Published online Sep 25, 2022. doi: 10.5501/wjv.v11.i5.352
Peer-review started: February 1, 2022
First decision: April 8, 2022
Revised: May 20, 2022
Accepted: July 25, 2022
Article in press: July 25, 2022
Published online: September 25, 2022
Processing time: 234 Days and 11.8 Hours
Coronavirus disease 2019 (COVID-19) has been the most talked-about disease of the past few years. Patients with significant comorbidities have been at particular risk of adverse outcomes. This study looked at the outcomes and risk factors for adverse outcomes among patients on chronic hemodialysis for end-stage renal disease, a group of patients known to be particularly susceptible to infectious complications.
To assess outcomes and risk factors for adverse outcomes of COVID-19 infection among patients on chronic hemodialysis.
We searched PubMed/MEDLINE, EMBASE, Reference Citation Analysis (https://www.referencecitationanalysis.com/) and Web of Science databases for relevant terms and imported the results into the Covidence platform. From there, studies were assessed in two stages for relevance and quality, and data from studies that satisfied all the requirements were extracted into a spreadsheet. The data was then analyzed descriptively and statistically.
Of the 920 studies identified through the initial database search, only 17 were included in the final analysis. The studies included in the analysis were mostly carried out during the first wave. We found that COVID-19 incidence among patients on hemodialysis was significant, over 10% in some studies. Those who developed COVID-19 infection were most likely going to be hospitalized, and over 1 in 5 died from the infection. Intensive care unit admission rate was lower than the infection lethality rate. Biochemical abnormalities and dyspnea were generally reported to be associated with adverse outcomes.
This systematic review confirms that patients on chronic hemodialysis are very high-risk individuals for COVID-19 infections, and a significant proportion was infected during the first wave. Their prognosis is overall much worse than in the general population, and every effort needs to be made to decrease their exposure.
Core tip: This is a systematic review to find out the mortality of coronavirus disease 2019 (COVID-19) infection in end stage kidney disease patients that are on regular maintenance hemodialysis. We found that COVID-19 incidence among patients on hemodialysis was significant, over 10% in some studies. Those who developed COVID-19 infection were most likely going to be hospitalized, and over 1 in 5 died from the infection. Intensive care unit admission rate was lower than the infection lethality rate. Biochemical abnormalities and dyspnea were generally reported to be associated with adverse outcomes.
- Citation: Cancarevic I, Nassar M, Daoud A, Ali H, Nso N, Sanchez A, Parikh A, Ul Hosna A, Devanabanda B, Ahmed N, Soliman KM. Mortality rate of COVID-19 infection in end stage kidney disease patients on maintenance hemodialysis: A systematic review and meta-analysis. World J Virol 2022; 11(5): 352-361
- URL: https://www.wjgnet.com/2220-3249/full/v11/i5/352.htm
- DOI: https://dx.doi.org/10.5501/wjv.v11.i5.352
Since early 2020, the coronavirus disease 2019 (COVID-19) pandemic has caused hundreds of thousands of deaths in the United States and millions worldwide, alongside unprecedented disruptions in everyday life. Elderly and patients with significant comorbidities are known to be more susceptible to severe forms of both viral and bacterial respiratory infections, and the same has been shown to be true with COVID-19[1-3]. Chronic kidney disease (CKD) is one of the most prevalent chronic conditions in the United States[4]. The high prevalence of diseases that frequently lead to CKD, such as cardiac disease, hypertension, and diabetes, likely means that the prevalence of CKD will remain high in years to come.
Patients with end-stage renal disease (ESRD) requiring hemodialysis are likely to be especially susceptible to infections. Infection-related complications in those patients exceed 40 in 100 patients per year[5]. Patients with ESRD often undergo in-center hemodialysis, making it more difficult to physically separate for infection control purposes. Also, frequent visits to healthcare facilities for routine check-ups may contribute to infection spread. Additionally, this group's comorbidities make them immunodeficient, increasing their risk of infection[6].
Furthermore, evidence suggests a high frequency of acute kidney injury (AKI) development among patients hospitalized with COVID-19, which is associated with significant mortality[7,8]. AKI is also a known risk factor for CKD development and progression[9].
All these factors make it plausible that COVID-19 would be an especially severe disease in patients with end-stage renal disease on hemodialysis. Due to the high prevalence of ESRD requiring HD and the number of COVID-19 infections worldwide, determining the actual impact COVID-19 has on this population could enable clinicians to target the factors associated with increased mortality and, subsequently, improve the care they provide are delivering.
This systematic review will attempt to determine the prognosis of end-stage renal disease patients on hemodialysis who test positive for COVID-19 and any clinical or laboratory findings associated with adverse outcomes.
