Published online Dec 20, 2025. doi: 10.5662/wjm.v15.i4.101033
Revised: February 17, 2025
Accepted: February 27, 2025
Published online: December 20, 2025
Processing time: 335 Days and 23.2 Hours
Dry eye disease (DED) represents a multifactorial condition characterized by ocular discomfort and visual disturbances. The management of DED relies heavily on accurate diagnosis to tailor effective treatments. Diagnostic approaches encompass both subjective and objective assessments.
To review the diagnostic methods used in the process of dry eye disease management.
A comprehensive review of diagnostic approaches for dry eye was performed using scientific databases. Studies published within the last four years were considered. Studies were excluded if a full text was absent or the article was not written in English. Articles were assessed for relevancy, and a total of 107 studies were selected. The selection method used a systematic methodology, which guaranteed an exhaustive assessment of the diagnostic techniques reported in current literature. The study adheres to principles for systematic reviews ensuring dependability and accuracy. The studies were assessed for emphasize on both novel traditional and diagnostic methods for dry eye disease management.
Key objective tests include tear break-up time, which evaluates tear film stability; fluorescein and lissamine green staining, which assess ocular surface damage and inflammation; tear osmolarity measurement, indicative of tear film quality; and tear volume assessment via Schirmer's test, which evaluates tear production. Advanced imaging techniques such as optical coherence tomography and meibography offer detailed anatomical insights into the ocular surface and meibomian glands, aiding in the diagnosis of underlying structural abnormalities. Moreover, emerging technologies such as matrix metalloproteinase-9 testing and inflammatory biomarkers provide additional diagnostic precision, particularly in identifying inflammatory components of DED.
Integrating a combination of subjective and objective diagnostic tools allows clinicians to comprehensively assess the condition, tailor treatment plans, and monitor therapeutic efficacy. Continued advancements in diagnostic technologies promise to enhance our understanding and management of this prevalent ocular condition.
Core Tip: Keratoconjunctivitis sicca, or dry eye disease (DED), is a common ocular illness with different incidence rates worldwide. The complicated etiology of DED involves tear film instability and can cause pain, decreased vision, and ocular surface damage. Evaporative and aqueous-deficient dry eye have different causes. Differentiating between these types is often required for appropriate diagnosis and effective therapy. A detailed diagnosis is needed as Sjögren's syndrome, an autoimmune condition, is connected to a type of DED. Recent advances aim to standardize diagnosis and improve therapy by addressing the causes of DED.
- Citation: Musa M, Suleman A, Okechukwu C, Bale BI, Gagliano C, D’Esposito F, Zeppieri M. Diagnostic methods for managing dry eyes. World J Methodol 2025; 15(4): 101033
- URL: https://www.wjgnet.com/2222-0682/full/v15/i4/101033.htm
- DOI: https://dx.doi.org/10.5662/wjm.v15.i4.101033
Dry eye disease (DED), also known as dry eye syndrome (DES) or keratoconjunctivitis sicca (KCS), is a common ocular condition affecting millions globally, with prevalence rates ranging from 5% to 50%[1-3]. This multifactorial disease of the ocular surface causes discomfort and visual disturbances[4] and is more likely to be encountered in primary care settings rather than secondary or tertiary centers[5]. The tear film, which consists of mucin, aqueous, and lipid layers[6], can become unstable due to disruptions in the normal anatomy or physiology of these layers. This instability may result from qualitative or quantitative abnormalities in the tear film’s aqueous, lipid, and mucin layers.
The 2017 DEWS II report redefined DED as “a multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film, accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play etiological roles”[7]. Ongoing Delphi analyses aim to enhance understanding of DED and establish a standardized framework for its diagnosis and management[8].
DED can result from reduced tear secretion by the lacrimal glands, increased tear evaporation, or the production of poor-quality tears. This tear instability can lead to ocular surface inflammation, damage, and abnormal nociception[9]. Symptoms include burning, foreign body sensations, blurred vision, and redness, which can cause discomfort and reduce work efficiency and quality of life[10]. Complications may include conjunctival scarring or corneal issues that can impair vision[11].
The primary roles of the aqueous component of the tear film are to lubricate the surface of the eye, remove unwanted objects or contaminants, and provide nourishment to the cornea, which lacks blood vessels (such as oxygen, inorganic salts, proteins, and glucose)[12]. Consequently, when these glands are not functioning properly, there is a decrease in the production of necessary fluids and other important substances required to maintain and protect the surface of the eye. This leads to dry eye and possibly severe damage to the eye's surface[13]. Dry eye is a prevalent ocular condition, with an estimated prevalence of 14% to 33% in adults, which tends to increase with age[14]. It is often accompanied by other ocular conditions, such as impaired vision[15]. The variation in the occurrence and frequency of dry eye in different regions of the world has been attributed, in part, to interracial variances across populations[16]. The preservation of clear vision and ocular comfort relies on the integrity and stability of the air-tear film interface, which serves as the principal refractive surface of the eye[17]. The more severe symptoms of DED are linked to reduced job productivity and activity levels, both when comparing different individuals (cross-sectionally) and over time within the same person (intra-individually)[18].
DED is a diverse disorder with multiple poorly understood subcategories, broadly classified into aqueous-deficient and evaporative DED. Five distinct subgroups have been identified, each exhibiting substantial differences in demo
Primary Sjögren's Syndrome (PSS) is a persistent condition characterized by symptoms of dryness in the mouth and eyes, as well as discomfort, exhaustion, anxiety, and despair. The Newcastle Sjögren's Stratification Tool may classify PSS patients based on the severity pattern of five significant symptoms[22]. Research revealed a higher prevalence of primary Sjögren syndrome in women compared to males. This condition is characterized by increased dryness, positive au
KCS, sometimes referred to as NSSDE, is a prevalent disorder marked by persistent dryness and irritation of the eyes. NSSDE, in contrast to Sjögren's syndrome, has no connection to an autoimmune illness that impacts tear-producing glands[29]. Alternatively, it can be attributed to many causes, such as environmental influences, hormone fluctuations, certain drugs, and natural aging[30]. Common symptoms of this condition include enduring dryness, a sensation of grittiness, and a burning feeling in the eyes. Additionally, individuals may have impaired vision and heightened sensitivity to light. Possible treatment modalities encompass the administration of artificial tears, prescription drugs, and modifications in lifestyle, such as using humidifiers and evading arid surroundings[31]. Sjögren's syndrome is associated with digestive[32], dental[33-35], cardiovascular[36-39], and renal health consequences[40,41]. DED can also arise as a result of other ocular/systemic disorders such as thyroid eye disease[42] and fibromyalgia[43]. Views on the management of dry eye can diverge significantly[44], even among a specific subset of people. Extensive research conducted in India found that 39.62% of dry eye patients had evaporative dry eye, whereas 34.7% had aqueous deficient dry eye[45].
The successful management of DED depends on the precise diagnosis of the condition to determine the root cause and use the most suitable treatment method[46,47]. This study examines the existing diagnostic procedures for DED, including their advantages and disadvantages. It also discusses new approaches that are being developed and have the potential to enhance the diagnosis and treatment of DED.
The authors searched the PubMed database using “Diagnostic methods in managing dry eyes” as keywords, as shown in Table 1.
| Search component | Keywords used |
| Diagnostic | "diagnosis" [MeSH Terms] OR "diagnosis" [All Fields] OR "diagnostic" [All Fields] OR "diagnostical" [All Fields] OR "diagnostically" [All Fields] OR "diagnostics" [All Fields] |
| Method | "methods" [All Fields] OR "methods" [MeSH Terms] OR "methods" [All Fields] OR "method" [All Fields] OR "methods" [MeSH Subheading] AND "manage" [All Fields] |
| Manage | "manage" [All Fields] OR "managed" [All Fields] OR "managements" [All Fields] OR "managements" [All Fields] OR "manager" [All Fields] OR "managers" [All Fields] OR "managers" [All Fields] OR "manages" [All Fields] OR "managing" [All Fields] OR "management" [All Fields] OR "organization and administration" [MeSH Terms] OR ("organization" [All Fields] AND "administration" [All Fields]) OR "organization and administration" [All Fields] OR "management" [All Fields] OR "disease management" [MeSH Terms] OR ("disease" [All Fields] AND "management" [All Fields]) OR "disease management" [All Fields]) |
| Dry eye syndromes | ("dry eye syndromes" [MeSH Terms] OR ("dry" [All Fields] AND "eye" [All Fields] AND "syndromes" [All Fields]) OR "dry eye syndromes" [All Fields] OR ("dry" [All Fields] AND "eye" [All Fields]) OR "dry eye" [All Fields])) AND ((ffrft[Filter]) AND (2020: 2024[pdat])). |
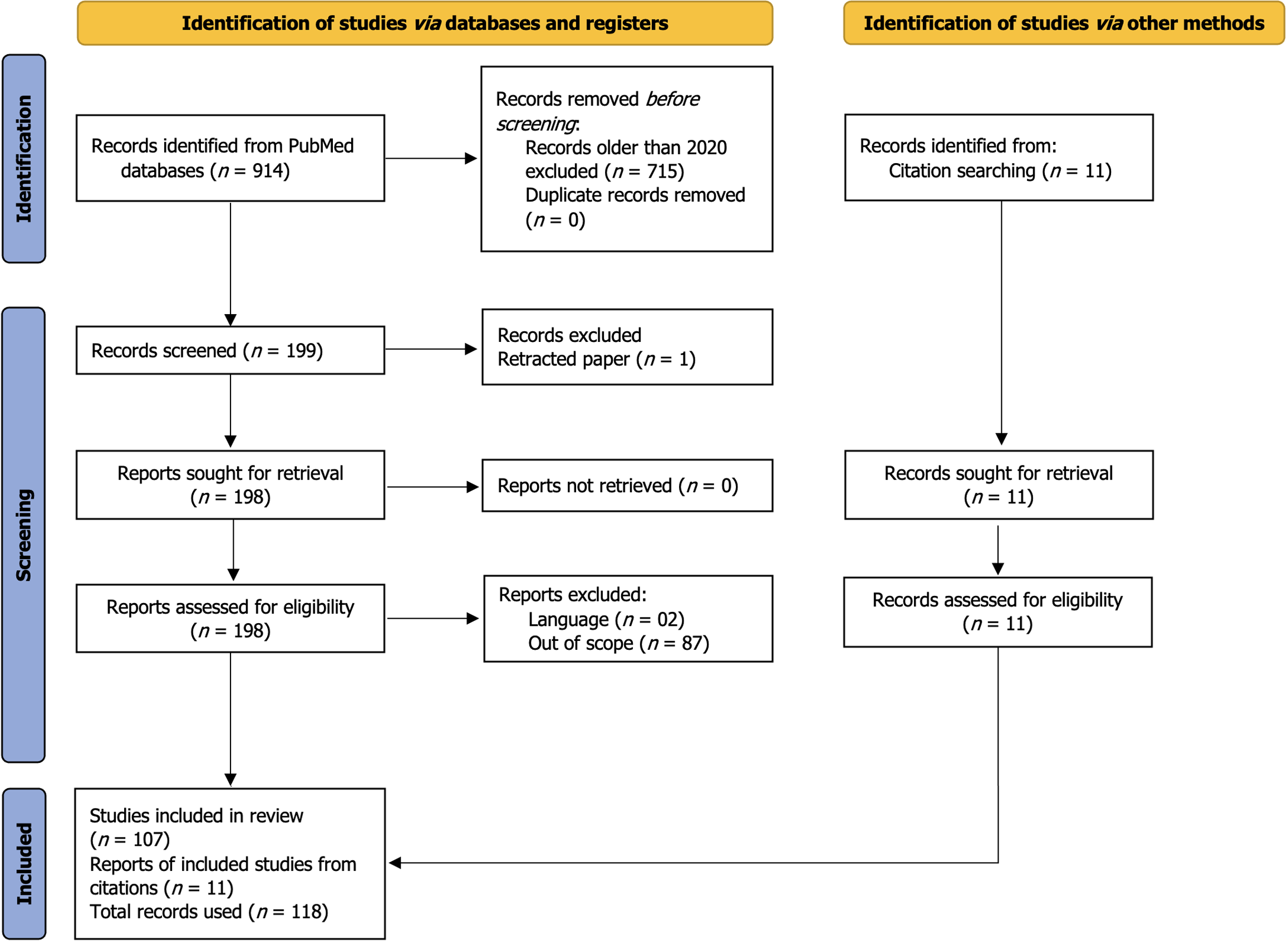
Records that were not in the English language, lacked full text, and/or not relevant were further excluded as shown in the PRISMA[47] flowchart below in Figure 1. The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist (Figure 1).
