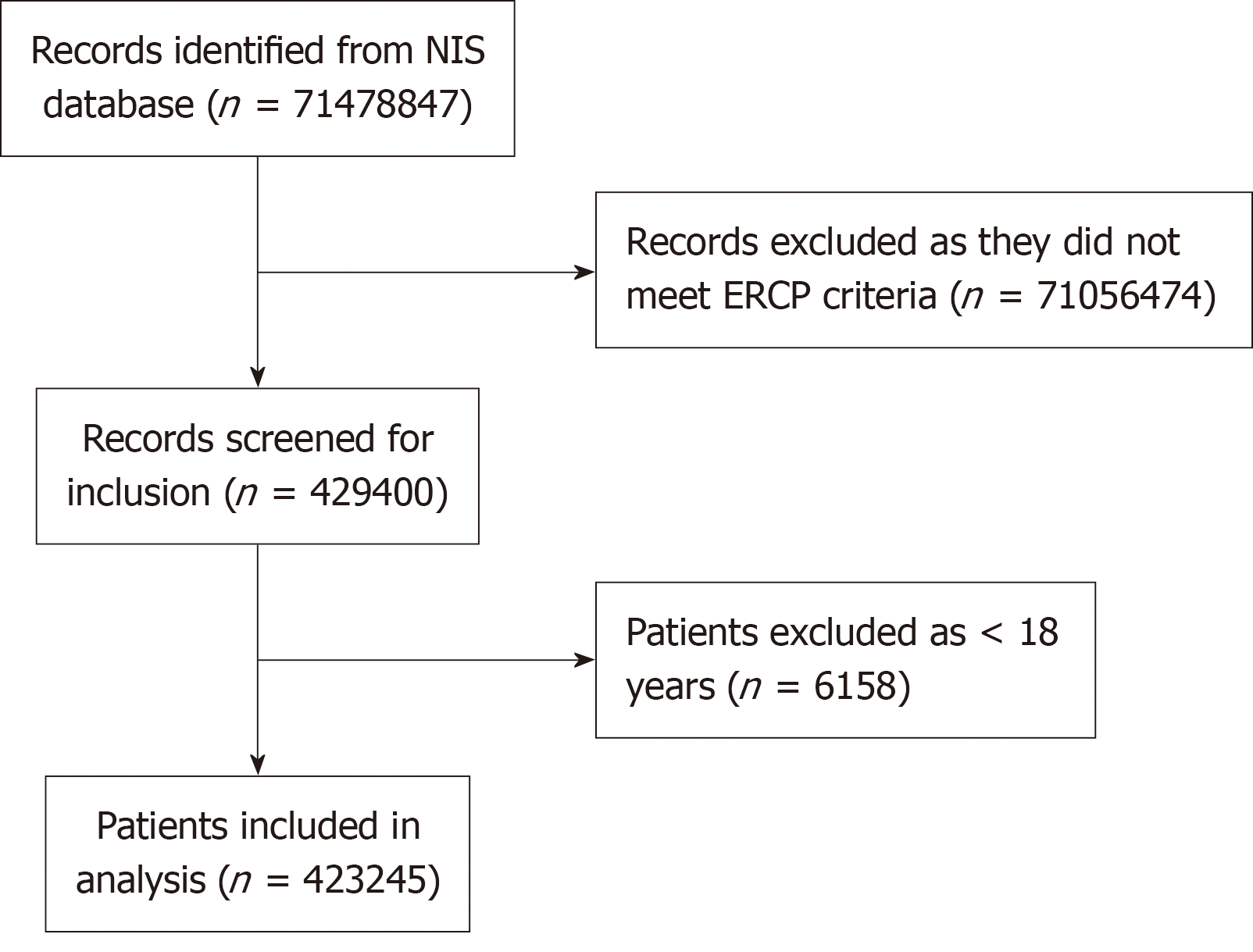
The inclusion criteria comprised all patients who underwent ERCP during hospitalization, totaling 429400 patients. Patients younger than 18 years were excluded. The total number of patients included in the study was 423245, divided into two groups: (1) 49018 patients with AF; and (2) 374227 patients without.
