Published online Dec 25, 2025. doi: 10.5527/wjn.v14.i4.110791
Revised: July 4, 2025
Accepted: September 24, 2025
Published online: December 25, 2025
Processing time: 191 Days and 14.1 Hours
Acute kidney injury (AKI) is a common and serious complication following heart transplantation, significantly impacting patient outcomes and survival rates. AKI after transplantation can lead to prolonged hospital stays, increased morbidity, and even mortality.
To identify and quantify significant risk factors associated with AKI following heart transplantation through a systematic review and meta-analysis. This study aims to distinguish predictive variables that may inform perioperative risk stratification and clinical decision-making.
Electronic searches on MEDLINE, Google Scholar, ScienceDirect, Clinical
Out of 1345 articles, 13 studies with 3330 patients were included. Significant risk factors included age [overall MD = 2.27 years (95%CI: 0.13 to 4.41)], body mass index (BMI) [MD = 1.42 (95%CI: 0.60 to 2.24)], diabetes [overall OR = 1.47 (95%CI: 1.16 to 1.85)], chronic kidney disease (CKD) [OR = 2.67 (95%CI: 1.73 to 4.14)], chronic obstructive pulmonary disorder (COPD) [OR = 0.49 (95%CI: 0.27 to 0.89)], previous thoracic surgery [(OR) = 1.27, 95%CI: (1.05 to 1.54)], cardio-pulmonary bypass time [(MD) = 17.10, 95%CI: (6.12 to 28.08)], mechanical ventilation duration [(MD) = 30.87 hours, 95%CI: (10.69 to 51.05)] and extracorporeal membrane oxygenation [(OR) = 2.31, 95%CI: (1.25 to 4.26)]. Factors not associated with AKI after heart transplantation included Recipients’ male sex (P = 0.55), donor sex (P = 0.11), hypertension (P = 0.13), smoking (P = 0.20), coronary artery disease (P = 0.90), pulmonary artery disease (P = 0.81), dilated cardiomyopathy (P = 0.79), ventilation duration (P = 0.24), ischemic time (P = 0.06), use of intra-aortic balloon pump (P = 0.14), LVAD transplantation (P = 0.83), and Inotropes use (P = 0.78).
Age, BMI, diabetes, CKD, COPD, previous thoracic surgery, prolonged CPB time, extended mechanical ventilation, and ECMO use are significant predictors of AKI following heart transplantation, necessitating vigilant monitoring and individualized risk assessment. Conversely, factors such as LVAD implantation and inotrope use showed no significant association, highlighting the need for further investigation into their roles. Future prospective studies are essential to validate these findings, elucidate underlying mechanisms, and develop targeted interventions to mitigate AKI risk and improve patient outcomes.
Core Tip: Acute kidney injury (AKI) is a potential complication after heart transplant surgery and various patient demo
- Citation: Khawar M, Sehar A, Shahzad M, Farooq H, Rehman OU, Alvi Z, Ali S, Hadeed Khawar MM, Saifullah M, Khail HA, Qadeer A, Villanueva MN, Mour GK. Risk factors for developing acute kidney injury after heart transplant: A systematic review and meta-analysis. World J Nephrol 2025; 14(4): 110791
- URL: https://www.wjgnet.com/2220-6124/full/v14/i4/110791.htm
- DOI: https://dx.doi.org/10.5527/wjn.v14.i4.110791
Acute kidney injury (AKI) is defined as a rapid, often abrupt decrease in renal function, encompassing both structural and functional dysfunction. It is characterized by an increased serum creatinine and/or a decreased urine volume[1]. Various criteria, such as the Acute Kidney Injury Network criteria and the Risk, Injury, Failure, Loss of kidney function, End-stage renal failure criteria have been used to define AKI. Merging the two criteria, the kidney disease: Improving Global Outcomes criteria has gradually become the standard, providing a simple and practical definition[2]. A meta-analysis has reported the incidence of AKI to be 21.6%, with a mortality of 23.9%[3]. In Pakistan, limited data suggest a higher incidence in hospitalized patients, ranging from 25% to 30%, particularly in critical care settings, though comprehensive national studies are lacking. These epidemiological differences highlight the need for region-specific research to address local healthcare challenges and inform targeted interventions.
AKI presents as one of the most common and serious complications in heart transplant (HT) patients. The reported incidence of AKI following heart transplantation ranges between 14% and 83%[4]. Heart transplantation involves replacing a failing heart with a donor heart, typically indicated for end-stage heart failure or severe cardiac conditions unresponsive to other treatments. Major risk factors for post-HT AKI include pre-existing renal impairment, ischemia susceptibility, venous congestion, and nephrotoxic medication exposure[5]. Patients with AKI post heart transplantation experience longer hospital stays, amounting to greater financial burden. In addition, complications of AKI can have deleterious effects on the outcomes of cardiac transplant, resulting in increased in-hospital and one-year mortality[6]. Greater rates of cardiac, neurological and serious infectious morbidity have also been observed in cardiac transplant patients who develop AKI[7,8]. Epidemiologically, heart transplantation shares similarities with AKI, with global data indicating approximately 20000 procedures annually, though in Pakistan, the procedure remains limited due to resource constraints. AKI in HT patients leads to prolonged hospital stays, increased financial burden, and higher in-hospital and one-year mortality, alongside elevated cardiac, neurological, and infectious morbidity.
Several observational studies analyzing the risk factors for AKI in cardiac transplant patients have been done over the years. However, a comprehensive synthesis of this evidence in a meta-analysis has not been done so far, which would allow for the statistical analysis of the predictors of AKI, thereby making it possible to risk-stratify patients. Risk stratification of patients using predictors of AKI can potentially reduce AKI-related morbidity and mortality in cardiac transplantation patients.
