Published online Sep 25, 2025. doi: 10.5527/wjn.v14.i3.108703
Revised: June 17, 2025
Accepted: July 31, 2025
Published online: September 25, 2025
Processing time: 147 Days and 20.2 Hours
Renal cysts, especially the cortical type, are a prevalent renal pathology. Most cases are asymptomatic and detected incidentally during abdominal imaging examination for unrelated complaints. They are often benign, but they can rarely transform into cystic renal malignancies. When huge or complicated, especially with an abscess, it may become symptomatic from the renal capsular stretch or inflammation. The open surgical, endoscopic, laparoscopic, and robotic appro
This is a 26-year-old housewife who was referred to the urology outpatient clinic with a history of left flank pain and swelling for 5 months, with the transabdo
Treatment of giant simple renal cortical cyst abscesses should be individualized depending on the pathology in question, the surgeon’s experience, patient preference and availability of facilities for endoscopic, laparoscopic or robotic modalities. Notwithstanding open surgical exploration, cyst unroofing and marsupialization are useful modalities in giant renal cortical cyst abscesses and are associated with patient satisfaction.
Core Tip: Giant renal cyst abscesses are uncommon but potentially serious complications of an infected renal cyst. They often pose a diagnostic and therapeutic challenge because of their atypical presentation and potential risk for serious complications. The treatment of a renal cyst abscess entails a multimodal strategy that includes precise diagnosis, antibiotic treatments, drainage techniques, and occasionally surgery. These surgical principles guided the patient’s treatment. Notwithstanding, the choice of open surgical intervention was primarily influenced by the patient’s preference after detailed counselling on the relative size of the cyst abscess, lack of insurance cover for services payment, concerns about the possibility of recurrence after percutaneous drainage under ultrasound or computed tomography guidance, surgeon’s experience and vis-à-vis the feasibility of laparoscopic and robotic interventions.
- Citation: Khalid A, Yakubu KB, Umar AM, Aljannare BG, Aminu NA, Obadele OG, Abdulwahab-Ahmed A. Uncommon presentation and management of a giant renal cyst abscess: A case report. World J Nephrol 2025; 14(3): 108703
- URL: https://www.wjgnet.com/2220-6124/full/v14/i3/108703.htm
- DOI: https://dx.doi.org/10.5527/wjn.v14.i3.108703
Renal masses are a relatively common pathology of the kidney, which may be benign or malignant. A renal cyst is one of the benign differential diagnoses of a renal mass, accounting for 8.5% of inpatient renal surgical admissions[1]. Their location within the kidney can be medullary or cortical. The benign cortical types are prevalent, affecting over half of the population above fifty years of age[2]. They constitute a remarkable financial and workload burden on radiological and urological services at a certain health facility[3]. Most cases are asymptomatic and detected incidentally during abdominal imaging examination for unrelated complaints[4,5]. Though generally benign, they may rarely undergo malignant transformation[6]. While the majority of renal cysts are asymptomatic, some can become infected, leading to renal cyst abscess formation. A renal cyst abscess develops when a simple or complex renal cyst becomes infected with subsequent suppuration and development of systemic symptoms such as fever and flank pain.
Because of the potential risk for serious complications such as urosepsis, formation of perinephric abscess and renal dysfunction, early diagnosis and treatment are desirable. The presentation of a giant renal cyst abscess may mimic other renal and intraabdominal pathologies; therefore, the diagnosis may be challenging. This involves using a combination of clinical, laboratory and radiological findings and rarely, the diagnosis may be done intraoperative[7,8]. The treatment generally involves the combination of antibiotic therapy and drainage of the abscess using various approaches. Surgical drainage is an important component of the treatment to avoid the associated morbidity and mortality of this serious infection[9]. This can be achieved percutaneously under ultrasound or computerized tomographic scan guidance or with open surgical, laparoscopic, or robotic approaches, depending on the cyst characteristics, presence of symptoms, surgeon’s expertise and experience and availability of facilities for a minimally invasive procedure. The common indications for surgical treatment of a simple renal cyst include pain due to the pressure effect or when it becomes infected with abscess formation. This manuscript reports a case of a giant left renal cyst abscess in a woman, providing a comprehensive discussion on the clinical presentation, diagnostic approach, and management strategies. The report aims to raise clinical awareness and improve outcomes for patients with this rare but potentially life-threatening condition.
This is a 26-year-old housewife, gravida 2, Para 2, currently not pregnant, who was referred to the urology outpatient clinic with a history of left flank pain and swelling for 5 months.
