Published online Jan 19, 2026. doi: 10.5498/wjp.v16.i1.109725
Revised: September 18, 2025
Accepted: November 7, 2025
Published online: January 19, 2026
Processing time: 133 Days and 22 Hours
Approximately 30% of patients with head and neck cancer experience adverse effects caused by anxiety and depression. Considering the high prevalence, imple
To evaluate the efficacy of cognitive behavioral therapy (CBT)-based psychological interventions in improving the psychological well-being and quality of life (QoL) of patients with laryngeal carcinoma.
This study enrolled 120 patients admitted from February 2022 to February 2024. The control group, comprising 50 participants, received standard supportive psy
The results demonstrated that the research group experienced superior outcomes, with significantly reduced durations of tracheostomy and nasogastric tube dependence, as well as shorter hospital stays, compared with the control group. Additionally, the research group exhibited markedly lower post-intervention Self-Rating Anxiety Scale, Self-Rating Depression Scale, Self-Rating Scale of Sleep, and Athens Insomnia Scale scores, along with minimal but higher change in serum albumin and hemoglobin levels compared with the control group. All five domains of Functional Assessment of Cancer Therapy-Head and Neck showed notable improvements in the research group, exceeding those observed in the control group.
CBT-based psychological support positively affects the mental well-being and QoL of patients with laryngeal carcinoma, highlighting its potential for broader clinical application.
Core Tip: This study primarily aimed to evaluate the efficacy of cognitive behavioral therapy-based psychological interventions in influencing the mental state and quality of life of 120 patients with laryngeal carcinoma. Through quan
- Citation: Tao HZ, Deng YM, Xia SF, Feng Y. Influence of cognitive behavioral therapy-based psychological interventions on psychological well-being and quality of life among laryngeal carcinoma patients. World J Psychiatry 2026; 16(1): 109725
- URL: https://www.wjgnet.com/2220-3206/full/v16/i1/109725.htm
- DOI: https://dx.doi.org/10.5498/wjp.v16.i1.109725
Laryngeal carcinoma (LC) accounts for 30%-40% of all head and neck malignancies and is the seventh most commonly diagnosed cancer globally[1]. The etiology of LC is complex and involves factors such as tobacco and alcohol consumption, unhealthy eating habits, dyslipidemia, gastroesophageal reflux disease, and Plummer-Vinson syndrome, among others. The clinical characteristics of LC include throat pain, hoarseness, dysphagia, and non-resolving lumps or ulcerations[2,3]. In 2022, the United States reported nearly 13000 new LC diagnoses and 3820 fatalities, reflecting a considerable mortality burden[4]. LC carries a risk of death and of complete or partial impairment in swallowing, mastication, respiration, and verbal communication. Additionally, the frequent and often severe disfiguration predisposes patients to anxiety and depression, thereby compromising mental well-being and overall quality of life (QoL)[5,6]. In additions to these triggers, concerns about disease outcomes, recurrence, and treatment response leads to clinically relevant mood disturbances in approximately 50% of head and neck cancer (including LC) cases[7,8]. Therefore, we propose imp
Conventional psychological protocols predominantly focus on disease-related education and basic emotional support[9]; however, cognitive behavioral therapy (CBT)-based psychological interventions comprise formulating personalized treatment plan, facilitating cognitive restructuring, and providing postoperative guidance and psychological support to address the root causes of patients’ psychological distress[10,11]. The therapeutic efficacy of CBT has been well docu
Research investigating the involvement of CBT-based interventions in the psychological well-being and QoL of patients with LC remains limited. Therefore, we hypothesize that CBT-based psych interventions have the potential to substantially improve mental health parameters and QoL indicators for these patients. Through rigorous validation, our research aims to boost their emotional well-being and overall QoL.