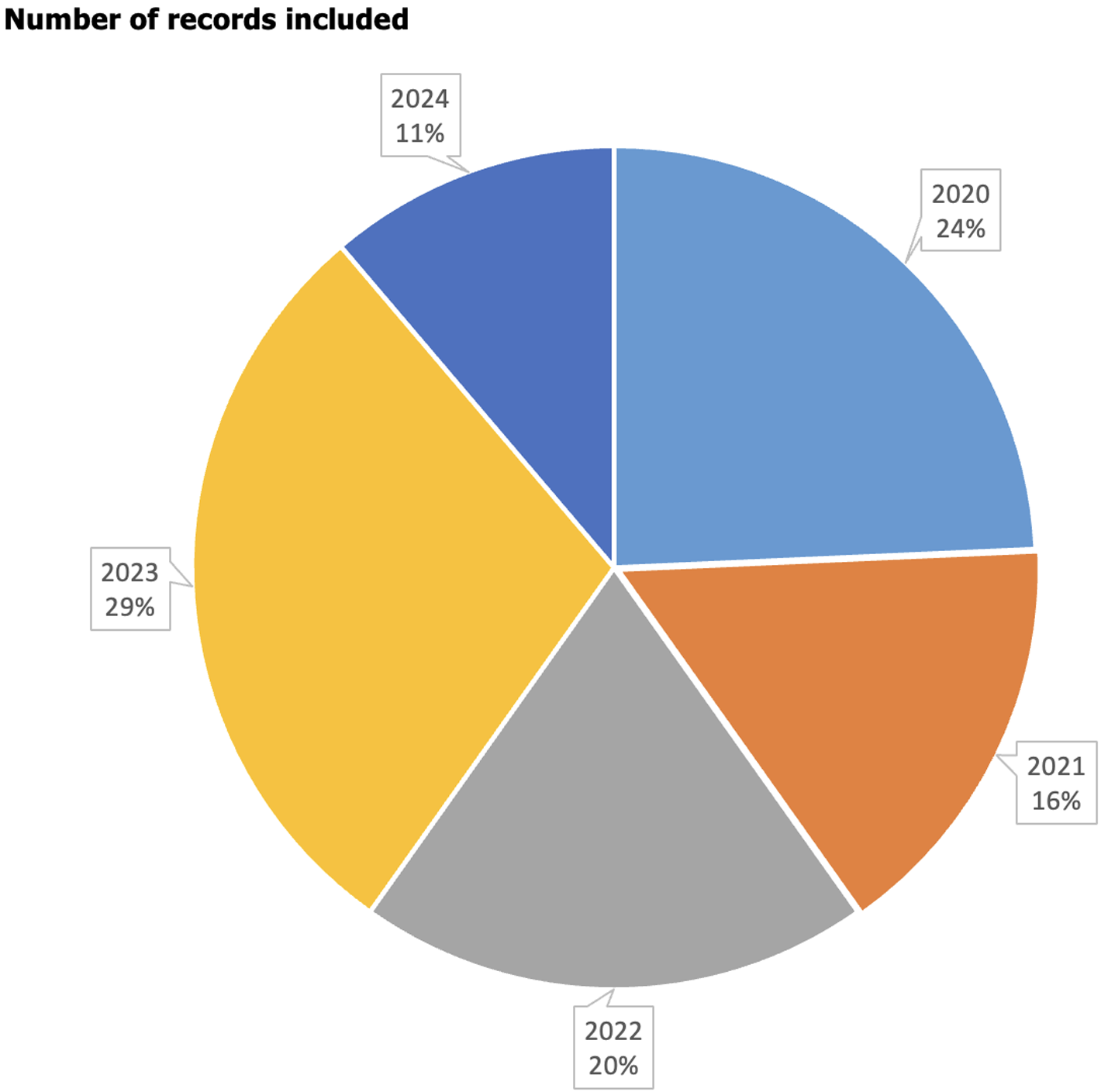
The search string initially returned 914 records. Articles published more than 4 years ago and those not in English were excluded, leaving 199 records. Additionally, articles that were not available as free full text and lacked abstracts were excluded. This filtering process resulted in 199 articles, which were then retrieved by the authors. One publication was excluded because it had been retracted, another two on the basis of language, and 89 publications were not used because they were out of scope. A total of 107 publications were included in this review. A spread of the number of papers included as segregated by year of publication is shown in Figure 2[48-53].
Some of the diagnostic methods reviewed are shown in Table 2. Accurate diagnosis and management of dry eye are essential for improving patient quality of life[54]. While objective measurements are crucial for diagnosing and managing DED, subjective evaluations provide valuable insights into the patient's experience[55]. Subjective evaluations, which include patient-reported symptoms and standardized questionnaires, are critical components in the diagnostic process[56].
| Method | Ref. | Sample size | Diagnostic rubric |
| American-European consensus group classification criteria | Lee et al[48] | 187 serum samples of age matched females | Authors suggest peptides treated with malondialdehyde increase the formation of autoantibodies, suggesting that they have diagnostic utility for primary Sjögren's Syndrome |
| Existing data analyses | Acar-Denizli et al[49] | 12084 patients with ESSDAI scores | Combination patterns of two antibodies-anti-Ro/SSA and anti La/SSB was used to define Sjogrens syndrome |
| Machine learning algorithm using routine healthcare data | Dros et al[50] | 1411 primary Sjögren's Syndrome patients and 929179 non-primary Sjögren's Syndrome patients | The task entailed employing logistic regression and random forest models for the purpose of categorizing patients. The models used characteristics such as age, gender, medical conditions, symptoms, medication prescriptions, and visits to general practitioners |
| Diagnostic criteria by Japanese research committee on severe cutaneous adverse reaction | Sotozono et al[51] | 94 Stevens-Johnson syndrome and toxic epidermal necrolysis patients with severe ocular complications | The diagnostic criteria for ocular involvement in instances of Stevens-Johnson syndrome and toxic epidermal necrolysis include particular ocular abnormalities, such as the creation of pseudo-membranes and defects in the epithelium. These symptoms are regarded to be high-risk indicators for ocular complications |
| DryEyeRhythm mobile app | Inomata et al[52] | 4454 individuals | The diagnostic rubric involved assessing subjective symptoms reported by the participants via the DryEyeRhythm app. The DryEyeRhythm is a mobile application that facilitates real-time monitoring of DED symptoms, allowing for remote symptom tracking and prompt intervention |
| Ultrasonographic techniques (grayscale and color Doppler sonography) and contrast-enhanced ultrasonography | Xu et al[53] | 161 patients with primary Sjögren's Syndrome and 66 non primary Sjögren's Syndrome patients | The diagnostic approach entailed assessing the ultrasonographic characteristics of the parotid and submandibular glands. Ultrasonographic methods, encompasses grayscale and Doppler imaging, to evaluate lacrimal gland structure and vascularity in patients with DED |
The diagnosis of DED is based mostly on the symptoms stated by the patient, as this gives direct insight into their experience. These symptoms include various discomforts, such as dryness, burning, stinging, grittiness, and vision problems[57]. Patients frequently complain of a chronic feeling of dryness or not enough tears, which can be made worse by external conditions like wind or low humidity[58]. Patients may also complain of these symptoms after prolonged screen time, which results in digital strain[59].
Clinical visits usually entail comprehensive patient discussions to assess these symptoms. Inquiries concerning symptoms' onset, length, frequency, and severity are among the detailed qualitative data collected. These data are essential for modifying treatment regimens to meet each patient's needs and tracking the long-term efficacy of treatments[60]. A thorough medical history is needed, as studies suggest a relationship between the white blood cell population and the symptoms experienced in DED patients[61]. Barrio-Cortes et al[62] concluded that other comorbidities positively correlated to the likelihood of patients presenting for treatment.