She was relatively well until five months before presentation when her attention was drawn to a painful left flank swelling shortly after a spontaneous vaginal delivery at a secondary health facility. The swelling increased progressively in size with worsening pain, which hindered her respiratory excursions. She had associated anorexia, weight loss, nausea, and intermittent fever, which on one occasion was severe and high-grade with chills and rigors. This warranted hospital admission, analgesics, antipyretic, and antibiotic therapy with resolution of fever. There were no associated lower urinary tract symptoms, chronic cough or contact with a chronically coughing individual, drenching night sweating, or ingestion of unpasteurized cow milk. She had no history to suggest the presence of hypertension, diabetes mellitus, retroviral disease, haemoglobinopathies, or the use of immunosuppressant medications. There was no traditional or orthodox preadmission intervention such as cyst aspiration or incision and drainage.
She had a transabdominal ultrasound before her last pregnancy, which confirmed a simple left renal cortical cyst for which a non-operative management was offered. The antenatal period was eventful, characterized by repeated hospitalization owing to recurrent episodes of vague abdominal pain and febrile illness treated with antimalarial medications, antibiotics, and analgesics. She had no information regarding the state of the left cortical renal cyst despite some antenatal transabdominal ultrasound scans being done on her.
There was no remarkable past surgical history.
There was no associated history of diabetes mellitus, hypertension, cystic renal disease, haemoglobinopathies or other remarkable histories among family members.
The physical examination was unremarkable at presentation. Her vital signs were stable with temperature, respiratory rate, pulse rate, and blood pressure of 36.8 °C, 20 cycles/minute, 88 beats/minute, and 110/70 mmHg, respectively. The abdomen was full and moved with respiration. There was an obvious left lumbar swelling which was ballotable, cystic, and tender. The digital rectal and other systemic examinations were unremarkable.
Blood investigations revealed leukocytosis (13.4 × 109/L) with neutrophilia (80.3%). Her packed cell volume, platelet count and electrolytes, urea and creatinine were within the normal range. Urinalysis was normal, but urine culture yielded Escherichia coli (E. coli) sensitive to levofloxacin.
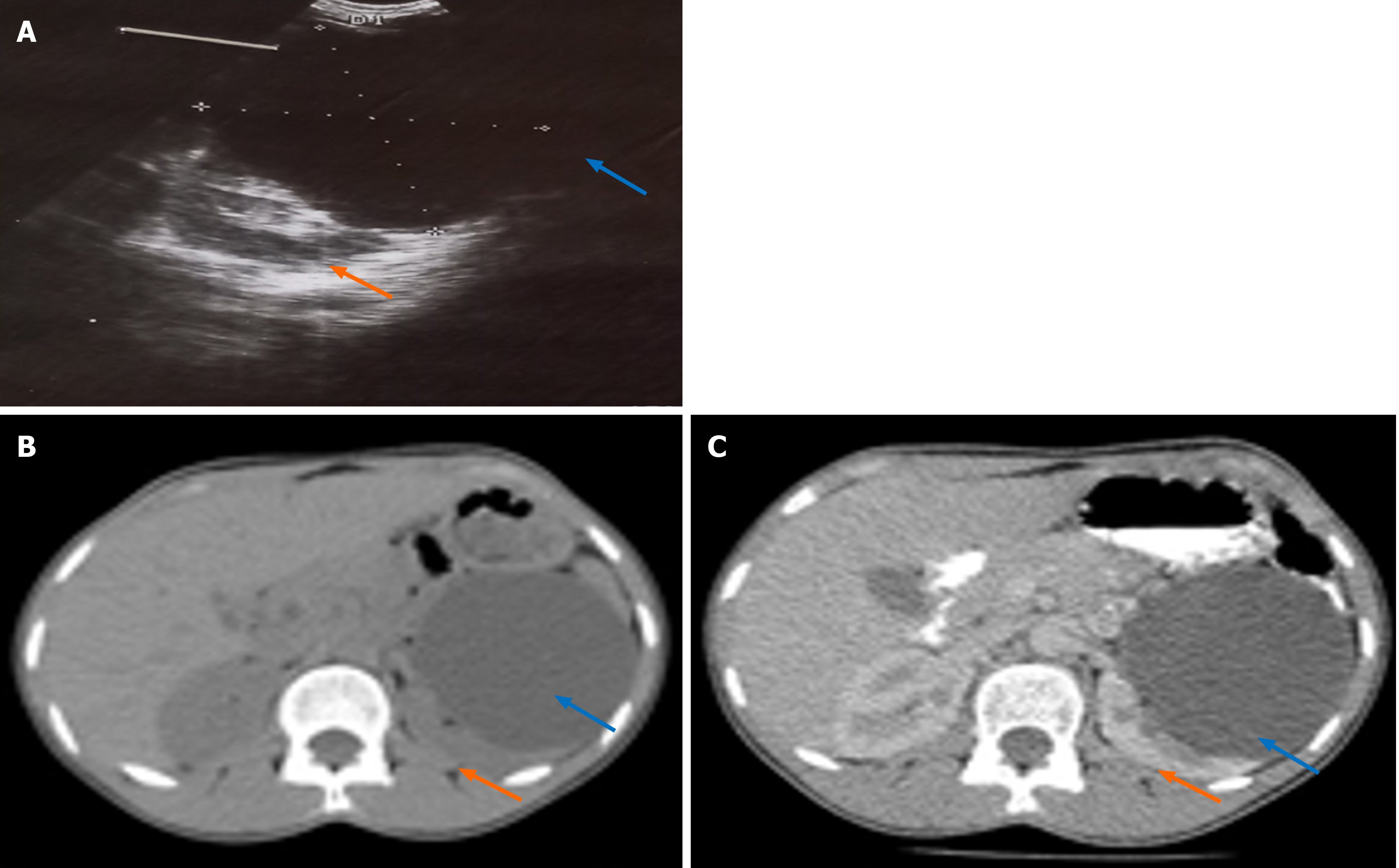