The inclusion criteria comprised patients with histologically confirmed LC[14]; who are above 18 years of age; scheduled for partial/total laryngectomy; eligible for first-line treatment; free of cognitive, communicative, or psychiatric disorders; and have complete clinical data. The exclusion criteria comprised patients with chronic pharmacotherapy-dependent conditions (e.g., essential hypertension, diabetes); severe systemic/organ dysfunction; a prior history of chemotherapy/radiotherapy; gastrointestinal disturbances; and coexisting malignant neoplasms. This study included 120 eligible patients with LC treated at Chongqing University Cancer Hospital from February 2022 to February 2024. The control group comprised 50 participants receiving standard supportive psychological care, and the research group included 70 participants undergoing CBT-based psychological interventions. Baseline characteristics insignificantly differed between the two groups (P > 0.05), ensuring comparable study populations.
The standard supportive psychological care provided to the control group consisted of disease-specific education (e.g., an overview of the condition, available treatments, potential risks during therapy, and preventive approaches) without any cognitive restructuring or behavioral training components. Additionally, the participants received basic psychological support, including active listening and guided emotional catharsis.
The research group underwent a CBT-based psychological intervention program comprising the following components. First, in addition to the standard disease education provided to the control group, the patients and families in the research group were introduced to CBT principles and were educated on how maladaptive thought patterns can negatively affect emotions, treatment adherence, and clinical outcomes. Considering the psychological burden of LC, patients frequently experience fear, anxiety, and distress during treatment, which can undermine their confidence in recovery, reduce treatment adherence, and ultimately impair postoperative rehabilitation and prognosis. The second component focused on enhancing disease awareness and recovery confidence. Patients and their families were provided interventions to alleviate anxiety and distress through education on LC-associated information, thereby improving their understanding of the disease. Patients received individualized psychological support tailored to their specific needs. The third component comprised psychological interventions for stress and negative emotion mitigation. This included guided relaxation techniques to alleviate stress by listening to music, taking warm baths, watching lighthearted movies, and ensuring adequate sleep. Additionally, clinicians employed therapeutic imagery to soothe mind by guiding patients to envision tranquil scenes, such as lounging in a sunlit meadow under clear blue skies, to induce peacefulness, serenity, and tranquility. Whole-body massage was also provided by therapists to relieve muscle tension, improve blood circu
Both groups successfully completed their respective psychological intervention courses. The intervention consisted of four sessions, each lasting 30-40 minutes, conducted over a 2-week period.
First, the postoperative recovery was assessed for both the groups by recording recovery outcomes that included the durations of tracheostomy and nasogastric tube dependence and length of hospital stay. Second, the pre-intervention and post-intervention psychological assessments for the mental state of the participants were conducted using the Self-Rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS)[15]. These 20-item questionnaires are rated on a 4-point scale. Standardized total scores (0-100 points) were obtained by multiplying raw scores by 1.25, with higher scores indicating increased anxiety or depressive symptoms. Third, nutritional status was evaluated pre- and post-intervention by measuring serum albumin (ALB) and hemoglobin (Hb) levels using the bromocresol green method and an automated hematology analyzer, respectively. Fourth, baseline and post-treatment sleep quality were assessed using the Self-Rating Scale of Sleep (SRSS) and the Athens Insomnia Scale (AIS). The SRSS (range: 10-50) uses an inverse scoring technique (lower scores = superior sleep quality)[16]. The AIS consists of 8 items, each scored from 0 (no difficulty) to 3 (severe difficulty), yielding total scores (0-24) that are directly proportional to the severity of insomnia. Fifth, QoL was evaluated pre-intervention and post-intervention using the Functional Assessment of Cancer Therapy-Head and Neck scale[17]. This 38-item questionnaire evaluates the physical, social/family, emotional, and functional well-being of the patients, along with head and neck cancer-specific symptoms. Items were rated on a 5-point Likert scale, yielding total scores from 0 to 156, with higher values indicating superior QoL.
In this study, measurement data were subjected to independent sample t-tests (between-group comparisons) or paired t-tests (pre-intervention vs post-intervention comparisons within groups). Categorical data [n (%)] were analyzed using χ2 tests. Statistical evaluations were performed in SPSS version 20.0, applying a two-tailed significance threshold of P-values < 0.05.
