Published online Jul 19, 2025. doi: 10.5498/wjp.v15.i7.106023
Revised: April 19, 2025
Accepted: June 10, 2025
Published online: July 19, 2025
Processing time: 124 Days and 20.6 Hours
An investigation is undertaken to assess the effects of permissive hypercapnia (PH) combined with goal-directed fluid therapy (GDFT) on postoperative reco
To ascertain whether the combination of PH and GDFT improves clinical recovery indicators, reduces postoperative complications, and alleviates anxiety, depre
A total of 120 elderly patients who underwent laparoscopic surgery in our hos
When compared with the control group, the study group demonstrated significantly shorter time to first flatus [(48.3 ± 6.2) hours vs (62.5 ± 7.8) hours], time to ambulation [(28.4 ± 4.2) hours vs (38.6 ± 5.1) hours], and length of hospital stay [(5.2 ± 1.1) days vs (7.4 ± 1.3) days] (P < 0.05). A significantly lower postoperative complication rate was observed in the study group (8.3% vs 21.7%, P < 0.05). Additionally, at 3 days postoperatively, significantly lower anxiety scores [(5.2 ± 1.4) vs (7.8 ± 1.6)] and depression scores [(4.8 ± 1.2) vs (7.1 ± 1.5)] were recorded in the study group compared to the control group (P < 0.05); Furthermore, at 24 hours postoperatively, serum levels of interleukin-6, tumor necrosis factor α, and C-reactive protein were found to be significantly lower in the study group than in the control group (P < 0.05).
Postoperative recovery is significantly expedited, postoperative complications are markedly reduced, anxiety-depression status is substantially improved, and inflammatory response is notably diminished in elderly patients undergoing laparoscopic surgery when PH is combined with GDFT, thereby making it worthy of clinical application.
Core Tip: This study highlights the benefits of permissive hypercapnia (PH) combined with goal-directed fluid therapy (GDFT) in elderly patients undergoing laparoscopic surgery. The PH + GDFT strategy is demonstrated to significantly accelerate postoperative recovery, reduce complications, and alleviate anxiety and depression. Additionally, it is observed to reduce levels of inflammatory markers, enhance sleep quality, and improve overall patient satisfaction. Multivariate analysis confirms PH + GDFT as an independent protective factor against postoperative psychological distress. These findings advocate for the integration of PH and GDFT into perioperative management to optimize both physical and psychological outcomes, particularly for elderly patients. This study offers clinical evidence supporting the refinement of anesthesia and fluid management strategies in minimally invasive surgery.
- Citation: Yuan L, Zhang XM, Liu N, Shi JQ, Sun XJ, Li GL, Teng JL. Permissive hypercapnia combined with goal-directed fluid therapy improve postoperative mental health in elderly patients undergoing laparoscopic surgery. World J Psychiatry 2025; 15(7): 106023
- URL: https://www.wjgnet.com/2220-3206/full/v15/i7/106023.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i7.106023
As the aging population accelerates, the percentage of elderly patients who receive laparoscopic surgery is also increasing. The elderly patients often present with multiple comorbidities, decreased organ function reserve, and greater risk of postoperative complications compared with younger patients. They are more prone to negative emotions like anxiety and depression[1-3]. Research has demonstrated that anxiety, depression, and other psychosocial factors after surgery negatively impact patients' quality of life and potentially delay wound healing, the incidence of complications, and the length of hospital stays. The highest rate of postoperative anxiety is reported among geriatric laparoscopic surgery patients, with rates ranging from 30%-45%, and depression ranges 25%-35%[4-7]. This postoperative psychological stress state is related with several surgical-associated factors, including both surgical trauma and inflammatory response as well as pain, which may influence postoperative recovery via the neuro-endocrine-immune network[7-10].
Recent years have brought new insights to optimizing perioperative management strategies to improve patient outcomes. As a lung-protective ventilation strategy, permissive hypercapnia (PH) can reduce mechanical ventilation-associated lung injury, improving tissue perfusion and exhibiting anti-inflammatory and organ-protective effects by moderately raising arterial carbon dioxide (CO2) pressure[11-14]. Individualized fluid management based on hemodynamic parameters termed as goal-directed fluid therapy (GDFT) can ensure optimization of tissue perfusion and avoidance of fluid overload or insufficiency. Studies on the perioperative mental state of elderly patients with PH combined with GDFT have not been conducted completely.
