Published online Mar 25, 2024. doi: 10.5501/wjv.v13.i1.87881
Peer-review started: August 31, 2023
First decision: October 24, 2023
Revised: November 7, 2023
Accepted: December 25, 2023
Article in press: December 25, 2023
Published online: March 25, 2024
Processing time: 193 Days and 2.3 Hours
The spread of the severe acute respiratory syndrome coronavirus 2 outbreak worldwide has caused concern regarding the mortality rate caused by the infection. The determinants of mortality on a global scale cannot be fully understood due to lack of information.
To identify key factors that may explain the variability in case lethality across countries.
We identified 21 Potential risk factors for coronavirus disease 2019 (COVID-19) case fatality rate for all the countries with available data. We examined univariate relationships of each variable with case fatality rate (CFR), and all independent variables to identify candidate variables for our final multiple model. Multiple regression analysis technique was used to assess the strength of relationship.
The mean of COVID-19 mortality was 1.52 ± 1.72%. There was a statistically significant inverse correlation between health expenditure, and number of computed tomography scanners per 1 million with CFR, and significant direct correlation was found between literacy, and air pollution with CFR. This final model can predict approximately 97% of the changes in CFR.
The current study recommends some new predictors explaining affect mortality rate. Thus, it could help decision-makers develop health policies to fight COVID-19.
Core Tip: The current study recommends some new predictors explaining affect mortality rate. Thus, it could help decision-makers develop health policies to fight coronavirus disease 2019.
- Citation: Sagheb S, Gholamrezanezhad A, Pavlovic E, Karami M, Fakhrzadegan M. Country-based modelling of COVID-19 case fatality rate: A multiple regression analysis. World J Virol 2024; 13(1): 87881
- URL: https://www.wjgnet.com/2220-3249/full/v13/i1/87881.htm
- DOI: https://dx.doi.org/10.5501/wjv.v13.i1.87881
Coronavirus Disease 2019 (COVID-19), an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has led to tremendous worldwide effects on the lives of people around the world, including large-scale morbidity and mortality and limited access to healthcare services (covid19.who.int)[1]. The worldwide case fatality rate (CFR) of COVID-19 has been estimated to be around 1.5% as of now[2]. Different variants of the SARS-CoV-2 virus have been discovered to cause the disease. The clinical presentation of the disease ranges from asymptomatic status to upper respiratory tract symptoms, mild pneumonia, severe respiratory symptoms, acute respiratory distress syndrome, extrapulmonary manifestations, and death[1,3].
Various risk factors for COVID-19 mortality have been named in the literature, including age, male gender, comorbidities (such as chronic kidney disease (CKD), cardiovascular disease, chronic obstructive pulmonary disease (COPD), diabetes mellitus, malignancy, underlying autoimmune disease, and hypertension), ethnicity, vaccination status, smoking history, obesity, and socioeconomic status[4-12] On the other hand, some factors have been proven to be protective, which may reduce the severity or mortality of COVID-19 infection, as among which vaccination[13], efficiently staffed facilities, particularly by registered nurses[14,15] corticosteroid treatment[16], and healthy diet[17] are the most notable. Gathering updated information from international data sources could throw light on the protective or potential risk factors to avoid COVID’s severe morbidities and mortality.
This study aims to assess the correlation between different known risk factors or protective measures and the COVID-19 CFR, described by the number of deaths relative to number of confirmed cases. A similar study was performed in 2020 on 39 countries[18]. Our study is an update to the former one.
In this modeling publicly available register-based ecological study, we started with a literature review focused on the potential risk factors of COVID-19 mortality through Our World in Data, and COVID-related mortality risk factors through World Bank, Our World in Data, Statistica, OECD Database, and World Population Review. Our approach was consistent with a study done by Jennifer Pan, a Modelling study of factors causing death variation estimation by country.
We included all the countries with available COVID-19 CFR data, which enclosed 188 countries. There were 17 countries that had not reported any mortality data until the last date of our data collection (June 24, 2022); therefore, they were not included in the study. We did not have any exclusion criteria. We determined 21 risk factors for the worthwhile COVID-19 deaths, including GDP per capita, Population density, health expenditure per capita, Age, Obesity, Diabetes, human immunodeficiency viruses (HIV), Tobacco Users, Life expectancy, General death rate per 1000, Hospital beds per 1000, Physicians per 1000, Radiologist per 100 K, computed tomography (CT) scanners per million, Air pollution, Literacy rate, Human development index, case fatality rate, Tests per 1 million, Doses per 100 people, Given 1+ dose, Percent Fully vaccinated. In calculating the CFR, we used the total number of confirmed cases and fatalities for a particular country from Our World in Data[19]. Therefore, the CFR formula would be as follows: CFR in % = Number of deaths from Corona/Number of confirmed cases of Corona * 100[20].
In regard to vaccination, people are placed in fully vaccination group two weeks after a second dose of mRNA COVID-19 vaccine, two weeks after receiving a second dose of the Novavax COVID-19 vaccine, or two weeks after they get a single dose of the Janssen/Johnson & Johnson COVID-19 vaccine. They are considered in given 1+ group if they have received at least one dose of COVID-19 vaccine, including fully vaccinated people[21]. Therefore, fully vaccinated people are those who have received two doses for most vaccines, or one or three doses for a few manufacturers[22].
A descriptive analysis of variables has been carried out. Data were presented as mean ± standard deviation for quantitative variables, and numbers (percentage) for qualitative data. We found that GDP, Health Expenditure per capita, Percent HIV, Air pollution, and tests per 1 million were highly positively skewed. In order to reduce the influence of extreme observations, we processed these variables at the logarithm scale.
As our dependent variable, we looked at the univariable relationships between case fatality rates in the next step, and all independent variables to identify candidate variables for our final multiple model.
Multiple regression analysis technique was used to assess the strength of the relationship between an outcome (the dependent variable) and several predictor variables as well as the importance of each of the predictors to the relationship, often with the effect of other predictors statistically eliminated by using the ordinary least squares[23], and the ability to identify outliers we found the multiple models for case fatality rate to be appropriate.
We pointed out the significance of each variable in these univariable models and finally selected variables for our multiple model at P value < 0.05. To detect the severity of multicollinearity, we focused on variance inflation factor (VIF)[24,25]. The model was designed by including all univariable candidate predictors and further developed by adding all significant interaction terms. Our preliminary final model included all 16 variable predictors significant at P values < 0.05. All reported P values were 2-sided with a 0.05 significance level. All variables screening in multiple regression methods led to choosing the most important variables that contribute to the response variable. Statistical analyses were conducted using SPSS version 28 and GraphPad Prism 8.