Thus, we conducted a comprehensive meta-analysis to identify risk factors associated with AKI in post-heart transplantation patients. This research aims to enhance clinical decision-making through improved risk stratification and inform future studies on preventive strategies and targeted interventions to mitigate AKI-related complications in this high-risk population.
This meta-analysis was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines[9,10]. The protocol is registered with the International Prospective Register of Systematic Reviews under the identifier CR. Ethical approval was not necessary for this study since it exclusively utilized publicly available data.
Electronic searches were conducted on MEDLINE (via PubMed), Google Scholar, Science Direct, ClinicalTrails.gov and Cochrane databases from inception up till September 1, 2024, to identify studies that discussed the risk factors of AKI in heart transplant patients. To maximize sensitivity, we used these words as keywords: “Acute Kidney Injury” AND “Heart Transplantation” AND “Risk Factors”. Additionally, the retrieved articles’ reference lists were reviewed for further possibly relevant research articles to be found in accordance with the selection criteria. The detailed search string is available in Supplementary Table 1.
The articles were assessed and selected based on the following inclusion criteria: (1) Only Randomized Controlled trials, Clinical Trials, Retrospective Cohort Studies, Observational studies were included; (2) Patients who had undergone heart transplantation and developed Acute kidney disease afterwards; and (3) Studies who compared AKI group with a non-AKI group after heart transplantation. Only full-text articles were included. Letter to editors, editorials, correspondences, case series, case reports were excluded. Any study involving healthy individuals as a population or included animals, was excluded from our study. Studies published in language other than English were excluded. Additionally, we did not include any preprint or unpublished data.
All the selected articles were uploaded on Zotero for further screening and were investigated by three independent reviewers (Shahzad M, Sehar A, and Farooq H) for duplications. All discrepancies between the three were resolved by discussion with the fourth independent reviewer (Khawar M). Data were extracted using the tables, figures, and texts of the retrieved articles.
We enlisted all the potential risk factors described in the included articles. Additionally, risk factors were categorized into several groups: These Risk factors include:
Demographics: (1) Recipient age; (2) Recipient body mass index (BMI); (3) Recipient's sex; and (4) Donor sex.
Co-morbidities: (1) Diabetes; (2) Hypertension; (3) Smoking; (4) Coronary artery disease; (5) Peripheral artery disease; (6) Chronic kidney disease (CKD); (7) COPD; (8) Dilated cardiomyopathy; (9) Valvular disease; and (10) Previous thoracic surgery.
Intraoperative parameters: (1) Cardiopulmonary bypass time (minutes); (2) Ischemic time (minutes), (3) Mechanical ventilation (duration), (4) Intra-aortic balloon pump; (5) LVAD implantation; (6) Extracorporeal membrane oxygenation; and (7) Inotropes.