We used international classification of diseases (ICD)-10-CM codes (l48, l48.1, l48.2, l48.91) to identify all adult (> 18 years old) patients with a primary or secondary diagnosis of AF, who underwent an ERCP (ICD-10: BF111ZZ) during hospitalization. We stratified this population according to the timing of ERCP: (1) ERCP within 24 hours of admission; (2) ERCP between 24-48 hours of admission; (3) ERCP between 48-72 hours of admission; and (4) ERCP after 72 hours of admission. Inclusion and exclusion criteria are shown in a flow diagram (Figure 1).
Patient and hospital level demographics collected included: (1) Age; (2) Sex; (3) Race; (4) Median household income; (5) Insurance; (6) Hospital bed size; (7) Hospital teaching status; (8) Hospital region; and (9) Hospital location. Burden of comorbidities was assessed using Charlson comorbidity index.
The primary outcome was all-cause in-hospital mortality. Secondary outcomes were: (1) Mean length of stay (LOS); (2) Mean hospitalization charges; (3) Costs mean time to ERCP; (4) Incidence of shock; (5) Incidence of sepsis; (6) Incidence of acute kidney injury (AKI); (7) Incidence of intensive care unit (ICU) admission; (8) Incidence of blood transfusion; and (9) Likelihood of discharge to home.
Statistical analyses were performed using STATA, version 16.0 (StataCorp., College Station, Texas, United States). Univariate screen was initially performed to calculate unadjusted odds ratio (OR) and a multivariate logistic regression model to calculate adjusted OR (aOR). Logistic regression was used for binary outcomes and linear regression was used for continuous outcomes. Proportions were compared using the Fisher exact test and continuous variables were compared using the Student t-test. Propensity score matching (PSM) with 1:1 matching was also performed on un
A total of 433245 adult patients underwent ERCP and 49615 (11.45%) had a diagnosis of AF. Mean age was 59.9 years, and majority of patients were female (57.44%) and white (66.98%). Medicare was the primary payer insurance (48.3%) and patients were predominantly admitted to teaching hospitals (71.84%) (Tables 1 and 2).
| Variable | |
| Total study population | 433245 |
| Female | 248856 (57.44) |
| Mean age in years | 59.9 |
| Insurance provider | |
| Medicare | 209257 (48.30) |
| Medicaid | 66200 (15.28) |
| Private | 134912 (31.14) |
| Uninsured | 22876 (5.28) |
| Charlson comorbidity index | |
| 0 | 168749 (38.95) |
| 1 | 89378 (20.63) |
| 2 | 56148 (12.96) |
| 3 or more | 118970 (27.46) |
| Median income in patient zip code | |
| $1–$38999 | 121611 (28.07) |
| $39000–$47999 | 114680 (26.47) |
| $48000–$62999 | 107401 (24.79) |
| $63000 | 89553 (20.67) |
| Hospital region | |
| Northwest | 74864 (17.28) |
| Midwest | 96180 (22.20) |
| South | 164806 (38.04) |
| West | 97395 (22.48) |
| Hospital location | |
| Rural | 20276 (4.68) |
| Urban | 412969 (95.32) |
| Hospital size | |
| Small | 67586 (15.60) |
| Medium | 119965 (27.69) |
| Large | 245694 (56.71) |
| Teaching hospital | 311243 (71.84) |
| Race | |
| White | 290187 (66.98) |
| Black | 41071 (9.48) |
| Hispanic | 67759 (15.64) |
| Asian or Pacific Islander | 16203 (3.74) |
| Native American | 3555 (0.82) |
| Other | 14470 (3.34) |
| Weekend admission | 102235 (23.60) |
| Variable | With AF: 49615 | Without AF: 383630 | P value |
| Female | 22475 (45.30) | 226380 (59.01) | < 0.01 |
| Mean age in years | 76.40 | 57.70 | < 0.01 |
| Insurance provider | < 0.01 | ||
| Medicare | 41910 (84.47) | 167032 (43.54) | |
| Medicaid | 1677 (3.38) | 64641 (16.85) | |
| Private | 5596 (11.28) | 129475 (33.75) | |
| Uninsured | 432 (0.87) | 22482 (5.86) | |
| Charlson comorbidity index | < 0.01 | ||
| 0 | 7482 (15.08) | 161239 (42.03) | |
| 1 | 9015 (18.17) | 80370 (20.95) | |
| 2 | 9104 (18.35) | 47071 (12.27) | |
| 3 or more | 24014 (48.40) | 94950 (24.75) | |