In the present study, outcome evaluators and data analysts were blinded. Researchers were not involved in assigning groups and remained unaware of the grouping strategy. They were responsible for assessing the outcomes that included administering scale evaluations, measuring laboratory markers (e.g., ALB, Hb), and documenting data (e.g., hospital stay duration). Another researcher, who had no knowledge of the assigned groups, managed the study’s data entry and statistical analysis. This workflow ensured blinding throughout the collection and processing of the data.
The Table 1 summarizes the baseline characteristics of the patients, demonstrating clinical comparability between the study groups. Attributes of the participants, including sex distribution, age, tumor stage, pathological type, education level, and other variables showed no statistically significant differences (P > 0.05).
| Factors | n | Control group (n = 50) | Research group (n = 70) | t/χ2 | P value |
| Gender | 0.192 | 0.661 | |||
| Male | 70 | 28 (56.00) | 42 (60.00) | ||
| Female | 50 | 22 (44.00) | 28 (40.00) | ||
| Age (years) | 120 | 50.52 ± 6.44 | 50.03 ± 7.26 | 0.382 | 0.703 |
| Tumor stage | 1.269 | 0.260 | |||
| I-II | 77 | 35 (70.00) | 42 (60.00) | ||
| III-IV | 43 | 15 (30.00) | 28 (40.00) | ||
| Pathological type | 0.323 | 0.851 | |||
| Glottic type | 69 | 30 (60.00) | 39 (55.71) | ||
| Supraglottic type | 32 | 12 (24.00) | 20 (28.57) | ||
| Subglottic type | 19 | 8 (16.00) | 11 (15.71) | ||