The ocular surface disease index (OSDI) is a questionnaire designed to measure the severity of dry eye symptoms and their impact on daily activities. It covers three main areas: Environmental triggers, visual function, and ocular symptoms[63]. The questionnaire consists of twelve questions, each scored from 0 to 4, with higher scores indicating more severe symptoms[64]. The total OSDI score ranges from 0 to 100 and helps track symptom progression and treatment effectiveness[65]. Table 3 below provides more comprehensive information on the OSDI questionnaire[63-65].
| Category | Questions | Scoring (0-4) |
| Ocular symptoms | Dryness, grittiness, discomfort | 0 (None) to 4 (Severe) |
| Visual function | Blurred vision, difficulty reading | 0 (None) to 4 (Severe) |
| Environmental factors | Wind sensitivity, air conditioning | 0 (None) to 4 (Severe) |
The standard patient evaluation of eye dryness (SPEED) questionnaire, developed by Korb and Blackie, is a tool used to quickly assess and track the symptoms of DED. It consists of eight questions evaluating the frequency and severity of symptoms such as dryness, grittiness, soreness, irritation, burning, watering, and eye fatigue[66]. Patients rate their symptoms on a scale from 0 to 4, with a total score ranging from 0 to 28. This standardized method helps healthcare providers monitor symptom progression and identify triggers, making it easier to diagnose and manage DED[67]. Its simplicity and efficiency make it useful in both clinical settings and research studies. Table 4 below provides more comprehensive information on the SPEED questionnaire[66,67].
| Question type | Symptoms evaluated | Scoring (0-4) |
| Frequency | Burning, grittiness, fatigue | 0 (Never) to 4 (Constant) |
| Severity | Discomfort level | 0 (None) to 4 (Severe) |
The McMonnies questionnaire is a diagnostic tool used to evaluate the severity and frequency of dry eye symptoms and identify risk factors[68]. It asks about environmental triggers and systemic conditions to help clinicians understand the underlying causes. Higher total scores indicate a greater likelihood of DED, aiding in diagnosis and treatment planning, which may include artificial tears, lifestyle changes, or other therapies to improve the patient's quality of life[69]. Table 5 below provides more comprehensive information on the McMonnies questionnaire[68,69].
| Question type | Symptoms evaluated | Scoring (0-4) |
| Risk factors | Age, sex, contact lens use, medications, systemic diseases (e.g., Sjögren’s) | Yes/No responses (Binary) |
| Symptoms frequency | Dryness, grittiness, burning, excessive tearing | 0 (Never) to 3 (Frequent) |
| Symptom severity | Eye discomfort, irritation, redness | 0 (None) to 3 (Severe) |
| Triggers | Environmental factors (wind, air condition, smoke), screen time impact | Yes/No responses (Binary) |
Subjective assessments are essential in diagnosing DED, although they require supplementation with objective metrics for precision. The OSDI and SPEED questionnaires offer symptomatic insights but should not serve as the exclusive diagnostic criterion. The OSDI and SPEED questionnaires are mostly diagnostic, evaluating symptom load. The McMonnies questionnaire is primarily designed for screening, but the DryEyeRhythm app facilitates the longitudinal tracking of symptoms. Clinicians must choose instruments according to the specific therapeutic purpose.
Proteomic indicators and exosomal biomarkers are recent means of objectively assessing tear film stability in dry eye treatment[70,71]. Although there are many high-end means of objectively assessing individuals with dry eyes, with each method having a specific level of specificity and sensitivity, the gold standard still remains the tear film ocular surface algorithm[72].
In the future, a workup on the particular microbes present in the anterior segment will help control inflammation and ocular surface complications from DED[73].
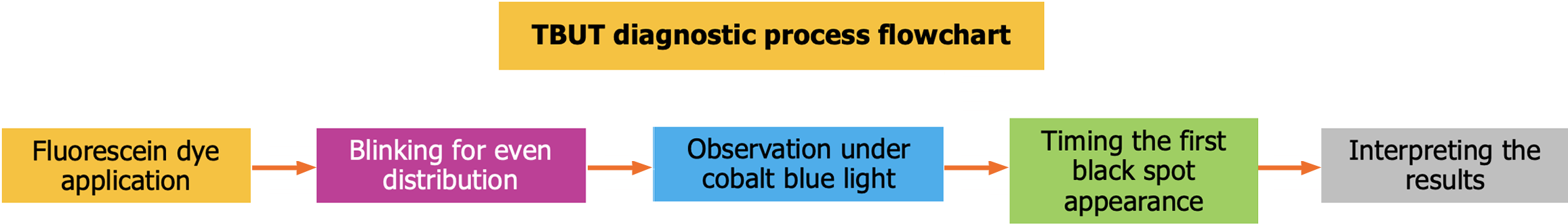
Tear break-up time (TBUT) assesses tear film stability by the application of fluorescein dye. A TBUT of less than 10 seconds indicates tear instability. The flowchart image below in Figure 3 illustrates the steps in measuring TBUT. Following a case-control study carried out by Pu et al[74], it was observed that assessing first non-invasive TBUT, average non-invasive TBUT, tear meniscus height, and meibomian gland assessment showed a correlation between the onset of obstructive sleep apnea and the onset of DED[74-76]. Ocular surface temperature reduces following phacoemulsification cataract surgery, partly due to instability of the tear film[77], potentially disrupting the tear film (Figure 3).
Ocular staining scores evaluate corneal damage utilizing fluorescein or lissamine green dyes, with grading determined by staining intensity. Ocular staining score has been found to have a higher degree of sensitivity and specificity when compared to other dry eye diagnostic parameters[78]. Sahlu et al[79] conducted a cross-sectional study and observed a significant drop in TBUT and corneal staining in glaucoma patients, especially those on multiple drops[79,80].
Using parameters like the Schirmer test score, Corneal staining score, and worse composite DED sign score as criteria for gender prevalence of complaints and in premenopausal and post-menopausal women, the result was in favor of premenopausal women compared to those that have reached menopause[81]. Software assessment of corneal staining, compared to individual objective assessment, shows more accuracy and is deemed fit to be used for monitoring purposes[82-84].
It was found in the DREAM study that there is no significant relationship between tear osmolarity in a patient with dry eyes and DED symptoms, so changes in tear film osmolarity cannot be regarded as a causal factor for the development or worsening of dry eyes[85,86]. A controlled environment chamber technique can be used in the assessment of dry eye complaints and symptoms, as it allows researchers to manipulate the testing location while observing tear parameters[87]. The OcuSense TearLab osmometer is a digital device that measures tear osmolarity from a very small sample. García et al[88]showed that this osmometer had good reproducibility indices and as such, can be very handy in DED diagnosis.
The Schirmer’s test evaluates tear volume using a wettable strip inserted into the lower fornix. Tortuous meibomian gland and a high composite score for features of the meibomian gland was associated with longer TBUT and longer length on the Schirmer strip[89]. The Schirmer test is the most common test for tear quantity and it is a tool for verifying/standardizing other tear volume testing techniques[90,91].
In cases of aqueous-deficient DED, Schirmer's test and tear osmolarity assessments are the most pertinent. In evaporative DED, meibography and lipid layer thickness assessment are essential. The prognostic evaluation is enhanced by OCT-based monitoring of tear meniscus height and in vivo confocal microscopy for assessing nerve injury.
In vivo, confocal microscopy is a great tool for assessing neurosensory changes that occur in eyes with DED[92]. These imaging techniques in DED management are more objective and provide real-time documentation of parameters both now and in the near future[93]. There is an emergence in the use of protein microarray technology in the management of ocular surface disease caused or worsened by diabetes[94]. Tracking field failure has been found to increase the severity of dry eyes, suggesting that the reduced lubrication occasioned by DED affected eye movement[95,96]. The use of app-based software in diagnosing dry eyes is, however, gaining more ground and has been found to offer as much information as the traditional diagnostic technique[97].
Epithelial thickness profile range and Epithelial irregularity factor obtained by using ultra-high OCT have been found to correlate with patient's complaints and symptoms, viz a viz, there is a direct relationship between symptoms and these two parameters[98]. There seems to be a significant difference in corneal morphology parameters when using Pentacam and the anterior segment OCT as measuring tools[99]. The most reliable method of assessing the tear meniscus height is the use of OCT, followed by the regular slit lamp examination. However, comparing tear meniscus height with lid margin thickness or number of lashes is not a reliable method as shown by research work[100].
The DryEyeRhythm app, an innovative tool developed by Juntendo University, serves as a sophisticated mechanism for the monitoring and management of dry eye symptoms. Utilizing the smartphone's camera for conducting a blink assessment, coupled with a concise questionnaire, users are afforded the capability to determine their dry eye score within a brief duration of approximately five minutes[52]. The application further enables users to systematically track daily lifestyle variables, including stress levels and sleep patterns, thereby elucidating the relationship between these factors and dry eye symptoms. The anonymized data collected via the app significantly contributes to dry eye research, facilitating advancements in early detection and treatment strategies[84].
Color Doppler imaging (CDI) has emerged as a valuable diagnostic tool in the assessment of ocular blood flow abnormalities associated with DED. By employing this non-invasive ultrasound technique, clinicians can visualize and quantify blood flow in the ophthalmic vessels, including the central retinal artery and posterior ciliary arteries[53]. CDI facilitates the detection of hemodynamic changes that may contribute to the pathophysiology of dry eye, such as reduced blood flow velocity and altered resistivity indices[53]. This advanced imaging modality offers a promising approach for early diagnosis and monitoring of DED, potentially leading to more effective therapeutic interventions and improved patient outcomes
Meibography employs infrared imaging to visualize the morphology of meibomian glands. Atrophy and gland loss correspond with the severity of DED. With this technique, the lower lid is everted and imaged. The image generated is then assessed and graded to account for any dilation, or atrophy blockage in the meibomian glands. This technique offers detailed anatomical insights into meibomian glands, aiding in diagnosing underlying structural abnormalities[101]. By capturing detailed images, meibography helps identify blockages or atrophy in these glands, which are essential for producing the lipid layer of the tear film that prevents tear evaporation. When combined with other dry eye tests, such as TBUT, osmolarity tests, and questionnaires like the OSDI, meibography provides a comprehensive understanding of a patient’s dry eye condition[102]. The use of the noninvasive keratograph, tear meniscus height, and bulbar injection, when compared to other clinical evaluation techniques such as the Schirmer test, etc., showed no correlation between the two techniques using the ocular surface disorder score[103]. In the detection of underlying issues, it has been found that there is a correlation between the onset of anterior segment endothelial anomalies in patients with dry eye.
Inflammatory biomarkers testing provide additional diagnostic precision, particularly in identifying inflammatory components of DED[104,105]. The ability to assess matrix metalloproteinase-9 can be a helpful tool in measuring response to treatment and monitoring the course of disease in cases of dry anophthalmic socket syndrome[104]. It was found that both patients with DED without Sjogren disease and those with Sjogren disease, with positive metalloproteinase-9, showed lower tear secretion and high tear osmolarity compared to those with negative metalloproteinase-9[106].
Artificial intelligence (AI) algorithms evaluate ocular images to identify early biomarkers of DED, improving diagnostic precision and efficiency. Deep learning algorithms, particularly deep transfer learning is said to be a new way of automatically analyzing inflammatory markers in the diagnosis and management of DED[107]. As an example, machine learning models have been shown to identify an increase or upregulation of tear proteins, in cases of DED of Sjogren origin or KCS[108,109]. These advancements in DED diagnostics enables better sensitivity in comparison to traditional methods.
Besides the use of AI in tear protein analysis as discussed earlier, it has also been integrated into immunoassay-based diagnostic techniques like the Chemiluminescent immunoassay and the Siemens immunonephelometric assay, which are close to precise methods for detecting immunoglobulins in related diseases and PSS[110]. There is an increased demand for the standardization of Schirmer’s strip production, processing of tear fluid, and analyte concentration normalization, and AI is primed to step in to ensure consistency and reproducibility in diagnostic protocols[111].
In addition to these efforts, AI models also support in clinical decision-making to assist eye care practitioners in the diagnosis of DED. For instance, Chatzaki et al[112] successfully developed an electronic tool for training primary eye care providers on accurate diagnosis of DED with commendable success with a 97.2% reported usability score[112].
Symptom evaluation: Employ validated questionnaires like the OSDI or SPEED to ascertain the intensity and frequency of symptoms.