An abdominal ultrasound scan revealed a huge left cystic renal mass which measured 9 cm in its widest diameter (Figure 1A). This was confirmed by a contrast-enhanced abdominal computerized tomography (CT) scan to be a huge Bosniak I simple left renal cortical cyst (Hounsfield unit = 4.1) with bilaterally functioning kidneys (Figure 1B and C).
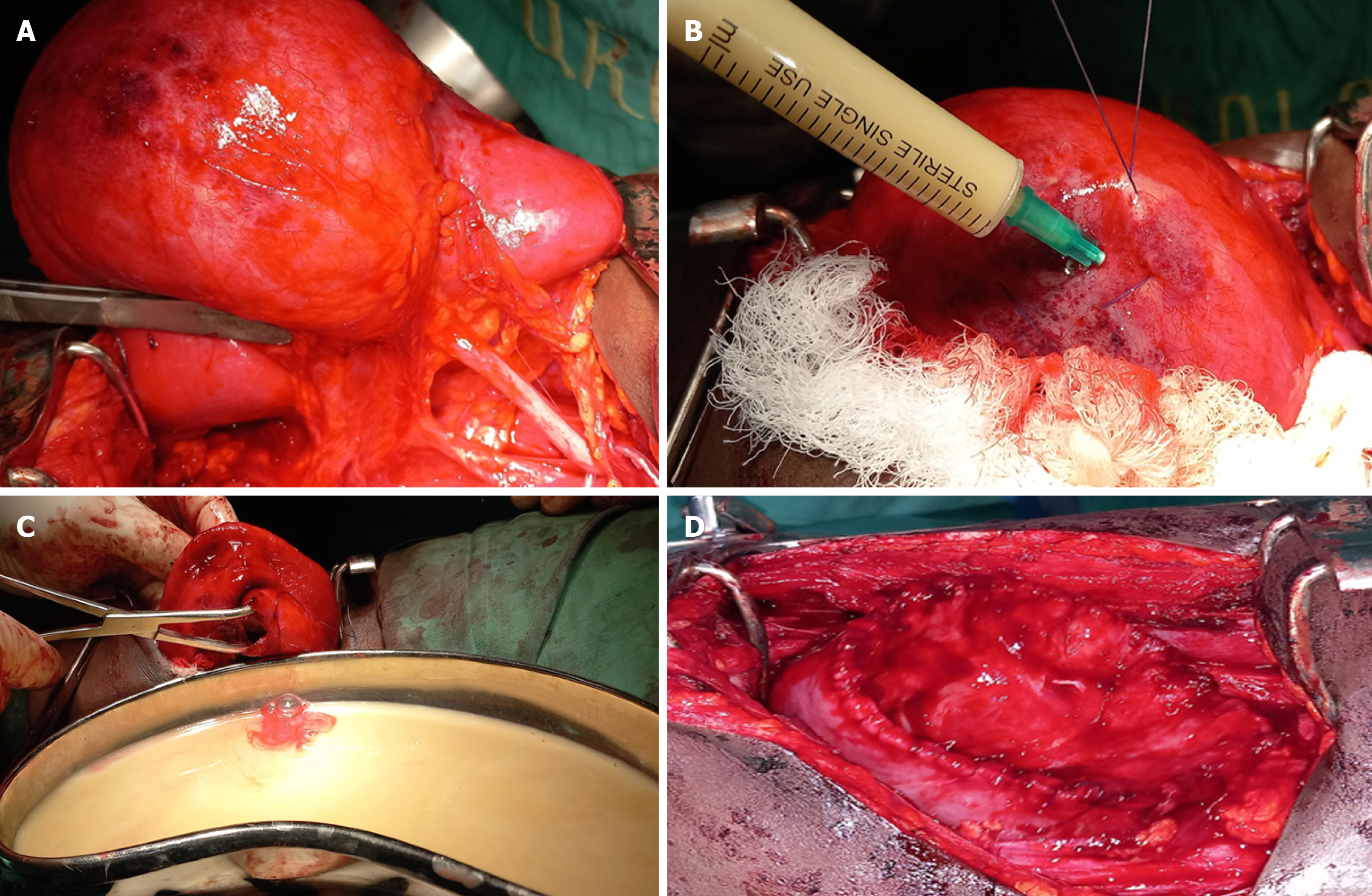
At this point, a diagnosis of an infected giant left renal cortical cyst with bilaterally functioning kidneys was entertained (Figure 2).
She received intravenous levofloxacin, normal saline infusion, and analgesics and underwent open surgical exploration of the left kidney after signing an informed written consent on March 1, 2024. During the exploration, 300 mL of pus were drained, followed by cyst unroofing and marsupialization (Figure 2). Her recovery was uneventful, and she was discharged home on the 10th postoperative day.
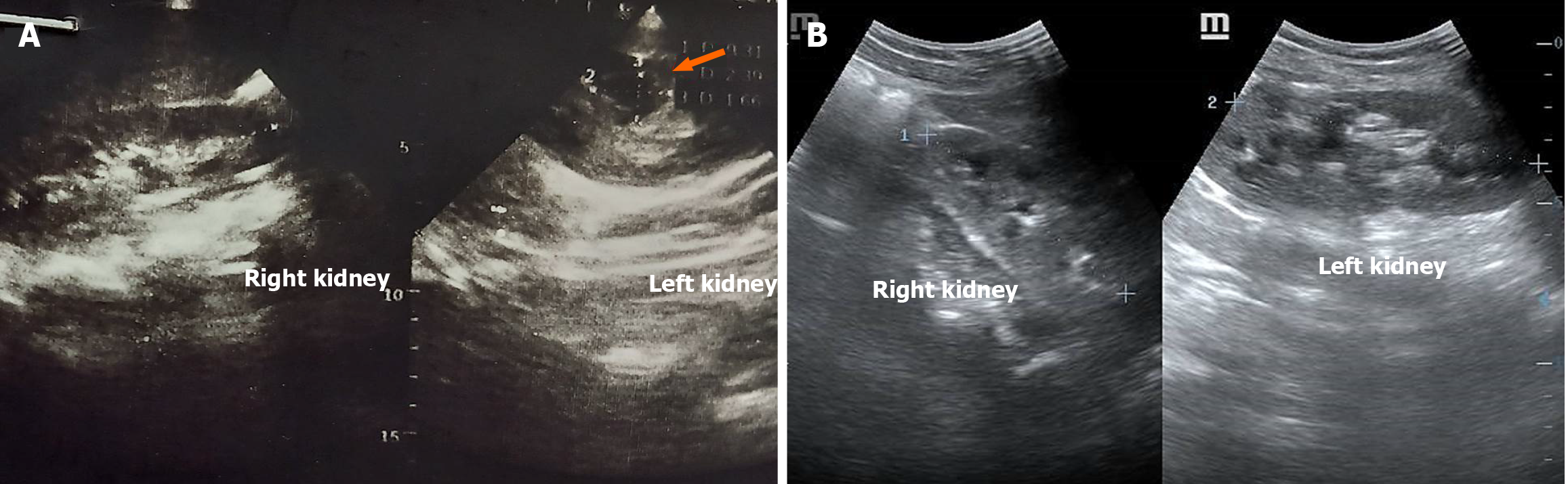
She presented to the clinic at 3 months post-surgery with a complaint of left flank pain. Her urine culture yielded E. coli, and she was treated with levofloxacin based on sensitivity. The renal ultrasound scan showed a medullary cyst in the mid aspect of the left kidney, measuring about 2.4 cm × 1.7 cm, as shown in Figure 3A. She reported complete resolution of symptoms during subsequent follow-up visits, and a repeat ultrasound scan (Figure 3B) at the twelfth-month follow-up visit was satisfactory with complete resolution of the cyst.