| Median income in patient zip code | < 0.01 | ||
| $1–$38999 | 11987 (24.16) | 109603 (28.57) | |
| $39000–$47999 | 13639 (27.49) | 101048 (26.34) | |
| $48000–$62999 | 12503 (25.2) | 94910 (24.74) | |
| $63000 | 11486 (23.15) | 78069 (20.35) | |
| Hospital region | < 0.01 | ||
| Northwest | 10141 (20.44) | 64718 (16.87) | |
| Midwest | 11958 (24.10) | 84206 (21.95) | |
| South | 17494 (35.26) | 147314 (38.40) | |
| West | 10022 (20.20) | 87392 (22.78) | |
| Hospital location | 0.05 | ||
| Rural | 2128 (4.29) | 18145 (4.73) | |
| Urban | 47487 (95.71) | 365485 (95.27) | |
| Hospital size | < 0.05 | ||
| Small | 7124 (14.36) | 59424 (15.49) | |
| Medium | 13922 (28.06) | 106073 (27.65) | |
| Large | 28569 (57.58) | 218133 (56.86) | |
| Teaching hospital | 35772 (72.10) | 275446 (71.80) | 0.59 |
| Race | < 0.01 | ||
| White | 41309 (83.26) | 249282 (64.98) | |
| Black | 2575 (5.19) | 38516 (10.04) | |
| Hispanic | 2789 (5.62) | 64526 (16.82) | |
| Asian or Pacific Islander | 1567 (3.16) | 14654 (3.82) | |
| Native American | 264 (0.53) | 3302 (0.86) | |
| Other | 1111 (2.24) | 13350 (3.48) | |
| Weekend admission | 11932 (24.05) | 90306 (23.54) | 0.27 |
The most common primary diagnosis was “sepsis (unspecified organism)” (6.6%). This was followed by “obstruction of bile duct” (5.02%), “calculus of bile duct without cholangitis or cholecystitis without obstruction” (4.31%), “calculus of bile duct without cholangitis or cholecystitis with obstruction” (3.43%) and “biliary acute pancreatitis” (2.97%) (Table 3).
| Serial number | Diagnosis |
| 1 | Sepsis, unspecified organism |
| 2 | Obstruction of bile duct |
| 3 | Calculus of bile duct without cholangitis or cholecystitis without obstruction |
| 4 | Calculus of bile duct without cholangitis or cholecystitis with obstruction |
| 5 | Biliary acute pancreatitis |
Total all cause in-hospital mortality was 1.44% (6245 out of 433245 patients). The total mortality was higher in patients with AF (1895 patients) compared to patients without AF (4350 patients) (3.82% vs 1.13%). There was a significant difference in all cause in-hospital mortality between patients with AF compared to patients without AF [aOR = 1.93, (95%CI: 1.68-2.22), P < 0.01].
The mean time to ERCP in all the study population was 2.22 days. In patients with AF, the mean time to ERCP was 2.94 days and in patients without AF, it was 2.13 days. Patients with AF had a significantly longer mean time to ERCP. The mean adjusted difference was 0.8 days (95%CI: 0.72-0.89, P < 0.01).
The overall mean LOS was 5.92 days for all patients undergoing ERCP. Mean LOS was 5.63 days (95%CI: 5.57-5.70) in patients without AF and 8.12 days (95%CI: 7.95-8.29) in patients with AF. Patients with AF had significantly longer mean LOS compared to patients who did not have AF (+1.71 days, P < 0.01).
The mean hospitalization charges and cost for patients undergoing ERCP was $82950 and $19939 respectively. There was a significant difference in mean hospitalization charges [$+21210 (95%CI: $18370-$24048, P < 0.01)], and in mean hospitalization costs [$+4869 (95%CI: $4183-$5556, P < 0.01)] between those with and without AF.
The overall incidence of shock was 4.06% in patients undergoing ERCP. The incidence of shock in patients with AF was 10.27% and in patients without AF was 3.26%. There was a significant difference in the likelihood of shock in patients who had AF compared to patients without AF (aOR = 2.17, 95%CI: 1.98-2.38, P < 0.01).
Out of the 433245 patients undergoing ERCP, 15880 (3.66%) patients were diagnosed with sepsis during the hospital stay. Patients with AF had 6.30% incidence of sepsis compared to 3.32% in patients without AF. There was a significant difference in the likelihood of sepsis between patients who had AF compared to patients without AF (aOR = 1.34, 95%CI: 1.21-1.48, P < 0.01).