Assess tear film stability: Perform TBUT and measure tear osmolarity to determine tear film integrity.
Ocular surface staining: Employ fluorescein and lissamine green staining to identify corneal injury.
Tear volume assessments: Conduct Schirmer’s test to evaluate tear production.
Imaging techniques: Meibography for assessing meibomian gland functionality and OCT for measuring tear meniscus.
Confirmatory and prognostic assessment: Employ in vivo confocal microscopy for nerve examination and tear film proteomics for inflammatory biomarkers.
DED therapy includes artificial tears, anti-inflammatory medications, punctal occlusion, and lifestyle adjustments. Recent therapeutics encompass regenerative medicine and biologics. Approved treatments encompass artificial tears, cyclosporine A, lifitegrast, and punctal plugs. Innovative therapies like regenerative eye drops and mesenchymal stem cell treatment are still in the experimental phase. Recent trials indicate that biologic medicines aimed at inflammation (e.g., IL-1 inhibitors) may surpass traditional anti-inflammatories in severe DED.
In the use of artificial tears as a DED therapy, the use of ocular lubricant for individuals with reflex tearing usually improves their complaints[113]. However, the use of orthokeratology lenses has been found to have little or no effect on tear film stability[114].
The addition of tear supplements to steroid and non-steroidal anti-inflammatory drugs following cataract surgery has been found to lessen DED symptoms post-operatively[115-117]. Water-free topical cyclosporin 0.1%, when used in comparison to a vehicle, had an earlier therapeutic effect on the ocular surface[118-120]. Hydroxyquinoline, when combined with cyclosporine, improved the Schirmer score and significantly reduced surface inflammation[121]. Topical spironolactone helps in the production of the lipid layer of tear film, which helps to reduce surface inflammation in cases of graft vs host disease[122]. Placebos have been employed to measure the intervention's efficacy in treating dry eyes[123].
Treating dry eyes with hyaluronic acid and Ginkobiloba eye drops significantly improves the symptoms of DED[124]. There is, however, no significant difference in the prolonged use of omega-3 fatty acids compared with those who discontinued their usage at some point[125-127]. Research has shown that Lacrimera drops improve dry eye treatment, using TBUT, Schirmer analysis, and corneal staining as parameters, and it has been found to have a high-level regeneration time that can be sustained for about a month after use[128]. Semi-fluorinated alkane eye drops improve symptoms of dry eyes in patients who underwent cataract surgery[129]. A similar outcome was achieved when a mirrored demographic was treated with sodium hyaluronate and dexpanthenol-containing eye drops also after cataract extraction[130].
Current studies on recombinant growth factors have been shown to give good symptom relief in the treatment of dry eyes[131]. The management of conjunctivochalasis is an important antidote in managing patients with dry eyes, especially those using high-frequency radio wave electrosurgery[132]. The use of contact lenses has been found to reduce inflammatory cell numbers on the ocular surface, thereby presenting a possible future management strategy for dry eyes[133] as it enhanced corneal nerve health while reducing activated/mature corneal inflammatory cell numbers, delivering a safe and promising new treatment for moderate-to-severe DED. Loteprenol-tobramycin combination drops have shown some promise in mitigating DED symptoms and progression, lending a voice to the characterization of DED and the inflammatory process[134].
In studies by Moon et al[135], autologous epithelial growth factor ointment successfully reduced areas of epithelial damage. Punctual cauterization using heat treatment can be helpful when dealing with severe, potentially scarring dry eyes[136]. In a similar vein, mesenchymal stem cells show promise in managing Sjorgen syndrome[137,138] due to their ability to stimulate nuclear factor id3. A summary of some of the methods used to manage dry eyes is shown in Table 6.
| Category | Ref. | Management tool | Details description |
| Management strategies | Akpek et al[118] | Topical cyclosporine 0.1% | A water-free cyclosporine formulation that improves the ocular surface in moderate-to-severe dry eye |
| Fogagnolo et al[124] | Hyaluronic acid and ginkgo biloba drops | Effective in improving symptoms, especially post-cataract surgery | |
| Wirta et al[131] | Recombinant human nerve growth factor | Promising in treating moderate-to-severe dry eye by enhancing corneal nerve regeneration | |
| Hu et al[138] | Mesenchymal stem cells | Shows promise in managing Sjögren's syndrome, potentially aiding in ocular surface repair | |
| Surgical options | Wang et al[136] | Punctal cauterization | Heat treatment that is useful for severe dry eye, particularly in preventing scarring |
| Ji et al[139] | High-frequency radiowave electrosurgery | Improves conjunctivochalasis, reducing symptoms and improving management outcomes | |
| Post-COVID-19 Considerations | Castillo et al[144] | Telehealthcare | Utilized to mitigate DED-linked ocular morbidity, particularly relevant post-COVID-19 |
The SARS-CoV-2 virus has forever changed the face of medicine and healthcare as we knew it[139-141]. In China and Italy for example, research has shown that the coronavirus disease 2019 (COVID-19) exacerbated symptoms in patients with rheumatoid related conditions, which are in themselves linked to DED[140-143]. The IMPULSE study carried out in Spain recommended that tele-healthcare can be utlized to mitigate DED-linked ocular morbidity[144]. Brito-Zerón et al[145] also reported a positive correlation between DED and exacerbation of COVID linked morbidities.
This paper was limited to reviewing records in the search pool published not older than 2020. A wider search criterion may have yielded more data to sample.
In conclusion, the effective management of DED begins with an accurate diagnosis. Integrating a combination of subjective and objective diagnostic tools allows clinicians to comprehensively assess the condition, tailor treatment plans, and monitor therapeutic efficacy. Continued advancements in diagnostic technologies promise to enhance our un
| 1. | Srivastava A, Makarenkova HP. Innate Immunity and Biological Therapies for the Treatment of Sjögren's Syndrome. Int J Mol Sci. 2020;21:9172. [PubMed] [DOI] [Full Text] |
| 2. | Sheppard J, Shen Lee B, Periman LM. Dry eye disease: identification and therapeutic strategies for primary care clinicians and clinical specialists. Ann Med. 2023;55:241-252. [PubMed] [DOI] [Full Text] |
| 3. | Wróbel-Dudzińska D, Osial N, Stępień PW, Gorecka A, Żarnowski T. Prevalence of Dry Eye Symptoms and Associated Risk Factors among University Students in Poland. Int J Environ Res Public Health. 2023;20:1313. [PubMed] [DOI] [Full Text] |
| 4. | Huang R, Su C, Fang L, Lu J, Chen J, Ding Y. Dry eye syndrome: comprehensive etiologies and recent clinical trials. Int Ophthalmol. 2022;42:3253-3272. [PubMed] [DOI] [Full Text] |
| 5. | Gu Q, Zheng Q, Zhang X, Lin L, Li S, Chen F, Zhang X, Yan LL, Chen W. Trends in Health Service Use for Dry Eye Disease From 2017 to 2021: A Real-World Analysis of 369,755 Outpatient Visits. Transl Vis Sci Technol. 2024;13:17. [PubMed] [DOI] [Full Text] |
| 6. | Pflugfelder SC, Stern ME. Biological functions of tear film. Exp Eye Res. 2020;197:108115. [PubMed] [DOI] [Full Text] |
| 7. | Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo CK, Liu Z, Nelson JD, Nichols JJ, Tsubota K, Stapleton F. TFOS DEWS II Definition and Classification Report. Ocul Surf. 2017;15:276-283. [PubMed] [DOI] [Full Text] |
| 8. | Warren NA, Maskin SL, Gurupur V, Rector DA, Adelman D, Howell S, McAree J, Dibble R, Carlisano C, Maconi DP, Schrotenboer D, Jaimes M, Marte N, Carlisano T, Toland C, Chung J, Cremers SL, Corbin GS. Engaging Stakeholders to Develop a Roadmap for Dry Eye and MGD PCORI-Funded Research. Patient Relat Outcome Meas. 2024;15:143-186. [PubMed] [DOI] [Full Text] |
| 9. | Rolando M, Barabino S. Dry Eye Disease: What Is the Role of Vitamin D? Int J Mol Sci. 2023;24:1458. [PubMed] [DOI] [Full Text] |
| 10. | Matossian C, Crowley M, Periman L, Sorkin S. Personalized Management of Dry Eye Disease: Beyond Artificial Tears. Clin Ophthalmol. 2022;16:3911-3918. [PubMed] [DOI] [Full Text] |
| 11. | Golden MI, Meyer JJ, Zeppieri M, Patel BC. Dry Eye Syndrome. 2024 Feb 29. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2025. [PubMed] |
| 12. | Conrady CD, Joos ZP, Patel BC. Review: The Lacrimal Gland and Its Role in Dry Eye. J Ophthalmol. 2016;2016:7542929. [PubMed] [DOI] [Full Text] |