Studies have demonstrated that appropriate intraoperative ventilation strategies and intraoperative fluid management can indirectly influence the psychological condition of patients by reducing the level of inflammatory factors, maintaining proper tissue perfusion and decreasing the incidence of postoperative complications[15-17]. The inflammatory response is highly associated with the onset of anxiety and depression, and the inflammatory factors [interleukin (IL)-6 and tumor necrosis factor α (TNF-α)] can participate in emotional regulation by influencing neurotransmitters metabolism and the activation of hypothalamic-pituitary-adrenal axis. In addition, good tissue perfusion and oxygen supply can decrease postoperative pain and facilitate recovery of gastrointestinal function, which may further help improve patients’ psychological state.
Psychological effects are especially relevant, and of complex significance, among older surgery patients. Postoperative anxiety and depression may be accompanied by sleep disorders, loss of appetite, social withdrawal, and cognitive impairment. Psychological symptoms can be more pronounced in the elderly as they have lower stress tolerability and adaptation ability. Postoperative mental health problems have been linked to impaired recovery of function, increased falls risk, and poorer adherence to rehabilitation programs. In addition, anxiety and depression has been linked to increased rates of readmission and worse long-term outcomes. The interaction effects between physical recovery and psychological well-being can lead to a vicious cycle where poor mental health may affect recovery while delayed physical recovery may lead to more psychological distress.
In view of this, this study will explore the effects of PH combined with GDFT on postoperative early recovery and anxiety-depression status of elderly patients undergoing laparoscopic surgery to provide new clinical evidence for optimizing the perioperative management strategy and improving the prognosis of patients. We aim to comprehensively clarify the clinical applicability of this strategic intervention to promote recovery by observing postoperative recovery indicators, complication rates, anxiety-depression scores and inflammatory factor level trends in patients undergoing surgery, in order to validate the formulation of this strategic model as a new therapeutic strategy for promoting integrated recovery in geriatric surgical patients.
This study was approved by the Hospital Ethics Committee, approval No. K2024141 and employed a retrospective case-control study design. Clinical data were collected from 120 elderly patients who underwent laparoscopic colorectal cancer surgery in our hospital’s General Surgery Department from July 2023 to June 2024. Inclusion criteria were: (1) Age ≥ 65 years; (2) Pathologically confirmed colorectal cancer; (3) American Society of Anesthesiologists (ASA) physical status II-III; (4) Underwent laparoscopic surgery; (5) Complete clinical data, including pre- and post-operative anxiety and depression assessments, inflammatory factor test results, etc.; and (6) Normal preoperative mental status (Hospital Anxiety and Depression (HAD) score < 7). Exclusion criteria were: (1) Severe cardiac, pulmonary, hepatic, or renal dysfunction; (2) Preexisting severe psychiatric disorders or cognitive impairment; (3) History of psychiatric medication use; (4) Conversion to open surgery; (5) Chemotherapy or radiotherapy within one month before surgery; and (6) Incomplete clinical data. Patients were divided into control group (n = 60) and study group (n = 60) based on different anesthesia and fluid management protocols. The control group received conventional ventilation parameters (tidal volume 8-10 mL/kg, respiratory rate 12-14 breaths/minute, maintaining PaCO2 35-45 mmHg) and routine fluid management. The study group received PH (tidal volume 6-8 mL/kg, respiratory rate 10-12 breaths/minute, maintaining PaCO2 45-55 mmHg) combined with GDFT (maintaining stroke volume variation at 12%-13%). There were no statistically significant differences between the two groups in baseline characteristics including age, gender, body mass index, ASA classification, and tumor stage (P > 0.05).