The overall incidence of AKI in patients undergoing ERCP was 63370 (14.62%). Patients with AF had 29.47% incidence of AKI compared to 12.7% in patients without AF. There was a significant difference in the likelihood of AKI between patients who had AF compared to patients without AF (aOR = 1.51, 95%CI: 1.43-1.60, P < 0.01).
The total incidence of ICU admission in patients undergoing ERCP was 12470 (2.87%). There was a significant difference in likelihood of ICU admission in patients who had AF compared to patients who did not have AF (7.27% vs 2.30%, aOR = 2.41, 95%CI: 2.16-2.69, P < 0.01).
Overall, 1365 (0.31%) patients undergoing ERCP needed blood transfusion. The rate of blood transfusion in patients with AF was 0.49% and in patients without AF was 0.29%. On multivariate analysis, there was no significant difference in blood transfusion in these groups (aOR = 1.37, 95%CI: 0.96-1.96, P = 0.08).
A total of 323985 (74.78%) patients undergoing ERCP were discharged home after the hospitalization. Total 78.2% patients without AF were discharged home compared to 48.34% patients with AF. There was a significant difference in likelihood of discharge to home in patients who had AF compared to patients who did not have AF (aOR = 0.59, 95%CI: 0.56-0.62, P < 0.01).
The results of the PSM outcome analysis are presented in Table 4. The results after PSM were consistent with results from multivariate regression analysis. Patients with AF had higher mortality rate (aOR = 3.29, P < 0.01), longer mean LOS (adjusted coefficient: +1.56 days, P < 0.01), longer time to ERCP (adjusted coefficient: +0.5 days, P < 0.01) and higher mean hospitalization charges (adjusted coefficient: $17972, P < 0.01). There was no difference in likelihood of blood transfusion between the two groups (aOR = 1.15, P = 0.57).
| Study population with ERCP (n = 433245) | ||||||
| Outcomes | Without AF | With AF (multivariate regression) | P value | With AF (after propensity matching) | P value | |
| 1 | In-hospital mortality | 1.13% | 3.82% | |||
| OR | Ref | 3.46 | < 0.01 | 3.29 | < 0.01 | |
| AOR | Ref | 1.93 | < 0.01 | 1.74 | < 0.01 | |
| 2 | Mean time to ERCP (days) | 2.13 | 2.94 | 2.97 | ||
| Adjusted coefficient | Ref | +0.8 | < 0.01 | +0.50 | < 0.01 | |
| 3 | Mean length of stay (days) | 5.6 | 8.12 | |||
| Adjusted coefficient | Ref | +1.71 | < 0.01 | +1.56 | < 0.01 | |
| 4 | Mean total charge ($) | 79963 | 106017 | 100359 | ||
| Adjusted coefficient ($) | Ref | 21209 | < 0.01 | 17972 | < 0.01 | |
| 5 | Mean total cost ($) | 19214 | 25534 | |||
| Adjusted coefficient ($) | Ref | 4869 | < 0.01 | Not applicable | ||
| 6 | Shock | 3.26% | 10.27% | |||
| OR | Ref | 3.39 | < 0.01 | 3.24 | < 0.01 | |
| AOR | Ref | 2.17 | < 0.01 | 2.04 | < 0.01 | |
| 7 | Sepsis | 3.32% | 6.30% | |||
| OR | Ref | 1.95 | < 0.01 | 1.96 | < 0.01 | |
| AOR | Ref | 1.34 | < 0.01 | 1.30 | < 0.01 | |
| 8 | Intensive care unit admission | 2.30% | 7.27% | |||
| OR | Ref | 3.31 | < 0.01 | 3.08 | < 0.01 | |
| AOR | Ref | 2.41 | < 0.01 | 2.31 | < 0.01 | |
| 9 | Acute kidney injury | 12.7% | 29.47% | |||
| OR | Ref | 2.87 | < 0.01 | 2.76 | < 0.01 | |
| AOR | Ref | 1.51 | < 0.01 | 1.42 | < 0.01 | |
| 10 | Blood transfusion | 0.29% | 0.49% | |||
| OR | Ref | 1.69 | < 0.01 | 1.67 | < 0.05 | |
| AOR | Ref | 1.37 | 0.08 | 1.15 | 0.57 | |
| 11 | Home discharge | 78.2% | 48.34% | |||
| OR | Ref | 0.26 | < 0.01 | 0.27 | < 0.01 | |
| AOR | Ref | 0.59 | < 0.01 | 0.62 | < 0.01 | |
The outcomes of subgroup analysis based on timing of ERCP are summarized in Table 5. Compared to ERCP within the first 24 hours of admission, there was no significant difference in mortality in patients getting ERCP after 24 hours but within 72 hours (aOR = 0.712, 95%CI: 0.50-1.00, P = 0. 0576; aOR = 0.86, 95%CI: 0.59-1.25 P = 0.43) respectively. Delaying ERCP to more than 72 hours increased the odds of mortality significantly (aOR = 1.46, 95%CI: 1.23-1.74, P < 0.06). The total hospitalization charges and costs were significantly increased when ERCP was delayed by more than 48 hours from admission. Patients who underwent ERCP after 72 hours had an additional $69150 (P < 0.01) and $16933 (P < 0.01) added to their total hospitalization charges and cost respectively.