| 13. | Manukhina EB, Downey HF, Shi X, Mallet RT. Intermittent hypoxia training protects cerebrovascular function in Alzheimer's disease. Exp Biol Med (Maywood). 2016;241:1351-1363. [PubMed] [DOI] [Full Text] |
| 14. | Rolando M, Cantera E, Mencucci R, Rubino P, Aragona P. The correct diagnosis and therapeutic management of tear dysfunction: recommendations of the P.I.C.A.S.S.O. board. Int Ophthalmol. 2018;38:875-895. [PubMed] [DOI] [Full Text] |
| 15. | Abbott K, Hanson KS, Lally J. Prevalence of dry eye disease in the low vision population at the University of Colorado. J Optom. 2024;17:100501. [PubMed] [DOI] [Full Text] |
| 16. | Tsubota K, Pflugfelder SC, Liu Z, Baudouin C, Kim HM, Messmer EM, Kruse F, Liang L, Carreno-Galeano JT, Rolando M, Yokoi N, Kinoshita S, Dana R. Defining Dry Eye from a Clinical Perspective. Int J Mol Sci. 2020;21:9271. [PubMed] [DOI] [Full Text] |
| 17. | Holland EJ, Luchs J, Karpecki PM, Nichols KK, Jackson MA, Sall K, Tauber J, Roy M, Raychaudhuri A, Shojaei A. Lifitegrast for the Treatment of Dry Eye Disease: Results of a Phase III, Randomized, Double-Masked, Placebo-Controlled Trial (OPUS-3). Ophthalmology. 2017;124:53-60. [PubMed] [DOI] [Full Text] |
| 18. | Greco G, Pistilli M, Asbell PA, Maguire MG; Dry Eye Assessment and Management Study Research Group. Association of Severity of Dry Eye Disease with Work Productivity and Activity Impairment in the Dry Eye Assessment and Management Study. Ophthalmology. 2021;128:850-856. [PubMed] [DOI] [Full Text] |
| 19. | Yu K, Asbell PA, Shtein RM, Ying GS; for Dry Eye Assessment and Management Study Research Group. Dry Eye Subtypes in the Dry Eye Assessment and Management (DREAM) Study: A Latent Profile Analysis. Transl Vis Sci Technol. 2022;11:13. [PubMed] [DOI] [Full Text] |
| 20. | Pal S, Vani G, Donthineni PR, Basu S, Arunasri K. Tear film microbiome in Sjogren's and non-Sjogren's aqueous deficiency dry eye. Indian J Ophthalmol. 2023;71:1566-1573. [PubMed] [DOI] [Full Text] |
| 21. | Pflugfelder SC, de Paiva CS. The Pathophysiology of Dry Eye Disease: What We Know and Future Directions for Research. Ophthalmology. 2017;124:S4-S13. [PubMed] [DOI] [Full Text] |
| 22. | Zhang Y, Chen JQ, Yang JY, Liao JH, Wu TH, Yu XB, Huang ZW, He Q, Wang Q, Song WJ, Luo J, Tao QW. Sex Difference in Primary Sjögren Syndrome: A Medical Records Review Study. J Clin Rheumatol. 2023;29:e78-e85. [PubMed] [DOI] [Full Text] |
| 23. | Lyne SA, Downie-Doyle S, Lester SE, Quinlivan A, Toby Coates P, Gordon TP, Rischmueller M. Primary Sjögren's syndrome in South Australia. Clin Exp Rheumatol. 2020;38 Suppl 126:57-63. [PubMed] |
| 24. | Tarn J, Lendrem D, Barnes M, Casement J, Ng WF. Comorbidities in the UK Primary Sjögren's Syndrome Registry. Front Immunol. 2022;13:864448. [PubMed] [DOI] [Full Text] |
| 25. | Deng X, Li J, Hou S, Ci B, Liu B, Xu K. Prevalence and impact of Sjögren's syndrome in primary biliary cholangitis: a systematic review and meta-analysis. Ann Hepatol. 2022;27:100746. [PubMed] [DOI] [Full Text] |
| 26. | Rihab B, Lina EH, Noémie ST, Jean S, Marjolaine G. The experience of dry mouth and screening for Sjogren's syndrome by the dentist: patient-reported experiences. BMC Oral Health. 2023;23:1010. [PubMed] [DOI] [Full Text] |
| 27. | Thwin KM, Kaneko N, Okubo H, Yamaga T, Suwama K, Yoshihara A, Iwasaki M, Ito Y, Tanaka J, Narita I, Ogawa H. Association between dry eye and periodontal disease in community-dwelling Japanese adults: data from the Uonoma cohort study. BMC Oral Health. 2024;24:47. [PubMed] [DOI] [Full Text] |
| 28. | Brzheskiy VV. [Modern possibilities of pathogenetically oriented therapy for dry eye syndrome]. Vestn Oftalmol. 2023;139:95-103. [PubMed] [DOI] [Full Text] |
| 29. | Cui D, Mathews P, Li G, VanCourt S, Akpek E. Outcomes of Sjögren's versus non-Sjögren's related dry eye in a longitudinal, tertiary clinic-based sample. PLoS One. 2021;16:e0261241. [PubMed] [DOI] [Full Text] |
| 30. | Tsai CY, Hong C, Hsu MY, Lai TT, Huang CW, Lu CY, Chen WL, Cheng CM. Fluorescence-based reagent and spectrum-based optical reader for lactoferrin detection in tears: differentiating Sjögren's syndrome from non-Sjögren's dry eye syndrome. Sci Rep. 2024;14:14505. [PubMed] [DOI] [Full Text] |
| 31. | Seror R, Chiche L, Beydon M, Desjeux G, Zhuo J, Vannier-Moreau V, Devauchelle-Pensec V. Estimated prevalence, incidence and healthcare costs of Sjögren's syndrome in France: a national claims-based study. RMD Open. 2024;10:e003591. [PubMed] [DOI] [Full Text] |
| 32. | Melchor S, Sánchez-Piedra C, Fernández Castro M, Andreu JL, Martínez Taboada V, Olivé A, Rosas J, Menor R, García-Aparicio Á, López Longo FJ, Manrique-Arija S, García Vadillo JA, López González R, Narváez J, Galisteo C, González Martín J, Naranjo A, Illera Ó, Moreira B, Raya E, Rodríguez López M, Júdez E, Moriano C, Torrente-Segarra V, García Magallón B, Guillén Astete C, Castellvi I, Bohórquez C, Loricera J, Belzunegui J, Carreira PE; Sjögrenser group, part of the Spanish Society of Rheumatology Systemic Autoimmune Diseases Study Group (EASSER). Digestive involvement in primary Sjögren's syndrome: analysis from the Sjögrenser registry. Clin Exp Rheumatol. 2020;38 Suppl 126:110-115. [PubMed] |
| 33. | Gomez GGF, Wang M, Siddiqui ZA, Gonzalez T, Capin OR, Willis L, Boyd L, Eckert GJ, Zero DT, Thyvalikakath TP. Longevity of dental restorations in Sjogren's disease patients using electronic dental and health record data. BMC Oral Health. 2024;24:203. [PubMed] [DOI] [Full Text] |
| 34. | Bukhari AF, Bugshan AS, Papas A, Desai B, Farag AM. Conservative Management of Chronic Suppurative Parotitis in Patients with Sjögren Syndrome: A Case Series. Am J Case Rep. 2021;22:e929553. [PubMed] [DOI] [Full Text] |
| 35. | Šijan Gobeljić M, Milić V, Pejnović N, Damjanov N. Chemosensory dysfunction, Oral disorders and Oral health-related quality of life in patients with primary Sjögren's syndrome: comparative cross-sectional study. BMC Oral Health. 2020;20:187. [PubMed] [DOI] [Full Text] |
| 36. | Sieiro Santos C, Oliveira MM, Solari PN, Mateus P, Santos MJ, Corominas H, Castro CÁ, Álvarez ED. Cardiovascular disease in patients with systemic autoimmune diseases: The relationship between self-perceived risk and actual risk. Reumatol Clin (Engl Ed). 2024;20:229-236. [PubMed] [DOI] [Full Text] |
| 37. | Amlani B, Elsayed G, Barvalia U, Kanne JP, Meyer KC, Sandbo N, Li Z, McCoy SS. Treatment of primary sjögren's syndrome-related interstitial lung disease: a retrospective cohort study. Sarcoidosis Vasc Diffuse Lung Dis. 2020;37:136-147. [PubMed] [DOI] [Full Text] |
| 38. | Lee AS, Scofield RH, Hammitt KM, Gupta N, Thomas DE, Moua T, Ussavarungsi K, St Clair EW, Meehan R, Dunleavy K, Makara M, Carsons SE, Carteron NL; Consensus Expert Panel (CEP) Members. Consensus Guidelines for Evaluation and Management of Pulmonary Disease in Sjögren's. Chest. 2021;159:683-698. [PubMed] [DOI] [Full Text] |
| 39. | Casal Moura M, Navin PJ, Johnson GB, Hartman TE, Baqir M, Yi ES, Ryu JH. Pulmonary nodules in patients with primary Sjögren's syndrome: Causes, clinico-radiologic features, and outcomes. Respir Med. 2020;174:106200. [PubMed] [DOI] [Full Text] |
| 40. | Lin CY, Wu CH, Chen HA, Hsu CY, Wang LH, Su YJ. Long-term renal prognosis among patients with primary Sjögren's syndrome and renal involvement: A nationwide matched cohort study. J Autoimmun. 2020;113:102483. [PubMed] [DOI] [Full Text] |
| 41. | Guo L, Zhao S, Liu X. Development of a nomogram for membranous nephropathy prediction in patients with primary Sjögren's syndrome: a 6-year retrospective study. Front Immunol. 2024;15:1320880. [PubMed] [DOI] [Full Text] |
| 42. | Smith TJ, Hegedüs L, Lesser I, Perros P, Dorris K, Kinrade M, Troy-Ott P, Wuerth L, Nori M. How patients experience thyroid eye disease. Front Endocrinol (Lausanne). 2023;14:1283374. [PubMed] [DOI] [Full Text] |
| 43. | Gau SY, Leong PY, Lin CL, Tsou HK, Wei JC. Higher Risk for Sjögren's Syndrome in Patients With Fibromyalgia: A Nationwide Population-Based Cohort Study. Front Immunol. 2021;12:640618. [PubMed] [DOI] [Full Text] |
| 44. | Casemore RK, Wolffsohn JS, Dutta D. Dry eye clinical practice patterns of UK optometrists. Cont Lens Anterior Eye. 2023;46:101889. [PubMed] [DOI] [Full Text] |
| 45. | Bhatt K, Singh S, Singh K, Kumar S, Dwivedi K. Prevalence of dry eye, its categorization (Dry Eye Workshop II), and pathological correlation: A tertiary care study. Indian J Ophthalmol. 2023;71:1454-1458. [PubMed] [DOI] [Full Text] |
| 46. | Novack GD, Asbell P, Barabino S, Bergamini MVW, Ciolino JB, Foulks GN, Goldstein M, Lemp MA, Schrader S, Woods C, Stapleton F. TFOS DEWS II Clinical Trial Design Report. Ocul Surf. 2017;15:629-649. [PubMed] [DOI] [Full Text] |
| 47. | Rolando M, Merayo-Lloves J. Management Strategies for Evaporative Dry Eye Disease and Future Perspective. Curr Eye Res. 2022;47:813-823. [PubMed] [DOI] [Full Text] |