We presented dichotomous outcomes as odds ratios (OR) and continuous outcomes as mean difference (MD) associated with corresponding 95% confidence intervals (CI). The inter-study heterogeneity was dealt by a random effect model using Mantel-Haenszel method for dichotomous outcomes and Inverse Variance method for continuous outcomes. The heterogeneity among the studies was assessed by I2 and X2 statistics (I2 values < 50% = low heterogeneity; I2 values 50%-75% = moderate heterogeneity; I2 values > 75% = significant heterogeneity). Sensitivity analysis was conducted to evaluate the influence of individual studies on the pooled effect size. All statistical calculations were performed using the meta-analysis software Review Manager 5.4.1 (The Cochrane Collaboration, Copenhagen, Denmark). A P value of < 0.050 represented statistical significance. Sensitivity analysis was conducted to evaluate the influence of individual studies on the pooled effect size.
The Newcastle-Ottawa Scale (NOS) was employed to evaluate the methodological rigor of the included cohort studies. The NOS assesses study quality across three domains: Selection (4 items), comparability (1 item), and outcome assess
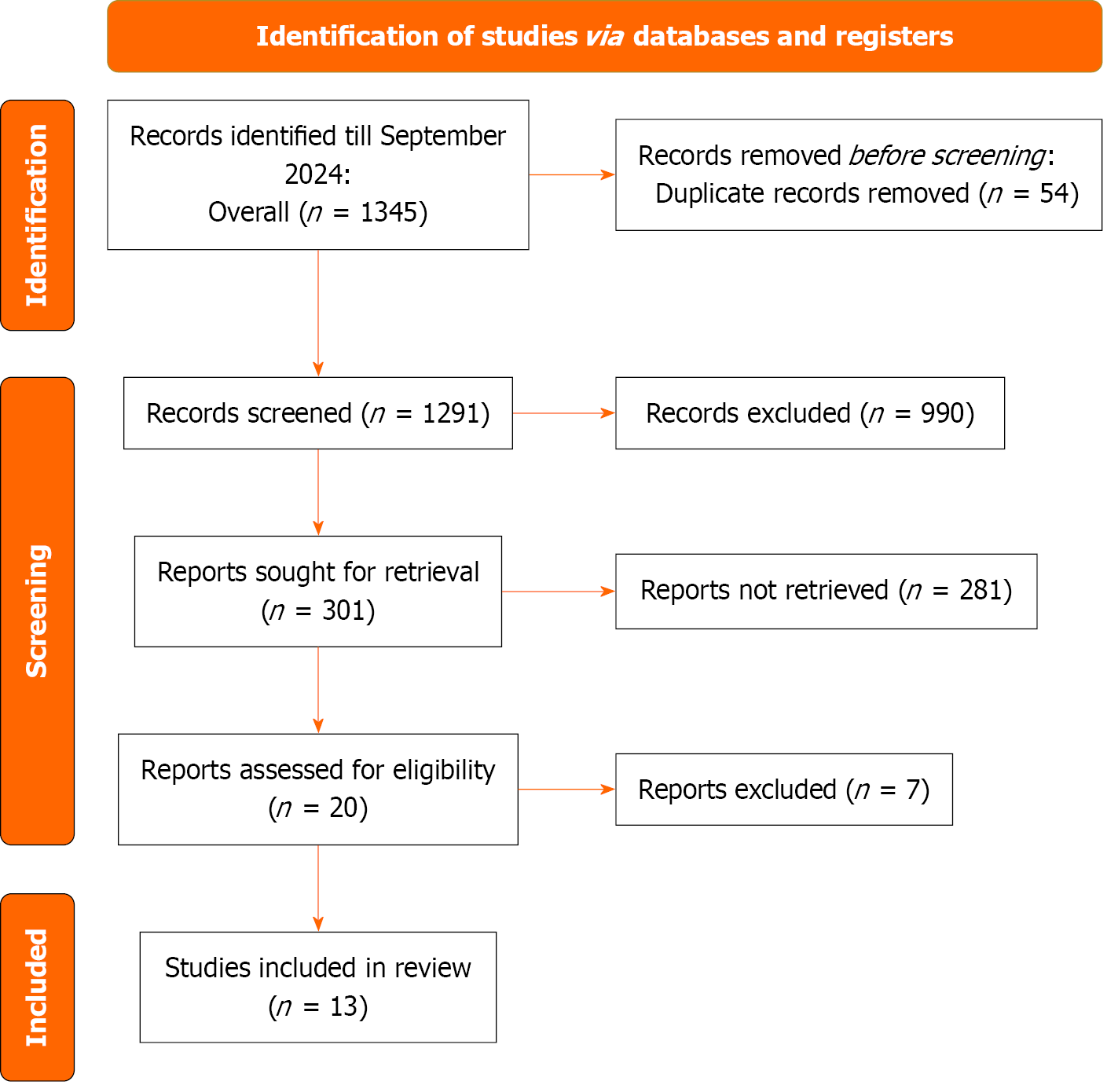
Figure 1 shows the PRISMA flowchart. The initial database search yielded a total of 1345 articles out of which 1291 were assessed for eligibility-based titles and abstracts after deduplication. The full texts of 20 articles were assessed for eligibility using the inclusion criteria, out of which 13[6,7,11-21] studies were included in this meta-analysis.
A total of 13 studies, published between 2006 and 2024 were included in the analysis. All the studies included were retrospective cohort studies. A total of 3330 patients were included in this review, which were subdivided into an AKI group and a non-AKI group. A total of 1376 patients were allocated to the AKI group and 1954 patients in the no AKI group. Detailed characteristics of each study can be found in Table 1.
| Ref. | Study design | Sample size | Age | ||
| AKI | No AKI | AKI mean (SD) | No AKI mean (SD) | ||
| Boyle et al[7], 2006 | Retrospective Cohort Study | 44 | 712 | 58.2 (9.50) | 56.23 (9.66) |
| Fortrie et al[11], 2015 | Retrospective Cohort Study | 405 | 126 | 50.05 (10.7) | 50.33 (7.50) |
| García-Gigorro et al[12], 2018 | Retrospective Cohort Study | 125 | 185 | 52.33 (10.50) | 50.67 (14.20) |
| Gude et al[13], 2010 | Retrospective Cohort Study | 145 | 440 | 52 (11) | 49 (12) |
| Hariri et al[14], 2024 | retrospective cohort study | 134 | 75 | 51.33 (13.49) | 52.67 (4.54) |
| Jahangirifard et al[15], 2021 | Retrospective Cohort Study | 74 | 52 | 44 (3.5) | 37 (4.1) |
| Jiang et al[16], 2020 | Retrospective Cohort Study | 33 | 62 | 55.12 (12.02) | 53.87 (11.94) |
| Jocher et al[6], 2021 | Retrospective Cohort Study | 145 | 83 | 55.67 (11.32) | 56 (11.32) |
| M‘Pembele et al[17], 2021 | Retrospective Cohort Study | 49 | 58 | 53 (11) | 51 (13) |
| Nadziakiewicz et al[18], 2020 | Retrospective Cohort Study | 7 | 32 | 46.7 ( 9.8) | 48.9 (10.5) |
| Tjahjono et al[19], 2016 | Retrospective Cohort Study | 65 | 46 | 49 (11) | 47 (13) |
| Türker et al[20], 2013 | Retrospective Cohort Study | 27 | 17 | 37.9 (15.6) | 24.6 (15.0) |
| Welz et al[21], 2024 | Retrospective Cohort Study | 123 | 66 | 49.13 (11.75) | 45.98 (12.89) |
Based on the NOS quality assessment, most studies demonstrated good methodological quality. Of the 12 studies evaluated, 2 scored 9 stars, 6 scored 8 stars, and 2 scored 7 stars, all classified as Good quality. The remaining 2 studies scored 6 stars, rated as Fair quality, indicating minor methodological deficiencies. No studies were classified as Poor quality. The highest score of 9 stars, achieved by two studies, signifies robust methodological rigor (Table 2).