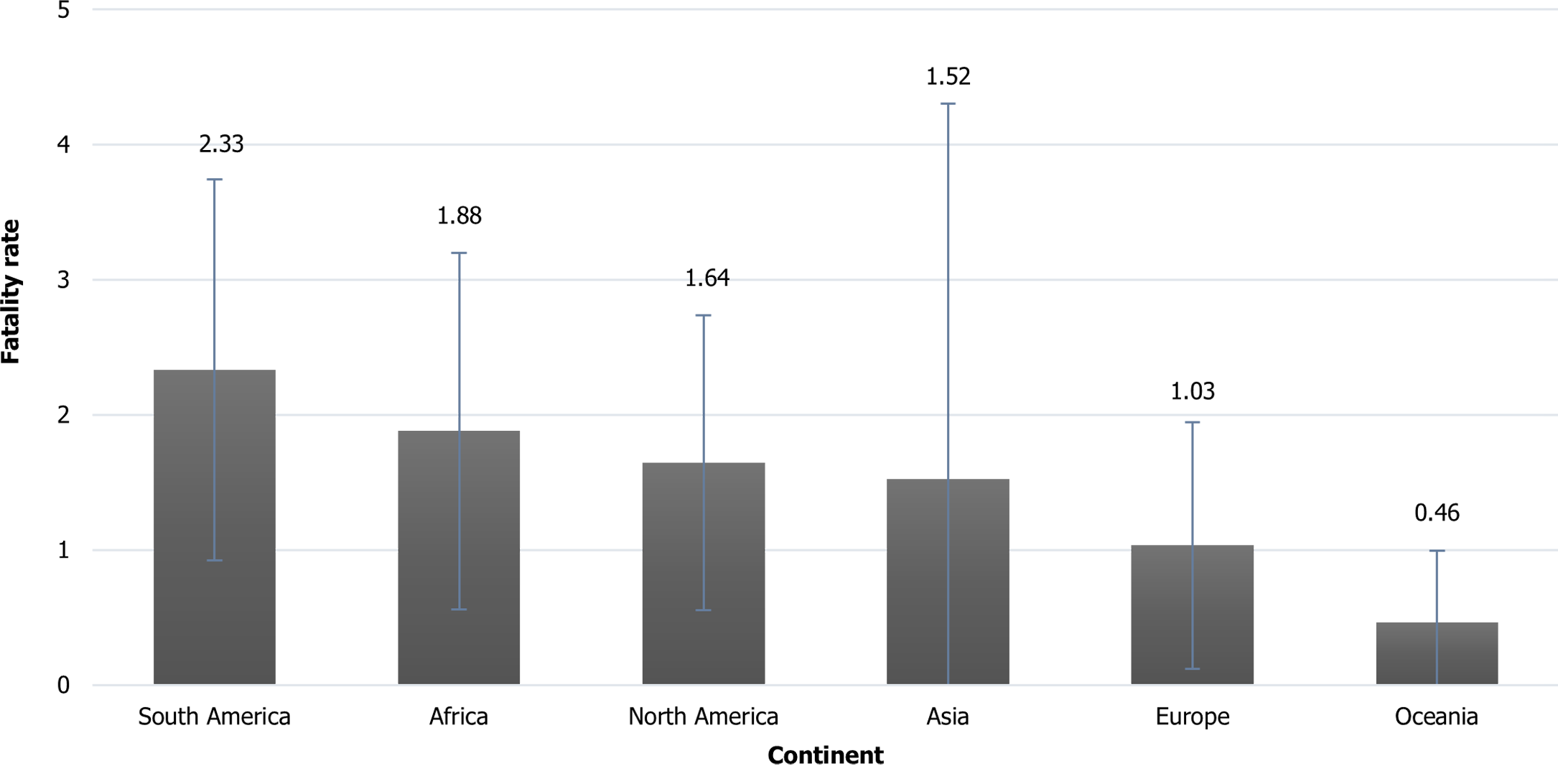
All 188 countries were included in the analysis. The total number of registered COVID-19 cases was 541937600 with a total mortality number of 6317644 patients. The mean of COVID-19 mortality was 1.52 ± 1.72%, with a range between a minimum of 0.03% (Bhutan country) to a maximum of 18.2% (Yemen country). Evaluation of CFR based on the continents, revealed the minimum fatality rate which was in Oceania continent (0.46%) and the maximum which was in South America (2.33%). It was mentioned that 50% of the studied countries had the case fatality rate > 1.15% (median) (Figure 1).
The mean population density was 447.6 ± 2113 person/Km2. The percentage of population > 70 years old was 5.42 ± 4.22% (min: 0.53, United Arab Emirates, max: 18.5, Japan). The mean GDP per capita in 2020 was 15389.61 ± 23441.43. The lowest life expectancy rate was in Central African Republic (53.6 years) and the highest was in Hong Kong (85.39 years). There were 2.35 ± 1.93 physicians per 1000, and hospital beds per 1000, with the highest for Cuba (8.3) and Japan (13.05) respectively. The lowest number of conducted tests per one million population was in Algeria (5083) and the highest was in Denmark (21880771). Regarding the vaccination rate, the lowest percentage of fully vaccinated rate was in Algeria (5083) and the highest was in Denmark (21880771). It was mentioned that 50.8% of the studied countries given 1+ dose vaccination rate < 65.4 (median), and 50.5% given full vaccinated rate < 60.7 (median).
With regards to the number of confirmed cases and performed COVID tests, the minimum and maximum rates were from Africa and Europe, respectively. The minimum and maximum vaccination rates associated with Africa and South America, respectively.
Means and standard deviations of candidate predictors along with the univariate regression coefficient for each individual predictor are shown in Table 1. In these univariate regression models, our analysis demonstrated a statistically significant inverse correlation between CFR and logarithm of population density (P = 0.025), logarithm of health expenditure per capita (P < 0.001), Population ages ≥ 70 Years (P < 0.001), percent obese (P = 0.006), percent diabetes (P = 0.018), life expectancy at birth and hospital beds per 1000 (P < 0.001), physicians per 1000 (P = 0.009), CT scanners per 1 million, Human Development Index (HDI), logarithm of tests per 1 million, given greater than one vaccination, and percent of fully vaccinated people (P < 0.001). Conversely, it revealed a statistically significant direct correlation between logarithm of air pollution (P = 0.014) and literacy rate (P = 0.023) with CFR (Table 1).