This case report describes the management of a huge left renal cyst abscess, a rare but potentially life-threatening condition. The kidneys can undergo cystic degeneration, resulting in the formation of fluid-filled sacs called renal cysts. These conditions are among the most prevalent pathologies in the kidneys and are grouped into two basic categories: Simple and complex cysts[10]. Most simple cysts are innocuous and asymptomatic. The complex cysts, contrary to the simple types, may require more cautious monitoring due to their potential to cause complications[11]. There is an increased risk of developing simple renal cysts with advancing age[12]. About 70% of asymptomatic renal masses are simple cysts, which are often benign fluid-filled sacs that can be single or multiple and vary in size[11]. They are mostly located in the renal cortex and are not in communication with the nephron or renal pelvis. Simple cysts usually appear as single, round or oval-shaped and filled with clear fluid. They are frequently discovered incidentally during imaging examinations done for unrelated illnesses and typically don’t cause any symptoms[4,5,13]. Unless they grow large enough to obstruct the urinary tract, simple renal cysts rarely impair kidney function and do not need to be treated[10,14]. Complex cysts, on the other hand, differ from simple cysts in that they contain internal structures such as septations, calcifications, or blood clots and usually cause symptoms, such as pain or hematuria. They may also be linked to a higher risk of malignancy, especially if they have irregular features. As a result, complex renal cysts are monitored more closely and may need surgery or biopsy to rule out cancer[15].
The index patient had a transabdominal ultrasound scan suggestive of a simple cortical cyst, which got complicated during pregnancy, probably by bleeding into the cyst with subsequent blood clot formation, and clot infection with a resultant suppuration of the cyst. Infection of a renal cyst and subsequent formation of an abscess may arise from an ascending urinary tract infection, hematogenous spread of infection or direct introduction of an infective organism during operation or biopsy[16]. Infection of a renal cyst is a severe complication which usually results in patient hospitalization and frequently requires invasive treatment[17]. Renal cysts could manifest as a hereditary condition known as polycystic kidney disease (PKD), which is characterized by the development of numerous cysts in both kidneys. Impairment of renal function results from the gradual growth of these cysts, which eventually replace a large portion of the kidney tissue. Autosomal dominant PKD (ADPKD), which is more prevalent, and autosomal recessive PKD, which is less common and more severe, are the two primary types of PKD. Most of the reported cases of infected renal cysts are in patients with ADPKD[18,19]. Hypertension, kidney stones, and renal failure are all possible outcomes of ADPKD, which frequently manifests symptoms in adulthood[11,13,17]. Although the index case presented in adulthood, the PKD is unlikely due to the solitary nature of her cyst, the absence of a family history of cystic renal disease, normal renal function, and normotension, among other reasons.
The majority of simple cysts are discovered incidentally[4,13]. When the following criteria are met, one can safely diagnose a classic benign simple cyst using ultrasonography: (1) No internal echoes; (2) A clearly defined, thin, and distinct wall with a smooth and distinct margin; (3) Good sound wave transmission through the cyst with resulting acoustic enhancement behind the cyst; and (4) A spherical or slightly ovoid shape[13,20]. There is very little likelihood of malignancy if all of these conditions are met[13]. Further assessments by the CT scan, or possibly needle aspiration or magnetic resonance imaging (MRI), are recommended when some of these criteria are not met. The CT criteria for a simple cyst are similar to those used in ultrasonography. Once the other CT and ultrasonography criteria are met, the absence of enhancement after an intravenous contrast agent administration with hyperdense cyst fluid (i.e., between 20 and 90 Hounsfield unit) is still likely to be a simple cyst[10,13]. Bosniak proposed a categorization to more clearly distinguish between surgical and nonsurgical kidney cysts. Categories I and II cysts are simple cysts that do not require surgery, while categories III and IV cysts have malignant features and may require surgery[4,11,13].