| Education level | 0.571 | 0.450 | |||
| < High school | 72 | 32 (64.00) | 40 (57.14) | ||
| ≥ High school | 48 | 18 (36.00) | 30 (42.86) |
The postoperative recovery of participants was assessed by comparing the duration of tracheotomy and nasogastric tube dependence and the length of hospital stay. As compared to the control group, the research group demonstrated statistically significant reductions across all three parameters (P < 0.05; Figure 1).
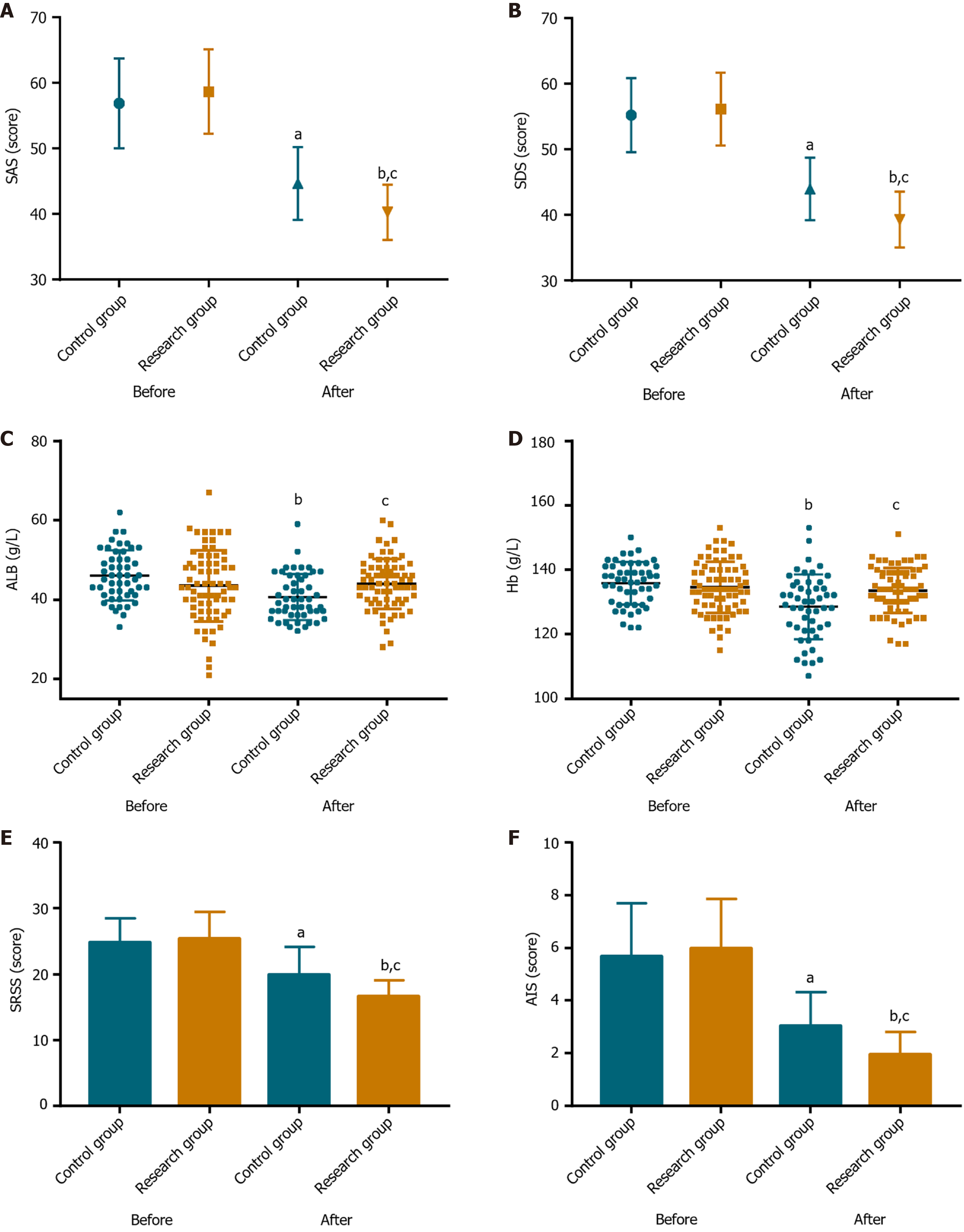
The baseline assessments revealed no notable intergroup differences in the psychological status (SAS/SDS; P > 0.05). Post-intervention, both groups demonstrated significant improvements; however, the research group achieved significantly lower post-intervention SAS and SDS scores than the control group (P < 0.05; Figure 2A and B).
The nutritional status of patients, assessed through serum ALB and Hb levels, revealed comparable baseline levels in both the groups (P > 0.05). Post-intervention, both parameters significantly decreased in the control group (P < 0.05), whereas, they remained stable (P > 0.05) in the research group and were significantly higher than those observed in the control group (P < 0.05; Figure 2C and D).
The sleep quality, evaluated using SRSS and AIS, demonstrated no evident intergroup differences at baseline (P > 0.05). However, these scores decreased significantly in both the groups (P < 0.05) post-intervention, with the research group achieving significantly lower scores (P < 0.05; Figure 2E and F).