| Ref. | Selection | Comparability | Outcome | Total | |||||
| 1 | 2 | 3 | 4 | 1 | 1 | 2 | 3 | ||
| Boyle et al[7], 2006 | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 8 |
| Fortrie et al[11], 2015 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9 |
| García-Gigorro et al[12], 2018 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | 8 | |
| Gude et al[13], 2010 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9 |
| Hariri et al[14], 2024 | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 8 |
| Jahangirifard et al[15], 2021 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | 8 | |
| Jiang et al[16], 2020 | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 7 | |
| Jocher et al[6], 2021 | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 7 | |
| M‘Pembele et al[17], 2021 | ★ | ★ | ★ | ★ | ★ | ★ | 6 | ||
| Nadziakiewicz et al[18], 2020 | ★ | ★ | ★ | ★ | ★ | ★ | 6 | ||
| Tjahjono et al[19], 2016 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | 8 | |
| Türker et al[20], 2013 | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 8 |
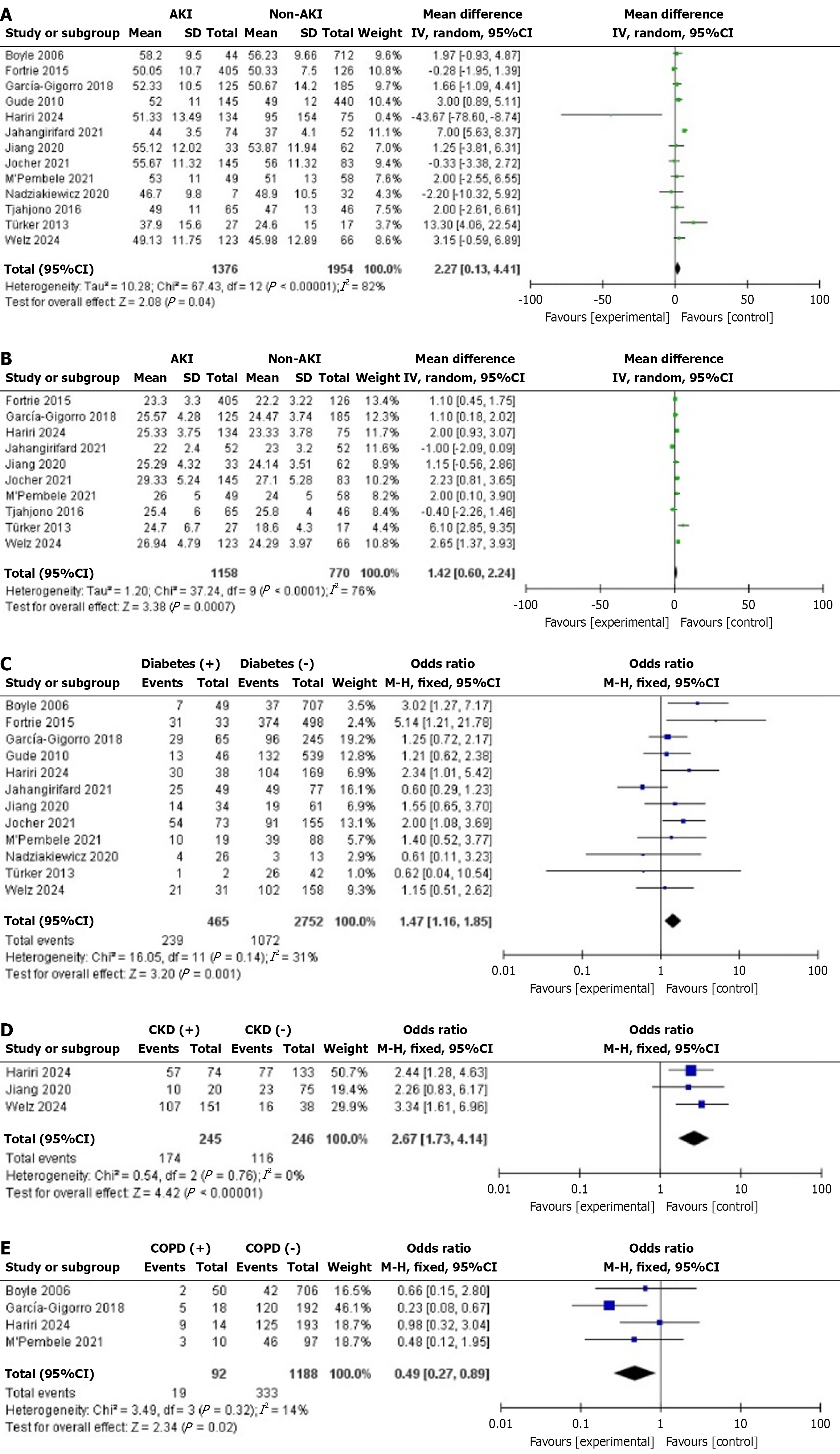
Demographics related risk factors: Recipient age: All 13 studies identified age as a risk factor. The MD was 2.27 years (95%CI: 0.13 to 4.41, P = 0.04), indicating individuals in the AKI group were older. Substantial heterogeneity (I² = 82%) dropped to 35% after excluding two studies[15,20] (Figure 2A).
Recipient BMI: Ten studies showed BMI as a risk factor. MD was 1.42 (95%CI: 0.60 to 2.24, P = 0.0007, I² = 76%). When Jahangirifard et al[15] and Türker et al[20] study were excluded, I² dropped to 39% which was analyzed through sensitivity analysis (Figure 2B).
Co-morbidities: Diabetes: Twelve studies identified diabetes as a significant risk factor [OR: 1.47, 95%CI: 1.16 to 1.85, P = 0.001]. Heterogeneity was low (I² = 31%) (Figure 2C).
CKD: Three studies showed CKD as a significant risk factor (OR: 2.67, 95%CI: 1.73 to 4.14, P = 0.0001). Heterogeneity was minimal (I² = 0%) (Figure 2D).
COPD: Four studies showed COPD as a potential risk factor (OR: 0.49, 95%CI: 0.27 to 0.89, P = 0.02). Low heterogeneity (I² = 14%) (Figure 2E).
Recipients’ male sex: Twelve studies showed no significant association (OR: 1.07, 95%CI: 0.87 to 1.31, P = 0.55). Heterogeneity was low (I² = 40%) (Supplementary Figure 1).