The databases used for our systematic review were PubMed/MEDLINE, EMBASE, Reference Citation Analysis (https://www.referencecitationanalysis.com/) and Web of Science, up to date as of April 10, 2022. The review aims to follow the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The search strategy for the PubMed database was: ("COVID-19"[Mesh] OR "SARS-CoV-2"[Mesh] OR "COVID-19" OR "COVID19" OR "novel coronavirus" OR "coronavirus 2019" OR "COVID" OR "SARS-CoV-2") AND ("Kidney Failure, Chronic"[Mesh] OR "CKD" OR "chronic kidney disease" OR "end-stage renal disease" OR "ESRD" OR " end stage kidney disease (ESKD) " OR "end-stage kidney disease" OR "end-stage renal disease" OR "end-stage kidney disease") AND ("Renal Dialysis"[Mesh] OR "renal dialysis" OR "hemodialysis" OR "dialysis") AND ("Prognosis"[Mesh] OR "Mortality"[Mesh] OR "Survival"[Mesh] OR "prognosis" OR "lethality" OR "mortality" OR “survival”). The search strategy for Web of Science and Embase was: ("COVID-19" OR "COVID 19" OR "novel coronavirus" OR "coronavirus 2019" OR "COVID" OR "SARS-CoV-2") AND ("CKD" OR "chronic kidney disease" OR "end-stage renal disease" OR "ESRD" OR "ESKD" OR "end-stage kidney disease" OR "end-stage renal disease" OR "end-stage kidney disease") AND ("renal dialysis" OR "hemodialysis" OR "dialysis") AND ("prognosis" OR "lethality" OR "mortality" OR “survival”).
Articles were then imported into the Covidence platform, which automatically removed duplicates. Two reviewers then independently screened titles and abstracts for relevance. Conflicts were resolved through direct communication between the two reviewers. Where consensus could not be reached, the third reviewer made the decision.
Afterward, full texts were obtained and screened for relevance. Those that were deemed relevant were assessed for quality using the National Institute of Health scoring systems according to the type of study in question, and only those studies that scored no less than three points below the maximum were included in the final review.
We included prospective and retrospective observational studies as well as clinical trials if they involved at least 100 adult patients with end-stage renal disease on chronic hemodialysis who dev-eloped COVID-19 infection. We excluded case reports, case series, all review articles, conference abstracts, letters, communications, and editorials. We also excluded studies that were written in languages other than English and those that could not be retrieved. Equally, we excluded studies that pertained to pediatric patients and those that involved patients on peritoneal dialysis.
A spreadsheet was created and used as a data extraction tool. The following data were extracted for all the studies: authors, title, quality assessment score, number of patients who were studied, the incidence of COVID-19 among patients on hemodialysis, number of patients who required intensive care unit (ICU) level of care, number of deaths, as well as any findings that were found to be associated with increased risk of death or severe disease.
Data were entered into the spreadsheet and analyzed descriptively. Afterward, statistical analysis was done using SPSS software, and the results were presented in the form of a forest plot.
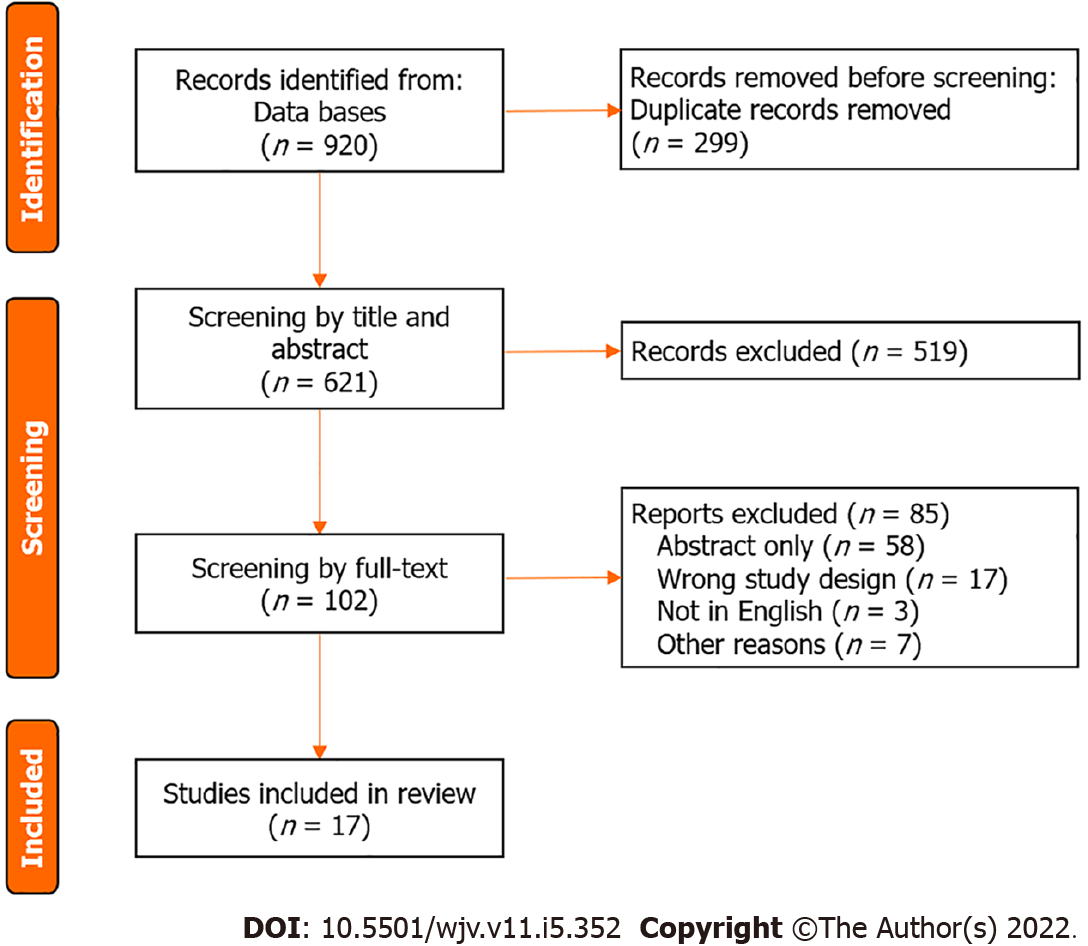
We found 920 articles through databases search. The 299 duplicate articles were automatically removed by the Covidence platform. The authors screened the titles and abstracts of 621 articles for relevance. The 519 articles were excluded at that stage. A total of 102 full texts were assessed for quality and relevance, and 85 of them were excluded. A total of 17 articles were included in our analysis, comprising a total of 37280 patients (Figure 1).