The diagnosis of renal cyst abscesses can be challenging. Currently, the gold standard for the diagnosis of renal cyst abscess is the presence of bacteria and/or neutrophils in a cyst aspirate[12,20]. Gram-negative bacilli are the most frequently isolated organisms, with E. coli being the commonest[12]. However, in most instances, because of the small size or location of the renal cyst, percutaneous cyst aspiration may be challenging[13]. Therefore, clinicians often rely on combination of clinical, laboratory, and imaging findings to diagnose the condition[17]. Fever and abdominal or flank pain are the most commonly reported symptoms in patients with renal cyst abscess[11,13,17]. Flank swelling is not a common presentation as most renal cyst abscesses are small. However, few patients like our index patient may present with a flank swelling due to the large size of the cyst.
An important part of diagnosis is imaging. The best imaging modalities are contrast-enhanced CT and MRI because they can help differentiate between a simple cyst and an infected one[4,21]. Thickened cyst walls, septations, gas formation, and surrounding inflammation are important imaging features of a cyst abscess[21]. Imaging investigations should be interpreted with caution because hemorrhagic cysts and proteinaceous cysts can similarly increase the renal cyst density[16]. Even though ultrasound scan and CT are useful in identifying renal cyst abscess, they can miss up to 40% of the infected cyst. MRI and contrast-enhanced CT scans are more reliable but require experience with these techniques[20]. Furthermore, the use of contrast agents is relatively contraindicated in the presence of renal function impairment[20].
Surgery is not recommended for an asymptomatic cyst once cancer has been ruled out[21]. Large renal cysts may induce flank or abdominal pain, but other possible causes should be ruled out. Nephrolithiasis is one such coexisting condition that may be the cause of this pain. Pain from bleeding into the cyst or calyceal or infundibular blockage from cyst impingement are other symptoms that can occur from simple cysts. Rarely, hypertension may develop, most likely as a result of segmental renal ischemia of the surrounding renal parenchyma brought on by cyst compression[13,22]. Treatment of the simple cyst should be addressed to the symptomatology. The recurrence of abdominal/flank pain and fever was the main indication of surgical intervention in this patient. When a benign simple cyst results in hypertension or pyelocaliceal blockage, the problem can be resolved percutaneously by aspirating the fluid and possibly injecting sclerosing agents such as glucose, phenol, iophendylate, bismuth phosphate, and absolute ethanol, especially if the fluid has reaccumulated following an earlier aspiration, or surgically by unroofing the cyst[21-23].
Cyst infection, though rare, is a potentially severe complication which may manifest with fever, flank pain, and, sometimes, a sympathetic pleural effusion. This patient had no pleural effusion but with limited chest excursions on the left hemithorax, she may develop pneumonia or pleural effusion later. Most of the patients with cyst infection are women, as seen in the index patient. The most common pathogen is E. coli, a similar finding in this patient; however, urine cultures can often be negative[4,17]. A renal cyst abscess is characterized by the infection and suppuration of a renal cyst, often seen in patients with underlying conditions like ADPKD, diabetes mellitus, or urinary tract obstruction[21,24]. There were none of these predisposing conditions found in this report.
The treatment of a renal cyst abscess entails a multimodal strategy that includes precise diagnosis, antibiotic treatments, other supportive care, drainage techniques, and occasionally surgery[21,22]. The treatment offered to this patient was guided by these surgical principles. The first line of treatment typically comprises empirical broad-spectrum intravenous antibiotics, covering gram-negative organisms (especially E. coli) and anaerobes. Third-generation cephalosporins, trimethoprim-sulfamethoxazole, and fluoroquinolones (like ciprofloxacin) are examples of antibiotics that should ideally have high cyst penetration. Once culture results are available, medication should be tailored to the individual infection and its antibiotic sensitivity. The duration of antibiotic therapy typically ranges from 2 to 6 weeks, depending on the clinical response, cyst size, and whether drainage was performed. The longer courses of antibiotic therapy may be required in patients with complex infections or those with immunocompromised patients[15,21,23]. E. coli was isolated in the index case urine specimen and treated with the sensitive levofloxacin, and associated with the resolution of the febrile episode preoperative.
Delayed treatment can lead to serious consequences such as sepsis, renal failure, or abscess rupture; hence, timely diagnosis is critical. Patients with these serious consequences usually report symptoms like fever, flank pain, dysuria, or malaise as found in the index case[21,23]. Laboratory results frequently show leukocytosis and elevated inflammatory markers, including C-reactive protein and erythrocyte sedimentation rate. The presence of leukocytosis with relative neutrophilia was suggestive of renal cyst infection and a high index of suspicion of cyst abscess before surgery in the patient. Urinalysis and culture may be non-specific or sterile, specifically if the abscess is confined to the cyst and not communicating with the renal collecting system. The possibility of cyst communication with the renal collecting system and infected urine as the cause of this cyst abscess formation could not be completely ruled out here.