| Variable | Mean (SD) | R2 | Beta (SD) | P value |
| Population density1 | 300.96 (1539.00) | 0.027 | -0.116 (0.051) | 0.025 |
| GDP per capita in 20201 | 15389.61 (23441.43) | 0.000 | 0.013 (0.053) | 0.812 |
| Health Expenditure per capita1 | 1161.25 (1865.17) | 0.176 | -0.251 (0.041) | < 0.001 |
| Population ages ≥ 70 yr | 5.42 (4.22) | 0.062 | -0.059 (0.017) | < 0.001 |
| Percent Obese | 18.93 (9.93) | 0.042 | -0.021 (0.007) | 0.006 |
| Percent Diabetes | 7.92 (4.09) | 0.030 | -0.042 (0.018) | 0.018 |
| Percent HIV1 | 1.91 (4.33) | 0.001 | 0.022 (0.066) | 0.743 |
| Percent Tobacco Users | 20.05 (9.55) | 0.016 | -0.013 (0.008) | 0.116 |
| Life expectancy at birth | 72.53 (7.31) | 0.157 | -0.054 (0.009) | < 0.001 |
| General death rate per 1000 | 7.87 (2.97) | 0.017 | 0.044 (0.025) | 0.075 |
| Hospital beds per 1000 | 3.29 (2.44) | 0.115 | -0.145 (0.041) | < 0.001 |
| Physicians per 1000 | 2.35 (1.93) | 0.064 | -0.197 (0.074) | 0.009 |
| Radiologist per 100 K | 13.56 (5.52) | 0.005 | 0.008 (0.026) | 0.759 |
| CT scanners per million | 29.05 (20.02) | 0.353 | -0.932 (0.213) | < 0.001 |
| Air pollution1 | 22.31 (14.73) | 0.066 | 0.416 (0165) | 0.014 |
| Literacy rate | 82.25 (17.33) | 0.067 | 0.013 (0.006) | 0.023 |
| Human development index | 0.72 (0.15) | 0.178 | -2.787 (0.445) | < 0.001 |
| Tests per 1 million1 | 1654560.98 (2994282.33) | 0.234 | -0.266 (0.036) | < 0.001 |
| Doses per 100 people | 133.56 (79.68) | 0.356 | -0.007 (0.001) | < 0.001 |
| Given 1+ dose | 57.71 (26.97) | 0.319 | -0.020 (0.002) | < 0.001 |
| Percent Fully vaccinated | 52.49 (26.82) | 0.341 | -0.021 (0.002) | < 0.001 |
There were also several cases of collinearity. For instance, there were strong positive correlations between the general death rate and Prevalence of current tobacco use (r = 0.333, P < 0.001), Hospital beds per 1000 (r = 0.598, P < 0.001), Physicians per 1000 (r = 0.467, P < 0.001), HDI (r = 0.176, P = 0.018), Current health expenditure per capita (r = 0.154, P = 0.042), and inverse correlation with Diabetes prevalence (r = -0.299, P < 0.001), and Air pollution (r = -0.317, P = 0.002). Also we find a significant positive correlation between CT scanners per 1M and Current health expenditure per capita (r = 0.337, P = 0.041), Hospital beds per 1000 (r = 0.479, P = 0.003), Human development index (r = 0.358, P = 0.029), and inverse correlation with obesity rate (r = -0.422, P = 0.009), and there was a significant direct correlation between HDI and Obesity Rates (r = 0.533, P < 0.001) and Diabetes (r = 0.224, P = 0.002).
In the following, we have multiple predictors without a statistically significant association with the response (all variable with P > 0.05 in Table 1). VIF values were < 5 which represents a medium level of collinearity, therefore we decided to keep all variables, thus we used model reduction (reduce the model by removing terms one at a time) to increases the precision of predictions from the model. To use the statistical significance criterion, after set the significance level on 0.05 we tried different variables to find a model with as many statistically significant terms as possible but with no statistically insignificant terms. We applied the statistical significance criterion manually, with stepwise regression algorithm.
It has been observed that first "Current Health expenditure per capita "with P < 0.001 was entered into the model (model 1), then the variable "Air pollution" has been added to the model with level of significance of 0.018 (model 2), in the third model, "number of CT scanners per 1000 people" has been added to the model and it has been observed that the entry of these changes the Air pollution level of significance from 0.018 (model 2) to 0.006 (model 3). In the fourth model, after entering the "Literacy rate" variable, the regression coefficients and P values of all three previous variables have changed in the model, but the direction of their relationship has not changed. After entering the last variable (literacy rate) into the other model, none of the candidate predictors had the criteria to enter the model, therefor the final model will be the fourth model, with the final multiple regression equation: Y = 3.1 - 0.58 (Health Expenditure per capita) + 1.01 (Air pollution) – 0.74 (Number of CT scanners) + 0.01 (Literacy rate).