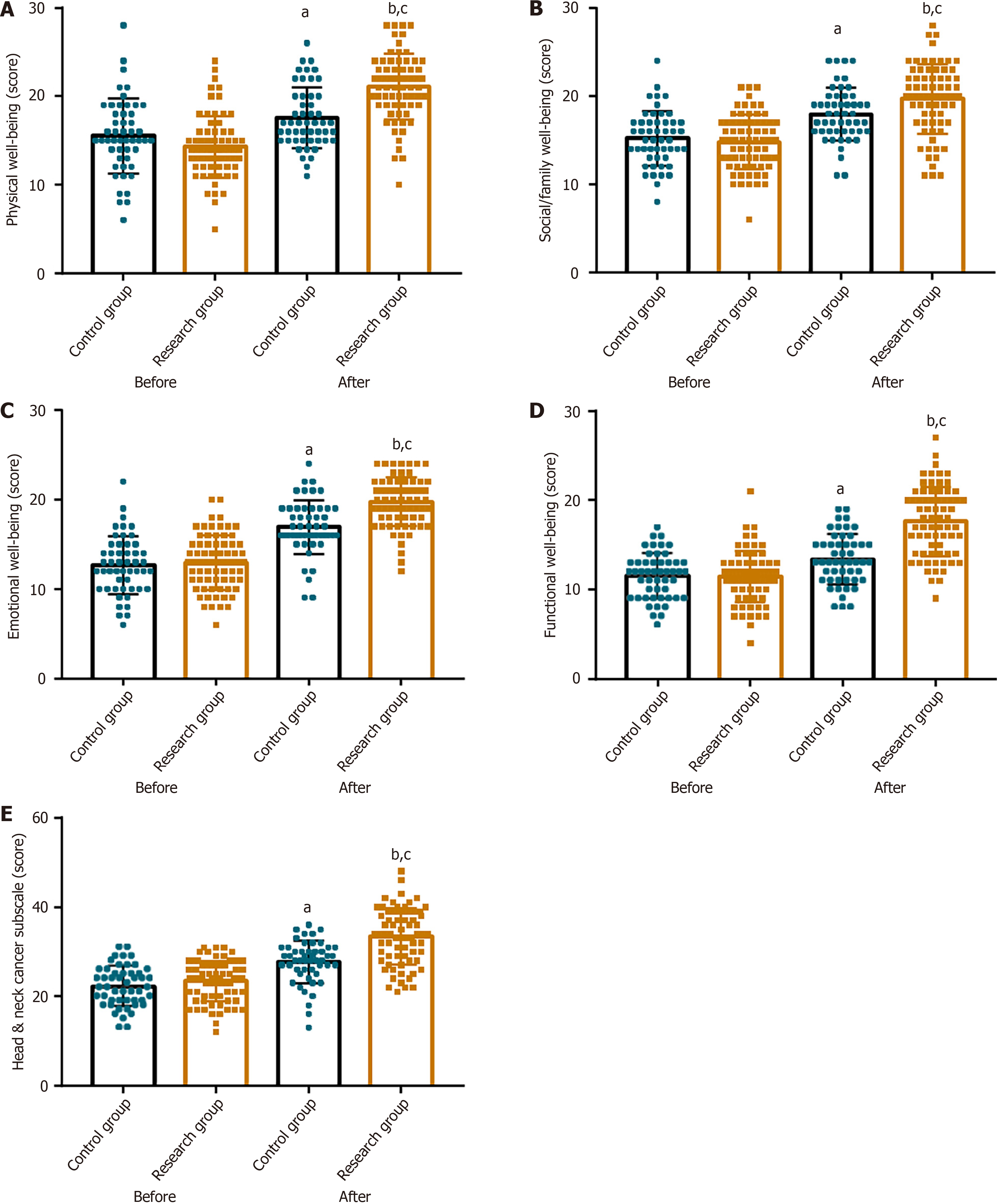
The five-dimensional Functional Assessment of Cancer Therapy-Head and Neck scale employed to assess the QoL showed no statistically different baseline measurements (P > 0.05). Post-intervention, both the groups demonstrated significant improvements across all measured domains (P < 0.05), with significantly higher performance recorded in the research group (P < 0.05; Figure 3).
This study presents novel findings demonstrating the positive influence of CBT-based psychological interventions in the postoperative recovery of patients with LC. These interventions significantly reduced the duration of tracheostomy and nasogastric tube dependence, along with the overall length of hospital stay. CBT effectively educates patients on accurate disease-related awareness, corrects misconceptions, and improves treatment adherence, thereby reducing the need for prolonged tracheostomy and nasogastric intubation. Additionally, the supplemental psychotherapy alleviates negative mood, thereby promoting recovery trajectories and shortening hospital stays[18,19].