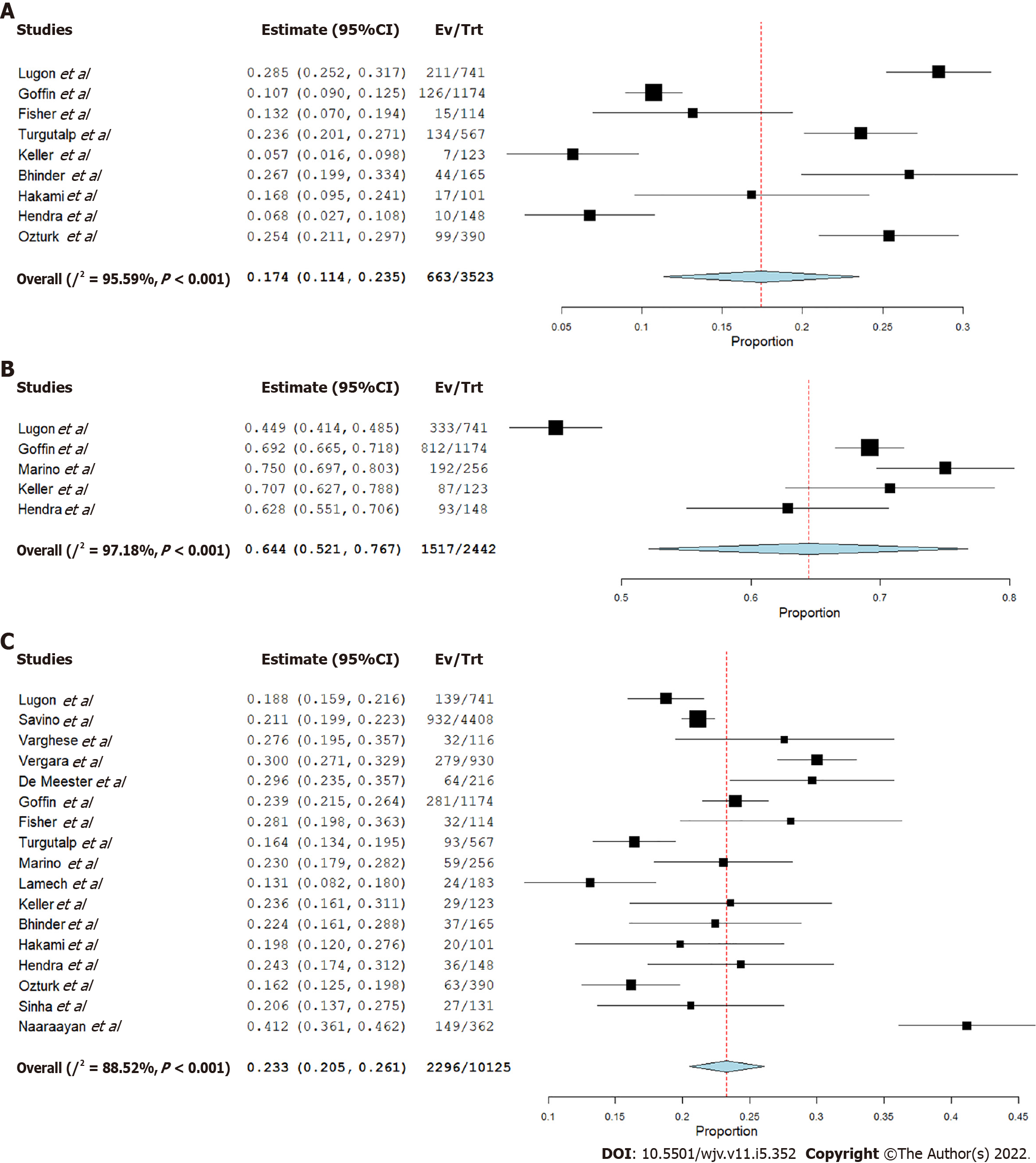
The number of ICU admissions was reported in 9 studies. The pooled analysis showed incidence of ICU admission of 17.4% (95%CI: 0.114-0.235) with high heterogeneity (I2 = 95.59%, P < 0.001) (Figure 2A).
The number of hospital admissions was reported in 5 studies. The incidence of hospitalization after COVID-19 infection among patients included in those studies is 64.4% (95%CI: 0.521-0.767) with high heterogeneity (I2 = 97.18%, P < 0.001) (Figure 2B).
All 17 studies reported mortality. The pooled estimate showed the incidence of mortality to be 23.3% (95%CI: 0.205-0.261) with significant heterogenicity I2 = 88.52%, P < 0.001) (Figure 2C).