| Patients getting ERCP with AF (n = 49615) | ||||||||
| Outcomes | ERCP 0-24 hours | ERCP 24-48 hours | P value | ERCP 48-72 hours | P value | ERCP > 72 hours | P value | |
| 19900 (40.10) | 9005 (18.14) | 6180 (12.45) | 14530 (29.28) | |||||
| 1 | In-hospital mortality | 3.46% | 2.55% | 3.07% | 5.4% | |||
| OR | Ref | 0.72 | 0.06 | 0.88 | 0.50 | 1.58 | < 0.01 | |
| AOR | Ref | 0.71 | 0.05 | 0.86 | 0.43 | 1.47 | < 0.01 | |
| 2 | Mean length of stay | |||||||
| Adjusted coefficient(days) | Ref | 0.65 | < 0.01 | 1.74 | < 0.01 | 6.5 | < 0.01 | |
| 3 | Mean total charge ($) | |||||||
| Adjusted coefficient ($) | Ref | 1918 | 0.45 | 11861 | < 0.01 | 69150 | < 0.01 | |
| 4 | Mean total cost | |||||||
| Adjusted coefficient ($) | Ref | 197 | 0.68 | 2628 | < 0.01 | 16933 | < 0.01 | |
| 5 | Shock | 10.42% | 7.27% | 6.71% | 13.45% | |||
| OR | Ref | 0.67 | < 0.01 | 0.61 | < 0.01 | 1.33 | < 0.01 | |
| AOR | Ref | 0.65 | < 0.01 | 0.60 | < 0.01 | 1.30 | < 0.01 | |
| 6 | Sepsis | 6.80% | 5.49% | 5.17% | 6.60% | |||
| OR | Ref | 0.76 | 0.6 | 0.74 | < 0.05 | 0.96 | 0.74 | |
| AOR | Ref | 0.8 | 0.07 | 0.72 | < 0.05 | 0.99 | 0.90 | |
| 7 | Intensive care unit admission | 7.01% | 4.27% | 5.01% | 10.46% | |||
| OR | Ref | 0.59 | < 0.01 | 0.70 | < 0.01 | 1.54 | < 0.01 | |
| AOR | Ref | 0.57 | < 0.01 | 0.70 | < 0.01 | 1.46 | < 0.01 | |
| 8 | Acute kidney injury | 25.12% | 25.76% | 28.72% | 38.05% | |||
| OR | Ref | 1.03 | 0.6 | 1.20 | < 0.05 | 1.8 | < 0.01 | |
| AOR | Ref | 0.98 | 0.8 | 1.13 | 0.11 | 1.72 | < 0.01 | |
| 9 | Blood transfusion | 0.5% | 0.16% | 0.24% | 0.72% | |||
| OR | Ref | 0.30 | 0.05 | 0.43 | 0.18 | 1.30 | 0.39 | |
| AOR | Ref | 0.20 | < 0.01 | 0.44 | 0.19 | 1.04 | 0.89 | |
| 10 | Home discharge | 56.39% | 55.10% | 50.54% | 39.26% | |||
| OR | Ref | 0.94 | 0.36 | 0.79 | < 0.01 | 0.49 | < 0.01 | |
| AOR | Ref | 0.99 | 0.97 | 0.85 | < 0.05 | 0.48 | < 0.01 | |
Performing ERCP after 24 hours but within 72 hours decreased the risk of shock in patients with AF (aOR = 0.65, 95%CI: 0.53-0.81, P < 0.01 and aOR = 0.60, 95%CI: 0.47-0.78, P < 0.01) respectively. ERCP after 72 hours increased the likelihood of shock (aOR = 1.30, 95%CI: 1.12-1.52, P < 0.01). Similar trend was observed for ICU admission as well. Patients with ERCP 24-48 hours of admission and 48-72 hours of admission had lower odds of ICU admission (aOR = 0.57, 95%CI: 0.43-0.75, P < 0.01 and aOR = 0.70, 95%CI: 0.52-0.94, P < 0.01) respectively. Delaying ERCP to more than 72 hours from admission resulted in increased odds of ICU admission (aOR = 1.46, 95%CI: 1.23-1.74, P < 0.06). Similarly, performing ERCP 48-72 hours of admission resulted in decreased odds of sepsis (aOR = 0.72, 95%CI: 0.54-0.97, P < 0.05). Patients with ERCP after 72 hours also had increased likelihood of AKI (aOR = 1.72, 95%CI: 1.53-1.92, P < 0.01). Patients with ERCP performed between 48-72 hours and after 72 hours were less likely to be discharged home (aOR = 0.85, 95%CI: 0.74-0.98, P < 0.01 and aOR = 0.48, 95%CI: 0.43-0.43, P < 0.01) respectively (Table 5).