Subsequently, patients with LC who underwent CBT-based psychological interventions exhibited reduced anxiety, depression, and psychological distress, indicating significant mental health benefits. These improvements likely result from the targeted psychological support provided by the CBT protocol, which incorporates guided relaxation, therapeutic imagery, and full-body massage to alleviate stress and psychological distress[20]. Furthermore, previous research reported the efficacy of psychological interventions in considerably reducing anxiety and depression in patients with LC and contributing to their earlier discharge from hospitals and lower treatment expenses[21], thereby corroborating and complementing our results. Additionally, Han et al[22] conducted research in orthopedic setting and demonstrated comparable effectiveness of CBT in perioperative mental health, achieving similar reductions in anxiety and sleep disturbances, which aligns with the outcomes observed in our study.
The CBT-based protocols effectively preserved the nutritional status of patients with LC pre-intervention and post-intervention. The significant reduction in negative emotions following CBT interventions partially explains this impro
Additionally, CBT-based psychological interventions effectively improved sleep quality and overall QoL of the patients, by alleviating distress and supporting the recovery process. A study by Yin[25] reported considerably reduced negative emotions in patients with LC and substantially improved sleep quality and QoL following mindfulness-based stress reduction training. Furthermore, Yang et al[26] reported that patients who underwent computer-assisted CBT protocol post-laryngectomy experienced significantly reduced anxiety, depression, insomnia, and pain severity levels along with enhanced QoL and satisfaction. Li et al[27] highlight the ability of psychological interventions in effectively mitigating negative emotions (reduced Hamilton Depression/Anxiety Scale scores) and improving QoL (increased European Organization for Research and Treatment of Cancer QoL Questionnaire scores) in patients with LC. Their outcomes corroborate our findings, despite the use of different assessment tools.
Previous scholarly work has expanded the clinical applications and significance of CBT. Nyman-Carlsson et al[28] noted that when combined with family or individual therapy, CBT facilitated weight recovery and alleviated eating disorder in young patients with anorexia nervosa. Wells-Di Gregorio et al[29] revealed that CBT, when integrated with acceptance and commitment therapy for patients with advanced cancer, improved sleep quality and reduced fatigue. Sherpa et al[30] reported that CBT treatment combined with oral creatine monohydrate for patients with depression effectively reduced depression symptoms while maintaining adequate safety.
However, several limitations in this study warrant further investigation and refinement. First, the sample source restricted to a single geographic area, potentially limits representativeness. Therefore, future studies are recommended to incorporate multi-regional samples to enhance generalizability and diversity. Second, the study did not assess long-term outcomes of the patients. Thus, 5-year follow-up research would be valuable to validate any extended prognostic benefits associated with CBT-based interventions. Third, the clinical contribution of each component of CBT, as well as their potential synergistic effects remains unclear. Thus, future studies should employ dismantling designs to identify the core components and to quantify how various components interact to produce combined effects.
CBT-based psychological interventions significantly improved post-surgical recovery in patients with LC by alleviating their anxiety and depression status, maintaining optimal nutritional levels during treatment, and improving sleep quality and QoL, thereby demonstrating substantial clinical value. Therefore, CBT-based psychological interventions significantly benefit patients with LC by promoting faster postoperative recovery, attenuating mental distress, main