Not all the studies that were included in this review analyzed both the incidence and prognosis of COVID-19 patients on chronic hemodialysis. The incidence of COVID-19 is very difficult to analyze, considering that different studies looked at very different patient populations and different periods. However, several studies looked at the incidence in 2020, before vaccines were available. Lugon et al[10] reported that 741 out of 9877 Brazilian patients developed COVID-19 in 2020. Savino et al[11] reported the incidence of 4408 out of 22415 in England, Wales, and Northern Ireland; however, their study included the month of January 2021, when the United Kingdom was averaging tens of thousands of cases per day, the highest recorded up to that point in time[11,12]. De Meester et al[13] and Keller et al[14] reported a lower incidence, but their study period ended in May 2020, only including the infections that occurred during the first wave. Marino et al[15], however, reported a relatively low incidence of only 256 out of 4942 with their study period extending to November 2020 but still not taking into account the spike in winter 2020/2021, unlike Savino et al[11]. Ozturk et al[16] reported the incidence of 148 out of 746 until 05/11/2020 only in a single center in London, which is notably higher than in other studies covering the same study period.
The reported incidence of COVID-19 in patients on chronic hemodialysis is higher than in the general population, where the overall incidence in the first wave was relatively low despite the havoc it caused[12,17]. Cases started rising significantly in the winter of 2020/2021, but only Savino et al[11] covered the majority of that wave[12,17]. It needs to be said, however, that part of the explanation for the low incidence of COVID-19 during the first wave can be explained by the scarcity of testing for the general public, while patients on chronic hemodialysis would likely have been among the first ones to get tested, skewing the incidence numbers. It is also true that patients on chronic hemodialysis clearly have been in a very precarious and vulnerable position early in the pandemic. They were required to spend significant amounts of time in health care facilities when both tests and personal protective equipment were not widely available. Overall, while it is likely that the results were skewed by a difference in the availability of tests between hemodialysis patients and the general public, it is still likely that the incidence of COVID-19 infections among them was higher.
There are multiple ways to look at the COVID-19 prognosis. In terms of the risk of hospitalization, it is significant among patients with end-stage renal disease. However, it is important to note that hospitalization criteria vary between institutions, and if, for example, desaturation is required to admit a patient without significant comorbidities, a far lower threshold may be employed for patients with ESRD. Furthermore, some of the studies only looked at hospitalized patients, possibly skewing numbers. In addition, most of the studies were done early in the course of the pandemic when the criteria were less clear, and there was a significant scarcity of ICU beds. That probably explains why in some of the studies, the incidence of death was higher than the incidence of ICU admission. While determining the exact COVID-19 Lethality is difficult due to the unknown number of cases that are undetected, what is undoubtedly true is that prognosis of COVID-19 infection is significantly worse in ESRD patients compared to the general public. In the studies involved in this systematic review, almost two-thirds of all the patients infected by COVID-19 were hospitalized, with 17.4% (95%CI: 0.114-0.235) P < 0.001 requiring ICU admission and 23.3% (95%CI: 0.205-0.261) P < 0.001 ultimately succumbing to the infection. There are no major outliers in terms of mortality, but it should be noted that studies such as Ozturk et al[16], Fisher et al[18], Turgutalp et al[19], Bhinder et al[20], Hakami et al[21], Sinha et al[22], and Naaraayan et al[23] only reported cases that led to hospitalization so the mortality rates in those articles may be less representative unless a way to adjust them for hospitalization rate was found. A possibly relevant study to point to is Lamech et al which reported that close to one-third of all patients who tested positive for COVID-19 required mechanical ventilation[24]. HD itself may be an independent risk factor for mortality because, despite the required immunosuppressive treatment, Goffin et al[25] found mortality significantly lower among kidney transplant recipients than patients with HD. At the same time, De Meester et al[13] found that overall mortality among HD patients did not increase compared to pre-pandemic levels. That finding is surprising given that both Lugon et al[10] and Savino et al[11] found that a very significant proportion of HD patients developed COVID-19, and almost all the studies showed that those who do get infected are at significant risk of mortality. That would ordinarily raise the question about a possible selection bias in De Meester et al[13]; however, the study included the entire hemodialysis population of a region in Belgium, so barring a significant environmental confounder in that particular region, the study should be generalizable.
We looked at a number of risk factors that may be associated with mortality among hemodialysis patients who got infected by COVID-19. A number of prior studies suggest that diabetes worsens the prognosis of COVID-19[26]. Lugon et al[10] found a statistically significant association between diabetes and COVID-19 mortality among HD patients with an HR of 1.52 (1.05–2.19) P = 0.026. Hakami et al[21], Sinha et al[22], and Varghese et al[27] similarly found diabetes to be associated with COVID-19 mortality. Savino et al[11], Fisher et al[18], Turgutalp et al[19], Marino et al[15], Lamech et al[24], and Hendra et al[28] found no statistically significant difference in mortality among those with diabetes. While it can be assumed that this can be explained by sample sizes alone, that is not the case since the Savino et al[11] study included 4408 patients. Overall, those findings are difficult to interpret. Diabetes is a common cause of end-stage renal disease that also seems to worsen COVID-19 outcomes in the general population; however, it needs to be noted that all ESRD patients have significant comorbidity at baseline, and it remains unclear whether diabetes is uniquely associated with COVID-19 mortality compared to other conditions which also lead to ESRD.
