Published online Dec 20, 2025. doi: 10.5662/wjm.v15.i4.101181
Revised: February 26, 2025
Accepted: March 18, 2025
Published online: December 20, 2025
Processing time: 332 Days and 3.5 Hours
Hyponatremia is the most common electrolyte imbalance, however the prognostic significance of hyponatremia in peripartum cardiomyopathy (PPCM) remains unclear.
To assess the prognostic significance of hyponatremia in PPCM patients.
We consecutively recruited patients with PPCM from 14 sites in Nigeria and followed them up for a median of 18 months. Serum sodium was measured at baseline, and patients with hyponatremia (< 135 mmol/L) were compared with those with normal sodium levels. Cox proportional hazards regression models were developed to identify factors associated with all-cause mortality.
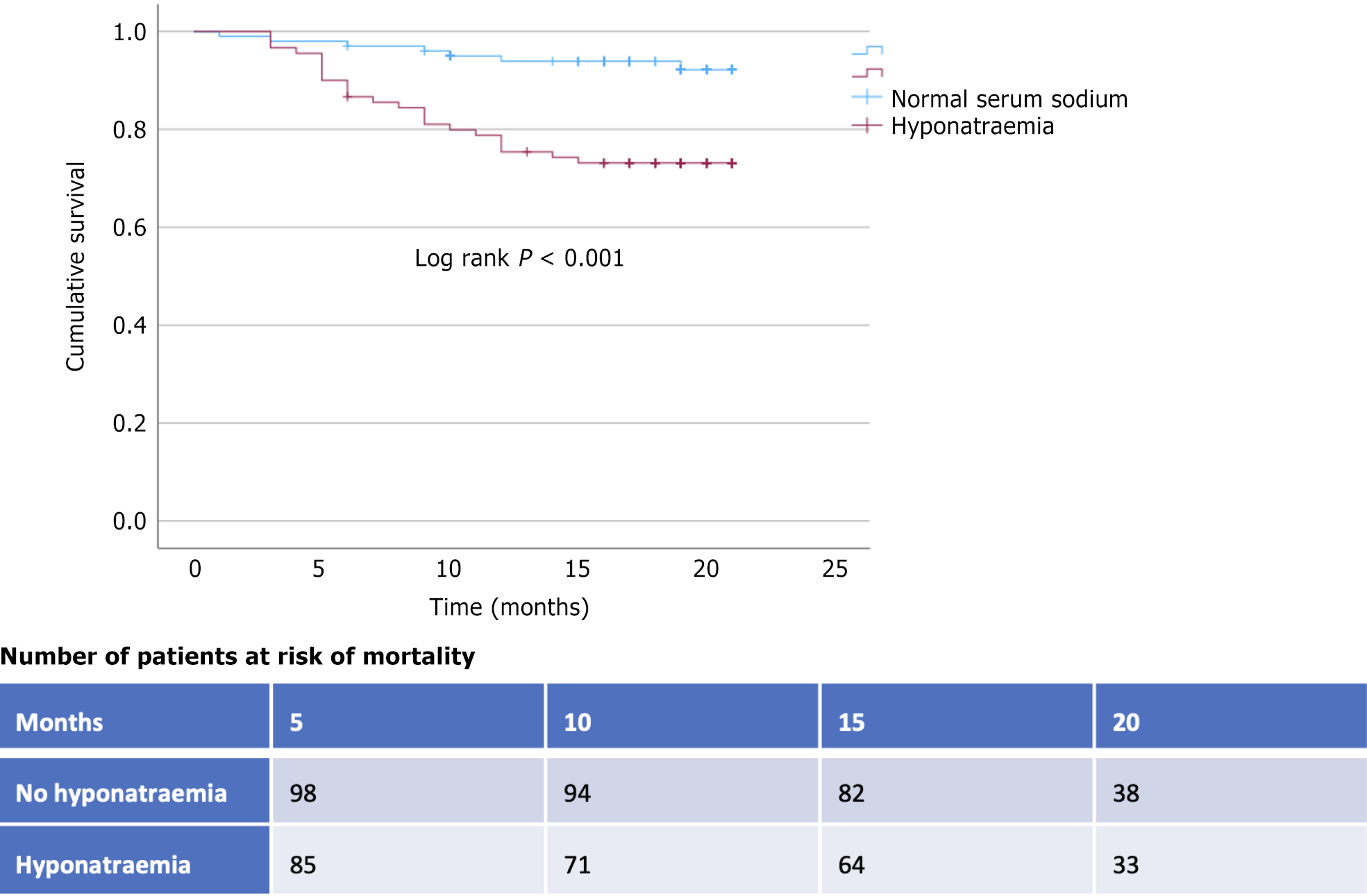
Of the 191 PPCM patients recruited, 90 (47.1%) had hyponatremia at presentation. All-cause mortality among the hyponatremic patients (24/90; 26.7%) was significantly higher than among patients with normal serum sodium (7/101; 6.9%) (P-value < 0.001). In the Cox proportional hazards regression model, hyponatremia was independently associated with an increased risk of all-cause mortality [hazard ratio: 3.18 (95% confidence interval: 1.35-7.52; P = 0.008)], as were hypotension (systolic blood pressure < 100 mmHg) [2.22 (1.03-4.79); P = 0.043] and left ventricular ejection fraction (LVEF) < 25% [3.14 (1.47-6.73), P = 0.003].