| 1. | Huang J, Chan SC, Ko S, Lok V, Zhang L, Lin X, Lucero-Prisno DE 3rd, Xu W, Zheng ZJ, Elcarte E, Withers M, Wong MC. Updated disease distributions, risk factors, and trends of laryngeal cancer: a global analysis of cancer registries. Int J Surg. 2024;110:810-819. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 52] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 2. | Falco M, Tammaro C, Takeuchi T, Cossu AM, Scafuro G, Zappavigna S, Itro A, Addeo R, Scrima M, Lombardi A, Ricciardiello F, Irace C, Caraglia M, Misso G. Overview on Molecular Biomarkers for Laryngeal Cancer: Looking for New Answers to an Old Problem. Cancers (Basel). 2022;14:1716. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 39] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 3. | Divakar P, Davies L. Trends in Incidence and Mortality of Larynx Cancer in the US. JAMA Otolaryngol Head Neck Surg. 2023;149:34-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 43] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 4. | Bonafede M, d'Errico A, Rugarli S, Mensi C, Miligi L, Calisti R, Della Gatta R, Piro S, Melis P, Vasselli D, Binazzi A. The psychological impact of diagnosis of sinonasal, nasopharyngeal, and laryngeal cancers: a systematic review. Front Psychol. 2024;15:1355186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 5. | Dadhich S, Shakrawal N, Soni K, Pareek P, Patro SK. Impact of Radiotherapy on Quality of Life in T2 and Early T3 Laryngeal Carcinoma. Indian J Otolaryngol Head Neck Surg. 2023;75:654-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | van Beek FE, Jansen F, Baatenburg de Jong RJ, Langendijk JA, Leemans CR, Smit JH, Takes RP, Terhaard CHJ, Custers JAE, Prins JB, Lissenberg-Witte BI, Verdonck-de Leeuw IM. Psychological Problems among Head and Neck Cancer Patients in Relation to Utilization of Healthcare and Informal Care and Costs in the First Two Years after Diagnosis. Curr Oncol. 2022;29:3200-3214. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 7. | Heyda A, Księżniak-Baran D, Wygoda A, Składowski K. Low Post-Treatment Quality of Life and the High Incidence of Pain Are Common and Significantly Exacerbated in Depressed Head and Neck Patients Treated with Definitive Accelerated Radiotherapy. Cancers (Basel). 2023;16:79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 8. | Wulff NB, Dalton SO, Wessel I, Arenaz Búa B, Löfhede H, Hammerlid E, Kjaer TK, Godballe C, Kjaergaard T, Homøe P. Health-Related Quality of Life, Dysphagia, Voice Problems, Depression, and Anxiety After Total Laryngectomy. Laryngoscope. 2022;132:980-988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 9. | Nye A, Delgadillo J, Barkham M. Efficacy of personalized psychological interventions: A systematic review and meta-analysis. J Consult Clin Psychol. 2023;91:389-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 58] [Reference Citation Analysis (0)] |
| 10. | Ong CW, Hayes SC, Hofmann SG. A process-based approach to cognitive behavioral therapy: A theory-based case illustration. Front Psychol. 2022;13:1002849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 11. | Bhattacharya S, Goicoechea C, Heshmati S, Carpenter JK, Hofmann SG. Efficacy of Cognitive Behavioral Therapy for Anxiety-Related Disorders: A Meta-Analysis of Recent Literature. Curr Psychiatry Rep. 2023;25:19-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 12. | Komariah M, Amirah S, Faisal EG, Prayogo SA, Maulana S, Platini H, Suryani S, Yosep I, Arifin H. Efficacy of Internet-Based Cognitive Behavioral Therapy for Depression and Anxiety among Global Population during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis of a Randomized Controlled Trial Study. Healthcare (Basel). 2022;10:1224. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 13. | Vlachou E, Ntikoudi A, Owens DA, Nikolakopoulou M, Chalimourdas T, Cauli O. Effectiveness of cognitive behavioral therapy-based interventions on psychological symptoms in adults with type 2 diabetes mellitus: An update review of randomized controlled trials. J Diabetes Complications. 2022;36:108185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 14. | Itamura K, Hsue VB, Barbu AM, Chen MM. Diagnostic Assessment (Imaging) and Staging of Laryngeal Cancer. Otolaryngol Clin North Am. 2023;56:215-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 15. | Cheng L, Gao W, Xu Y, Yu Z, Wang W, Zhou J, Zang Y. Anxiety and depression in rheumatoid arthritis patients: prevalence, risk factors and consistency between the Hospital Anxiety and Depression Scale and Zung's Self-rating Anxiety Scale/Depression Scale. Rheumatol Adv Pract. 2023;7:rkad100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 20] [Reference Citation Analysis (0)] |