Several studies looked at the association between common laboratory values and COVID-19 mortality. White blood cell (WBC) count and C-reactive peptide (CRP) were commonly reported as they normally correlate with the severity of infections. Varghese et al[27] and Hendra et al[28] found both to be associated with mortality, with CRP difference between those who died and those who survived being reported as 78.82 ± 89.16 vs 40.49 ± 43.16 (P = 0.002) by Varghese et al[27] and 128.0 (75.0-261.8) vs 40.5 (23.0-108.8) P < 0.0001 by Hendra et al[28] and WBC count difference 14.14 ± 8.88 vs 6.03 ± 2.37 (P = 0.001) reported by Varghese et al[27] and 7.45 (5.6-9.8) vs 5.40 (4-7) P = 0.0007 by Hendra et al[28]. In the study done by Keller et al[14], CRP was found to be associated with mortality [14.2 (10.2-27) vs 9.3 (3.8-18.9) P = 0.005], while WBC count was not [6.7 (4.7-9.5) vs 5.5 (3.9-7.6) P = 0.6]. Hakami et al[21] and Sinha et al[22] only reported the WBC difference as follows: 9.1 ± 1.3 vs 6.3 ± 0.4 P = 0.04 reported by Hakami et al[21] and 11.059 ± 5929 vs 7022 ± 2935 P < 0.001 reported by Sinha et al[22]. Keller et al[14] only reported the CRP difference and found it to be statistically significant: 95 (49-192) vs 44.5 (19-92) P = 0.0003.
Overall, it does appear that elevations in both CRP and WBC count are associated with worse outcomes. A meta-analysis by Malik et al[29] also reported that CRP elevation is associated with adverse outcomes in COVID-19 in the general population. It is worth noting that a number of conditions and treatments other than COVID-19 can be associated with CRP and WBC elevations. For example, corticosteroids can lead to elevated WBC counts, and corticosteroids are a common treatment for both severe COVID-19 and a number of conditions that may ultimately lead to ESRD. Further subgroup analysis would be required to evaluate further whether a significant confounder exists.
Varghese et al[27] also found hyponatremia and hyperkalemia to be associated with poor outcomes, while studies by Hakami et al[21] and Sinha et al[22] found no significant difference in outcomes based on sodium or potassium levels. Electrolyte abnormalities would, in general, be expected among patients on hemodialysis, especially on days when dialysis sessions are not scheduled. However, other studies have found that both sodium and potassium abnormalities are associated with worse COVID-19 outcomes in the general population[30,31]. It is almost undeniably true that every effort should be made to keep electrolytes within reference ranges, whether hyponatremia and hyperkalemia at presentation are associated with increased COVID-19 severity or simply a consequence of the dialysis schedule.
Ferritin is both an inflammatory marker and a relevant marker of iron stores in the body. Five of the studies included in this analysis looked at the significance of ferritin in determining the prognosis of COVID-19, and all found ferritin to be significantly higher among hemodialysis patients who succumb to COVID-19 in comparison to those who survive[18,19,21,27,28]. It is notable, however, that average ferritin levels varied widely between studies, and while in each study, patients with higher ferritin were more likely to die, in some studies, even the levels among those who survived were notably higher than those of those who died in a different study. Moreover, it needs to be remembered that patients with ESRD are likely to be anemic at baseline. Therefore, even though all the studies point towards an association between higher ferritin and mortality, it is difficult to interpret clinically.
Finally, dyspnea is one of the most common symptoms of severe respiratory infection, and decreased oxygen saturation is a marker of worsening respiratory status. The same has generally held true for COVID-19 throughout the pandemic, and oxygen saturation level is frequently used as one of the main criteria for the hospital admission. As would be expected, both dyspnea and oxygen saturation were associated with mortality. Of the five studies that analyzed the association between dyspnea and COVID-19 mortality in HD patients, all 5 showed statistical significance, with a P value never reaching 0.03[15,19,21,22,27]. Studies by Varghese et al[27] and Fisher et al[18] found a significant association between lower SpO2 and mortality. Keller et al[14] and Hendra et al[28] failed to find a significant association. It should be noted that all 4 of the aforementioned studies had relatively small sample sizes, and oxygen saturation generally falls within a narrow range, likely impacting some of the findings. Moreover, patients tend to desaturate later in the course of the disease, and if HD patients were admitted to the hospital early due to their pre-existing comorbidities, it is possible that this could make SpO2 at presentation less reliable as an indicator of COVID-19 severity in those patients.
The study has several notable limitations. Firstly, most of the studies only looked at COVID-19 prognosis in the early phases of the pandemic when treatment options were also more limited, and no vaccines were available. Secondly, we excluded three as they were written in languages other than English. The way data was reported varied across studies, limiting the number of studies that reported each variable. Finally, hospital and ICU admission criteria vary between institutions, so they may not be a perfect indicator of disease severity.
Patients on chronic hemodialysis due to end-stage renal disease are among the most vulnerable members of society at increased risk of both catching and succumbing to COVID-19 infection. We found that the incidence of COVID-19 in hemodialysis patients was significant, and in some studies, more than one-tenth caught COVID-19 during the first wave. The prognosis was overall much poorer than in the general population, with the majority requiring hospitalization and more than one in five deaths. Generally, biochemical abnormalities and early dyspnea were associated with a higher degree of mortality. It would be interesting to see how much the numbers would change if the same studies were done during subsequent COVID-19 waves.
