Published online Feb 19, 2026. doi: 10.5498/wjp.v16.i2.111196
Revised: October 15, 2025
Accepted: November 10, 2025
Published online: February 19, 2026
Processing time: 156 Days and 22.7 Hours
Anxiety and depression are significant contributors to adverse outcomes in patients with colon cancer (CC). Therefore, investigating the key determinants of this psychological distress in such patients is essential.
To examine the correlation of anxiety/depression status with stress-related mar
The study enrolled 120 patients with CC treated at the Affiliated Yongchuan Hos
The analysis revealed prevalence rates of 30.00% for anxiety and 38.33% for depression among the 120 patients with CC, of whom 51.67% exhibited either condition, and 16.67% showed comorbidity. Both groups showed an initial increase in HSP70, CRP, and BFI-C followed by a decrease compared with those at T0, with the anxie
A subset of patients with CC exhibits anxiety and depressive symptoms, which are significantly positively correlated with stress-related markers and CRF. Moreover, patients with CC, female patients, those aged 60 years or older, and patients diagnosed with stage III-IV tumors are more prone to anxiety or depression.
Core Tip: Focusing on patients with colon cancer (CC; n = 120), this study comprehensively explored psychological and clinical correlates. Results indicated anxiety/depression in over 50% of patients with CC, with symptoms primarily falling into the mild category. Notably, anxiety and depression correlated significantly and positively with stress-related factors (heat shock protein 70 and C-reactive protein) and cancer-induced fatigue. Moreover, certain clinical features—specifically being female, being 60 years old or older, and having a stage III or IV tumor—were confirmed to increase the risk of patients with CC to developing anxiety or depression. These results offer valuable evidence-based support for clinical practice, such as screening for psychological distress, classifying patients by risk level, and implementing tailored psychological support for patients with CC.
- Citation: Zhao L, Jian B, Chen DH. Correlation of anxiety/depression status with stress-related markers and cancer-related fatigue in patients with colon cancer. World J Psychiatry 2026; 16(2): 111196
- URL: https://www.wjgnet.com/2220-3206/full/v16/i2/111196.htm
- DOI: https://dx.doi.org/10.5498/wjp.v16.i2.111196
Colon cancer (CC), a major subtype of colorectal cancer (CRC), ranks as the third most commonly diagnosed malignancy worldwide and the second leading cause of cancer-related deaths, particularly affecting older adults[1]. Approximately 1.4 million new CC cases are recorded annually, constituting nearly 15% of all cancer diagnoses, with persistently high mortality rates[2]. Accumulating evidence shows that unhealthy lifestyle habits, such as obesity, alcohol intake, tobacco smoking, and poor dietary patterns, can increase the risk of CC development. Addressing these risk factors and improving health management may help prevent CC onset[3]. The primary treatment modalities for CC currently include surgery, chemotherapy, and radiotherapy. Although these methods are continually being optimized, patients often experience adverse effects, such as fatigue and gastrointestinal symptoms (e.g., abdominal pain, diarrhea, nausea, and vomiting)[4,5]. These physical manifestations often precipitate or exacerbate psychological comorbidities, particularly anxiety disorders, depressive moods, and cancer-related distress regarding recurrence or progression[6]. Studies have established a connection between high anxiety levels and increased risks of tumor recurrence and metastatic spread (including CC) as well as more frequent hospital readmissions[7,8]. Depression in populations with cancer, including CC, has been linked to a series of adverse events, such as diminished treatment compliance, dysregulated immune function, amplified inflammatory responses, and reduced overall survival[9]. The psychological distress experienced by patients with CC acts as a stressor, further exacerbating tumor burden and accelerating disease progression. This negative interaction can interfere with patient treatment, compromising therapeutic efficacy and hindering post-therapeutic rehabilitation[10,11].