In cases where medical therapy alone is insufficient, particularly in large or multiloculated abscesses, percutaneous drainage under ultrasound or CT guidance becomes necessary. This minimally invasive technique allows for direct evacuation of pus and provides samples for microbiological analysis. Because of its high efficacy and relatively low risk, it is considered a first-line interventional treatment[21,22]. Surgery is only performed in situations that are recalcitrant to drainage and antibiotics, or when there is a possibility of cancer or concurrent structural problems. Surgical options for severely damaged or non-functioning kidneys include nephrectomy, partial nephrectomy, or open or laparoscopic cyst decortication[10,15,21,22]. Notwithstanding, the choice of open surgical intervention in this report was primarily influenced by the patient’s preference after detailed counselling on the relative size of the cyst abscess, lack of insurance cover for services payment, concerns about the possibility of recurrence after percutaneous drainage under ultrasound or CT guidance, surgeon’s experience vis-à-vis the feasibility of laparoscopic and robotic interventions. Treatment plans may need to be adjusted for patients with immunosuppression, diabetes mellitus, or kidney transplantation. A lower threshold for intervention is frequently justified since these patients are more vulnerable to unusual organisms. Multiple infected cysts and the difficulties of reaching appropriate antibiotic concentrations make infections in PKD more difficult[17,19].
The kidney is a vital organ not only for its filtration and urination function but also for its role in hematopoiesis, especially by producing erythropoietin, synthesis of vitamin D, helping in the regulation of blood glucose in prolonged starvation, and regulating blood pressure, all or some which can be compromised by a giant renal cyst abscess. Hence, the importance of early renal cyst abscess detection cannot be overemphasized to avoid attendant challenges ranging from septicemia, renal loss, morbidity and mortality among others. In addition, it makes it amenable to nonoperative management, like antibiotic therapy and minimally invasive options like percutaneous drainage. It entails the identification of risk factors in patients such as prior history of renal cyst, pregnancy with immune system alteration, immunosuppressive disorders, diabetic mellitus, urolithiasis, and urinary tract instrumentation, to mention a few. These can be complemented by the emergence of symptoms such as fever and chills, malaise, nausea, vomiting, recurrent flank pain or abdominal pain, and urinary tract symptoms[25]. The index case had an initial ultrasound scan diagnosis of a renal cyst with abdominal and constitutional symptoms during pregnancy to indicate the development of a renal cyst abscess, but this was missed because of improper monitoring.
This paper highlights the stepwise approach to the management of the uncommon presentation of a renal cortical cyst. Patients with this potentially fatal illness continue to have better results because of the ongoing research, advancements in imaging, and minimally invasive procedures. The principle of management should include establishing the diagnosis, which requires a combination of clinical evaluation, laboratory and imaging investigations. The role of perioperative antibiotic therapy is invaluable. The treatment of giant simple renal cortical cyst abscesses is surgical. However, it should be individualized depending on the characteristics of the pathology in question, the surgeon’s experience, patient preference and availability of facilities for endoscopic, laparoscopic or robotic modalities. Notwithstanding open surgical exploration, cyst unroofing and marsupialization are useful modalities in giant renal cortical cyst abscesses and are associated with patient satisfaction.
We sincerely thank all the hospital staff who assisted financially or in kind during the patient’s treatment.