Laparoscopic resection of colorectal cancer is a technique of minimally invasive surgery, which involves minimum trauma and also provides rapid recovery. But a precise surgical process is a multi-stage plan to achieve successful surgery from preoperative to postoperative. Preoperative Preparation. The patient is given a detailed assessment of their medical history, physical exams, imaging (computed tomography and magnetic resonance imaging), and laboratory evaluations to help define the indications for surgery as well as any possible contraindications. Furthermore, the patient must be prepared through vigorous bowel preparation to minimize the risk of an intraoperative contaminant and infections. At the same time, the surgical team prepares surgical instruments and equipment for laparoscopic surgery, including a high-definition imaging system, a pneumoperitoneum machine, an irrigation and suction device, and surgical instruments. It begins with pneumoperitoneum by inserting a pneumoperitoneum needle into the umbilicus (or a different access site) making a small incision, and injected CO2 gas into the abdomen. Subsequently, a laparoscope is inserted, and the intra-abdominal situation is observed through a monitor. Initially, a thorough exploration of the abdomen is conducted to assess the location, size, depth of invasion, and presence of distant metastases of the tumor. Next, based on the location and stage of the tumor, an appropriate range of lymph node dissection is selected[18-20]. For colon cancer, the principle of Complete Mesocolic Excision is usually followed; for rectal cancer, the principle of Total Mesorectal Excision is adhered to. Then, the affected bowel segment, including the tumor and surrounding mesentery, is mobilized. Surgical approaches include medial, lateral, and cranial medial approaches, with the specific choice depending on the tumor location and the surgeon's preference. The bowel segment is resected under laparoscopic guidance, ensuring tumor-free margins. Finally, depending on the surgical approach, an appropriate method of gastrointestinal reconstruction is chosen. Two common methods are small incision-assisted reconstruction and complete laparoscopic reconstruction. Anastomosis methods include end-to-end, side-to-side, and end-to-side anastomosis. After the surgery, the resected specimen is removed through a small incision or a natural orifice (such as the anus or vagina). The incision is carefully managed to prevent tumor cell implantation. Postoperatively, the patient's vital signs are closely monitored to prevent and manage potential complications.
The study assessed both primary and secondary outcomes. The primary outcomes encompassed three main aspects: Psychological status, inflammatory response, and sleep quality. Psychological assessment included HAD scale evaluations conducted preoperatively and at 3 days and 7 days after surgery, with anxiety and depression subscales scored separately (scores ≥ 7 indicating presence of symptoms), along with postoperative delirium monitoring using the Confusion Assessment Method CAM. For inflammatory and stress response evaluation, serum samples were collected at three time points - preoperatively, 24 hours, and 72 hours postoperatively - to measure levels of IL-6, TNF-α, CRP, cortisol, and norepinephrine. Sleep quality was evaluated using the Pittsburgh Sleep Quality Index (PSQI), and postoperative analgesic usage was recorded. Secondary outcome measures included enhanced recovery indicators (specifically time to first flatus, time to ambulation, and length of hospital stay), postoperative complication rate, hemodynamic changes during surgery and within 24 hours postoperatively, and patient satisfaction scores.
Data analysis was performed using SPSS 26.0 software. Normally distributed measurement data were expressed as mean ± SD, with independent sample t-tests for between-group comparisons. Count data were expressed as numbers (percentages) and analyzed using χ2 tests. Ranked data were analyzed using rank-sum tests. Repeated measures analysis of variance was used to compare indicators at different time points. Pearson correlation analysis was used to evaluate the correlation between inflammatory factor levels and anxiety/depression scores. P < 0.05 was considered statistically significant.
The baseline demographic and clinical characteristics were comparable between the two groups. The mean age was similar (study group: 71.3 ± 5.2 years vs control group: 70.8 ± 5.5 years, P = 0.65), as was the gender distribution (male/female: 34/26 vs 32/28, P = 0.78) and body mass index (23.5 ± 2.8 kg/m² vs 23.8 ± 2.6 kg/m², P = 0.54). ASA classification distribution and tumor staging showed no significant differences between groups (P = 0.89 and P = 0.92, respectively). The prevalence of comorbidities was also similar between groups (30 patients vs 28 patients, P = 0.73), including hypertension (25 patients vs 23 patients, P = 0.85) and diabetes mellitus (12 patients vs 10 patients, P = 0.79). Lifestyle factors such as smoking (20 patients vs 18 patients, P = 0.81) and alcohol consumption (15 patients vs 12 patients, P = 0.76) were also comparable. Additionally, there were no significant differences in previous surgery history (10 patients vs 8 patients, P = 0.71), family history of cancer (15 patients vs 13 patients, P = 0.82), or previous cancer treatment history including chemotherapy (5 patients vs 3 patients, P = 0.75) and radiotherapy (3 patients vs 2 patients, P = 0.83). All P values were greater than 0.05, indicating no statistically significant differences in baseline characteristics between the two groups (Table 1).