Thus, this study aimed to clarify the interplay between anxiety/depression and stress-related markers as well as cancer-related fatigue (CRF) in patients with CC while identifying potential contributors to the development of anxiety and depression in this population. Given the paucity of robust clinical data in this research topic, our findings may con
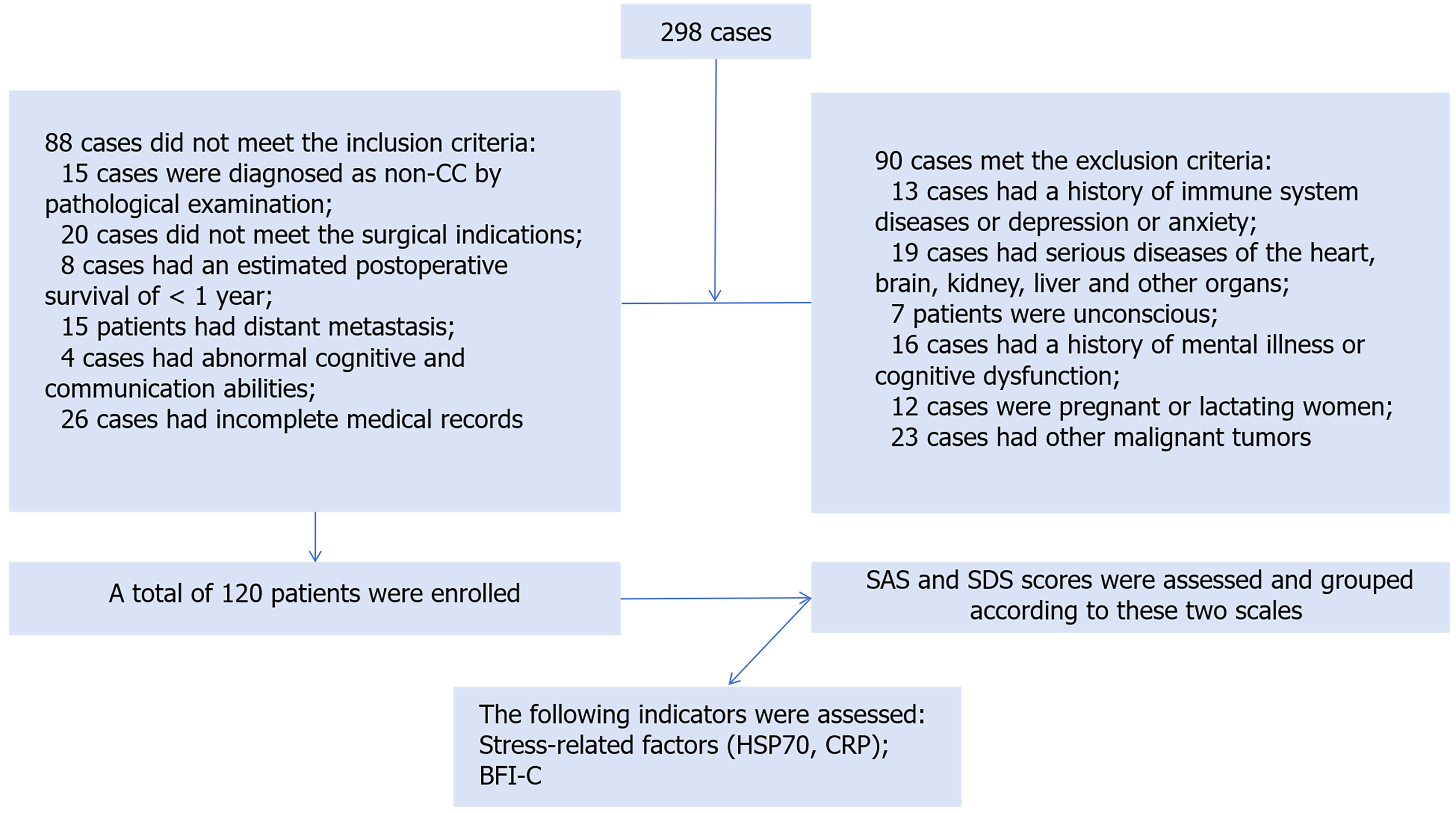
This study enrolled 120 patients with CC admitted to the Affiliated Yongchuan Hospital of Chongqing Medical University from February 2022 to February 2025 and stratified them into two groups based on psychological evaluation results using the Self-Rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS). The observation group (n = 62) exhibited clinically significant anxiety or depression (SAS ≥ 50 or SDS ≥ 53), whereas the control group (n = 58) had no psychological symptoms. Figure 1 depicts the patient enrollment process across all stages.
Inclusion criteria: (1) Histopathologically confirmed CC[12]; (2) Surgical eligibility[13]; (3) Expected postoperative survival ≥ 12 months; (4) Absence of distant metastasis; (5) Intact cognitive and communicative functions; and (6) Available and complete case data.
Exclusion criteria: (1) Preexisting immune disorders or depression/anxiety; (2) Significant comorbidities involving the heart, brain, kidneys, liver, or other organs; (3) Impaired consciousness, severe cardiopulmonary insufficiency, or organic brain lesions; (4) Pregnancy or lactation status; or (5) Coexisting malignancies.
Anxiety/depression: Psychological status assessments were performed preoperatively using the SAS and SDS scales[14], two commonly employed tools with established reliability and validity. Based on their subjective feelings, participants provided a 1-4 rating for each of the 20 items in these scales. A raw score was derived from the sum of the item scores and then converted to a standard score using a multiplier of 1.25. Based on clinical evaluation criteria, the scoring is interpreted as follows: SAS (anxiety severity): < 50, within the normal range; 50-59, mild anxiety symptoms; 60-69, moderate anxiety; and ≥ 70, severe anxiety. SDS (depression level): < 53, within the normal range; 53-62, mild; 63-72, moderate; and ≥ 73, severe.