| 48. | Lee YJ, Lin YC, Liao CC, Chang YS, Huang YH, Tsai IJ, Chen JH, Lin SH, Lin YF, Hsieh TW, Chen YS, Wu CY, Chang CC, Lin CY. Using anti-malondialdehyde-modified peptide adduct autoantibodies in serum of taiwanese women to diagnose primary Sjogren's syndrome. Clin Biochem. 2022;108:27-41. [PubMed] [DOI] [Full Text] |
| 49. | Acar-Denizli N, Horváth IF, Mandl T, Priori R, Vissink A, Hernandez-Molina G, Armagan B, Praprotnik S, Sebastian A, Bartoloni E, Rischmueller M, Pasoto SG, Nordmark G, Nakamura H, Fernandes Moça Trevisani V, Retamozo S, Carsons SE, Maure-Noia B, Sánchez-Berná I, López-Dupla M, Fonseca-Aizpuru E, Melchor Díaz S, Vázquez M, Díaz Cuiza PE, de Miguel Campo B, Ng WF, Rasmussen A, Dong X, Li X, Baldini C, Seror R, Gottenberg JE, Kruize AA, Sandhya P, Gandolfo S, Kwok SK, Kvarnstrom M, Solans R, Sene D, Suzuki Y, Isenberg DA, Valim V, Hofauer B, Giacomelli R, Devauchelle-Pensec V, Atzeni F, Gheita TA, Morel J, Izzo R, Kalyoncu U, Szántó A, Olsson P, Bootsma H, Ramos-Casals M, Kostov B, Brito-Zerón P; Sjögren Big Data Consortium. Systemic phenotype related to primary Sjögren's syndrome in 279 patients carrying isolated anti-La/SSB antibodies. Clin Exp Rheumatol. 2020;38 Suppl 126:85-94. [PubMed] |
| 50. | Dros JT, Bos I, Bennis FC, Wiegersma S, Paget J, Seghieri C, Barrio Cortés J, Verheij RA. Detection of primary Sjögren's syndrome in primary care: developing a classification model with the use of routine healthcare data and machine learning. BMC Prim Care. 2022;23:199. [PubMed] [DOI] [Full Text] |
| 51. | Sotozono C, Ueta M, Kinoshita S. Japan: Diagnosis and Management of Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis With Severe Ocular Complications. Front Med (Lausanne). 2021;8:657327. [PubMed] [DOI] [Full Text] |
| 52. | Inomata T, Nakamura M, Iwagami M, Midorikawa-Inomata A, Sung J, Fujimoto K, Okumura Y, Eguchi A, Iwata N, Miura M, Fujio K, Nagino K, Hori S, Tsubota K, Dana R, Murakami A. Stratification of Individual Symptoms of Contact Lens-Associated Dry Eye Using the iPhone App DryEyeRhythm: Crowdsourced Cross-Sectional Study. J Med Internet Res. 2020;22:e18996. [PubMed] [DOI] [Full Text] |
| 53. | Xu S, Luo J, Zhu C, Jiang J, Cheng H, Wang P, Hong J, Fang J, Pan J, Brown MA, Zhu X, Wang X. Performance Evaluation of Multiple Ultrasonographical Methods for the Detection of Primary Sjögren's Syndrome. Front Immunol. 2021;12:777322. [PubMed] [DOI] [Full Text] |
| 54. | Kaur RP, Gurnani B, Kaur K. Intricate insights into immune response in dry eye disease. Indian J Ophthalmol. 2023;71:1248-1255. [PubMed] [DOI] [Full Text] |
| 55. | Sheppard AL, Wolffsohn JS. Digital eye strain: prevalence, measurement and amelioration. BMJ Open Ophthalmol. 2018;3:e000146. [PubMed] [DOI] [Full Text] |
| 56. | Lu C, Han D, Zeng L, Hong J, Fadel D, Zhou X, Chen Z, Le Q. Short-Term Efficacy and Safety of Scleral Lenses in the Management of Severe Dry Eye in a Chinese Population. J Clin Med. 2025;14:658. [PubMed] [DOI] [Full Text] |
| 57. | Palikhey A, Koiree S, Kumar Mehta R, Kumar Shrivastava A. Dry Eye Disease among Patients with Glaucoma under Topical Antiglaucoma Agents in a Tertiary Care Centre: A Descriptive Cross-sectional Study. JNMA J Nepal Med Assoc. 2022;60:800-804. [PubMed] [DOI] [Full Text] |
| 58. | McDonnell PJ, Pflugfelder SC, Stern ME, Hardten DR, Conway T, Villanueva L, Hollander DA. Study design and baseline findings from the progression of ocular findings (PROOF) natural history study of dry eye. BMC Ophthalmol. 2017;17:265. [PubMed] [DOI] [Full Text] |
| 59. | Talens-Estarelles C, Cerviño A, García-Lázaro S, Fogelton A, Sheppard A, Wolffsohn JS. The effects of breaks on digital eye strain, dry eye and binocular vision: Testing the 20-20-20 rule. Cont Lens Anterior Eye. 2023;46:101744. [PubMed] [DOI] [Full Text] |
| 60. | Yu K, Bunya V, Maguire M, Asbell P, Ying GS; Dry Eye Assessment and Management Study Research Group. Systemic Conditions Associated with Severity of Dry Eye Signs and Symptoms in the Dry Eye Assessment and Management Study. Ophthalmology. 2021;128:1384-1392. [PubMed] [DOI] [Full Text] |
| 61. | Postnikoff CK, Huisingh C, McGwin G, Nichols KK. Leukocyte Distribution in the Open Eye Tears of Normal and Dry Eye Subjects. Curr Eye Res. 2018;43:1253-1259. [PubMed] [DOI] [Full Text] |
| 62. | Barrio-Cortes J, Gómez-Gascón T, Benito-Sánchez B, Domínguez-Berjón MF, Esteban-Vasallo MD, Chalco-Orrego JP, Vicente-Rabaneda EF, Baldini C, Seghieri C, Goules AV, Fotiadis DI, Tzioufas AG. Utilisation of primary healthcare services by Sjögren's syndrome patients in the Community of Madrid and associated factors: a population-based cross-sectional study. Clin Exp Rheumatol. 2023;41:2397-2408. [PubMed] [DOI] [Full Text] |
| 63. | Abuallut I, Hurissi E, Khawaji EA, Khormi G, Othathi R, Azyabi FY, Awlaqi A, Bakreen MGM, Ghulaysi S. Dry Eye Symptoms in Jazan University Lecturers During the COVID-19 Pandemic Using Ocular Surface Disease Index (OSDI). Cureus. 2023;15:e49123. [PubMed] [DOI] [Full Text] |
| 64. | Liampas A, Parperis K, Erotocritou MF, Nteveros A, Papadopoulou M, Moschovos C, Akil M, Coaccioli S, Hadjigeorgiou GM, Hadjivassiliou M, Zis P. Primary Sjögren syndrome-related peripheral neuropathy: A systematic review and meta-analysis. Eur J Neurol. 2023;30:255-265. [PubMed] [DOI] [Full Text] |
| 65. | Nagai N, Otake H. Novel drug delivery systems for the management of dry eye. Adv Drug Deliv Rev. 2022;191:114582. [PubMed] [DOI] [Full Text] |
| 66. | Ngo W, Situ P, Keir N, Korb D, Blackie C, Simpson T. Psychometric properties and validation of the Standard Patient Evaluation of Eye Dryness questionnaire. Cornea. 2013;32:1204-1210. [PubMed] [DOI] [Full Text] |
| 67. | Wang MTM, Misra SL, Gokul A, Kim JS, Kim AD, Xue AL, Cruzat A, Craig JP. Repeatability of tear film lipid layer interferometry measurements: A randomized, crossover study. Optom Vis Sci. 2025;. [PubMed] [DOI] [Full Text] |
| 68. | Samur Salbas C, Uslu S, Salbas E. Evaluation of lacrimal gland vascularisation using superb microvascular imaging: a potential diagnostic tool in Sjögren's syndrome. Mod Rheumatol. 2025;35:320-325. [PubMed] [DOI] [Full Text] |
| 69. | Guo Y, Peng R, Feng K, Hong J. Diagnostic Performance of McMonnies Questionnaire as a Screening Survey for Dry Eye: A Multicenter Analysis. J Ophthalmol. 2016;2016:6210853. [PubMed] [DOI] [Full Text] |
| 70. | Wu KY, Serhan O, Faucher A, Tran SD. Advances in Sjögren's Syndrome Dry Eye Diagnostics: Biomarkers and Biomolecules beyond Clinical Symptoms. Biomolecules. 2024;14:80. [PubMed] [DOI] [Full Text] |
| 71. | Huang Y, Li R, Ye S, Lin S, Yin G, Xie Q. Recent Advances in the Use of Exosomes in Sjögren's Syndrome. Front Immunol. 2020;11:1509. [PubMed] [DOI] [Full Text] |
| 72. | De Luca A, Ferraro A, De Gregorio C, Laborante M, Coassin M, Sgrulletta R, Di Zazzo A. Promising High-Tech Devices in Dry Eye Disease Diagnosis. Life (Basel). 2023;13:1425. [PubMed] [DOI] [Full Text] |
| 73. | Willis KA, Postnikoff CK, Freeman A, Rezonzew G, Nichols K, Gaggar A, Lal CV. The closed eye harbours a unique microbiome in dry eye disease. Sci Rep. 2020;10:12035. [PubMed] [DOI] [Full Text] |
| 74. | Pu Q, Wu Z, Li AL, Guo XX, Hu JJ, Li XY. Association between poor sleep quality and an increased risk of dry eye disease in patients with obstructive sleep apnea syndrome. Front Med (Lausanne). 2022;9:870391. [PubMed] [DOI] [Full Text] |
| 75. | Zheng Q, Li S, Wen F, Lin Z, Feng K, Sun Y, Bao J, Weng H, Shen P, Lin H, Chen W. The Association Between Sleep Disorders and Incidence of Dry Eye Disease in Ningbo: Data From an Integrated Health Care Network. Front Med (Lausanne). 2022;9:832851. [PubMed] [DOI] [Full Text] |
| 76. | Ebrahimi F, Ayatollahi H, Aghaei H. A clinical decision support system for diagnosing and determining severity of dry eye disease. Eye (Lond). 2023;37:1619-1624. [PubMed] [DOI] [Full Text] |
| 77. | Modrzejewska A, Cieszyński Ł, Zaborski D, Parafiniuk M. Infrared thermography for the analysis of ocular surface temperature after phacoemulsification. Arq Bras Oftalmol. 2020;83:202-208. [PubMed] [DOI] [Full Text] |
| 78. | Gonzales JA, Shiboski SC, Bunya VY, Akpek EK, Rose-Nussbaumer J, Seitzman GD, Criswell LA, Shiboski CH, Lietman TM. Ocular Clinical Signs and Diagnostic Tests Most Compatible With Keratoconjunctivitis Sicca: A Latent Class Approach. Cornea. 2020;39:1013-1016. [PubMed] [DOI] [Full Text] |
| 79. | Sahlu M, Giorgis AT. Dry eye disease among Glaucoma patients on topical hypotensive medications, in a tertiary hospital, Ethiopia. BMC Ophthalmol. 2021;21:155. [PubMed] [DOI] [Full Text] |