To our knowledge, this is the first nationwide study examining the impact of AF in hospitalized patients undergoing ERCP. Our study highlights that AF predisposes one to significantly increased in-hospital mortality rates, increased LOS, longer time to ERCP, and higher total hospitalization cost and charges.
We hypothesize that risk of increased in-hospital mortality is attributed to a combination of patients’ clinical comorbidities and medication use–namely anticoagulants. Pilgrim et.al observed that in patients with coronary artery disease undergoing revascularization with drug eluting stents, AF increased the risk of all-cause mortality (hazard ratio = 1.67, P < 0.003)[11]. Another study noticed higher in-hospital mortality in patients with stroke and AF (12.1% vs 6.5%)[12]. These studies highlight the negative impact of AF on in-hospital outcomes of patients. This is consistent with the findings in our study and indicates that invasive procedures are likely riskier in patients with AF[13]. Additionally, in our study, almost 30% of patients with AF undergoing ERCP were found to have AKI, and patients with AF had 50% higher odds of developing AKI. We postulate that these additional comorbidities probably account for the increase in LOS and resource utilization in patients with AF.
With use of anticoagulants for stroke prevention in AF, timing of ERCP can get challenging[14]. A key finding of our study is that delayed ERCP (> 72 hours) had increased odds of mortality compared to ERCP < 24 hours of admission. Similar findings have been previously reported by Mulki et al[15] in which they compared outcomes of early vs delayed ERCP in patients with acute cholangitis. In contrast, our study demonstrated that in patients with AF, performing ERCP within 24-48 hours resulted in shorter LOS compared to ERCP within 24 hours. Likewise, performing ERCP after 24 hours but within 72 hours resulted in decreased incidence of shock, sepsis and ICU admission[16]. Delaying ERCP until after 24 hours of admission leads to improved resuscitation efforts with intravenous fluids and antibiotics in patients needing ERCP[17], and this is likely the reason for our observation.
Furthermore, ERCP after 72 hours of admission had consistently poor outcomes when compared to ERCP within 24 hours of admission. These patients had higher in-hospital mortality, longer LOS, increased shock, increased AKI, increased ICU admission and reduced likelihood of home discharge. This is uniform with most of the studies and guideline recommendation of ERCP within 72 hours in patients without cholangitis[17-20]. Our study is constrained by its retrospective nature and utilization of billing database. Nevertheless, the revelations in our study warrant prospective studies to determine the optimum timing of ERCP in patients with AF, to solidify the gap of uncertainty among physicians.