Stress-related markers: Fasting venous blood samples (5 mL) were obtained from the antecubital vein before the surgical procedure (T0), as well as 3 (T1) and 7 (T2) days afterward. Following centrifugation, serum concentrations of heat shock protein 70 (HSP70) and C-reactive protein (CRP) were quantified using the enzyme-linked immunosorbent assay technique. This assay is a sensitive and specific analytical method based on immunoassay principles. It capitalizes on the precise interaction between antibodies and antigens to detect a target protein. Then, its concentration is determined by measuring the signal produced in an enzymatic reaction, typically observable as a colorimetric change. Under normal conditions, circulating CRP remains under 3-5 mg/L. Its elevation in the 10-100 mg/L range often reflects moderate inflammatory processes, tissue damage, or localized infections. Values > 100 mg/L are strongly indicative of severe bacterial infection or systemic inflammation[15]. By comparison, HSP70 is present at baseline levels of 0.1-10 ng/mL, with increases observed during periods of physiological stress[16].
CRF: Its level was measured using the validated Brief Fatigue Inventory-Chinese version (BFI-C)[17]. This nine-item measure employs a 0-10 numerical rating scale for each item. The overall fatigue score was calculated by averaging all nine responses, with high scores reflecting more severe fatigue symptoms.
Questionnaires were distributed by investigators from our institution who had received standardized training. Questionnaires were, in principle, completed independently by study participants. For individuals unable to self-report because of specific limitations, the investigators administered standardized interviews, asking each question verbatim and ob
Data were processed using IBM SPSS Statistics version 26.0 (IBM Corp., Armonk, NY, United States). Categorical variables were presented as frequencies and percentages [n (%)], whereas continuous variables were reported as mean ± SE of the mean. For categorical data, group comparisons utilized the χ2 test. For continuous variables, independent samples t-tests were applied to identify between-group differences, whereas multiple timepoint analyses were conducted using repeated measures analysis