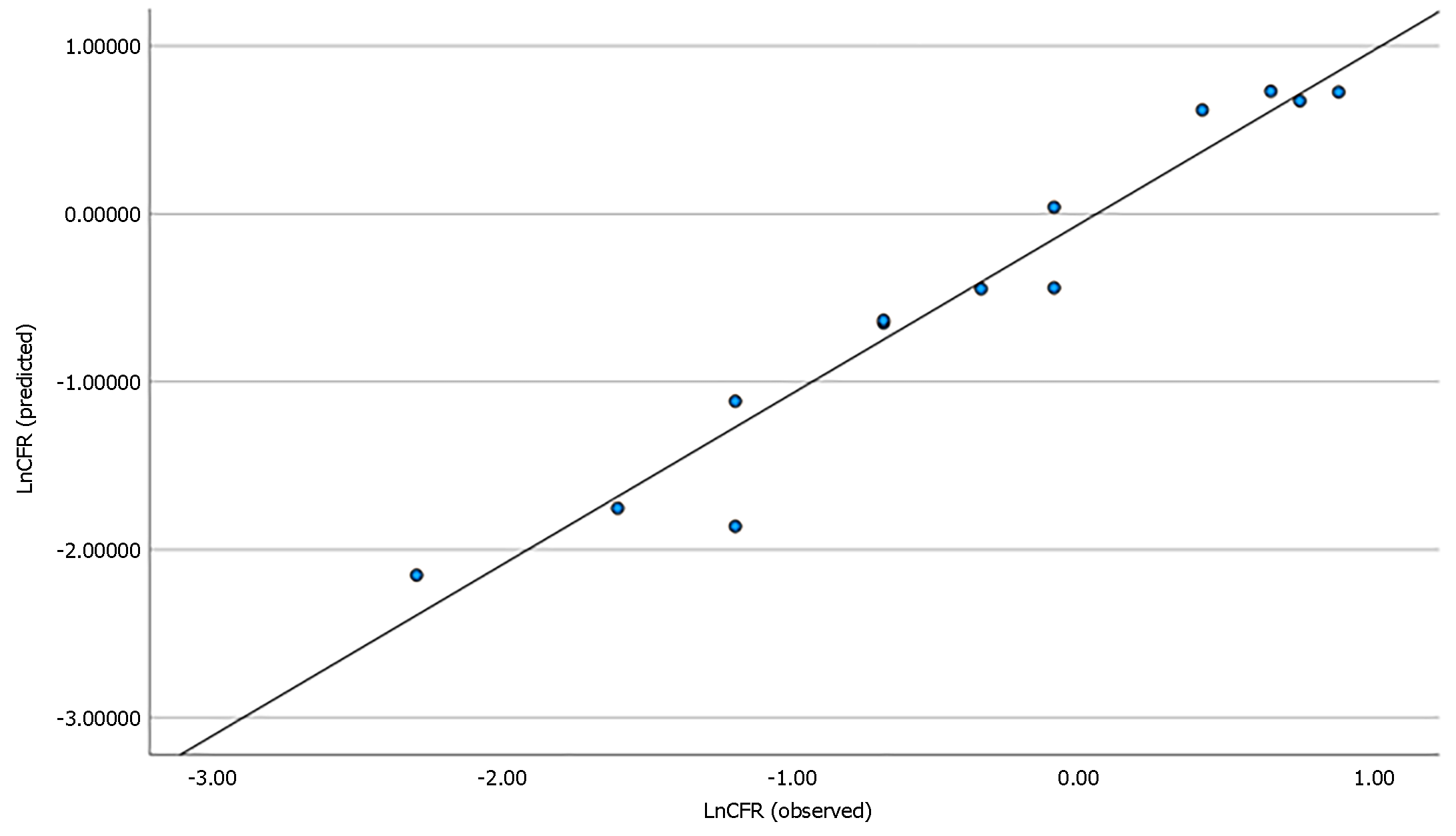
Base on this model, we could claim that this final model can predict approximately 97% of the changes in CFR. Therefore, it suggested an optimal model (Table 2, Figure 2). In this model, there was a statistically significant inverse correlation between health expenditure (P < 0.001) and number of CT scanners per 1 million (P = 0.002) with CFR. In addition, a statistically significant direct correlation was found between literacy rate (P = 0.038) and air pollution (P < 0.001) with CFR.
| Model | Variable | Beta (SD) | Standardized beta | P value | R square (P value) |
| 1 | (Constant) | 7.80 (1.30) | < 0.001 | 0.799 (< 0.001) | |
| Health expenditure per capita | -1.06 (0.17) | -0.894 | < 0.001 | ||
| 2 | (Constant) | 3.42 (1.82) | 0.093 | 0.895 (< 0.001) | |
| Health expenditure per capita | -0.79 (0.16) | -0.667 | < 0.001 | ||
| Air pollution | 0.93 (0.32) | 0.384 | 0.018 | ||
| 3 | (Constant) | 4.29 (1.40) | 0.016 | 0.947 (< 0.001) | |
| health Expenditure per capita | -0.69 (0.12) | -0.580 | < 0.001 | ||
| Air pollution | 0.91 (0.24) | 0.377 | 0.006 | ||
| Number of CT scanners (1 million people) | -0.51 (0.18) | -0.246 | 0.023 | ||
| 4 | (Constant) | 3.10 (1.14) | 0.030 | 0.974 (< 0.001) | |
| Health expenditure per capita | -0.58 (0.10) | -0.486 | < 0.001 | ||
| Air pollution | 1.01 (0.19) | 0.415 | < 0.001 | ||
| Number of CT scanners (per 1 million people) | -0.74 (0.16) | -0.357 | 0.002 | ||
| Literacy rate | 0.01 (0.00) | 0.199 | 0.031 |
The correlation between estimated model and CFR is shown in Figure 2. As mentioned before, despite the fact that the model has shown an appropriate fit, due to the lack of data in some variables, including the CT variable, we have lost a lot of data.
Out study provides new population-based insights regarding the risk factors of COVID-19 mortality. This is an update on our previous efforts to identify indices and predictors of fatal outcomes in different populations based on their socioeconomic status and healthcare system resources.
In previous studies there was a direct association between CFR and increasing age with or without comorbidities[7-9,16-18,26,27]; however, in this study, age 70 and above showed a negative correlation with CFR. This finding can be explained by variance factors such as priority in receiving jabs, strict isolation and social distancing for seniors and lower threshold of intensive care unit (ICU) admission. A higher development index in the countries with a higher median age was also reported as another explanation[19].
With regard to the association between CFR and smoking, there have been discrepant results in the literature. A meta-analysis by Hou et al[28] revealed that smoking was independently associated with increased mortality rate in COVID-19 patients, particularly in former smokers. A review article by World Health Organization (WHO) in 2020 demonstrated an increased severity and mortality of COVID-19 in hospitalized smoking patients[29]. Conversely, in a review article in Alberta, there was no significant increase in severity of COVID-19 in smokers[12]. Comparably, smoking did not have statistically significant correlation with CFR in our study. The reasonable explanation for this controversy could be a lower threshold to use antivirals in these patients or admit them to an ICU.
Life expectancy at birth is described by the average number of years that a newborn is expected to live, considering the age- and sex-specific rates at the time of birth[30]. It is an indicator of the overall mortality level of a population which summarizes the mortality pattern including all age groups - children and adolescents, adults, and the elderly. In our study, countries with a higher COVID-19 CFR had a lower life expectancy at birth which have a latitude of explanations such as better health service coverage and higher health literacy rate in those countries with longer life expectancy. This finding was in agreement of the results of life expectancy evaluation in several countries, including United States and Canada, during the COVID-19 pandemic[31-35].
In a study by Sen-Crowe et al[36] on 183 countries, there was a weakly positive significant association between the number of ICU beds per 100000 population and COVID-19 mortality. Though, there was no significant association between the number of hospital beds or acute care beds per 100000 populations and COVID-19 mortality. In other studies, a negative association between hospital capacity, especially hospital beds, and COVID-19 mortality has been confirmed[18,37,38]. Similarly, our study revealed lower COVID-19 CFR in the countries with a higher number of hospital beds per 1000 population, which potentially can be explained by the higher level of care for COVID-19 patients in these countries. Similar findings were noted in association of COVID-19 CFR and the number of physicians per 1000 population, which was in line with the cross-sectional study by Tchicaya et al[39] in France in 2020. Increased staffing, particularly with Registered Nurses, has been reported as a protective factor leading to decreased mortality[15]. In another study by Stephen Rocks in 2020 on the effects of hospital capacity on COVID-19 mortality in 33 countries, a negative association between hospital capacity, especially hospital beds, and COVID-19 mortality rate was found. However, they realized that the main determinants in these countries were mostly variables other than treatment capacity per se, including earlier lock-down restrictive measures, which limited the number of new cases. Moreover, they found that low hospital capacity can affect mortality by detracting other sources from non-health sections leading to indirect effects on COVID-19 mortality rather than a direct effect[37].