Donor sex: Three studies found no significant association (OR: 0.82, 95%CI: 0.65 to 1.05, P = 0.11). Heterogeneity was absent (I² = 0%) (Supplementary Figure 2).
Hypertension: Nine studies showed no significant association (OR: 1.38, 95%CI: 0.91 to 2.10, P = 0.13). Moderate heterogeneity (I² = 56%) reduced to 44% after excluding one study (Supplementary Figure 3).
Smoking: Three studies found no significant association (OR: 1.42, 95%CI: 0.83 to 2.40, P = 0.20). Heterogeneity was low (I² = 45%) (Supplementary Figure 4).
Coronary artery disease: Seven studies showed no significant association (OR: 1.01, 95%CI: 0.81 to 1.27, P = 0.93). Moderate heterogeneity (I² = 49%) (Supplementary Figure 5).
Peripheral artery disease: Two studies found no significant association (OR: 1.17, 95%CI: 0.32 to 4.34, P = 0.81). High heterogeneity (I² = 77%) (Supplementary Figure 6).
Dilated cardiomyopathy: Six studies found no significant association (OR: 0.95, 95%CI: 0.63 to 1.42, P = 0.79). Moderate heterogeneity (I² = 59%) dropped to 32% after removing Jahangirifard et al[15] study (Supplementary Figure 7).
Valvular disease: Four studies found no significant association (OR: 1.41, 95%CI: 0.80 to 2.50, P = 0.24). Low heterogeneity (I² = 35%) (Supplementary Figure 8).
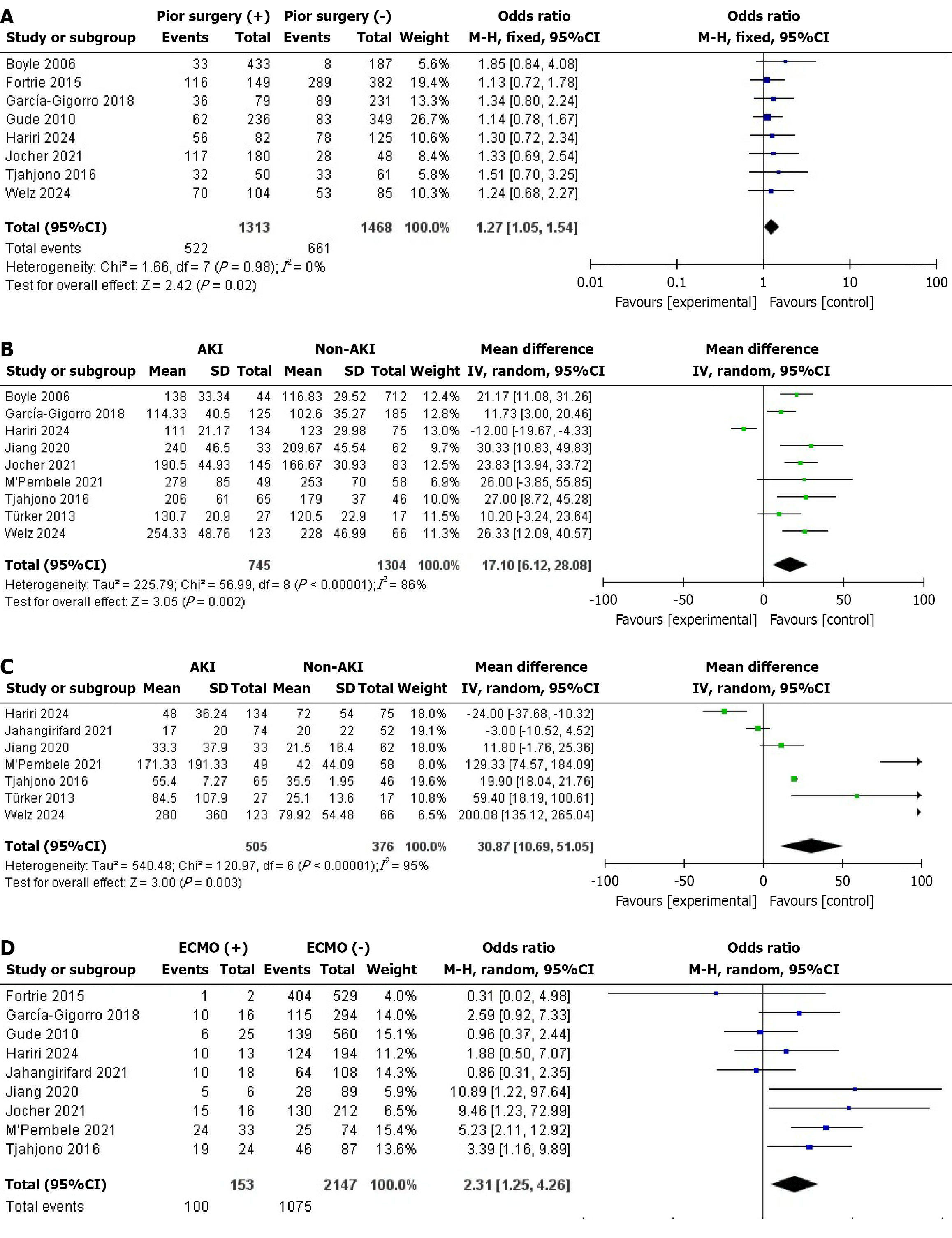
Previous thoracic surgery: Eight studies showed prior thoracic surgery as a significant risk factor (OR: 1.27, 95%CI: 1.05 to 1.54, P = 0.02). No heterogeneity (I² = 0%) (Figure 3A).
Intraoperative parameters: Cardiopulmonary bypass time (minutes): Data from nine studies showed a significant MD of 17.10 minutes [95%CI: (6.12 to 28.08), P = 0.002], indicating longer bypass times in individuals who developed AKI. High heterogeneity (I² = 86%) dropped to 19% after excluding the Hariri et al[14] study (Figure 3B).