of variance. Pearson or Spearman correlation analysis examined associations between anxiety/depression levels in patients with CC and biomarkers (HSP70 and CRP) as well as fatigue scale scores. Univariate and multivariate binary logistic regression models identified factors that influence anxiety or depressive states. A significance threshold of P < 0.05 was applied for all statistical tests. The sample size was determined in two steps: (1) A preliminary calculation, guided by the intention to include seven variables in the multivariable modeling and the events per variable (EPV) ≥ 10 principle, indicated a need for 156 subjects; and (2) A subsequent adjustment to 120 participants was made, considering practical research constraints and patient recruitment timelines. Power analysis confirmed that with an expected anxiety and depression prevalence of 50% (yielding approximately 60 events), the lower sample size still provides an EPV of 8.57, exceeding the EPV > 5 benchmark.
Among the 120 patients with CC, the mean SAS score was 45.58 ± 8.72, with 30.00% meeting the criteria for anxiety. Depression metrics showed a mean SDS score of 51.02 ± 7.64, affecting 38.33% of the study population. Overall, over half (51.67%) screened positive for either condition, whereas concurrent anxiety and depression were observed in 16.67% (Table 1).
| Category | n = 120 |
| SAS (points) | 45.58 ± 8.72 |
| Normal (< 50) | 84 (70.00) |
| Mild (50-59) | 31 (25.83) |
| Moderate (60-69) | 5 (4.17) |
| Severe (≥ 70) | 0 (0.00) |
| SDS (points) | 51.02 ± 7.64 |
| Normal (< 53) | 74 (61.67) |
| Mild (53-62) | 37 (30.83) |
| Moderate (63-72) | 9 (7.50) |
| Severe (≥ 73) | 0 (0.00) |
| Anxiety or depression | 62 (51.67) |
| Anxiety and depression | 20 (16.67) |
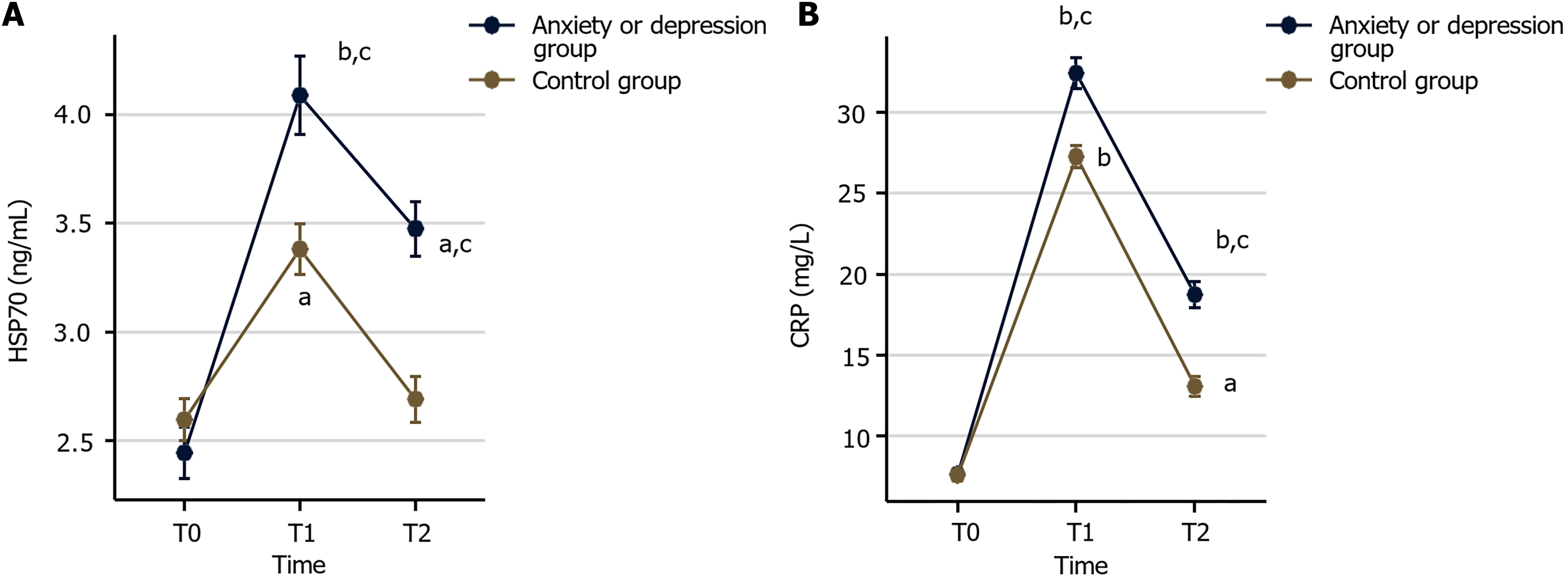
Using established cutoff values of SAS ≥ 50 or SDS ≥ 53, the participants were categorized into either an anxiety/depression group (n = 62) or a control group (n = 58). Stress-related biomarkers, including HSP70 and CRP, were measured preoperatively (T0), 3 days postoperatively (T1), and 7 days postoperatively (T2). No significant differences were observed between the groups at baseline (T0, P > 0.05). However, at T1 and T2, both biomarkers displayed an initial rise followed by a decline, with significantly higher levels in the anxiety/depression group than the control group (P < 0.05; Figure 2).