With regards to COVID-19 testing, the more COVID tests were performed, the lower was the CFR. This finding was in agreement with the previous studies in which a negative association between COVID-19 testing and mortality was demonstrated[40-42], particularly among low-income countries and those with fewer hospital beds[41]. Timely testing can lead to earlier isolation and effectively limit the disease spread, as well as appropriate treatment interventions, if required[43,44].
HDI is defined by having a standard living with a healthy and long life and access to education (Our World in Data). Studies on the association between HDI and COVID-19 CFR, found a negative correlation[45-48]. However, there have been a few studies that have reported positive correlation which was explained by a higher infection rate as a result of higher rate of chronic disease, higher number of performed COVID-19 tests and older population in these high HDI countries[14,49,50]. Our study demonstrated less CFR in countries with a higher HDI worldwide. This also could be due to more access to education in these countries.
Several types of COVID vaccines have been produced from inactivated or weakened virus vaccines to RNA and DNA vaccines[51]. To date, based on the WHO vaccine tracker, 169 and 198 vaccines have been under clinical and pre-clinical development, respectively. Vaccination by COVID-19 vaccine has been mentioned as a protective factor against the disease severity and mortality in the literature[9,17]. In a meta-analysis by Huang et al[13] in 2021, it was found that all types of vaccines, compared with no vaccine status, were effective to decrease the frequency of severe cases and consequently, to decrease the mortality rate. In a longitudinal study on 90 countries, 10% increase in vaccine coverage led to 7.6% decrease in CFR[52]. Our study also revealed a negative association between the number of COVID-19 vaccine doses, receiving at least one dose vaccine and fully vaccination with CFR.
With regard to the correlation between comorbidities such as diabetes and obesity with CFR, there have been various results in the literature. In a meta-analysis of 87 studies on the association between COVID-19 mortality and the comorbidities, diabetes mellitus was one of the most important factors associated with mortality[53]. Similar findings have been reported in the literature[54,55]. Comparably, there has been an increased COVID-19 mortality in obese patients (body mass index over 30 kg/m2), both in adults and pediatrics[17,56,57]; however, in an evidence-based review in Alberta, there has not been a consistent association between obesity and mortality. Moreover, there was not a high strength association between diabetes and COVID-19 mortality[12]. Our study revealed a negative correlation between diabetes and obesity with CFR indicating decreased CFR in diabetics or obese patients (Table 1). The higher prevalence of obesity and diabetes in countries with higher HDI[11,14,45,47,48] which can explain the lower CFR in this population.
Our regression analysis modeling was able to define the effects of the above given variables on the CFR, when considering them together. Our subsequent modeling and regression analysis revealed that the following variables have the highest connection with CFR: Health expenditure per capita, CT scanner per 1 million, air pollution, and literacy rate.
Health expenditure means all expenditures required for the planning of health services, family planning activities, nutrition activities and emergency aid designated for health, except for the provision of drinking water and sanitation (WHO). There has been a negative correlation between health expenditure and rigorous policies regarding COVID-19, including closure of the schools, universities and working places, home confinement, as well as internal and international travel restrictions[58]. Despite the thought that higher health expenses should decrease mortality due to better patient care, a positive correlation between health expenditure and COVID-19 mortality is reported in the literature[59]. This finding is in agreement with our study. It could be the result of lower efficacy of the health care in regions with higher health expenses.
In a literature review by Pan et al[18] on 39 countries in 2020, the number of CT scanners per one million was associated with decreased CFR. We also found statistically significant association between the number of CT scanners per one million and COVID-19 CFR. This can be explained by earlier detection of lung involvement through CT scan which leads to timely treatment[60,61], particularly in low- to mid-income countries with less availability of COVID-19 tests , earlier in the course of pandemic[62] which can prevent more severe disease and subsequently decreases mortality.
Several studies have considered air pollution as a risk factor which increases morbidity and mortality of COVID-19[43,44,63]. This was in agreement with our study, both in univariate regression and multiple regression analysis. This could be because of the detrimental cardiovascular effects of air pollution, both short- and long-term, through oxidative stress and inflammation in lungs and heart vessels, leading to reduced lung function, atherosclerosis, and acute thrombotic complications[64].
There are many studies indicating negative correlation of health literacy with COVID-19 morbidity and mortality[65,66]. To the best of our knowledge, the correlation between COVID-19 CFR and literacy rate has not been reviewed in the literature. This study revealed a negative correlation between CFR and literacy rate, based on the WHO’s definition of literacy rate. High health literacy rate may originate from a better literacy rate leading to lower mortality due to healthier behavior.
This study revealed controversial findings pertaining to the different variables analysis per se. However, adding multiple variables in a model increased the accuracy of the evaluation of those risk factors. Our multiple-model regression analysis explained a higher percentage of changes in CFR in relation with health expenditure, number of CT scanners per one million, air pollution, as well as literacy rate.
There were some limitations to this study. Firstly, source of the analysed data in our study was based on the reports from different countries; therefore, the true CFR could be more than the reported one. Moreover, in this study, we could not include all countries due to inadequate recording of data on CFR. Secondly, we could not evaluate or achieve statistically significant correlation between CFR and some variables due to incomplete data on some variables that have been already mentioned in some isolated reports.
The worldwide case fatality rate (CFR) of coronavirus disease 2019 (COVID-19) has been estimated to be around 1.5% as of now. Different variants of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus have been discovered to cause the disease. The clinical presentation of the disease ranges from asymptomatic status to upper respiratory tract symptoms, mild pneumonia, severe respiratory symptoms, acute respiratory distress syndrome, extrapulmonary manifestations, and death. Various risk factors for COVID-19 mortality including age, male gender, comorbidities (such as chronic kidney disease, cardiovascular disease, chronic obstructive pulmonary disease), diabetes mellitus, malignancy, underlying autoimmune disease, and hypertension), ethnicity, vaccination status, smoking history, obesity, and socioeconomic status. On the other hand, some factors have been proven to be protective, which may reduce the severity or mortality of COVID-19 infection, as among which vaccination, efficiently staffed facilities, particularly by registered nurses corticosteroid treatment, and healthy diet are the most notable. Gathering updated information from international data sources could throw light on the protective or potential risk factors to avoid COVID’s severe morbidities and mortality.