| Characteristic | Study group (n = 60) | Control group (n = 60) | P value |
| Age (year), mean ± SD | 71.3 ± 5.2 | 70.8 ± 5.5 | 0.65 |
| Gender (male/female) | 34/26 | 32/28 | 0.78 |
| BMI (kg/m2) | 23.5 ± 2.8 | 23.8 ± 2.6 | 0.54 |
| ASA classification distribution | I: 10, II: 30, III: 20 | I: 12, II: 32, III: 16 | 0.89 |
| Tumor staging | I: 10, II: 20, III: 20, IV: 10 | I: 12, II: 22, III: 18, IV: 8 | 0.92 |
| Comorbidities (n) | 30 | 28 | 0.73 |
| Smoking history (yes/no) | 20/40 | 18/42 | 0.81 |
| Alcohol consumption (yes/no) | 15/45 | 12/48 | 0.76 |
| Hypertension (yes/no) | 25/35 | 23/37 | 0.85 |
| Diabetes mellitus (yes/no) | 12/48 | 10/50 | 0.79 |
| Previous surgery (yes/no) | 10/50 | 8/52 | 0.71 |
| Family history of cancer (yes/no) | 15/45 | 13/47 | 0.82 |
| Chemotherapy history (yes/no) | 5/55 | 3/57 | 0.75 |
| Radiotherapy history (yes/no) | 3/57 | 2/58 | 0.83 |
The study group demonstrated significantly better postoperative recovery outcomes compared to the control group across all measured indicators. Recovery of gastrointestinal function was faster in the study group, with shorter time to first flatus (48.3 ± 6.2 vs 62.5 ± 7.8 hours, P = 0.002) and earlier resumption of diet (36.2 ± 5.0 vs 48.7 ± 6.3 hours, P = 0.001). Physical recovery was also enhanced, with reduced time to ambulation (28.4 ± 4.2 vs 38.6 ± 5.1 hours, P = 0.001) and shorter length of hospital stay (5.2 ± 1.1 vs 7.4 ± 1.3 days, P = 0.003). Patient comfort and safety indicators showed notable improvements in the study group, including lower postoperative pain scores (3.1 ± 1.2 vs 4.5 ± 1.5, P = 0.004), reduced incidence of postoperative nausea and vomiting (10 patients vs 20 patients, P = 0.012), and lower infection rates (5.0% ± 2.2% vs 10.0% ± 3.1%, P = 0.021). Overall postoperative complications were fewer in the study group (8 cases vs 15 cases, P = 0.034). These improvements were reflected in higher patient satisfaction scores in the study group (8.5 ± 1.0 vs 7.0 ± 1.2, P = 0.001). All differences were statistically significant with P values less than 0.05 (Table 2).
| Indicator | Study group (n = 60) | Control group (n = 60) | P value |
| Time to first flatus (hours) | 48.3 ± 6.2 | 62.5 ± 7.8 | 0.002 |
| Time to ambulation (hours) | 28.4 ± 4.2 | 38.6 ± 5.1 | 0.001 |
| Length of hospital stay (days) | 5.2 ± 1.1 | 7.4 ± 1.3 | 0.003 |
| Postoperative pain score (0-10) | 3.1 ± 1.2 | 4.5 ± 1.5 | 0.004 |
| Time to first diet (hours) | 36.2 ± 5.0 | 48.7 ± 6.3 | 0.001 |
| Postoperative nausea and vomiting (yes/no) | 10/50 | 20/40 | 0.012 |
| Postoperative infection rate (%) | 5.0 ± 2.2 | 10.0 ± 3.1 | 0.021 |
| Postoperative complications (n) | 8 | 15 | 0.034 |
| Patient satisfaction score (0-10) | 8.5 ± 1.0 | 7.0 ± 1.2 | 0.001 |
The study group exhibited significantly better psychological outcomes across all measured parameters. Anxiety and depression scores were markedly lower in the study group (anxiety: 5.2 ± 1.4 vs 7.8 ± 1.6, P = 0.001; depression: 4.8 ± 1.2 vs 7.1 ± 1.5, P = 0.001). The incidence of clinically significant psychological symptoms (HAD score ≥ 7) was also lower in the study group, with fewer patients experiencing anxiety (15.0% vs 35.0%, P = 0.008) and depression (13.3% vs 31.7%, P = 0.012). Pain-related psychological indicators showed more favorable outcomes in the study group, with lower Fear of Pain scores (3.5 ± 1.0 vs 5.0 ± 1.2, P = 0.002) and reduced Fear Avoidance Belief scores (2.8 ± 0.9 vs 4.2 ± 1.1, P = 0.003). Additionally, the study group demonstrated higher psychological resilience (7.5 ± 1.5 vs 5.8 ± 1.4, P = 0.001) and better postoperative quality of recovery as measured by the PostopQRS scale (85.2 ± 10.3 vs 72.4 ± 12.1, P = 0.001). All differences were statistically significant with P values less than 0.05, indicating that the PH + GDFT intervention was associated with improved psychological outcomes and better overall recovery quality (Table 3).