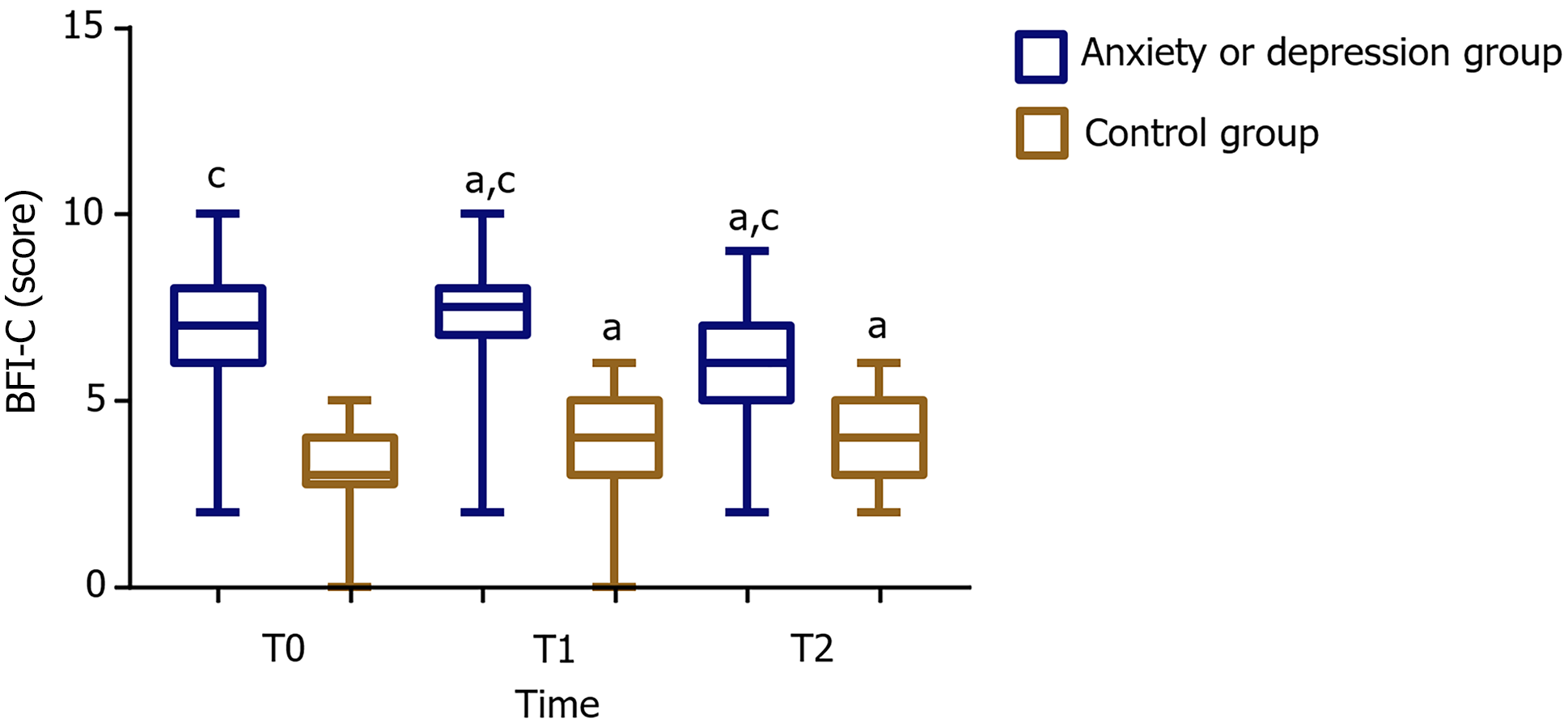
In both cohorts, CRF was longitudinally assessed using the BFI-C scale across three measurement intervals. Comparative analysis revealed consistently high BFI-C scores in the anxiety/depression group relative to that in the control group at all time points (P < 0.05). In addition, both groups exhibited a characteristic pattern of initial score elevation (T1-T2) followed by subsequent reduction when compared with baseline (T0), with these temporal variations reaching significance (P < 0.05; Figure 3).
A Pearson or Spearman correlation analysis was conducted to examine the relationships among anxiety symptoms, stress-related biomarkers, and CRF. The results revealed significant positive correlations between SAS scores and HSP70 (r = 0.379), CRP (r = 0.299), and BFI-C (r = 0.398), all reaching significance (P < 0.001; Table 2).
| Category | SAS (points) | SDS (points) | ||
| r value | P value | r value | P value | |
| HSP70 (ng/mL) | 0.379 | < 0.001 | 0.287 | 0.002 |
| CRP (mg/L) | 0.299 | < 0.001 | 0.331 | < 0.001 |
| BFI-C (points) | 0.398 | < 0.001 | 0.283 | 0.002 |
Similarly, Pearson’s or Spearman’s correlation was employed to assess the connections among depressive symptoms, stress-related markers, and CRF levels in patients with CC. The analysis demonstrated significant (P < 0.01) positive associations between depression scores (SDS) and the following variables: HSP70 (r = 0.287), CRP (r = 0.331), and fatigue severity (BFI-C; r = 0.283; Table 2).
Univariate analysis demonstrated significant associations between anxiety/depression and sex, age, marital status, monthly household income, tumor stage, and comorbidities (P < 0.05). In contrast, education level, employment status and surgical approach did not exhibit significant relationships (P > 0.05).
Subsequent multivariate logistic regression confirmed that female sex [odds ratio (OR) = 2.755], older age (OR = 2.649), and advanced tumor stage (OR = 2.349) independently predicted higher anxiety/depression risk in this patient population (P < 0.05). Table 3 (univariate analysis) and Table 4 (multivariate analysis) present detailed results.