Although our results are robust, several limitations within the study must be considered. First, this is a database study that heavily relies on accurate coding of all inpatient and procedure codes. We have to accept that there may be instances of underreporting or selective reporting. Second, ERCP is an invasive procedure and certain amount of selection bias naturally exists. The NIS does not contain important clinical information such as laboratory and imaging data. These are often used to determine the necessity and urgency of procedures and to predict outcomes[21,22]. Despite such limitations, our study has numerous strengths. The largest strength is the fact that we included a large sample size (> 300000 patients) providing an accurate representation of the entire United States population. We used multivariate regression analysis and PSM to account for potential confounders. PSM helps to design observational studies to mimic randomized experiments to produce unbiased treatment effects[23]. In the absence of any relevant study looking at the effect of AF on ERCP, our study was able to analyze various outcomes not reported in the literature yet. Furthermore, we also stratified patients based on the timing of ERCP giving an additional perspective to the analysis of outcomes in patients with or without AF. Our large sample size from the NIS database could well be a generalized representation of the United States population
Our study demonstrates that AF is associated with significantly worse hospital outcomes in patients undergoing ERCP, including increased in-hospital mortality, longer LOS, delayed ERCP timing, and higher healthcare costs. These findings emphasize the complexity of managing patients with AF in the setting of invasive procedures, likely influenced by comorbidities, anticoagulation use, and procedural risks.
Clinically, these results highlight the importance of optimizing perioperative management in patients with AF undergoing ERCP. Careful risk stratification, anticoagulation management, and timely intervention are crucial to improving outcomes. Our study suggests that performing ERCP between 24-72 hours after admission may reduce the risk of sepsis, shock, ICU admission, and mortality, reinforcing the need for individualized procedural timing in this high-risk population.
Despite the robust nature of our analysis, our study is limited by its retrospective design and reliance on administrative coding. Future prospective studies are necessary to validate these findings, explore the mechanisms underlying poor outcomes in AF patients undergoing ERCP, and determine the optimal timing of intervention. Establishing evidence-based guidelines tailored to this subgroup of patients will be essential in improving patient outcomes and guiding clinical decision-making.
| 1. | McCune WS, Shorb PE, Moscovitz H. Endoscopic cannulation of the ampulla of vater: a preliminary report. Ann Surg. 1968;167:752-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 410] [Cited by in RCA: 383] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 2. | Ahmed M, Kanotra R, Savani GT, Kotadiya F, Patel N, Tareen S, Fasullo MJ, Kesavan M, Kahn A, Nalluri N, Khan HM, Pau D, Abergel J, Deeb L, Andrawes S, Das A. Utilization trends in inpatient endoscopic retrograde cholangiopancreatography (ERCP): A cross-sectional US experience. Endosc Int Open. 2017;5:E261-E271. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 3. | Adler DG, Baron TH, Davila RE, Egan J, Hirota WK, Leighton JA, Qureshi W, Rajan E, Zuckerman MJ, Fanelli R, Wheeler-Harbaugh J, Faigel DO; Standards of Practice Committee of American Society for Gastrointestinal Endoscopy. ASGE guideline: the role of ERCP in diseases of the biliary tract and the pancreas. Gastrointest Endosc. 2005;62:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 291] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 4. | Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285:2370-2375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4468] [Cited by in RCA: 4676] [Article Influence: 187.0] [Reference Citation Analysis (0)] |
| 5. | Gerson LB, Gage BF, Owens DK, Triadafilopoulos G. Effect and outcomes of the ASGE guidelines on the periendoscopic management of patients who take anticoagulants. Am J Gastroenterol. 2000;95:1717-1724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Fisher L, Fisher A, Thomson A. Cardiopulmonary complications of ERCP in older patients. Gastrointest Endosc. 2006;63:948-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 74] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 7. | Odutayo A, Wong CX, Hsiao AJ, Hopewell S, Altman DG, Emdin CA. Atrial fibrillation and risks of cardiovascular disease, renal disease, and death: systematic review and meta-analysis. BMJ. 2016;354:i4482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 596] [Cited by in RCA: 601] [Article Influence: 60.1] [Reference Citation Analysis (0)] |