| Indicator | Study group (n = 60) | Control group (n = 60) | P value |
| Anxiety score (mean ± SD) | 5.2 ± 1.4 | 7.8 ± 1.6 | 0.001 |
| Depression score (mean ± SD) | 4.8 ± 1.2 | 7.1 ± 1.5 | 0.001 |
| Patients with clinically significant anxiety (HAD score ≥ 7) (%) | 15.0% (9/60) | 35.0% (21/60) | 0.008 |
| Patients with clinically significant depression (HAD score ≥ 7) (%) | 13.3% (8/60) | 31.7% (19/60) | 0.012 |
| FOP score (mean ± SD) | 3.5 ± 1.0 | 5.0 ± 1.2 | 0.002 |
| FAB score (mean ± SD) | 2.8 ± 0.9 | 4.2 ± 1.1 | 0.003 |
| Psychological resilience score (mean ± SD) | 7.5 ± 1.5 | 5.8 ± 1.4 | 0.001 |
| PostopQRS score (mean ± SD) | 85.2 ± 10.3 | 72.4 ± 12.1 | 0.001 |
The study group demonstrated significantly lower levels of pro-inflammatory markers compared to the control group. Specifically, key inflammatory cytokines were markedly reduced, including IL-6 (42.3 ± 8.5 vs 68.7 ± 12.4 pg/mL, P < 0.001), TNF-α (28.4 ± 5.6 vs 45.2 ± 8.9 pg/mL, P < 0.001), and CRP (38.5 ± 7.2 vs 62.4 ± 11.3 mg/L, P < 0.001). Other pro-inflammatory mediators also showed significant reductions in the study group, including IL-1β (12.5 ± 3.4 vs 18.7 ± 4.5 pg/mL, P = 0.002), monocyte chemoattractant protein-1 (20.3 ± 4.2 vs 28.6 ± 5.8 pg/mL, P = 0.003), interferon-gamma (9.8 ± 2.3 vs 14.5 ± 3.7 pg/mL, P = 0.004), and S100A8 (1.2 ± 0.3 vs 2.1 ± 0.5 ng/mL, P = 0.001).
Notably, the anti-inflammatory cytokine IL-10 showed significantly higher levels in the study group (15.2 ± 2.8 vs 10.5 ± 2.1 pg/mL, P = 0.001), suggesting an enhanced anti-inflammatory response. All differences were statistically significant with P values less than 0.05, indicating that the PH + GDFT intervention effectively modulated the inflammatory response by reducing pro-inflammatory markers while enhancing anti-inflammatory mediators (Table 4).
| Inflammatory marker | Study group (n = 60) | Control group (n = 60) | P value |
| IL-6 (pg/mL) | 42.3 ± 8.5 | 68.7 ± 12.4 | < 0.001 |
| TNF-α (pg/mL) | 28.4 ± 5.6 | 45.2 ± 8.9 | < 0.001 |
| CRP (mg/L) | 38.5 ± 7.2 | 62.4 ± 11.3 | < 0.001 |
| IL-1β (pg/mL) | 12.5 ± 3.4 | 18.7 ± 4.5 | 0.002 |
| IL-10 (pg/mL) | 15.2 ± 2.8 | 10.5 ± 2.1 | 0.001 |
| MCP-1 (pg/mL) | 20.3 ± 4.2 | 28.6 ± 5.8 | 0.003 |
| IFN-γ (pg/mL) | 9.8 ± 2.3 | 14.5 ± 3.7 | 0.004 |
| S100A8 (ng/mL) | 1.2 ± 0.3 | 2.1 ± 0.5 | 0.001 |
The study group demonstrated significantly better sleep quality parameters compared to the control group. The global PSQI score was notably lower in the study group (5.2 ± 1.3 vs 7.8 ± 1.8, P = 0.002), indicating better overall sleep quality. Sleep metrics showed significant improvements, including shorter sleep latency (20.4 ± 5.6 vs 30.2 ± 7.1 minutes, P = 0.003), longer total sleep time (6.8 ± 1.2 vs 5.4 ± 1.0 hours, P = 0.001), and higher sleep efficiency (85.2 ± 6.3% vs 72.4 ± 7.8%, P = 0.001). Pain management outcomes were also superior in the study group, with lower postoperative morphine equivalent consumption (15.3 ± 3.2 vs 23.6 ± 4.5 mg, P = 0.001). The study group experienced fewer sleep disturbances (12 cases vs 24 cases, P = 0.004), reduced need for sleep medication (5 patients vs 15 patients, P = 0.012), and fewer instances of daytime dysfunction (8 cases vs 18 cases, P = 0.015). The Epworth Sleepiness Scale score was also significantly lower in the study group (4.5 ± 1.2 vs 6.8 ± 1.5, P = 0.001), indicating better daytime alertness. All differences were statistically significant with P values less than 0.05, suggesting that the PH + GDFT intervention effectively improved both sleep quality and pain management outcomes (Table 5).