| Factors | n | Anxiety/depression group (n = 62) | Control group (n = 58) | χ2 | P value |
| Gender | 6.318 | 0.012 | |||
| Male | 73 | 31 (50.00) | 42 (72.41) | ||
| Female | 47 | 31 (50.00) | 16 (27.59) | ||
| Age (years) | 9.522 | 0.002 | |||
| < 60 | 55 | 20 (32.26) | 35 (60.34) | ||
| ≥ 60 | 65 | 42 (67.74) | 23 (39.66) | ||
| Marital status | 6.541 | 0.011 | |||
| Married | 96 | 48 (77.42) | 48 (82.76) | ||
| Unmarried/widowed/divorced | 24 | 14 (22.58) | 10 (17.24) | ||
| Educational level | 0.534 | 0.465 | |||
| < High school | 85 | 44 (70.97) | 41 (70.69) | ||
| ≥ High school | 35 | 18 (29.03) | 17 (29.31) | ||
| Employment status | 0.769 | 0.381 | |||
| Employed | 53 | 25 (40.32) | 28 (48.28) | ||
| Retired | 67 | 37 (59.68) | 30 (51.72) | ||
| Monthly household income (RMB) | 4.097 | 0.043 | |||
| < 4000 | 83 | 48 (77.42) | 35 (60.34) | ||
| ≥ 4000 | 37 | 14 (22.58) | 23 (39.66) | ||
| Surgical approach | 2.157 | 0.340 | |||
| Dixon operation | 36 | 20 (32.26) | 16 (27.59) | ||
| Miles operation | 67 | 31 (50.00) | 36 (62.07) | ||
| Sphincter-preserving surgery | 17 | 11 (17.74) | 6 (10.34) | ||
| Tumor stage | 6.486 | 0.011 | |||
| II | 58 | 23 (37.10) | 35 (60.34) | ||
| III-IV | 62 | 39 (62.90) | 23 (39.66) | ||
| Comorbidities | 3.922 | 0.048 | |||
| No | 53 | 22 (35.48) | 31 (53.45) | ||
| Yes | 67 | 40 (64.52) | 27 (46.55) |
| Category | B | SE | Wald | P value | Exp(B) | 95%CI |
| Gender | 1.014 | 0.424 | 5.725 | 0.017 | 2.755 | 1.201-6.320 |
| Age (years) | 0.974 | 0.417 | 5.455 | 0.020 | 2.649 | 1.170-6.001 |
| Marital status | 0.227 | 0.513 | 0.196 | 0.658 | 1.255 | 0.459-3.433 |
| Monthly household income (RMB) | -0.805 | 0.455 | 3.134 | 0.077 | 0.447 | 0.183-1.090 |
| Tumor stage | 0.854 | 0.411 | 4.320 | 0.038 | 2.349 | 1.050-5.254 |
| Comorbidities | 0.418 | 0.420 | 0.991 | 0.319 | 1.520 | 0.667-3.463 |
The prevalence of anxiety and depression in patients with advanced tumors can be as high as 85.0%[18]. These adverse psychological states can significantly alter treatment outcomes, diminish quality of life, and undermine patients’ confidence in battling the disease, including those diagnosed with CC[19]. To mitigate the effects of such psychological distress, thoroughly analyzing and identifying key factors contributing to anxiety and depression in patients with CC are essential.
In this study involving 120 participants, the observed rates of anxiety and depression were 30.00% and 38.33%, respectively. These findings align with the results of a systematic review by Peng et al[20], which reported anxiety rates ranging from 1.0% to 47.2% and depression rates ranging from 1.6% to 57.0%. HSP70, a 70-kDa molecular chaperone in essence, takes on crucial roles in stress responses, apoptosis, and inflammation associated with tumors. Additionally, it has been implicated in the pathophysiological mechanisms of CRC and is considered a potential therapeutic target[21,22]. Similarly, CRP is linked to inflammatory stress induced by malignancies, other diseases, and stress responses triggered by surgical interventions[23,24]. Consequently, this study investigated stress-related markers represented by HSP70 and CRP. After T0, the anxiety/depression and control groups demonstrated similar dynamic patterns in these stress mar
In this study, the BFI-C scores of patients who underwent surgery in both groups followed a similar trend, rising initially before declining. Moreover, the anxiety/depression group demonstrated significantly higher CRF severity than the control group at all measurement points. Correlation analysis established significant positive correlations between SAS/SDS scores and HSP70, CRP, and BFI-C levels in patients with CC, proposing an intimate relationship between the psychological state of these patients and their physiological stress response, as well as fatigue levels. Supporting evidence comes from the study by Renna et al[28], whose findings of an association among mood disorders (anxiety/depression), high CRP levels, and fatigue in patients with CRC corroborate the results of the present study. Initial univariate screening revealed several demographic and clinical factors (sex, age, marital status, monthly household income, tumor stage, and comorbidities) showing significant associations (P < 0.05) with anxiety and depression in patients with CC. Subsequent multivariate modeling identified sex, age, and tumor stage as robust independent predictors for psychological distress in such patients. These findings find partial resonance in the study by Zhang et al[29], who similarly reported female sex, single/divorced status, advanced age ≥ 60 years, rural residence, and disease severity indirectly influencing anxiety and depression in patients with CRC receiving postoperative adjuvant chemotherapy. Additionally, Braamse et al[30] highlighted sex (female) and comorbidity burden as critical contributors to anxiety and depression in CRC survivors, which complements the findings of this study.
This research has certain limitations. First, the investigation was confined to patients with CC from one healthcare institution, which may lead to limited sample diversity and geographical bias. To enhance data representativeness, future studies could broaden the sampling range across multiple medical facilities. Second, several potentially significant variables, including psychological resilience, self-efficacy, social support, and personality traits, were not examined. Incorporating these parameters in subsequent research would enable more thorough evaluation outcomes. Third, combining individuals with either anxiety or depression into a unified group could limit insights into subgroup differences. Although this merging is supported by the frequent co-occurrence and overlapping neurobiology of these conditions and boosts statistical power, it potentially overlooks variations specific to those with solely anxiety, solely depression, or both disorders. Fourth, the analysis lacked an in-depth exploration of the causal links connecting anxiety/depression severity with stress-related factors or CRF. Thus, further longitudinal follow-up studies would help elucidate the complex interactions among these elements.