Hyponatremia was common in our cohort of PPCM patients, and was independently associated with a threefold increased risk for all-cause mortality. Hypotension and a LVEF below 25% at presentation were also independent predictors of mortality.
Core Tip: Hyponatremia was common in our cohort of peripartum cardiomyopathy (PPCM) patients, and independently associated with threefold increased risk for all-cause mortality. Hypotension and a left ventricular ejection fraction below 25% at presentation were also independently associated with mortality. Our findings suggest that presence of hyponatraemia in PPCM patients at admission should prompt a thorough clinical evaluation and close clinical monitoring, to identify and address factors contributing to increased mortality risk.
- Citation: Karaye KM, Ishaq NA, Saidu H, Balarabe SA, Talle MA, Isa MS. Prognostic significance of hyponatremia in peripartum cardiomyopathy. World J Methodol 2025; 15(4): 101181
- URL: https://www.wjgnet.com/2222-0682/full/v15/i4/101181.htm
- DOI: https://dx.doi.org/10.5662/wjm.v15.i4.101181
Hyponatremia is the most common electrolyte imbalance, occuring in 10%-30% of hospitalized heart failure (HF) patients[1]. It is a well-described independent predictor of poor prognosis for both hospitalised and ambulatory HF patients[2]. Importantly, the reversal of the hyponatremia in HF is associated with improved survival[1]. Hyponatremia in HF can be either dilutional, which is more common and results from excessive neurohumoral upregulation leading to impaired water excretion, or depletional, which is primarily due to excessive natriuresis with the use of loop diuretics, or a combination of both mechanisms[3]. Hyponatremia is a strong predictor of mortality among HF patients, but it is unclear whether it has a direct effect on mortality or is only a marker of HF severity[1,2].
Peripartum cardiomyopathy (PPCM) is an important cause of HF among women in northern Nigeria and many other parts of the world, with an incidence as high as 1 in 96 live births, and maternal age < 20 years, hypotension, tachycardia, and left ventricular ejection fraction (LVEF) < 25% at baseline independently predicted mortality[4,5]. However, the prognostic significance of hyponatremia in PPCM is unknown. In this post-hoc analysis of PEACE (PPCM in Nigeria) registry data, we aimed to determine the prognostic significance of hyponatremia in PPCM patients. We hypothesised that hyponatremia would be associated with worse prognosis in PPCM patients.
In the PEACE registry, PPCM patients were consecutively recruited from 14 sites across the geopolitical regions of Nigeria, and followed for a median of 18 months. The details of the study protocol have been previously published[6]. All data and supporting materials are available with the published article. PPCM patients were enrolled into the study after obtaining written informed consent, if they had HF symptoms and LVEF below 45%. Ethical approval for the study was obtained from the Research Ethics Committees of all the participating centres before the commencement of the study[6]. The study conformed to the ethical guidelines of the Declaration of Helsinki on the principles of medical research involving human subjects[7].
Serum sodium was measured at baseline using standard methods at the study sites, and patients with hyponatremia (< 135 mmol/L) were compared with those with normal values[8]. Unrecovered left ventricular (LV) systolic function was defined as LVEF ≤ 55% at the last follow-up.
Investigators were encouraged to prescribe standard and locally available HF drug therapies. These included a diuretic, beta-blocker, angiotensin converting enzyme inhibitor or an angiotensin II receptor blocker or nitrate-hydralazine combination, and a mineralocorticoid receptor antagonist, unless such use was contraindicated or resulted in unacceptable side effects. In addition, drug doses were individually tailored, in accordance with guideline recommendations[9].