| 80. | Srivastava K, Bhatnagar KR, Shakrawal J, Tandon M, Jaisingh K, Pandey L, Roy F. Ocular surface changes in primary open-angle glaucoma on anti-glaucoma medications versus treatment-naïve patients. Indian J Ophthalmol. 2024;72:374-380. [PubMed] [DOI] [Full Text] |
| 81. | Zhao M, Yu Y, Roy NS, Ying GS, Asbell P, Bunya VY. Sex-related differences and hormonal effects in the Dry Eye Assessment and Management (DREAM) study. Br J Ophthalmol. 2023;108:23-29. [PubMed] [DOI] [Full Text] |
| 82. | Kourukmas R, Roth M, Geerling G. Automated vs. human evaluation of corneal staining. Graefes Arch Clin Exp Ophthalmol. 2022;260:2605-2612. [PubMed] [DOI] [Full Text] |
| 83. | Inomata T, Sung J, Nakamura M, Iwagami M, Akasaki Y, Fujio K, Nakamura M, Ebihara N, Ide T, Nagao M, Okumura Y, Nagino K, Fujimoto K, Eguchi A, Hirosawa K, Midorikawa-Inomata A, Muto K, Fujisawa K, Kikuchi Y, Nojiri S, Murakami A. Using the AllerSearch Smartphone App to Assess the Association Between Dry Eye and Hay Fever: mHealth-Based Cross-Sectional Study. J Med Internet Res. 2023;25:e38481. [PubMed] [DOI] [Full Text] |
| 84. | Fujio K, Nagino K, Huang T, Sung J, Akasaki Y, Okumura Y, Midorikawa-Inomata A, Fujimoto K, Eguchi A, Miura M, Hurramhon S, Yee A, Hirosawa K, Ohno M, Morooka Y, Murakami A, Kobayashi H, Inomata T. Clinical utility of maximum blink interval measured by smartphone application DryEyeRhythm to support dry eye disease diagnosis. Sci Rep. 2023;13:13583. [PubMed] [DOI] [Full Text] |
| 85. | Greiner JV, Ying GS, Pistilli M, Maguire MG, Asbell PA; Dry Eye Assessment and Management (DREAM) Study Research Group. Association of Tear Osmolarity With Signs and Symptoms of Dry Eye Disease in the Dry Eye Assessment and Management (DREAM) Study. Invest Ophthalmol Vis Sci. 2023;64:5. [PubMed] [DOI] [Full Text] |
| 86. | Chan KY, Guo B, Tse JS, Li PH, Cheong AM, Ngo W, Lam TC. A cross-sectional study of optometrists' attitudes towards dry eye disease management in Hong Kong: A web-based survey in Hong Kong. Heliyon. 2024;10:e31181. [PubMed] [DOI] [Full Text] |
| 87. | Abusharha A, Pearce EI, Afsar T, Razak S. Evaluation of therapeutic efficacy of Emustil drops for ocular discomfort and tear film osmolarity using different treatment management modes under dry environmental conditions. BMC Ophthalmol. 2024;24:129. [PubMed] [DOI] [Full Text] |
| 88. | García N, Melvi G, Pinto-Fraga J, Calonge M, Maldonado MJ, González-García MJ. Lack of Agreement among Electrical Impedance and Freezing-Point Osmometers. Optom Vis Sci. 2016;93:482-487. [PubMed] [DOI] [Full Text] |
| 89. | Daniel E, Pistilli M, Ying GS, Bunya VY, Massaro-Giordano M, Asbell PA, Maguire MG; Dry Eye Assessment and Management (DREAM) Study Research Group. Association of meibomian gland morphology with symptoms and signs of dry eye disease in the Dry Eye Assessment and Management (DREAM) study. Ocul Surf. 2020;18:761-769. [PubMed] [DOI] [Full Text] |
| 90. | Valim V, Trevisani VF, de Sousa JM, Vilela VS, Belfort R Jr. Current Approach to Dry Eye Disease. Clin Rev Allergy Immunol. 2015;49:288-297. [PubMed] [DOI] [Full Text] |
| 91. | Humayun S, Noor M, Shahid M, Naqvi SAH, Ishaq M, Humayun Q. Diagnosis of Dry Eye Syndrome Using Ocular Surface Disease Index, Tear Film Break-up Time, and Schirmer Test. J Coll Physicians Surg Pak. 2024;34:308-312. [PubMed] [DOI] [Full Text] |
| 92. | Barros A, Lozano-Sanroma J, Queiruga-Piñeiro J, Fernández-Vega Cueto L, Anitua E, Alcalde I, Merayo-Lloves J. Recovery of Corneal Innervation after Treatment in Dry Eye Disease: A Confocal Microscopy Study. J Clin Med. 2023;12:1841. [PubMed] [DOI] [Full Text] |
| 93. | Schmidl D, Schlatter A, Chua J, Tan B, Garhöfer G, Schmetterer L. Novel Approaches for Imaging-Based Diagnosis of Ocular Surface Disease. Diagnostics (Basel). 2020;10:589. [PubMed] [DOI] [Full Text] |
| 94. | Bu Y, Shih KC, Tong L. The ocular surface and diabetes, the other 21st Century epidemic. Exp Eye Res. 2022;220:109099. [PubMed] [DOI] [Full Text] |
| 95. | Camp AS, Long CP, Galor A, Yamane M, Proudfoot JA, Weinreb RN. Dry Eye Symptom Severity and Visual Field Reliability Metrics. J Glaucoma. 2022;31:305-309. [PubMed] [DOI] [Full Text] |
| 96. | Gorimanipalli B, Muthu S, Shetty R, Ranade RR, Khamar P. Nexus of ocular motility and dry eye. Indian J Ophthalmol. 2023;71:1546-1550. [PubMed] [DOI] [Full Text] |
| 97. | Inomata T, Sung J, Yee A, Murakami A, Okumura Y, Nagino K, Fujio K, Akasaki Y, Midorikawa-Inomata A, Eguchi A, Fujimoto K, Huang T, Morooka Y, Miura M, Shokirova H, Hirosawa K, Ohno M, Kobayashi H. P4 Medicine for Heterogeneity of Dry Eye: A Mobile Health-based Digital Cohort Study. Juntendo Iji Zasshi. 2023;69:2-13. [PubMed] [DOI] [Full Text] |
| 98. | Abou Shousha M, Wang J, Kontadakis G, Feuer W, Canto AP, Hoffmann R, Perez VL. Corneal epithelial thickness profile in dry-eye disease. Eye (Lond). 2020;34:915-922. [PubMed] [DOI] [Full Text] |
| 99. | Fujimoto K, Inomata T, Okumura Y, Iwata N, Fujio K, Eguchi A, Nagino K, Shokirova H, Karasawa M, Murakami A. Comparison of corneal thickness in patients with dry eye disease using the Pentacam rotating Scheimpflug camera and anterior segment optical coherence tomography. PLoS One. 2020;15:e0228567. [PubMed] [DOI] [Full Text] |
| 100. | Niedernolte B, Trunk L, Wolffsohn JS, Pult H, Bandlitz S. Evaluation of tear meniscus height using different clinical methods. Clin Exp Optom. 2021;104:583-588. [PubMed] [DOI] [Full Text] |
| 101. | Swiderska K, Read ML, Blackie CA, Maldonado-Codina C, Morgan PB. Latest developments in meibography: A review. Ocul Surf. 2022;25:119-128. [PubMed] [DOI] [Full Text] |
| 102. | Li S, Wang Y, Yu C, Li Q, Chang P, Wang D, Li Z, Zhao Y, Zhang H, Tang N, Guan W, Fu Y, Zhao YE. Unsupervised Learning Based on Meibography Enables Subtyping of Dry Eye Disease and Reveals Ocular Surface Features. Invest Ophthalmol Vis Sci. 2023;64:43. [PubMed] [DOI] [Full Text] |
| 103. | Sutphin JE, Ying GS, Bunya VY, Yu Y, Lin MC, McWilliams K, Schmucker E, Kuklinski EJ, Asbell PA, Maguire MG; Dry Eye Assessment and Management (DREAM) Study Research Group. Correlation of Measures From the OCULUS Keratograph and Clinical Assessments of Dry Eye Disease in the Dry Eye Assessment and Management Study. Cornea. 2022;41:845-851. [PubMed] [DOI] [Full Text] |
| 104. | Rokohl AC, Wall K, Trester M, Wawer Matos PA, Guo Y, Adler W, Pine KR, Heindl LM. Novel point-of-care biomarkers of the dry anophthalmic socket syndrome: tear film osmolarity and matrix metalloproteinase 9 immunoassay. Graefes Arch Clin Exp Ophthalmol. 2023;261:821-831. [PubMed] [DOI] [Full Text] |
| 105. | Dohlman TH, Ciralsky JB, Lai EC. Tear film assessments for the diagnosis of dry eye. Curr Opin Allergy Clin Immunol. 2016;16:487-491. [PubMed] [DOI] [Full Text] |
| 106. | Oh JY, Chun YS, Kim KW. Dichotomous versus 5-scale grading system for the interpretation of the point-of-care immunoassay for tear matrix metalloproteinase-9 in dry eye. Sci Rep. 2023;13:6085. [PubMed] [DOI] [Full Text] |
| 107. | Xu F, Qin Y, He W, Huang G, Lv J, Xie X, Diao C, Tang F, Jiang L, Lan R, Cheng X, Xiao X, Zeng S, Chen Q, Cui L, Li M, Tang N. A deep transfer learning framework for the automated assessment of corneal inflammation on in vivo confocal microscopy images. PLoS One. 2021;16:e0252653. [PubMed] [DOI] [Full Text] |
| 108. | Yoon SP, Yu Z, Pflugfelder SC, de Paiva CS. Differentially Expressed Tear Proteins in Sjögren's Syndrome Keratoconjunctivitis Sicca. Transl Vis Sci Technol. 2023;12:8. [PubMed] [DOI] [Full Text] |
| 109. | Zhang S, Echegoyen J. Point of care diagnosis of dry eye disease with a sensitive immunoassay for dual biomarker detection. Biochem Biophys Rep. 2022;32:101396. [PubMed] [DOI] [Full Text] |
| 110. | Qin Y, Jia Y, Liang C, Fu R, Liang Z, Wang Y, Feng M, Gao C, Luo J. Clinical Performance of Immunonephelometric Assay and Chemiluminescent Immunoassay for Detection of IgG Subclasses in Chinese. J Clin Lab Anal. 2024;38:e25033. [PubMed] [DOI] [Full Text] |
| 111. | Gijs M, Arumugam S, van de Sande N, Webers CAB, Sethu S, Ghosh A, Shetty R, Vehof J, Nuijts RMMA. Pre-analytical sample handling effects on tear fluid protein levels. Sci Rep. 2023;13:1317. [PubMed] [DOI] [Full Text] |
| 112. | Chatzaki C, Goules A, De Vita S, Zabotti A, Delporte C, Soyfoo MS, Barone F, Fisher BA, Brito-Zerón P, Bartoloni E, Mavragani CP, Fotiadis DI, Tzioufas AG, Tsiknakis M. A Training Tool to support the management and diagnosis of Sjögren's syndrome. Clin Exp Rheumatol. 2020;38 Suppl 126:174-179. [PubMed] |
| 113. | Gagliano C, Salvetat ML, Musa M, D'Esposito F, Rusciano D, Maniaci A, Pellegrini F, Scibilia G, Zeppieri M. Bacterial Insights: Unraveling the Ocular Microbiome in Glaucoma Pathogenesis. Front Biosci (Landmark Ed). 2024;29:310. [PubMed] [DOI] [Full Text] |
| 114. | Ruan J, Zhang Y, Chen Y. Influence of overnight orthokeratology on tear film and meibomian glands in myopic children: a prospective study. BMC Ophthalmol. 2023;23:136. [PubMed] [DOI] [Full Text] |