| 16. | Duan H, Gong M, Zhang Q, Huang X, Wan B. Research on sleep status, body mass index, anxiety and depression of college students during the post-pandemic era in Wuhan, China. J Affect Disord. 2022;301:189-192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 46] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 17. | Pfeifer MP, Keeney C, Bumpous J, Schapmire TJ, Studts JL, Myers J, Head B. Impact of a telehealth intervention on quality of life and symptom distress in patients with head and neck cancer. J Community Support Oncol. 2015;13:14-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Qin PP, Jin JY, Min S, Wang WJ, Shen YW. Association Between Health Literacy and Enhanced Recovery After Surgery Protocol Adherence and Postoperative Outcomes Among Patients Undergoing Colorectal Cancer Surgery: A Prospective Cohort Study. Anesth Analg. 2022;134:330-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 19. | Aglio LS, Mezzalira E, Mendez-Pino L, Corey SM, Fields KG, Abbakar R, Baez LA, Kelly-Aglio NJ, Vetter T, Jamison RN, Edwards RR. Surgical Prehabilitation: Strategies and Psychological Intervention to Reduce Postoperative Pain and Opioid Use. Anesth Analg. 2022;134:1106-1111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Sansoni M, Scarzello G, Serino S, Groff E, Riva G. Mitigating negative emotions through virtual reality and embodiment. Front Hum Neurosci. 2022;16:916227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Zhang S, Chen H, Zhang M, Sun X, Liu X. Reduction of depression symptoms in laryngeal cancer patients receiving psychology services. Am J Transl Res. 2020;12:6637-6645. [PubMed] |
| 22. | Han H, Chen C, Sheng R, Wang S. Psychological intervention based on cognitive behavioral therapy for patients with orthopedic surgical anxiety. Medicine (Baltimore). 2024;103:e39401. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 23. | Yan L, Zhang X, Li Y, Liu C, Yang H, Yang C. The role of psychological factors in functional gastrointestinal disorders: a systematic review and meta-analysis. Int J Colorectal Dis. 2023;38:65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (1)] |
| 24. | Irandoust K, Taheri M, Hamzehloo K, Hamzeloo A, Weiss K, Ghram A, Souissi A, Dergaa I, Knechtle B. The effects of cognitive behavioral therapy on selected physical, physiological parameters, exercise and nutritional behaviors in diabetic persons. Eur Rev Med Pharmacol Sci. 2022;26:6805-6812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 25. | Yin L. Effects of mindfulness-based stress reduction training on the negative emotions and social functioning of patients with laryngeal cancer. Clin Transl Oncol. 2025;27:1760-1766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 26. | Yang Y, Zhang H, Li Y, Liu Z, Liu S, Li X, Fan G, Xu Y, Wang BQ. The effectiveness of computer-assisted Cognitive Behavioral Therapy (cCBT) for psychological outcomes in patients with laryngectomy: Randomized controlled trial. J Affect Disord. 2022;300:59-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 27. | Li X, Li J, Shi Y, Wang T, Zhang A, Shao N, Wang Z. Psychological intervention improves life quality of patients with laryngeal cancer. Patient Prefer Adherence. 2017;11:1723-1727. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 28. | Nyman-Carlsson E, Norring C, Engström I, Gustafsson SA, Lindberg K, Paulson-Karlsson G, Nevonen L. Individual cognitive behavioral therapy and combined family/individual therapy for young adults with Anorexia nervosa: A randomized controlled trial. Psychother Res. 2020;30:1011-1025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 29. | Wells-Di Gregorio S, Flowers S, Peng J, Marks DR, Probst D, Zaleta A, Benson D, Cohn DE, Lustberg M, Carson W, Magalang U, Baltimore S, Ancoli-Israel S. Combined Treatment With Cognitive Behavioral Therapy for Insomnia and Acceptance and Commitment Therapy Enhances Objective and Subjective Reports of Sleep in Patients With Advanced Cancer. Psychooncology. 2025;34:e70141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 30. | Sherpa NN, De Giorgi R, Ostinelli EG, Choudhury A, Dolma T, Dorjee S. Efficacy and safety profile of oral creatine monohydrate in add-on to cognitive-behavioural therapy in depression: An 8-week pilot, double-blind, randomised, placebo-controlled feasibility and exploratory trial in an under-resourced area. Eur Neuropsychopharmacol. 2025;90:28-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/