Mechanical ventilation (duration): Analysis of seven studies found a significant MD of 30.87 hours [95%CI: (10.69 to 51.05), P = 0.003], with prolonged ventilation linked to AKI. Heterogeneity was very high (I² = 95%) but decreased to 85% after excluding the Hariri et al[14], Jahangirifard et al[15], and Welz et al[21] studies (Figure 3C).
Extracorporeal membrane oxygenation: Nine studies indicated a significant OR of 2.31 [95%CI: (1.25 to 4.26), P = 0.008], associating ECMO with AKI. Moderate heterogeneity (I² = 52%) dropped to 45% upon excluding the Jahangirifard et al[15] study (Figure 3D).
Ischemic time (minutes): Data from eleven studies showed a nonsignificant MD of 10.57 minutes [95%CI: (−0.27 to 21.41), P = 0.06] for AKI, with high heterogeneity (I² = 82%) that dropped to 21% upon excluding Hariri et al[14] and Jahangirifard et al[15] (Supplementary Figure 9).
Intra-aortic balloon pump: Seven studies yielded a nonsignificant OR of 1.64 [95%CI: (0.85 to 3.16), P = 0.14] for IABP use and AKI. Moderate heterogeneity (I² = 68%) reduced to 48% when the Boyle et al[7] study was excluded (Supplemen
LVAD implantation: Nine studies showed no significant association between LVAD use and AKI [OR: 1.03, 95%CI: (0.78 to 1.36), P = 0.83] with no heterogeneity (I² = 0%) (Supplementary Figure 11).
Inotropes: Four studies showed a nonsignificant OR of 1.08 [95%CI: (0.65 to 1.79), P = 0.78] for inotrope use and AKI. Moderate heterogeneity (I² = 71%) dropped to 0% when the García-Gigorro et al[12] study was excluded (Supplementary Figure 12).
This meta-analysis identified the various demographical, preoperative, and intraoperative risk factors for developing AKI in patients after heart transplantation. Among the patients developing AKI, Age and BMI were significantly higher as compared to those who did not develop AKI. Furthermore, comorbidities such as diabetes, CKD, and previous thoracic surgery served as risk factors for developing AKI post heart transplant surgery. However, patients with hypertension, smoking history, coronary artery disease, peripheral artery disease, dilated cardiomyopathy, and valvular disease did not have a statistically significant risk of developing AKI after heart transplantation. Patients who had a higher cardiopulmonary bypass time, and mechanical ventilation time intra-operatively were more likely to develop AKI post heart transplant. Furthermore, the pooled results showed that patients who had an LVAD implantation and were given inotropes during the surgery did not have a statistically significant risk of developing AKI post heart transplant.
Regarding donor age, previous literature has established a relationship with AKI occurrence, contrary to the implication that this association is unclear. A retrospective cohort study utilizing the United Network for Organ Sharing heart transplant database reported that donors aged 50 years or older were associated with a higher risk of developing chronic allograft vasculopathy, which is a major cause of mortality after heart transplant[22]. Additionally, a multicenter study of 1423 heart transplant recipients found that older donor age (≥ 40 years) was independently associated with an increased risk of postoperative AKI, potentially due to reduced renal reserve in older donor organs. This suggests that donor age is a significant factor in the development of AKI, likely due to its impact on graft quality and renal function post-transplantation. We identified BMI as a risk factor for developing AKI and our results are in accordance with the relevant literature. A higher BMI with dyslipidemia and diabetes are known risk factors for developing AKI post cardiac transplant operation[23]. An analysis of 468 critically ill patients in the intensive care unit reported that overweight patients had a significantly higher risk of developing AKI[24]. An observational study of more than 8000 patients who underwent cardiac surgery reported that around 36.5% and 46% of patients who developed AKI were overweight and obese, respectively[25]. Furthermore, patients having a higher BMI had a poorer survival[25].
We found out that pre-existing diabetes mellitus (DM) is significantly associated with the development of AKI after heart transplant. Patients with diabetes are more likely to develop AKI[26]. A retrospective cohort study of 4325 patients reported that the incidence and severity of AKI was higher in patients undergoing coronary artery bypass grafting who had DM as compared to patients who did not have DM[27]. A cohort study of more than 3000 patients undergoing heart transplant reported that pre-existing insulin-dependent DM in patients at the time of surgery is a risk factor for the development of AKI[28]. However, another cohort study presented evidence that patients having diabetes had a statistically non-significant association with the development of AKI after cardiac surgery[29].
LVAD implantation significantly increased the risk of development of AKI post heart transplant. In a retrospective cohort study of 138 patients who underwent LVAD implantation, 35 patients developed AKI, and the right ventricular failure was significantly associated with the development of AKI[30]. Another retrospective cohort study on 241 patients who underwent LVAD implantation reported the development of AKI in 169 patients[31]. Patients who underwent LVAD implantation and subsequently developed moderate to severe AKI had a higher rate of respiratory failure and death as compared to patients who developed mild or no AKI[32]. Our meta-analysis identified post-operative inotrope use as a significant predictor for development of AKI. A retrospective cohort study suggested the development of AKI in patients receiving inotropes after cardiac surgery[33]. Another cohort study on 1326 patients reported that mortality and renal dysfunction was independently associated with inotrope exposure after adjusting for differences in left ventricular ejection fraction, Parsonnet score, perioperative balloon counter pulsation, the need for reoperation, and cardiopulmonary bypass time[34]. We identified that preoperative eGFR levels are not a strong risk factor for predicting the development of AKI after heart transplant. An observational study of 184 adults who underwent heart transplant reported that preoperative eGFR was not associated with the development of AKI[35].