Data was cleaned then summarised using standard statistical methods including mean (± SD), and proportions. Patients were classified into two groups (hyponatremic vs normal sodium levels) and compared based on baseline and last follow-up characteristics of interest. χ2, Fisher’s exact test, and student’s t and Mann-Whitney tests were used to compare categorical and continuous variables, as appropriate. Mortality (occurring from baseline profiling to end of follow-up) was analysed in all 191 cases with complete follow-up using the Kaplan-Meier method followed by a Cox proportional hazards model (entry method with proportional hazards confirmed by visual inspection) to derive adjusted hazard ratios (HR) and 95% confidence interval (95%CI), with consideration of baseline demographic and clinical characteristics as independent correlates of all-cause mortality. Variables included in the model have been previously linked with increased risk for either mortality or hyponatremia in PPCM and HF patients[2,5]. A two-sided P-value < 0.05 was considered statistically significant. Statistical analyses were performed using “Statistical Package for Social Sciences” version 23.0 software.
A total of 191 PPCM patients were recruited from 14 sites across five out of the six geopolitical regions of Nigeria (155 patients from North-West, 17 patients from North-Central, 15 patients from South-West, 1 patient from South-East and 3 patients from South-South).
Overall, 90 of the 191 (47.1%) PPCM patients had hyponatremia at presentation. The clinical characteristics and prescriptions for diuretics and other HF drugs were well-balanced between the 2 groups; with and without hyponatremia (Table 1). None of the patients in both groups reported history of smoking and diabetes mellitus, and only one patient in each group reported alcohol intake. In addition,16.7% and 15.8% of the patients with and without hyponatremia respectively (P = 0.877) were recruited as in-patients.
| Variables | Hyponatremia (n = 90) | Normal serum sodium (n = 101) | P value |
| Serum sodium, mmol/L | 126.7 ± 22.3 | 139.9 ± 3.2 | < 0.001 |
| Age, years | 28.5 ± 7.2 | 30.3 ± 7.2 | 0.086 |
| NYHA II-IV | 66 (73.3) | 83 (82.2) | 0.141 |
| Unemployment | 66 (73.3) | 74 (73.3) | 0.878 |
| Uneducated | 67 (74.4) | 67 (66.3) | 0.289 |
| Multiparity | 65 (72.2) | 76 (75.3) | 0.757 |
| Twin pregnancy | 18 (20.0) | 13 (12.9) | 0.256 |
| Obesity | 1 (1.1) | 5 (5.0) | 0.270 |
| Stroke | 3 (3.3) | 1 (1.0) | 0.344 |
| History of preeclampsia | 17 (18.9) | 19 (18.8) | 0.960 |
| Systolic BP, mmHg | 108 ± 16 | 110 ± 18 | 0.255 |
| Diastolic BP, mmHg | 74 ± 13 | 76 ± 15 | 0.233 |
| Heart rate/min | 100 ± 17 | 100 ± 19 | 0.789 |
| Ascites | 22 (24.4) | 27 (26.7) | 0.718 |
| Left atrium, mm | 45.4 ± 7.0 | 44.6 ± 6.7 | 0.465 |
| LV end-diastolic dimension, mm | 61.7 ± 9.2 | 62.5 ± 6.9 | 0.525 |
| LV ejection fraction at baseline | 30.1 ± 8.0 | 29.8 ± 7.4 | 0.777 |
| LV ejection fraction at last follow-up | 44.2 ± 12.7 | 42.5 ± 13.3 | 0.398 |
| Serum creatinine, µmol/L | 82.8 ± 29.3 | 82.5 ± 29.3 | 0.949 |
| Heart failure treatment | |||
| Loop diuretics | 77 (85.6) | 86 (85.2) | 0.762 |
| Thiazide diuretics | 1 (1.1) | 0 | 0.471 |
| ACEI or ARB or BB | 32 (35.6) | 38 (37.6) | 0.767 |
| Spironolactone | 84 (93.3) | 94 (93.1) | 0.942 |
All-cause mortality among the hyponatremic patients (26.7%) was significantly higher than among patients with normal serum sodium (6.9%) (P value < 0.001) (Table 2; Figure 1). The risk for all-cause mortality was independently increased by hyponatremia (HR 3.2; 95%CI: 1.4-7.5; P-value = 0.008), hypotension (systolic blood pressure < 100 mmHg) [HR 2.2 (95%CI: 1.0-4.8); P = 0.043], and LVEF < 25% [HR 3.1 (95%CI: 1.5-6.7); P = 0.003], after adjusting for loop diuretics (HR 1.1; P = 0.924), serum creatinine (HR 1.01; P = 0.425), preeclampsia (HR 0.8; P = 0.713) and tachycardia (HR 2.1; P = 0.130), at presentation respectively. Majority of the patients did not recover LV systolic function and rehospitalization was uncommon in both groups.