Coronavirus disease 2019 (COVID-19) has been the most talked-about disease of the past few years. Patients with significant comorbidities have been at particular risk of adverse outcomes. We looked at the outcomes and risk factors for adverse outcomes among patients on chronic hemodialysis.
The authors assess outcomes and risk factors for adverse outcomes of COVID-19 infection among patients on chronic hemodialysis.
The objective of this study is to assess outcomes and risk factors for adverse outcomes of COVID-19 infection among patients on chronic hemodialysis.
The authors searched PubMed/MEDLINE, EMBASE, Reference Citation Analysis (https://www.referencecitationanalysis.com/) and Web of Science databases for relevant terms and imported the results into the Covidence platform. From there, studies were assessed in two stages for relevance and quality, and data from studies that satisfied all the requirements were extracted into a spreadsheet. The data was then analyzed descriptively and statistically.
Of the 920 studies identified through the initial database search, only 17 were included in the final analysis. The studies included in the analysis were mostly carried out during the first wave. The authors found that COVID-19 incidence among patients on hemodialysis was significant, over 10% in some studies. Those who developed COVID-19 infection were most likely going to be hospitalized, and over 1 in 5 died from the infection. ICU admission rate was lower than the infection lethality rate. Biochemical abnormalities and dyspnea were generally reported to be associated with adverse outcomes.
This systematic review confirms that patients on chronic hemodialysis are very high-risk individuals for COVID-19 infections, and a significant proportion was infected during the first wave. Their prognosis is overall much worse than in the general population, and every effort needs to be made to decrease their exposure.
Further research can be done to assess the efficacy of protective measures and vaccines against COVID-19 among dialysis patients.
| 1. | Kim L, Garg S, O'Halloran A, Whitaker M, Pham H, Anderson EJ, Armistead I, Bennett NM, Billing L, Como-Sabetti K, Hill M, Kim S, Monroe ML, Muse A, Reingold AL, Schaffner W, Sutton M, Talbot HK, Torres SM, Yousey-Hindes K, Holstein R, Cummings C, Brammer L, Hall AJ, Fry AM, Langley GE. Risk Factors for Intensive Care Unit Admission and In-hospital Mortality Among Hospitalized Adults Identified through the US Coronavirus Disease 2019 (COVID-19)-Associated Hospitalization Surveillance Network (COVID-NET). Clin Infect Dis. 2021;72:e206-e214. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 238] [Cited by in RCA: 450] [Article Influence: 90.0] [Reference Citation Analysis (0)] |
| 2. | Nassar M, Nso N, Alfishawy M, Novikov A, Yaghi S, Medina L, Toz B, Lakhdar S, Idrees Z, Kim Y, Gurung DO, Siddiqui RS, Zheng D, Agladze M, Sumbly V, Sandhu J, Castillo FC, Chowdhury N, Kondaveeti R, Bhuiyan S, Perez LG, Ranat R, Gonzalez C, Bhangoo H, Williams J, Osman AE, Kong J, Ariyaratnam J, Mohamed M, Omran I, Lopez M, Nyabera A, Landry I, Iqbal S, Gondal AZ, Hassan S, Daoud A, Baraka B, Trandafirescu T, Rizzo V. Current systematic reviews and meta-analyses of COVID-19. World J Virol. 2021;10:182-208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (1)] |
| 3. | Nassar M, Nso N, Ariyaratnam J, Sandhu J, Mohamed M, Baraka B, Ibrahim A, Alfishawy M, Zheng D, Bhangoo H, Soliman KM, Li M, Rizzo V, Daoud A. Coronavirus disease 2019 and renal transplantation. World J Clin Cases. 2021;9:7986-7997. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Murphy D, McCulloch CE, Lin F, Banerjee T, Bragg-Gresham JL, Eberhardt MS, Morgenstern H, Pavkov ME, Saran R, Powe NR, Hsu CY; Centers for Disease Control and Prevention Chronic Kidney Disease Surveillance Team. Trends in Prevalence of Chronic Kidney Disease in the United States. Ann Intern Med. 2016;165:473-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 383] [Cited by in RCA: 452] [Article Influence: 45.2] [Reference Citation Analysis (0)] |
| 5. | Dalrymple LS, Mu Y, Nguyen DV, Romano PS, Chertow GM, Grimes B, Kaysen GA, Johansen KL. Risk Factors for Infection-Related Hospitalization in In-Center Hemodialysis. Clin J Am Soc Nephrol. 2015;10:2170-2180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Hsu CM, Weiner DE, Aweh G, Miskulin DC, Manley HJ, Stewart C, Ladik V, Hosford J, Lacson EC, Johnson DS, Lacson E Jr. COVID-19 Among US Dialysis Patients: Risk Factors and Outcomes From a National Dialysis Provider. Am J Kidney Dis. 2021;77:748-756.e1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 114] [Cited by in RCA: 177] [Article Influence: 35.4] [Reference Citation Analysis (0)] |