While our meta-analysis provides a comprehensive assessment of risk factors associated with AKI post heart transplant, several limitations should be considered when interpreting the findings.
The inclusion of only English-language published works may have introduced publication bias, potentially excluding relevant studies published in other languages or unpublished data that could influence the pooled results.
The inclusion of only observational studies contributed to heterogeneity in the pooled results. Although sensitivity analysis and a random-effects model were used to mitigate this, variability in study populations, definitions of AKI, and data collection methods may limit the generalizability of our findings.
The reliance on observational studies, which are prone to confounding and selection bias, may affect the robustness of our conclusions. The lack of randomized controlled trials in this field further restricts the ability to establish causality between identified risk factors and AKI development.
To advance the understanding of AKI risk factors in heart transplantation, future research should focus on several key areas. First, longitudinal studies are needed to further elucidate the mechanisms by which donor age influences AKI development, particularly the role of renal senescence and its interaction with recipient factors. Second, randomized controlled trials could explore interventions to mitigate AKI risk in high-BMI patients, such as optimized perioperative weight management or targeted anti-inflammatory therapies. Additionally, investigating the impact of novel inotrope regimens or alternative hemodynamic support strategies on AKI incidence could provide insights into safer perioperative management. Finally, integrating machine learning models to predict AKI risk based on a combination of donor, recipient, and intraoperative factors may enhance personalized risk stratification and guide clinical decision-making.
In conclusion, AKI is a potential complication after heart transplant surgery and various patient demographics and comorbidities including intraoperative, perioperative, and postoperative interventions might contribute to the develop
| 1. | Goyal A, Daneshpajouhnejad P, Hashmi MF, Bashir K. Acute Kidney Injury. 2023 Nov 25. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. [PubMed] |
| 2. | Zhou J, Zhang X, Lyu L, Ma X, Miao G, Chu H. Modifiable risk factors of acute kidney injury after liver transplantation: a systematic review and meta-analysis. BMC Nephrol. 2021;22:149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 3. | Susantitaphong P, Cruz DN, Cerda J, Abulfaraj M, Alqahtani F, Koulouridis I, Jaber BL; Acute Kidney Injury Advisory Group of the American Society of Nephrology. World incidence of AKI: a meta-analysis. Clin J Am Soc Nephrol. 2013;8:1482-1493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 972] [Cited by in RCA: 1097] [Article Influence: 84.4] [Reference Citation Analysis (0)] |
| 4. | Alba AC, E Bain, Ng N, Stein M, O'Brien K, Foroutan F, Ross H. Complications after Heart Transplantation: Hope for the Best, but Prepare for the Worst. Int J Transplant Res Med. 2016;2. [DOI] [Full Text] |
| 5. | Gale D, Al-Soufi S, MacDonald P, Nair P. Severe Acute Kidney Injury Postheart Transplantation: Analysis of Risk Factors. Transplant Direct. 2024;10:e1585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 6. | Jocher BM, Schilling JD, Fischer I, Nakajima T, Wan F, Tanaka Y, Ewald GA, Kutkar K, Masood M, Itoh A. Acute kidney injury post-heart transplant: An analysis of peri-operative risk factors. Clin Transplant. 2021;35:e14296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 7. | Boyle JM, Moualla S, Arrigain S, Worley S, Bakri MH, Starling RC, Heyka R, Thakar CV. Risks and outcomes of acute kidney injury requiring dialysis after cardiac transplantation. Am J Kidney Dis. 2006;48:787-796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 97] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 8. | Ronco C, Bellomo R, Kellum JA. Acute kidney injury. Lancet. 2019;394:1949-1964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 633] [Cited by in RCA: 1321] [Article Influence: 188.7] [Reference Citation Analysis (0)] |
| 9. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44932] [Cited by in RCA: 51767] [Article Influence: 10353.4] [Reference Citation Analysis (2)] |
| 10. | Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tungwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Ottawa Hospital Research Institute, 2000. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. |
| 11. | Fortrie G, Manintveld OC, Caliskan K, Bekkers JA, Betjes MG. Acute Kidney Injury as a Complication of Cardiac Transplantation: Incidence, Risk Factors, and Impact on 1-year Mortality and Renal Function. Transplantation. 2016;100:1740-1749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 61] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 12. | García-Gigorro R, Renes-Carreño E, Corres Peiretti MA, Arribas López P, Perez Vela JL, Gutierrez Rodríguez J, Delgado JF, Cortina Romero JM, Montejo González JC. Incidence, Risk Factors and Outcomes of Early Acute Kidney Injury After Heart Transplantation: An 18-year Experience. Transplantation. 2018;102:1901-1908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 13. | Gude E, Andreassen AK, Arora S, Gullestad L, Grov I, Hartmann A, Leivestad T, Fiane AE, Geiran OR, Vardal M, Simonsen S. Acute renal failure early after heart transplantation: risk factors and clinical consequences. Clin Transplant. 2010;24:E207-E213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 14. | Hariri G, Henocq P, Coutance G, Mansouri S, Tohme J, Guillemin J, Varnous S, Dureau P, Duceau B, Leprince P, Dechartres A, Bouglé A. Perioperative Risk Factors of Acute Kidney Injury After Heart Transplantation and One-Year Clinical Outcomes: A Retrospective Cohort Study. J Cardiothorac Vasc Anesth. 2024;38:1514-1523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Jahangirifard A, Ahmadi ZH, Khalili N, Naghashzadeh F, Afshar A, Amiri A, Dalili N. Early post-operative acute kidney injury after cardiac transplantation: Incidence and predictive factors. Clin Transplant. 