| Variables | Hyponatremia (n = 90) | Normal serum sodium (n = 101) | P value |
| Mortality | 24 (26.7) | 7 (6.9) | < 0.001 |
| Unrecovered left ventricular function | 57 (63.3) | 73 (72.3) | 0.521 |
| Rehospitalization | 6 (6.7) | 10 (9.9) | 0.587 |
The paper was written according to the STROBE (Strengthening the Reporting of Observational studies in Epidemiology) Statement-checklist of items for cohort studies.
This study has shown, perhaps for the first time in PPCM patients, that hyponatremia at presentation was common and independently associated with threefold higher risk of all-cause mortality. The risk for mortality was also independently increased by hypotension and LVEF < 25% at baseline. It was however not associated with rehospitalisation and unrecovered LV systolic function. The LV systolic function in both groups still improved by 13-14%, irrespective of the hyponatremia status, in keeping with the natural history of PPCM. Thus, PPCM patients presenting with a combination of hyponatremia, hypotension and LVEF < 25% are at significantly high risk of short-term mortality, thus should be closely monitored and referred early to a specialized centre.
The prevalence of hyponatraemia in our study (47.1%) is higher than what was found in the European Society of Cardiology (ESC) HF long-term registry (20%) among patients hospitalized for acute HF[1]. In this retrospective analysis of the ESC Registry data, hyponatraemia at admission, defined as serum sodium concentration < 135 mmol/L, was associated with more advanced HF and worse in-hospital and post-discharge outcomes[1]. Importantly, HF patients with persisting hyponatraemia throughout admission had the highest in-hospital mortality as well as worst post-discharge outcomes, with all-cause mortality 60% higher than the reference group[1].
The prevalence of hyponatremia among HF patients of mixed aetiology admitted to a tertiary-level hospital in Ethiopia was lower than our finding among PPCM patients (28.9% vs 47.1% respectively)[10]. In that cohort, 49.3% were females and ischaemic heart disease was the predominant cause of HF (41%), followed by valvular heart disease (21%), hypertensive heart disease (17%) and dilated cardiomyopathy (11%). The lower prevalence of hyponatremia in this study was probably due to the lesser use of diuretics relative to our cohort (loop diuretics 29% vs 85%; spironolactone 9% vs 93%; thiazides 5% vs 1% respectively). However it is not clear whether PPCM has a predilection for hyponatremia.
In the Hyponatremia Registry for patients with euvolemic and hypervolemic hyponatremia in the United States, 29% of the HF patients had hyponatraemia. Unfortunately, the most commonly used treatment approaches for hyponatraemia in acute HF only increased serum sodium minimally, and most patients remained hyponatraemic at discharge[11].
Hyponatremia is considered a powerful independent marker of poor outcomes in patients with acute or chronic HF[12]. Given that hyponatraemia in HF is primarily dilutional, treatment is based on water restriction or vasopressin antagonists. Fluid should be restricted to less than 800-1000 mL/day to achieve a negative water balance and treat the hyponatraemia[12]. However, severe hyponatremia (£125 mmol/L) should be treated with intravenous hypertonic saline, targeting an increase in serum sodium of 1-2 mmol/L per hour, and ensuring that the increase is less than 8 mmol/L in a 24 hour period, to avoid the risk of myelinolysis[12].
Our results suggest that presence of hyponatraemia in PPCM patients at admission should prompt a thorough clinical evaluation and close clinical monitoring, to detect and treat the hyponatremia as well as other factors associated with increased risk of mortality. However, it is important to emphasise the post-hoc nature of our analysis and the overall pragmatic design of the PEACE registry; given the inherent challenges in optimally diagnosing and treating PPCM in an African setting.
Hyponatremia was common in our cohort of PPCM patients, and independently associated with 3-fold higher risk for all-cause mortality. Hypotension and LVEF below 25% at presentation were also independently associated with mortality.