| 7. | Chan L, Chaudhary K, Saha A, Chauhan K, Vaid A, Zhao S, Paranjpe I, Somani S, Richter F, Miotto R, Lala A, Kia A, Timsina P, Li L, Freeman R, Chen R, Narula J, Just AC, Horowitz C, Fayad Z, Cordon-Cardo C, Schadt E, Levin MA, Reich DL, Fuster V, Murphy B, He JC, Charney AW, Böttinger EP, Glicksberg BS, Coca SG, Nadkarni GN; Mount Sinai COVID Informatics Center (MSCIC). AKI in Hospitalized Patients with COVID-19. J Am Soc Nephrol. 2021;32:151-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 502] [Cited by in RCA: 502] [Article Influence: 100.4] [Reference Citation Analysis (0)] |
| 8. | Gabarre P, Dumas G, Dupont T, Darmon M, Azoulay E, Zafrani L. Acute kidney injury in critically ill patients with COVID-19. Intensive Care Med. 2020;46:1339-1348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 261] [Cited by in RCA: 345] [Article Influence: 57.5] [Reference Citation Analysis (0)] |
| 9. | Kurzhagen JT, Dellepiane S, Cantaluppi V, Rabb H. AKI: an increasingly recognized risk factor for CKD development and progression. J Nephrol. 2020;33:1171-1187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 147] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 10. | Lugon JR, Neves PDMM, Pio-Abreu A, do Nascimento MM, Sesso R; COVID-19 HD-Brazil Investigators. Evaluation of central venous catheter and other risk factors for mortality in chronic hemodialysis patients with COVID-19 in Brazil. Int Urol Nephrol. 2022;54:193-199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 11. | Savino M, Santhakumaran S, Currie CSM, Onggo BSS, Evans KM, Medcalf JF, Nitsch D, Steenkamp R. Comparison of Outcomes of In-Centre Haemodialysis Patients between the 1st and 2nd COVID-19 Outbreak in England, Wales, and Northern Ireland: A UK Renal Registry Analysis. Nephron. 2022;1-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | UK Cit. Cases in the UK Coronavirus in the UK 2022 [cited May 5, 2022]. Available from: https://coronavirus.data.gov.uk/details/cases. |
| 13. | De Meester J, De Bacquer D, Naesens M, Meijers B, Couttenye MM, De Vriese AS; NBVN Kidney Registry Group. Incidence, Characteristics, and Outcome of COVID-19 in Adults on Kidney Replacement Therapy: A Regionwide Registry Study. J Am Soc Nephrol. 2021;32:385-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 114] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 14. | Keller N, Chantrel F, Krummel T, Bazin-Kara D, Faller AL, Muller C, Nussbaumer T, Ismer M, Benmoussa A, Brahim-Bouna M, Beier S, Perrin P, Hannedouche T. Impact of first-wave COronaVIrus disease 2019 infection in patients on haemoDIALysis in Alsace: the observational COVIDIAL study. Nephrol Dial Transplant. 2020;35:1338-1411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 15. | Marino C, Angelici L, Pistolesi V, Morabito S, Di Napoli A, Calandrini E, Cascini S, Bargagli AM, Petrosillo N, Agabiti N, Davoli M, On Behalf Of The Regional Registry Dialysis And Transplant Lazio Region. SARS-CoV-2 Infection in Patients on Dialysis: Incidence and Outcomes in the Lazio Region, Italy. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Ozturk S, Turgutalp K, Arici M, Odabas AR, Altiparmak MR, Aydin Z, Cebeci E, Basturk T, Soypacaci Z, Sahin G, Elif Ozler T, Kara E, Dheir H, Eren N, Suleymanlar G, Islam M, Ogutmen MB, Sengul E, Ayar Y, Dolarslan ME, Bakirdogen S, Safak S, Gungor O, Sahin I, Mentese IB, Merhametsiz O, Oguz EG, Genek DG, Alpay N, Aktas N, Duranay M, Alagoz S, Colak H, Adibelli Z, Pembegul I, Hur E, Azak A, Taymez DG, Tatar E, Kazancioglu R, Oruc A, Yuksel E, Onan E, Turkmen K, Hasbal NB, Gurel A, Yelken B, Sahutoglu T, Gok M, Seyahi N, Sevinc M, Ozkurt S, Sipahi S, Bek SG, Bora F, Demirelli B, Oto OA, Altunoren O, Tuglular SZ, Demir ME, Ayli MD, Huddam B, Tanrisev M, Bozaci I, Gursu M, Bakar B, Tokgoz B, Tonbul HZ, Yildiz A, Sezer S, Ates K. Mortality analysis of COVID-19 infection in chronic kidney disease, haemodialysis and renal transplant patients compared with patients without kidney disease: a nationwide analysis from Turkey. Nephrol Dial Transplant. 2020;35:2083-2095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 149] [Cited by in RCA: 153] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 17. | Times NY. Covid in the US: Latest Maps, Case and Death Counts: The New York Times; 2022 [cited May 5, 2022]. Available from: https://www.nytimes.com/interactive/2021/us/covid-cases.html. |