| 115. | Bharucha K, Zanzarukiya J, Hegade A, Deshpande R, Shetty R, Deshpande M. A comparative study to evaluate the effect of various postoperative treatment protocols on dry eye and patient satisfaction after phacoemulsification. Indian J Ophthalmol. 2023;71:1638-1642. [PubMed] [DOI] [Full Text] |
| 116. | Fogagnolo P, Giannaccare G, Mencucci R, Villani E, Orfeo V, Aragona P; Italian Dry Eye Study Group. Effectiveness of a New Active Tear Substitute Containing 0.2% Hyaluronic Acid and 0.001% Hydrocortisone on Signs and Symptoms of Dry Eye Disease by Means of Low- and High-Tech Assessments. Ophthalmol Ther. 2024;13:251-266. [PubMed] [DOI] [Full Text] |
| 117. | Akpek EK, Sheppard JD, Hamm A, Angstmann-Mehr S, Krösser S. Efficacy of a new water-free topical cyclosporine 0.1% solution for optimizing the ocular surface in patients with dry eye and cataract. J Cataract Refract Surg. 2024;50:644-650. [PubMed] [DOI] [Full Text] |
| 118. | Akpek EK, Wirta DL, Downing JE, Tauber J, Sheppard JD, Ciolino JB, Meides AS, Krösser S. Efficacy and Safety of a Water-Free Topical Cyclosporine, 0.1%, Solution for the Treatment of Moderate to Severe Dry Eye Disease: The ESSENCE-2 Randomized Clinical Trial. JAMA Ophthalmol. 2023;141:459-466. [PubMed] [DOI] [Full Text] |
| 119. | Deshmukh R, Ting DSJ, Elsahn A, Mohammed I, Said DG, Dua HS. Real-world experience of using ciclosporin-A 0.1% in the management of ocular surface inflammatory diseases. Br J Ophthalmol. 2022;106:1087-1092. [PubMed] [DOI] [Full Text] |
| 120. | Rao AT, Gupta A, Chauhan T, Basu S, Batra N, Sharma N, Sangwan VS, Gupta V, Mukherjee S. Efficacy and safety of 0.05% micellar nano-particulate (MNP) cyclosporine ophthalmic emulsion in the treatment of moderate-to-severe keratoconjunctivitis sicca: a 12-week, multicenter, randomized, active-controlled trial. BMC Ophthalmol. 2023;23:121. [PubMed] [DOI] [Full Text] |
| 121. | Periman LM, Perez VL, Saban DR, Lin MC, Neri P. The Immunological Basis of Dry Eye Disease and Current Topical Treatment Options. J Ocul Pharmacol Ther. 2020;36:137-146. [PubMed] [DOI] [Full Text] |
| 122. | Wong CW, Yang AA, Liu CY, Watsky MA, Lu X, Le HL, Yee RW. Topical Spironolactone in the Treatment of Ocular Graft-Versus-Host Disease. Cureus. 2023;15:e45136. [PubMed] [DOI] [Full Text] |
| 123. | Prinz J, Maffulli N, Fuest M, Walter P, Hildebrand F, Migliorini F. Placebo administration for dry eye disease: a level I evidence based systematic review and meta-analysis. Int J Clin Pharm. 2022;44:1087-1101. [PubMed] [DOI] [Full Text] |
| 124. | Fogagnolo P, Romano D, De Ruvo V, Sabella P, Rossetti L. Clinical Efficacy of an Eyedrop Containing Hyaluronic Acid and Ginkgo Biloba in the Management of Dry Eye Disease Induced by Cataract Surgery. J Ocul Pharmacol Ther. 2022;38:305-310. [PubMed] [DOI] [Full Text] |
| 125. | Hussain M, Shtein RM, Pistilli M, Maguire MG, Oydanich M, Asbell PA; DREAM Study Research Group. The Dry Eye Assessment and Management (DREAM) extension study - A randomized clinical trial of withdrawal of supplementation with omega-3 fatty acid in patients with dry eye disease. Ocul Surf. 2020;18:47-55. [PubMed] [DOI] [Full Text] |
| 126. | Roy NS, Yu Y, Ying GS, Maguire MG, Asbell PA; DREAM Study Group. Effect of Omega-3 on HLA-DR Expression by Conjunctival Cells and Tear Cytokine Concentrations in the Dry Eye Assessment and Management Study. Eye Contact Lens. 2022;48:384-390. [PubMed] [DOI] [Full Text] |
| 127. | Oydanich M, Maguire MG, Pistilli M, Hamrah P, Greiner JV, Lin MC, Asbell PA; Dry Eye Assessment and Management Study Research Group. Effects of Omega-3 Supplementation on Exploratory Outcomes in the Dry Eye Assessment and Management Study. Ophthalmology. 2020;127:136-138. [PubMed] [DOI] [Full Text] |
| 128. | Nepp J, Knoetzl W, Prinz A, Hoeller S, Prinz M. Management of moderate-to-severe dry eye disease using chitosan-N-acetylcysteine (Lacrimera®) eye drops: a retrospective case series. Int Ophthalmol. 2020;40:1547-1552. [PubMed] [DOI] [Full Text] |
| 129. | Son HS, Yildirim TM, Khoramnia R, Poompokawat P, Knorz MC, Auffarth GU. Semi-fluorinated Alkane Eye Drops Reduce Signs and Symptoms of Evaporative Dry Eye Disease After Cataract Surgery. J Refract Surg. 2020;36:474-480. [PubMed] [DOI] [Full Text] |
| 130. | Köppe MK, Hallak MK, Stengele AL, Khoramnia R, Auffarth GU. Evaluation of Dry Eye Treatment with Sodium Hyaluronate- and Dexpanthenol-Containing Eye Drops on Ocular Surface Improvement after Cataract Surgery. Diagnostics (Basel). 2024;14:1097. [PubMed] [DOI] [Full Text] |
| 131. | Wirta D, Lipsky W, Toyos M, Martel J, Goosey J, Verachtert A, El-Harazi S, Karpecki P, Allegretti M, Goisis G, Pasedis G, Mantelli F. Recombinant human nerve growth factor (cenegermin) for moderate-to-severe dry eye: phase II, randomized, vehicle-controlled, dose-ranging trial. BMC Ophthalmol. 2024;24:290. [PubMed] [DOI] [Full Text] |
| 132. | Marmalidou A, Palioura S, Dana R, Kheirkhah A. Medical and surgical management of conjunctivochalasis. Ocul Surf. 2019;17:393-399. [PubMed] [DOI] [Full Text] |
| 133. | Travé-Huarte S, Wolffsohn JS. Sutureless Dehydrated Amniotic Membrane (Omnigen) Application Using a Specialised Bandage Contact Lens (OmniLenz) for the Treatment of Dry Eye Disease: A 6-Month Randomised Control Trial. Medicina (Kaunas). 2024;60:985. [PubMed] [DOI] [Full Text] |
| 134. | Deom JE, Kannarr S, Vollmer P. Real-World Use of Loteprednol Etabonate 0.5%/Tobramycin 0.3% Ophthalmic Suspension for the Treatment of Ocular Surface Inflammatory Conditions. Clin Ophthalmol. 2022;16:3803-3809. [PubMed] [DOI] [Full Text] |
| 135. | Moon HS, Li L, Yoon HJ, Ji YS, Yoon KC. Effect of epidermal growth factor ointment on persistent epithelial defects of the cornea. BMC Ophthalmol. 2020;20:147. [PubMed] [DOI] [Full Text] |
| 136. | Wang Y, Carreno-Galeano JT, Singh RB, Dana R, Yin J. Long-term Outcomes of Punctal Cauterization in the Management of Ocular Surface Diseases. Cornea. 2021;40:168-171. [PubMed] [DOI] [Full Text] |
| 137. | Musa M, Zeppieri M, Enaholo ES, Salati C, Parodi PC. Adipose Stem Cells in Modern-Day Ophthalmology. Clin Pract. 2023;13:230-245. [PubMed] [DOI] [Full Text] |
| 138. | Hu L, Xu J, Wu T, Fan Z, Sun L, Liu Y, Li Y, Zhang C, Wang J, Ding Y, Wang S. Depletion of ID3 enhances mesenchymal stem cells therapy by targeting BMP4 in Sjögren's syndrome. Cell Death Dis. 2020;11:172. [PubMed] [DOI] [Full Text] |
| 139. | Ji YW, Seong H, Lee S, Alotaibi MH, Kim TI, Lee HK, Seo KY. The correction of conjunctivochalasis using high-frequency radiowave electrosurgery improves dry eye disease. Sci Rep. 2021;11:2551. [PubMed] [DOI] [Full Text] |
| 140. | Salvetat ML, Musa M, Pellegrini F, Salati C, Spadea L, Zeppieri M. Considerations of COVID-19 in Ophthalmology. Microorganisms. 2023;11:2220. [PubMed] [DOI] [Full Text] |
| 141. | Maniaci A, Lavalle S, Masiello E, Lechien JR, Vaira L, Boscolo-Rizzo P, Musa M, Gagliano C, Zeppieri M. Platelet-Rich Plasma (PRP) in the Treatment of Long COVID Olfactory Disorders: A Comprehensive Review. Biomedicines. 2024;12:808. [PubMed] [DOI] [Full Text] |
| 142. | Ferri C, Giuggioli D, Raimondo V, L'Andolina M, Tavoni A, Cecchetti R, Guiducci S, Ursini F, Caminiti M, Varcasia G, Gigliotti P, Pellegrini R, Olivo D, Colaci M, Murdaca G, Brittelli R, Mariano GP, Spinella A, Bellando-Randone S, Aiello V, Bilia S, Giannini D, Ferrari T, Caminiti R, Brusi V, Meliconi R, Fallahi P, Antonelli A; COVID-19 & ASD Italian Study Group. COVID-19 and rheumatic autoimmune systemic diseases: report of a large Italian patients series. Clin Rheumatol. 2020;39:3195-3204. [PubMed] [DOI] [Full Text] |
| 143. | Ren Y, Tian J, Shi W, Feng J, Liu Y, Kang H, Chen B, He Y. Evaluation and correlation analysis of ocular surface disorders and quality of life in autoimmune rheumatic diseases: a cross-sectional study. BMC Ophthalmol. 2023;23:229. [PubMed] [DOI] [Full Text] |
| 144. | Benítez Del Castillo JM, Alejandre Alba N, Henares I, Ferraris MP, Águila M. IMPULSE Study: Impact of COVID-19 in the present of ophthalmology focusing on ocular surface and future trends. Arch Soc Esp Oftalmol (Engl Ed). 2023;98:213-219. [PubMed] [DOI] [Full Text] |
| 145. | Brito-Zerón P, Acar-Denizli N, Romão VC, Armagan B, Seror R, Carubbi F, Melchor S, Priori R, Valim V, Retamozo S, Pasoto SG, Trevisani VFM, Hofauer B, Szántó A, Inanc N, Hernández-Molina G, Sebastian A, Bartoloni E, Devauchelle-Pensec V, Akasbi M, Giardina F, Bandeira M, Sisó-Almirall A, Ramos-Casals M; Sjögren Big Data Consortium. Post-COVID-19 syndrome in patients with primary Sjögren's syndrome after acute SARS-CoV-2 infection. Clin Exp Rheumatol. 2021;39 Suppl 133:57-65. [PubMed] [DOI] [Full Text] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/