The authors wish to acknowledge and thank all investigators that contributed data at the study sites.
| 1. | Kapłon-Cieślicka A, Benson L, Chioncel O, Crespo-Leiro MG, Coats AJS, Anker SD, Ruschitzka F, Hage C, Drożdż J, Seferovic P, Rosano GMC, Piepoli M, Mebazaa A, McDonagh T, Lainscak M, Savarese G, Ferrari R, Mullens W, Bayes-Genis A, Maggioni AP, Lund LH; on behalf of the Heart Failure Association (HFA) of the European Society of Cardiology (ESC) and the ESC Heart Failure Long-Term Registry Investigators. Hyponatraemia and changes in natraemia during hospitalization for acute heart failure and associations with in-hospital and long-term outcomes - from the ESC-HFA EORP Heart Failure Long-Term Registry. Eur J Heart Fail. 2023;25:1571-1583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 2. | Corona G, Giuliani C, Parenti G, Norello D, Verbalis JG, Forti G, Maggi M, Peri A. Moderate hyponatremia is associated with increased risk of mortality: evidence from a meta-analysis. PLoS One. 2013;8:e80451. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 164] [Cited by in RCA: 211] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 3. | Tee SL, Sindone A, Roger S, Atherton J, Amerena J, D'Emden M, Erlich J, De Pasquale C. Hyponatraemia in heart failure. Intern Med J. 2020;50:659-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Karaye KM, Ishaq NA, Sa'idu H, Balarabe SA, Talle MA, Isa MS, Adamu UG, Umar H, Okolie HI, Shehu MN, Mohammed IY, Sanni B, Ogah OS, Oboirien I, Umuerri EM, Mankwe AC, Shidali VY, Njoku P, Dodiyi-Manuel S, Shogade TT, Olunuga T, Ojji D, Josephs V, Mbakwem AC, Tukur J, Isezuo SA; PEACE Registry Investigators. Incidence, clinical characteristics, and risk factors of peripartum cardiomyopathy in Nigeria: results from the PEACE Registry. ESC Heart Fail. 2020;7:235-243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | Karaye KM, Sa'idu H, Balarabe SA, Ishaq NA, Adamu UG, Mohammed IY, Oboirien I, Umuerri EM, Mankwe AC, Shidali VY, Njoku P, Dodiyi-Manuel S, Olunuga T, Josephs V, Mbakwem AC, Okolie H, Talle MA, Isa MS, Ogah OS, Stewart S; PEACE Registry Investigators. Clinical Features and Outcomes of Peripartum Cardiomyopathy in Nigeria. J Am Coll Cardiol. 2020;76:2352-2364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 6. | Karaye KM, Mohammed IY, Ogah OS, Okeahialam BN. Rationale and Design for the Peripartum Cardiomyopathy in Nigeria (PEACE) Registry. ICFJ. 2018;12. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Postgrad Med. 2002;48:206-208. [PubMed] |
| 8. | Malandrini S, Lava SAG, Bianchetti MG, Meani F, Faré PB, Camozzi P, Cugliari M, Agostoni C, Milani GP. Which laboratory technique is used for the blood sodium analysis in clinical research? A systematic review. Clin Chem Lab Med. 2021;59:1501-1506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Sliwa K, Hilfiker-Kleiner D, Petrie MC, Mebazaa A, Pieske B, Buchmann E, Regitz-Zagrosek V, Schaufelberger M, Tavazzi L, van Veldhuisen DJ, Watkins H, Shah AJ, Seferovic PM, Elkayam U, Pankuweit S, Papp Z, Mouquet F, McMurray JJ; Heart Failure Association of the European Society of Cardiology Working Group on Peripartum Cardiomyopathy. Current state of knowledge on aetiology, diagnosis, management, and therapy of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Working Group on peripartum cardiomyopathy. Eur J Heart Fail. 2010;12:767-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 616] [Cited by in RCA: 659] [Article Influence: 54.9] [Reference Citation Analysis (0)] |
| 10. | Ali K, Workicho A, Gudina EK. Hyponatremia in patients hospitalized with heart failure: a condition often overlooked in low-income settings. Int J Gen Med. 2016;9:267-273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Dunlap ME, Hauptman PJ, Amin AN, Chase SL, Chiodo JA 3rd, Chiong JR, Dasta JF. Current Management of Hyponatremia in Acute Heart Failure: A Report From the Hyponatremia Registry for Patients With Euvolemic and Hypervolemic Hyponatremia (HN Registry). J Am Heart Assoc. 2017;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (1)] |
| 12. | McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Coats AJS, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Kathrine Skibelund A; ESC Scientific Document Group. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42:3599-3726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8225] [Cited by in RCA: 8584] [Article Influence: 1716.8] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/