This study revealed that > 50% of patients with CC exhibited signs of anxiety or depression, primarily mild. Furthermore, a strong positive association was observed between the psychological condition of these patients and stress-related markers HSP70 and CRP, as well as CRF. This study also revealed that female patients, those aged > 60, and individuals diagnosed with stage III-IV CC have higher vulnerability to anxiety or depression.
| 1. | Guan Y, Yao W, Yu H, Feng Y, Zhao Y, Zhan X, Wang Y. Chronic stress promotes colorectal cancer progression by enhancing glycolysis through β2-AR/CREB1 signal pathway. Int J Biol Sci. 2023;19:2006-2019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 42] [Reference Citation Analysis (0)] |
| 2. | Bourakkadi Idrissi M, El Bouhaddouti H, Mouaqit O, Ousadden A, Ait Taleb K, Benjelloun EB. Left-Sided Colon Cancer and Right-Sided Colon Cancer: Are They the Same Cancer or Two Different Entities? Cureus. 2023;15:e37563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 3. | Roshandel G, Ghasemi-Kebria F, Malekzadeh R. Colorectal Cancer: Epidemiology, Risk Factors, and Prevention. Cancers (Basel). 2024;16:1530. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 177] [Reference Citation Analysis (1)] |
| 4. | Shinji S, Yamada T, Matsuda A, Sonoda H, Ohta R, Iwai T, Takeda K, Yonaga K, Masuda Y, Yoshida H. Recent Advances in the Treatment of Colorectal Cancer: A Review. J Nippon Med Sch. 2022;89:246-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 142] [Reference Citation Analysis (2)] |
| 5. | Taieb J, Lonardi S, Desai J, Folprecht G, Gallois C, Marques EP, Khan S, Castagné C, Wasan H. Adverse Events Associated with Encorafenib Plus Cetuximab in Patients with BRAFV600E-mutant Metastatic Colorectal Cancer: An in-depth Analysis of the BEACON CRC Study. Clin Colorectal Cancer. 2023;22:59-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 6. | Kaisinova AS, Achabaeva AB, Uzdenov MB, Dzhanibekova AA, Kaitova MM, Illarionov VE, Suvorov AY. [Exercise therapy in outpatient rehabilitation programmes for patients with comorbid digestive pathology in colon cancer and chronic pancreatitis. (Open randomized controlled trial)]. Vopr Kurortol Fizioter Lech Fiz Kult. 2024;101:5-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Dong Q, Wang T, Bu X, Chen L, Zhong F, Liu C. Latent profile analysis of anxiety, depression, and resilience among elderly colorectal cancer patients in China. Sci Rep. 2025;15:14897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 8. | Wang X, Wang N, Zhong L, Wang S, Zheng Y, Yang B, Zhang J, Lin Y, Wang Z. Prognostic value of depression and anxiety on breast cancer recurrence and mortality: a systematic review and meta-analysis of 282,203 patients. Mol Psychiatry. 2020;25:3186-3197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 275] [Cited by in RCA: 314] [Article Influence: 52.3] [Reference Citation Analysis (0)] |
| 9. | Walker J, Mulick A, Magill N, Symeonides S, Gourley C, Burke K, Belot A, Quartagno M, van Niekerk M, Toynbee M, Frost C, Sharpe M. Major Depression and Survival in People With Cancer. Psychosom Med. 2021;83:410-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 72] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 10. | Więckiewicz G, Weber S, Florczyk I, Gorczyca P. Socioeconomic Burden of Psychiatric Cancer Patients: A Narrative Review. Cancers (Basel). 2024;16:1108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 9] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 11. | Song JY, Cao J, Mao J, Wang JL. Effect of rapid rehabilitation nursing on improving clinical outcomes in postoperative patients with colorectal cancer. World J Gastrointest Surg. 2024;16:2119-2126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (12)] |
| 12. | Vogel JD, Felder SI, Bhama AR, Hawkins AT, Langenfeld SJ, Shaffer VO, Thorsen AJ, Weiser MR, Chang GJ, Lightner AL, Feingold DL, Paquette IM. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Management of Colon Cancer. Dis Colon Rectum. 2022;65:148-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 229] [Article Influence: 57.3] [Reference Citation Analysis (1)] |
| 13. | Engdahl J, Öberg A, Bech-Larsen S, Bergenfeldt H, Vedin T, Edelhamre M, Öberg S. Short- and long-term outcome after colon cancer resections performed by male and female surgeons: A single-center retrospective cohort study. Scand J Surg. 2024;113:131-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 14. | Wang P, Pang X, He M, Liu J. Effect of stepwise psychological intervention on improving adverse mood and quality of life after colon cancer surgery. Am J Transl Res. 2023;15:4055-4064. [PubMed] |