We find it interesting the topic trend analysis in the COVID-19 literature, and the success of modeling studies in the field of predicting disease behavior was a turning point for us.
The objective motivation for doing this study is to assess the correlation between different known risk factors or protective measures and the COVID-19 case fatality rate and we decided to design and conduct a new study based on modeling.
Twenty-one potential risk factors were identified for COVID-19 case fatality rate for all the countries with available data. Univariate relationships of each variable with case fatality rate, and all independent variables to identify candidate variables for our final multiple model were examined. Finally multiple regression analysis technique was used to assess the strength of relationship between case fatality rate and several predictors’ variables as well as the importance of each predictor to the relationship.
There was a statistically significant inverse correlation between health expenditure, and number of computed tomography scanners per 1 million with case fatality rate, and a significant direct correlation was found between literacy, and air pollution with case fatality rate, this final model can predict approximately 97% of the changes in case fatality rate, conclusion: The current study recommends some new predictors explaining affect mortality rate. Thus, it could help decision-makers develop health policies to fight COVID-19.
I suggest to do the same study with the updated data and compare the results. Multiple regression analysis technique is used as the most wrong and reliable method.
Considering that global vaccination has been carried out, it is suggested that the approach of future realizations is to investigate the effectiveness of vaccines and compare the performance of vaccines with each other.
| 1. | Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239-1242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11409] [Cited by in RCA: 11623] [Article Influence: 1937.2] [Reference Citation Analysis (2)] |
| 2. | Our World in Data. Cumulative case fatality rate of the COVID-19 pandemic. Available from: https://ourworldindata.org/grapher/covid-cfr-exemplars. |
| 3. | Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35178] [Cited by in RCA: 30494] [Article Influence: 5082.3] [Reference Citation Analysis (13)] |
| 4. | Chishinga N, Smith S, Gandhi NR, Onwubiko UN, Telford C, Prieto J, Chamberlain AT, Khan S, Williams S, Khan F, Sarita Shah N. Characteristics and Risk Factors for Mortality by Coronavirus Disease 2019 Pandemic Waves in Fulton County, Georgia: A Cohort Study March 2020-February 2021. Open Forum Infect Dis. 2022;9:ofac101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | AbuRuz S, Al-Azayzih A, ZainAlAbdin S, Beiram R, Al Hajjar M. Clinical characteristics and risk factors for mortality among COVID-19 hospitalized patients in UAE: Does ethnic origin have an impact. PLoS One. 2022;17:e0264547. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 6. | Astengo M, Tassinari F, Paganino C, Simonetti S, Gallo D, Amicizia D, Piazza MF, Orsi A, Icardi G, Ansaldi F. Weight of risk factors for mortality and short-term mortality displacement during the COVID-19 pandemic. J Prev Med Hyg. 2021;62:E864-E870. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 7. | Liu W, Yang C, Liao YG, Wan F, Lin L, Huang X, Zhang BH, Yuan Y, Zhang P, Zhang XJ, She ZG, Wang L, Li H. Risk factors for COVID-19 progression and mortality in hospitalized patients without pre-existing comorbidities. J Infect Public Health. 2022;15:13-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 8. | Rezaei F, Ghelichi-Ghojogh M, Hemmati A, Ghaem H, Mirahmadizadeh A. Risk factors for COVID-19 severity and mortality among inpatients in Southern Iran. J Prev Med Hyg. 2021;62:E808-E813. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Sezen YI, Senoglu S, Karabela SN, Yesilbag Z, Borcak D, Canbolat Unlu E, Korkusuz R, Ozdemir Y, Kart Yasar K. Risk factors and the impact of vaccination on mortality in COVID-19 patients. Bratisl Lek Listy. 2022;123:440-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 10. | Lehmann A, Gysan M, Bernitzky D, Bal C, Prosch H, Zehetmayer S, Milos RI, Vonbank K, Pohl W, Idzko M, Gompelmann D. Comparison of pulmonary function test, diffusion capacity, blood gas analysis and CT scan in patients with and without persistent respiratory symptoms following COVID-19. BMC Pulm Med. 2022;22:196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 11. | Dessie ZG, Zewotir T. Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect Dis. 2021;21:855. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 553] [Article Influence: 110.6] [Reference Citation Analysis (0)] |
| 12. |
Abaluck J, Kwong LH, Styczynski A, Haque A, Kabir A.
"COVID-19 Scientific Advisory Group Rapid Response Report." |
| 13. | Huang YZ, Kuan CC. Vaccination to reduce severe COVID-19 and mortality in COVID-19 patients: a systematic review and meta-analysis. Eur Rev Med Pharmacol Sci. 2022;26:1770-1776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 28] [Reference Citation Analysis (0)] |
| 14. | Khazaei Z, Goodarzi E, Naemi H, Hasanpour-Dehkordi A, Naghibzadeh-Tahami A. COVID-19 pandemic in the world and its relation to Human Development Index: A global study. Arch Clin Infect Dis. 2020;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Dykgraaf SH, Matenge S, Desborough J, Sturgiss E, Dut G, Roberts L, McMillan A, Kidd M. Protecting Nursing Homes and Long-Term Care Facilities From COVID-19: A Rapid Review of International Evidence. J Am Med Dir Assoc. 2021;22:1969-1988. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 101] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 16. | Soto A, Quiñones-Laveriano DM, Azañero J, Chumpitaz R, Claros J, Salazar L, Rosales O, Nuñez L, Roca D, Alcantara A. Mortality and associated risk factors in patients hospitalized due to COVID-19 in a Peruvian reference hospital. PLoS One. 2022;17:e0264789. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 17. | Zhang JJ, Dong X, Liu GH, Gao YD. Risk and Protective Factors for COVID-19 Morbidity, Severity, and Mortality. Clin Rev Allergy Immunol. 2023;64:90-107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 279] [Cited by in RCA: 412] [Article Influence: 137.3] [Reference Citation Analysis (0)] |
| 18. | Pan J, St Pierre JM, Pickering TA, Demirjian NL, Fields BKK, Desai B, Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19): A Modeling Study of Factors Driving Variation in Case Fatality Rate by Country. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 19. | Mathieu E, Ritchie H, Rodés-Guirao L, Appel C, Gavrilov D, Giattino C, Hasell J, Macdonald B, Dattani S, Beltekian D, Ortiz-Ospina E, Roser M. Coronavirus Pandemic (COVID-19). Available from: https://ourworldindata.org/coronavirus. |