| 8. | Mardini MT, Raś ZW. Discovering Primary Medical Procedures and their Associations with Other Procedures in HCUP Data. Inf Syst Front. 2022;24:133-147. [DOI] [Full Text] |
| 9. | Chen CY, Liao KM. The impact of atrial fibrillation in patients with COPD during hospitalization. Int J Chron Obstruct Pulmon Dis. 2018;13:2105-2112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Olsson LG, Swedberg K, Ducharme A, Granger CB, Michelson EL, McMurray JJ, Puu M, Yusuf S, Pfeffer MA; CHARM Investigators. Atrial fibrillation and risk of clinical events in chronic heart failure with and without left ventricular systolic dysfunction: results from the Candesartan in Heart failure-Assessment of Reduction in Mortality and morbidity (CHARM) program. J Am Coll Cardiol. 2006;47:1997-2004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 397] [Cited by in RCA: 445] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 11. | Pilgrim T, Kalesan B, Zanchin T, Pulver C, Jung S, Mattle H, Carrel T, Moschovitis A, Stortecky S, Wenaweser P, Stefanini GG, Räber L, Meier B, Jüni P, Windecker S. Impact of atrial fibrillation on clinical outcomes among patients with coronary artery disease undergoing revascularisation with drug-eluting stents. EuroIntervention. 2013;8:1061-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Keller K, Geyer M, Münzel T, Ostad MA, Gori T. Impact of atrial fibrillation on in-hospital mortality of ischemic stroke patients and identification of promoting factors of atrial thrombi - Results from the German nationwide inpatient sample and a single-center retrospective cohort. Medicine (Baltimore). 2019;98:e14086. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Novo-Veleiro I, Pose-Reino A, Gullón A, Díez-Manglano J, Cepeda JM, Formiga F, Camafort M, Mostaza JM, Suárez C. Acute kidney injury is linked to higher mortality in elderly hospitalized patients with non-valvular atrial fibrillation. Aging Clin Exp Res. 2019;31:455-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | ASGE Standards of Practice Committee; Acosta RD, Abraham NS, Chandrasekhara V, Chathadi KV, Early DS, Eloubeidi MA, Evans JA, Faulx AL, Fisher DA, Fonkalsrud L, Hwang JH, Khashab MA, Lightdale JR, Muthusamy VR, Pasha SF, Saltzman JR, Shaukat A, Shergill AK, Wang A, Cash BD, DeWitt JM. The management of antithrombotic agents for patients undergoing GI endoscopy. Gastrointest Endosc. 2016;83:3-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 417] [Cited by in RCA: 484] [Article Influence: 48.4] [Reference Citation Analysis (2)] |
| 15. | Mulki R, Shah R, Qayed ES. 167 Outcomes of Early Versus Late Ercp in Hospitalized Patients with Acute Cholangitis: A Nationwide Analysis. Gastrointest Endosc. 2018;87:AB58-AB59. [DOI] [Full Text] |
| 16. | Khashab MA, Tariq A, Tariq U, Kim K, Ponor L, Lennon AM, Canto MI, Gurakar A, Yu Q, Dunbar K, Hutfless S, Kalloo AN, Singh VK. Delayed and unsuccessful endoscopic retrograde cholangiopancreatography are associated with worse outcomes in patients with acute cholangitis. Clin Gastroenterol Hepatol. 2012;10:1157-1161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 95] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 17. | Tenner S, Baillie J, DeWitt J, Vege SS; American College of Gastroenterology. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108:1400-15; 1416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1232] [Cited by in RCA: 1428] [Article Influence: 109.8] [Reference Citation Analysis (3)] |
| 18. | Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M; Early Goal-Directed Therapy Collaborative Group. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368-1377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7787] [Cited by in RCA: 6472] [Article Influence: 258.9] [Reference Citation Analysis (0)] |
| 19. | Fogel EL, Sherman S. ERCP for gallstone pancreatitis. N Engl J Med. 2014;370:150-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Tse F, Yuan Y. Early routine endoscopic retrograde cholangiopancreatography strategy versus early conservative management strategy in acute gallstone pancreatitis. Cochrane Database of Systematic Reviews. 2012;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 21. | Aylin P, Lees T, Baker S, Prytherch D, Ashley S. Descriptive study comparing routine hospital administrative data with the Vascular Society of Great Britain and Ireland's National Vascular Database. Eur J Vasc Endovasc Surg. 2007;33:461-465; discussion 466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 65] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Aylin P, Bottle A, Majeed A. Use of administrative data or clinical databases as predictors of risk of death in hospital: comparison of models. BMJ. 2007;334:1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 228] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 23. | Pattanayak CW, Rubin DB, Zell ER. Propensity Score Methods for Creating Covariate Balance in Observational Studies. Revista Española de Cardiología (English Edition). 2011;64:897-903. [DOI] [Full Text] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/