| 15. | Bakkaloglu OK, Sen G, Kepil N, Eskazan T, Kurt EA, Onal U, Candan S, Balamir M, Hatemi I, Erzin Y, Celik AF. Comparative Value of CRP and FCP for Endoscopic and Histologic Remissions in Ulcerative Colitis. Diagnostics (Basel). 2024;14:2283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Nakhjavani M, Morteza A, Khajeali L, Esteghamati A, Khalilzadeh O, Asgarani F, Outeiro TF. Increased serum HSP70 levels are associated with the duration of diabetes. Cell Stress Chaperones. 2010;15:959-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 100] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 17. | Liu D, Weng JS, Ke X, Wu XY, Huang ST. The relationship between cancer-related fatigue, quality of life and pain among cancer patients. Int J Nurs Sci. 2023;10:111-116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 27] [Reference Citation Analysis (0)] |
| 18. | Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10:19-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 21] [Reference Citation Analysis (0)] |
| 19. | Eseadi C, Ngwu MO. Significance of music therapy in treating depression and anxiety disorders among people with cancer. World J Clin Oncol. 2023;14:69-80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 15] [Reference Citation Analysis (7)] |
| 20. | Peng YN, Huang ML, Kao CH. Prevalence of Depression and Anxiety in Colorectal Cancer Patients: A Literature Review. Int J Environ Res Public Health. 2019;16:411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 117] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 21. | Alsaab HO, Almalki AH. Anti-HSP70 alleviates cell migration and proliferation in colorectal cancer cells (CRC) by targeting CXCR4 (in vitro study). Med Oncol. 2023;40:256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 22. | Singh MK, Han S, Ju S, Ranbhise JS, Ha J, Yeo SG, Kim SS, Kang I. Hsp70: A Multifunctional Chaperone in Maintaining Proteostasis and Its Implications in Human Disease. Cells. 2025;14:509. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 22] [Reference Citation Analysis (0)] |
| 23. | Osawa H, Nakamura N, Tsutaya C, Saitoh H, Shimada M, Murakami R, Fujita T, Narita-Kinjo I, Nagawa D, Nakata M, Yokota T, Ohyama C, Tomita H. Role of High-sensitivity C-reactive Protein in Future Cardiovascular Events in Hemodialysis Patients. In Vivo. 2024;38:1351-1358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 24. | Crippa J, Calini G, Santambrogio G, Sassun R, Siracusa C, Maggioni D, Mari G; AIMS Academy Clinical Research Network. ERAS Protocol Applied to Oncological Colorectal Mini-invasive Surgery Reduces the Surgical Stress Response and Improves Long-term Cancer-specific Survival. Surg Laparosc Endosc Percutan Tech. 2023;33:297-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 21] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 25. | Meng L, Jiang X, Liang J, Pan Y, Pan F, Liu D. Postoperative psychological stress and expression of stress-related factors HSP70 and IFN-γ in patients with early lung cancer. Minerva Med. 2023;114:43-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | Kennedy E, Niedzwiedz CL. The association of anxiety and stress-related disorders with C-reactive protein (CRP) within UK Biobank. Brain Behav Immun Health. 2022;19:100410. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 24] [Reference Citation Analysis (0)] |
| 27. | Tan Y, Zhou L, Huang J, Chen X, Wu Y, Song X, Wang J, Hu H, Yang Q. Vitamin B12, Folate, Homocysteine, Inflammatory Mediators (Interleukin-6, Tumor Necrosis Factor-α and C-Reactive Protein) Levels in Adolescents with Anxiety or Depressive Symptoms. Neuropsychiatr Dis Treat. 2023;19:785-800. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 28. | Renna ME, Shrout MR, Madison AA, Alfano CM, Povoski SP, Lipari AM, Carson WE 3rd, Malarkey WB, Kiecolt-Glaser JK. Depression and anxiety in colorectal cancer patients: Ties to pain, fatigue, and inflammation. Psychooncology. 2022;31:1536-1544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 43] [Reference Citation Analysis (0)] |
| 29. | Zhang MF, Zheng MC, Liu WY, Wen YS, Wu XD, Liu QW. The influence of demographics, psychological factors and self-efficacy on symptom distress in colorectal cancer patients undergoing post-surgical adjuvant chemotherapy. Eur J Oncol Nurs. 2015;19:89-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 30. | Braamse AM, van Turenhout ST, Terhaar Sive Droste JS, de Groot GH, van der Hulst RW, Klemt-Kropp M, Kuiken SD, Loffeld RJ, Uiterwaal MT, Mulder CJ, Dekker J. Factors associated with anxiety and depressive symptoms in colorectal cancer survivors. Eur J Gastroenterol Hepatol. 2016;28:831-835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/