| 18. | Fisher M, Yunes M, Mokrzycki MH, Golestaneh L, Alahiri E, Coco M. Chronic Hemodialysis Patients Hospitalized with COVID-19: Short-term Outcomes in the Bronx, New York. Kidney360. 2020;1:755-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 51] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 19. | Turgutalp K, Ozturk S, Arici M, Eren N, Gorgulu N, Islam M, Uzun S, Sakaci T, Aydin Z, Sengul E, Demirelli B, Ayar Y, Altiparmak MR, Sipahi S, Mentes IB, Ozler TE, Oguz EG, Huddam B, Hur E, Kazancioglu R, Gungor O, Tokgoz B, Tonbul HZ, Yildiz A, Sezer S, Odabas AR, Ates K. Determinants of mortality in a large group of hemodialysis patients hospitalized for COVID-19. BMC Nephrol. 2021;22:29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 47] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 20. | Bhinder OS, Swarnim S, Mantan M, Dabas A, Ahlawat RS. Chronic Kidney Disease and COVID-19: Outcomes of hospitalised adults from a tertiary care centre in North India. Med J Armed Forces India. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Hakami A, Badedi M, Elsiddig M, Nadeem M, Altherwi N, Rayani R, Alhazmi A. Clinical Characteristics and Early Outcomes of Hospitalized COVID-19 Patients with End-Stage Kidney Disease in Saudi Arabia. Int J Gen Med. 2021;14:4837-4845. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Sinha S, Swami R, Shakir A, Salman Ali S, Bansode J, Mehta K. Clinical Profile and Outcome of Hemodialysis Patients with SARS COV2 Infection in a Tertiary Care Centre in Mumbai, India. Indian J Nephrol. 2021;31:442-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Naaraayan A, Nimkar A, Hasan A, Pant S, Durdevic M, Elenius H, Nava Suarez C, Basak P, Lakshmi K, Mandel M, Jesmajian S. End-Stage Renal Disease Patients on Chronic Hemodialysis Fare Better With COVID-19: A Retrospective Cohort Study From the New York Metropolitan Region. Cureus. 2020;12:e10373. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Lamech TM, Nithya G, Aiswarya D, Gopalakrishnan N, Vathsalyan P, Sajmi S, Goutham K, Krishna R, Dineshkumar T, Sakthirajan R, Dhanapriya J, Padmaraj R. Clinical Profile and Outcomes of Coronavirus Disease 2019 (COVID-19) in Patients Undergoing Hemodialysis. Indian J Nephrol. 2022;32:16-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Goffin E, Candellier A, Vart P, Noordzij M, Arnol M, Covic A, Lentini P, Malik S, Reichert LJ, Sever MS, Watschinger B, Jager KJ, Gansevoort RT; ERACODA Collaborators. COVID-19-related mortality in kidney transplant and haemodialysis patients: a comparative, prospective registry-based study. Nephrol Dial Transplant. 2021;36:2094-2105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 69] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 26. | Singh AK, Gupta R, Ghosh A, Misra A. Diabetes in COVID-19: Prevalence, pathophysiology, prognosis and practical considerations. Diabetes Metab Syndr. 2020;14:303-310. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 581] [Cited by in RCA: 482] [Article Influence: 80.3] [Reference Citation Analysis (1)] |
| 27. | Varghese B, Raja N, Rajagopalan A, Arunachalam J, Durai R, Prasath A, Kumar S, Velu S. Clinical Characteristics and Short-Term Outcomes of ESKD Patients Undergoing Hemodialysis with COVID-19 Infection in Madurai, South India. Turkish J Nephrol. 2022;31. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 28. | Hendra H, Vajgel G, Antonelou M, Neradova A, Manson B, Clark SG, Kostakis ID, Caplin B, Salama AD. Identifying prognostic risk factors for poor outcome following COVID-19 disease among in-centre haemodialysis patients: role of inflammation and frailty. J Nephrol. 2021;34:315-323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 29. | Malik P, Patel U, Mehta D, Patel N, Kelkar R, Akrmah M, Gabrilove JL, Sacks H. Biomarkers and outcomes of COVID-19 hospitalisations: systematic review and meta-analysis. BMJ Evid Based Med. 2021;26:107-108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 376] [Cited by in RCA: 403] [Article Influence: 80.6] [Reference Citation Analysis (0)] |
| 30. | Ruiz-Sánchez JG, Núñez-Gil IJ, Cuesta M, Rubio MA, Maroun-Eid C, Arroyo-Espliguero R, Romero R, Becerra-Muñoz VM, Uribarri A, Feltes G, Trabattoni D, Molina M, García Aguado M, Pepe M, Cerrato E, Alfonso E, Castro Mejía AF, Roubin SR, Buzón L, Bondia E, Marin F, López Pais J, Abumayyaleh M, D'Ascenzo F, Rondano E, Huang J, Fernandez-Perez C, Macaya C, de Miguel Novoa P, Calle-Pascual AL, Estrada Perez V, Runkle I; HOPE COVID-19 investigators. Prognostic Impact of Hyponatremia and Hypernatremia in COVID-19 Pneumonia. A HOPE-COVID-19 (Health Outcome Predictive Evaluation for COVID-19) Registry Analysis. Front Endocrinol (Lausanne). 2020;11:599255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 72] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 31. | Amin A, Moon R, Agiro A, Rosenthal N, Brown H, Legg R, Pottorf W. In-hospital mortality, length of stay, and hospitalization cost of COVID-19 patients with and without hyperkalemia. Am J Med Sci. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Urology and nephrology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Badri M, Iran; Wang MK, China A-Editor: Yao QG, China S-Editor: Ma YJ L-Editor: A P-Editor: Li X