| 20. | Ghani AC, Donnelly CA, Cox DR, Griffin JT, Fraser C, Lam TH, Ho LM, Chan WS, Anderson RM, Hedley AJ, Leung GM. Methods for estimating the case fatality ratio for a novel, emerging infectious disease. Am J Epidemiol. 2005;162:479-486. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 172] [Cited by in RCA: 156] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 21. | Staff MC. Fully vaccinated? Get the facts. (accessed on). Available from: https://www.mayoclinic.org/coronavirus-covid-19/fully-vaccinated. |
| 22. | Our World in Data. People fully vaccinated per hundred. (accessed on). Available from: https://ourworldindata.org/grapher/share-people-fully-vaccinated-covid?time=earliest. |
| 23. | Uyanık GK, Güler N. A study on multiple linear regression analysis. Procedia-Social and Behavioral Sciences. 2013;106:234-240. [RCA] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 147] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 24. | Neter J, Kutner MH, Nachtsheim CJ, Wasserman W. Applied linear statistical models. 1996. |
| 25. | Cueto-Manzano AM, Espinel-Bermúdez MC, Hernández-González SO, Rojas-Campos E, Nava-Zavala AH, Fuentes-Orozco C, Balderas-Peña LMA, González-Ojeda A, Cortes-Sanabria L, Mireles-Ramírez MA, Ramírez-Márquez JJ, Martínez-Gutiérrez PE, Ávila-Morán M, De-Dios-Pérez RI, Acosta-Ramírez C, Hernández-García HR. Risk factors for mortality of adult patients with COVID-19 hospitalised in an emerging country: a cohort study. BMJ Open. 2021;11:e050321. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 26. | Fernández Ibáñez JM, Morales Ballesteros MDC, Galindo Andúgar MÁ, Fernández Anguita MJ, Arias Arias Á, Barberá-Farré JR. [Risk factors for mortality in patients over 65 years old hospitalized by COVID-19]. Rev Esp Geriatr Gerontol. 2022;57:6-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 27. | Riera J, Alcántara S, Bonilla C, Fortuna P, Blandino Ortiz A, Vaz A, Albacete C, Millán P, Ricart P, Boado MV, Ruiz de Gopegui P, Santa Teresa P, Sandoval E, Pérez-Chomón H, González-Pérez A, Duerto J, Gimeno R, Colomina J, Gómez V, Renedo G, Naranjo J, García MA, Rodríguez-Ruiz E, Silva PE, Pérez D, Veganzones J, Voces R, Martínez S, Blanco-Schweizer P, García M, Villanueva-Fernández H, Fuset MP, Luna SM, Martínez-Martínez M, Argudo E, Chiscano L, Roncon-Albuquerque R Jr. Risk factors for mortality in patients with COVID-19 needing extracorporeal respiratory support. Eur Respir J. 2022;59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 28. | Hou H, Li Y, Zhang P, Wu J, Shi L, Xu J, Diao J, Wang Y, Yang H. Smoking Is Independently Associated With an Increased Risk for COVID-19 Mortality: A Systematic Review and Meta-analysis Based on Adjusted Effect Estimates. Nicotine Tob Res. 2021;23:1947-1951. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 29. | World Health Organization. Smoking and COVID-19: Scientific brief. UCSF: Center for Tobacco Control Research and Education. 2020. Available from: https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-Sci_Brief-Smoking-2020.2. |
| 30. | Life expectancy. (accessed on). Available from: https://ourworldindata.org/grapher/Life-expectancy. |
| 31. | Castro MC, Gurzenda S, Turra CM, Kim S, Andrasfay T, Goldman N. Reduction in life expectancy in Brazil after COVID-19. Nat Med. 2021;27:1629-1635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 71] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 32. | Andrasfay T, Goldman N. Reductions in 2020 US life expectancy due to COVID-19 and the disproportionate impact on the Black and Latino populations. medRxiv. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 33. | Reyes de la Rocha S, Brown MA. Asthma in children: emergency management. Ann Emerg Med. 1987;16:79-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 34. | Woolf SH, Masters RK, Aron LY. Changes in Life Expectancy Between 2019 and 2020 in the US and 21 Peer Countries. JAMA Netw Open. 2022;5:e227067. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 54] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 35. | Aburto JM, Schöley J, Kashnitsky I, Zhang L, Rahal C, Missov TI, Mills MC, Dowd JB, Kashyap R. Quantifying impacts of the COVID-19 pandemic through life-expectancy losses: a population-level study of 29 countries. Int J Epidemiol. 2022;51:63-74. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 209] [Cited by in RCA: 186] [Article Influence: 46.5] [Reference Citation Analysis (0)] |
| 36. | Sen-Crowe B, Sutherland M, McKenney M, Elkbuli A. A Closer Look Into Global Hospital Beds Capacity and Resource Shortages During the COVID-19 Pandemic. J Surg Res. 2021;260:56-63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 146] [Cited by in RCA: 170] [Article Influence: 34.0] [Reference Citation Analysis (0)] |
| 37. | Rocks S, Idriss O. Did hospital capacity affect mortality during the pandemic’s first wave. London: The Health Foundation 2020. Available from: https://www.health.org.uk/news-and-comment/charts-and-infographics/did-hospital-capacity-affect-mortality-during-the-pandemic. |
| 38. | Janke AT, Mei H, Rothenberg C, Becher RD, Lin Z, Venkatesh AK. Analysis of Hospital Resource Availability and COVID-19 Mortality Across the United States. J Hosp Med. 2021;16:211-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 92] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 39. | Tchicaya A, Lorentz N, Leduc K, de Lanchy G. COVID-19 mortality with regard to healthcare services availability, health risks, and socio-spatial factors at department level in France: A spatial cross-sectional analysis. PLoS One. 2021;16:e0256857. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 40. | Wei C, Lee CC, Hsu TC, Hsu WT, Chan CC, Chen SC, Chen CJ. Correlation of population mortality of COVID-19 and testing coverage: a comparison among 36 OECD countries. Epidemiol Infect. 2020;149:e1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 41. | Liang LL, Tseng CH, Ho HJ, Wu CY. Covid-19 mortality is negatively associated with test number and government effectiveness. Sci Rep. 2020;10:12567. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 140] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 42. | Terriau A, Albertini J, Montassier E, Poirier A, Le Bastard Q. Estimating the impact of virus testing strategies on the COVID-19 case fatality rate using fixed-effects models. Sci Rep. 2021;11:21650. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 43. | Semczuk-Kaczmarek K, Rys-Czaporowska A, Sierdzinski J, Kaczmarek LD, Szymanski FM, Platek AE. Association between air pollution and COVID-19 mortality and morbidity. Intern Emerg Med. 2022;17:467-473. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 44. | Wu X, Nethery RC, Sabath BM, Braun D, Dominici F. Exposure to air pollution and COVID-19 mortality in the United States: A nationwide cross-sectional study. medRxiv. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 433] [Cited by in RCA: 397] [Article Influence: 66.2] [Reference Citation Analysis (0)] |