2021;35:e14420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 16. | Jiang YY, Kong XR, Xue FL, Chen HL, Zhou W, Chai JW, Wu F, Jiang SS, Li ZL, Wang K. Incidence, risk factors and clinical outcomes of acute kidney injury after heart transplantation: a retrospective single center study. J Cardiothorac Surg. 2020;15:302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | M'Pembele R, Roth S, Stroda A, Lurati Buse G, Sixt SU, Westenfeld R, Polzin A, Rellecke P, Tudorache I, Hollmann MW, Aubin H, Akhyari P, Lichtenberg A, Huhn R, Boeken U. Risk Factors for Acute Kidney Injury Requiring Renal Replacement Therapy after Orthotopic Heart Transplantation in Patients with Preserved Renal Function. J Clin Med. 2021;10:4117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Nadziakiewicz P, Grochla M, Krauchuk A, Szyguła-Jurkiewicz B, Cymerys M, Zembala MO, Przybyłowski P. Prognostic Value of Creatinine Concentration and Glomerular Filtration Rate in Acute Kidney Injury Development in the Early Postoperative Period After Heart Transplantation. Transplant Proc. 2020;52:2091-2093. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 19. | Tjahjono R, Connellan M, Granger E. Predictors of Acute Kidney Injury in Cardiac Transplantation. Transplant Proc. 2016;48:167-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Türker M, Zeyneloglu P, Sezgin A, Pirat A, Arslan G. RIFLE criteria for acute kidney dysfunction following heart transplantation: incidence and risk factors. Transplant Proc. 2013;45:3534-3537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 21. | Welz F, Schoenrath F, Friedrich A, Wloch A, Stein J, Hennig F, Ott SC, O'Brien B, Falk V, Knosalla C, Just IA. Acute Kidney Injury After Heart Transplantation: Risk Factors and Clinical Outcomes. J Cardiothorac Vasc Anesth. 2024;38:1150-1160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 22. | Nagji AS, Hranjec T, Swenson BR, Kern JA, Bergin JD, Jones DR, Kron IL, Lau CL, Ailawadi G. Donor age is associated with chronic allograft vasculopathy after adult heart transplantation: implications for donor allocation. Ann Thorac Surg. 2010;90:168-175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 83] [Cited by in RCA: 83] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 23. | Zhu S, Qiao W, Wang Y, Zhou Y, Xu Y, Wang S, Xia T, Wang G, Chen S, Shi J, Dong N. A contemporary simple risk score for prediction of severe acute kidney injury after heart transplantation. ESC Heart Fail. 2025;12:1166-1175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 24. | Ju S, Lee TW, Yoo JW, Lee SJ, Cho YJ, Jeong YY, Lee JD, Kim JY, Lee GD, Kim HC. Body Mass Index as a Predictor of Acute Kidney Injury in Critically Ill Patients: A Retrospective Single-Center Study. Tuberc Respir Dis (Seoul). 2018;81:311-318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 25. | Zou Z, Zhuang Y, Liu L, Shen B, Xu J, Luo Z, Teng J, Wang C, Ding X. Role of Body Mass Index in Acute Kidney Injury Patients after Cardiac Surgery. Cardiorenal Med. 2017;8:9-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Kaur A, Sharma GS, Kumbala DR. Acute kidney injury in diabetic patients: A narrative review. Medicine (Baltimore). 2023;102:e33888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 26] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 27. | Wang R, Zhang H, Zhu Y, Chen W, Chen X. The impact of diabetes mellitus on acute kidney injury after coronary artery bypass grafting. J Cardiothorac Surg. 2020;15:289. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 28. | Wang L, Wang T, Rushton SN, Parry G, Dark JH, Sheerin NS. The impact of severe acute kidney injury requiring renal replacement therapy on survival and renal function of heart transplant recipients - a UK cohort study. Transpl Int. 2020;33:1650-1666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Moschopoulou M, Ampatzidou FC, Loutradis C, Boutou A, Koutsogiannidis CP, Drosos GE, Sarafidis PA. Diabetes mellitus does not affect the incidence of acute kidney injury after cardiac surgery; a nested case-control study. J Nephrol. 2016;29:835-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 30. | Gündüz E. Acute kidney injury early after left ventricular assist device implantation: incidence, risk factors and clinical consequences. Eur Rev Med Pharmacol Sci. 2023;27:3336-3343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 31. | Muslem R, Caliskan K, Akin S, Sharma K, Gilotra NA, Constantinescu AA, Houston B, Whitman G, Tedford RJ, Hesselink DA, Bogers AJJC, Russell SD, Manintveld OC. Acute kidney injury and 1-year mortality after left ventricular assist device implantation. J Heart Lung Transplant. 2018;37:116-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 32. | Harmon DM, Tecson KM, Lima B, Collier JDG, Shaikh AF, Still S, Baxter RD, Lew N, Thakur R, Felius J, Hall SA, Gonzalez-Stawinski GV, Joseph SM. Outcomes of Moderate-to-Severe Acute Kidney Injury following Left Ventricular Assist Device Implantation. Cardiorenal Med. 2019;9:100-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 33. | Hernández-leiva E, Hernández-huertas F. The use of inotropes and not hyperchloremia is an independent risk factor for acute kidney injury during the postoperative period of cardiac surgery. A prospective cohort-study. Int J Surg Open. 2022;45:100507. [RCA] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 34. | Shahin J, DeVarennes B, Tse CW, Amarica DA, Dial S. The relationship between inotrope exposure, six-hour postoperative physiological variables, hospital mortality and renal dysfunction in patients undergoing cardiac surgery. Crit Care. 2011;15:R162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 73] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 35. | Bianco JC, Stang MV, Denault AY, Marenchino RG, Belziti CA, Musso CG. Acute Kidney Injury After Heart Transplant: The Importance of Pulmonary Hypertension. J Cardiothorac Vasc Anesth. 2021;35:2052-2062. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/