| 1. | Nguyen KA, Brito J, Hsiang W, Nolte A, Syed JS, Suarez-Sarmiento A, Leapman MS, Shuch B. National trends and economic impact of surgical treatment for benign kidney tumors. Urol Oncol. 2019;37:183.e9-183.e15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Graumann O, Osther SS, Karstoft J, Hørlyck A, Osther PJ. Evaluation of Bosniak category IIF complex renal cysts. Insights Imaging. 2013;4:471-480. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Cullivan O, Wong R, Albu C, D'Arcy F, O'Malley E, McCarthy P, Dowling CM. Assessment of the workload and financial burden of Bosniak IIF renal cyst surveillance in a tertiary referral hospital. Ir J Med Sci. 2022;191:2771-2775. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 4. | Nicolau C, Antunes N, Paño B, Sebastia C. Imaging Characterization of Renal Masses. Medicina (Kaunas). 2021;57:51. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 5. | Allen R, Paz-Soldan G, Wilson M, Huang J, Omer T, Mailhot T, Sajed D. Incidental Renal Cysts Found by Point-of-Care Ultrasound: A Retrospective Chart Review. J Emerg Med. 2024;67:e209-e216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Sakai N, Kanda F, Kondo K, Fukuoka H, Tanaka T. Sonographically detected malignant transformation of a simple renal cyst. Int J Urol. 2001;8:23-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Yen DH, Hu SC, Tsai J, Kao WF, Chern CH, Wang LM, Lee CH. Renal abscess: early diagnosis and treatment. Am J Emerg Med. 1999;17:192-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Fair WR, Higgins MH. Renal abscess. J Urol. 1970;104:179-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Fowler JE Jr, Perkins T. Presentation, diagnosis and treatment of renal abscesses: 1972-1988. J Urol. 1994;151:847-851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 32] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Hindman NM. Cystic renal masses. Abdom Radiol (NY). 2016;41:1020-1034. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Mantovani A, Hendry J, Mishra P. Kidney and Ureter: Congenital and Acquired Anomalies. In: Aboumarzouk OM. Blandy’s Urology. United States: John Wiley & Sons, 2019: 145-164. |
| 12. | Khan T, Sajjad T, Qureshi HM, Fonseca A, Khan A, Bano S, Ezenagu UE. An Infected Simple Renal Cyst at Each Pole of the Left Kidney and Its Management: A Case Report. Cureus. 2022;14:e26044. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 13. | William P, Parker WP, Gettman MT. Benign Renal Tumors. In: Dmochowski RR, Kavoussi LR, Craig A. Peters CA. Campbell-Walsh-Wein Urology. Amsterdam: Elsevier, 2021: 2121-2132. |
| 14. | Zhu M, Chu X, Liu C. Effects of Renal Cysts on Renal Function. Arch Iran Med. 2022;25:155-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 15. | Alrumayyan M, Raveendran L, Lawson KA, Finelli A. Cystic Renal Masses: Old and New Paradigms. Urol Clin North Am. 2023;50:227-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 16. | Mansour P, Ammar L, O Gomez Urena E, Chow A, El Labban M. A Unique Presentation of an Infected Renal Cyst: A Case Report and Literature Review. Cureus. 2023;15:e47966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 17. | Colbert GB, Elrggal ME, Gaur L, Lerma EV. Update and review of adult polycystic kidney disease. Dis Mon. 2020;66:100887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 18. | Gupta M, Sherman A, Rosen DC, Chandhoke R. Infected Renal Cyst: Elusive Diagnosis and Percutaneous Management. J Endourol Case Rep. 2020;6:89-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 19. | Lantinga MA, Casteleijn NF, Geudens A, de Sévaux RG, van Assen S, Leliveld AM, Gansevoort RT, Drenth JP; DIPAK Consortium. Management of renal cyst infection in patients with autosomal dominant polycystic kidney disease: a systematic review. Nephrol Dial Transplant. 2017;32:144-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Lantinga MA, Darding AJ, de Sévaux RG, Alam A, Bleeker-Rovers CP, Bobot M, Cornec-Le Gall E, Gevers TJ, Hassoun Z, Meijer E, Mrug M, Nevens F, Onuchic LF, Pei Y, Piccoli GB, Pirson Y, Rangan GK, Torra R, Visser FW, Jouret F, Kanaan N, Oyen WJ, Suwabe T, Torres VE, Drenth JP; Delphi collaborators. International Multi-Specialty Delphi Survey: Identification of Diagnostic Criteria for Hepatic and Renal Cyst Infection. Nephron. 2016;134:205-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Agarwal MM, Hemal AK. Surgical management of renal cystic disease. Curr Urol Rep. 2011;12:3-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 22. | Bas O, Nalbant I, Can Sener N, Firat H, Yeşil S, Zengin K, Yalcınkaya F, Imamoglu A. Management of renal cysts. JSLS. 2015;19:e2014.00097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 23. | Skolarikos A, Laguna MP, de la Rosette JJ. Conservative and radiological management of simple renal cysts: a comprehensive review. BJU Int. 2012;110:170-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 24. | Spillane RJ, Byrne DW. Infected renal cyst. Conn State Med J. 1954;18:587-588. [PubMed] |
| 25. | Zhang X, Xie Y, Huang G, Fu H. Analysis of 17 children with renal abscess. Int J Clin Exp Pathol. 2019;12:3179-3184. [PubMed] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/