| 45. | Ameye SA, Ojo TO, Adetunji TA, Awoleye MO. Is there an association between COVID-19 mortality and Human development index? The case study of Nigeria and some selected countries. BMC Res Notes. 2022;15:186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 46. | Zhou L, Puthenkalam JJ. Effects of the Human Development Index on COVID-19 Mortality Rates in High-Income Countries. EJ-DEVELOP. 2022;2:26-31. [DOI] [Full Text] |
| 47. | Palamim CVC, Boschiero MN, Valencise FE, Marson FAL. Human Development Index Is Associated with COVID-19 Case Fatality Rate in Brazil: An Ecological Study. Int J Environ Res Public Health. 2022;19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 48. | Dorregaray-Farge ZE, Tarazona AS, De La Cruz-Vargas JA. Correlation between mortality due to COVID-19, wealth index, human development and population density in districts of Metropolitan Lima during 2020. Revista de la Facultad de Medicina Humana. 2021;21:11. [DOI] [Full Text] |
| 49. | Liu K, He M, Zhuang Z, He D, Li H. Unexpected positive correlation between human development index and risk of infections and deaths of COVID-19 in Italy. One Health. 2020;10:100174. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 50. | Gill Z, Mulpuri S, Jalil Y, Ma J, Taparia K. Human Development and COVID-19: An Unforeseen Positive Correlation. Human Development 2022. |
| 51. | World Health Organization. Coronavirus disease (COVID-19): Vaccines. (accessed on). Available from: https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-(covid-19)-vaccines. |
| 52. | Liang LL, Kuo HS, Ho HJ, Wu CY. COVID-19 vaccinations are associated with reduced fatality rates: Evidence from cross-country quasi-experiments. J Glob Health. 2021;11:05019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 53. | Corona G, Pizzocaro A, Vena W, Rastrelli G, Semeraro F, Isidori AM, Pivonello R, Salonia A, Sforza A, Maggi M. Diabetes is most important cause for mortality in COVID-19 hospitalized patients: Systematic review and meta-analysis. Rev Endocr Metab Disord. 2021;22:275-296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 147] [Article Influence: 29.4] [Reference Citation Analysis (0)] |
| 54. | Ran J, Zhao S, Han L, Ge Y, Chong MKC, Cao W, Sun S. Increase in Diabetes Mortality Associated With COVID-19 Pandemic in the U.S. Diabetes Care. 2021;44:e146-e147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 55. | Sourij H, Aziz F, Bräuer A, Ciardi C, Clodi M, Fasching P, Karolyi M, Kautzky-Willer A, Klammer C, Malle O, Oulhaj A, Pawelka E, Peric S, Ress C, Sourij C, Stechemesser L, Stingl H, Stulnig T, Tripolt N, Wagner M, Wolf P, Zitterl A, Kaser S; COVID-19 in diabetes in Austria study group. COVID-19 fatality prediction in people with diabetes and prediabetes using a simple score upon hospital admission. Diabetes Obes Metab. 2021;23:589-598. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 56. | Lamichhane DK, Shrestha S, Kim HC. District-Level Risk Factors for COVID-19 Incidence and Mortality in Nepal. Int J Environ Res Public Health. 2022;19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 57. | Al-Sabah S, Al-Haddad M, Al-Youha S, Jamal M, Almazeedi S. COVID-19: Impact of obesity and diabetes on disease severity. Clin Obes. 2020;10:e12414. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 58. | Jalloh MF, Zeebari Z, Nur SA, Prybylski D, Nur AA, Hakim AJ, Winters M, Steinhardt LC, Gatei W, Omer SB, Brewer NT, Nordenstedt H. Drivers of COVID-19 policy stringency in 175 countries and territories: COVID-19 cases and deaths, gross domestic products per capita, and health expenditures. J Glob Health. 2022;12:05049. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 59. | Blondel S, Vranceanu R. COVID-19 mortality and health expenditures across European countries: The positive correlation puzzle. Available at SSRN 3679972 2020.. [DOI] [Full Text] |
| 60. | Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020;296:E32-E40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3614] [Cited by in RCA: 3297] [Article Influence: 549.5] [Reference Citation Analysis (2)] |
| 61. | Fields BKK, Demirjian NL, Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19) diagnostic technologies: A country-based retrospective analysis of screening and containment procedures during the first wave of the pandemic. Clin Imaging. 2020;67:219-225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 62. | Davarpanah AH, Mahdavi A, Sabri A, Langroudi TF, Kahkouee S, Haseli S, Kazemi MA, Mehrian P, Falahati F, Tuchayi AM, Bakhshayeshkaram M, Taheri MS. Novel Screening and Triage Strategy in Iran During Deadly Coronavirus Disease 2019 (COVID-19) Epidemic: Value of Humanitarian Teleconsultation Service. J Am Coll Radiol. 2020;17:734-738. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 55] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 63. | Nobile F, Michelozzi P, Ancona C, Cappai G, Cesaroni G, Davoli M, Di Martino M, Nicastri E, Girardi E, Beccacece A, Scognamiglio P, Sorge C, Vairo F, Stafoggia M. Air pollution, SARS-CoV-2 incidence and COVID-19 mortality in Rome - a longitudinal study. Eur Respir J. 2022;60. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 64. | Pope III CA, Dockery DW. Health effects of fine particulate air pollution: lines that connect. J. Air & Waste Manage. Assoc. 2006;56:709-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4493] [Cited by in RCA: 2642] [Article Influence: 132.1] [Reference Citation Analysis (0)] |
| 65. | Panahi R, Dehghankar, L, Anbari M. The role of health literacy in the prevention of Covid-19. JHL. 2021;5:63-64. [DOI] [Full Text] |
| 66. | McCaffery KJ, Dodd RH, Cvejic E, Ayrek J, Batcup C, Isautier JM, Copp T, Bonner C, Pickles K, Nickel B, Dakin T, Cornell S, Wolf MS. Health literacy and disparities in COVID-19-related knowledge, attitudes, beliefs and behaviours in Australia. Public Health Res Pract. 2020;30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 164] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Virology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fabbri N, Italy; Wang K, China S-Editor: Liu JH L-Editor: A P-Editor: Chen YX