| Indicator | Study group (n = 60) | Control group (n = 60) | P value |
| Global PSQI score (mean ± SD) | 5.2 ± 1.3 | 7.8 ± 1.8 | 0.002 |
| Postoperative morphine equivalent consumption (mg) | 15.3 ± 3.2 | 23.6 ± 4.5 | 0.001 |
| Sleep latency (minutes) | 20.4 ± 5.6 | 30.2 ± 7.1 | 0.003 |
| Total sleep time (hours) | 6.8 ± 1.2 | 5.4 ± 1.0 | 0.001 |
| Sleep efficiency (%) | 85.2 ± 6.3 | 72.4 ± 7.8 | 0.001 |
| Sleep disturbances (n) | 12 | 24 | 0.004 |
| Use of sleep medication (yes/no) | 5/55 | 15/45 | 0.012 |
| Daytime dysfunction (n) | 8 | 18 | 0.015 |
| ESS score (mean ± SD) | 4.5 ± 1.2 | 6.8 ± 1.5 | 0.001 |
To comprehensively evaluate the impact of PH + GDFT on postoperative psychological outcomes, we conducted multiple regression analyses. Logistic regression analysis identified several independent risk factors for postoperative anxiety (HAD-A ≥ 7). The PH + GDFT intervention showed a protective effect [odds ratio (OR) = 0.38, 95% confidence interval (CI): 0.24-0.62, P = 0.001], while advanced age (≥ 75 years; OR = 1.85, 95%CI: 1.32-2.59, P = 0.003), elevated IL-6 levels at 24 hours (OR = 1.42, 95%CI: 1.18-1.71, P = 0.002), poor sleep quality (PSQI > 5; OR = 2.13, 95%CI: 1.56-2.91, P < 0.001), and postoperative complications (OR = 2.45, 95%CI: 1.73-3.46, P < 0.001) were associated with increased risk (Table 6).
| Risk factor | Variable | OR (95%CI) | P value |
| Postoperative anxiety (HAD-A ≥ 7) | PH + GDFT intervention | 0.38 (0.24-0.62) | 0.001 |
| Age ≥ 75 years | 1.85 (1.32-2.59) | 0.003 | |
| IL-6 levels at 24 hours (pg/mL) | 1.42 (1.18-1.71) | 0.002 | |
| PSQI > 5 | 2.13 (1.56-2.91) | < 0.001 | |
| Postoperative complications | 2.45 (1.73-3.46) | < 0.001 | |
| Postoperative pain score (NRS) | 1.25 (1.05-1.48) | 0.012 | |
| Duration of surgery (≥ 120 minutes) | 1.60 (1.10-2.33) | 0.015 | |
| Postoperative depression (HAD-D ≥ 7) | PH + GDFT intervention | 0.41 (0.26-0.65) | 0.001 |
| Age ≥ 75 years | 1.78 (1.25-2.53) | 0.002 | |
| IL-6 levels at 24 hours (pg/mL) | 1.35 (1.12-1.63) | 0.003 | |
| PSQI > 5 | 2.05 (1.48-2.84) | < 0.001 | |
| Postoperative complications | 2.30 (1.60-3.33) | < 0.001 | |
| Postoperative pain score (NRS) | 1.30 (1.08-1.56) | 0.007 | |
| Duration of surgery (≥ 120 minutes) | 1.55 (1.08-2.22) | 0.018 |
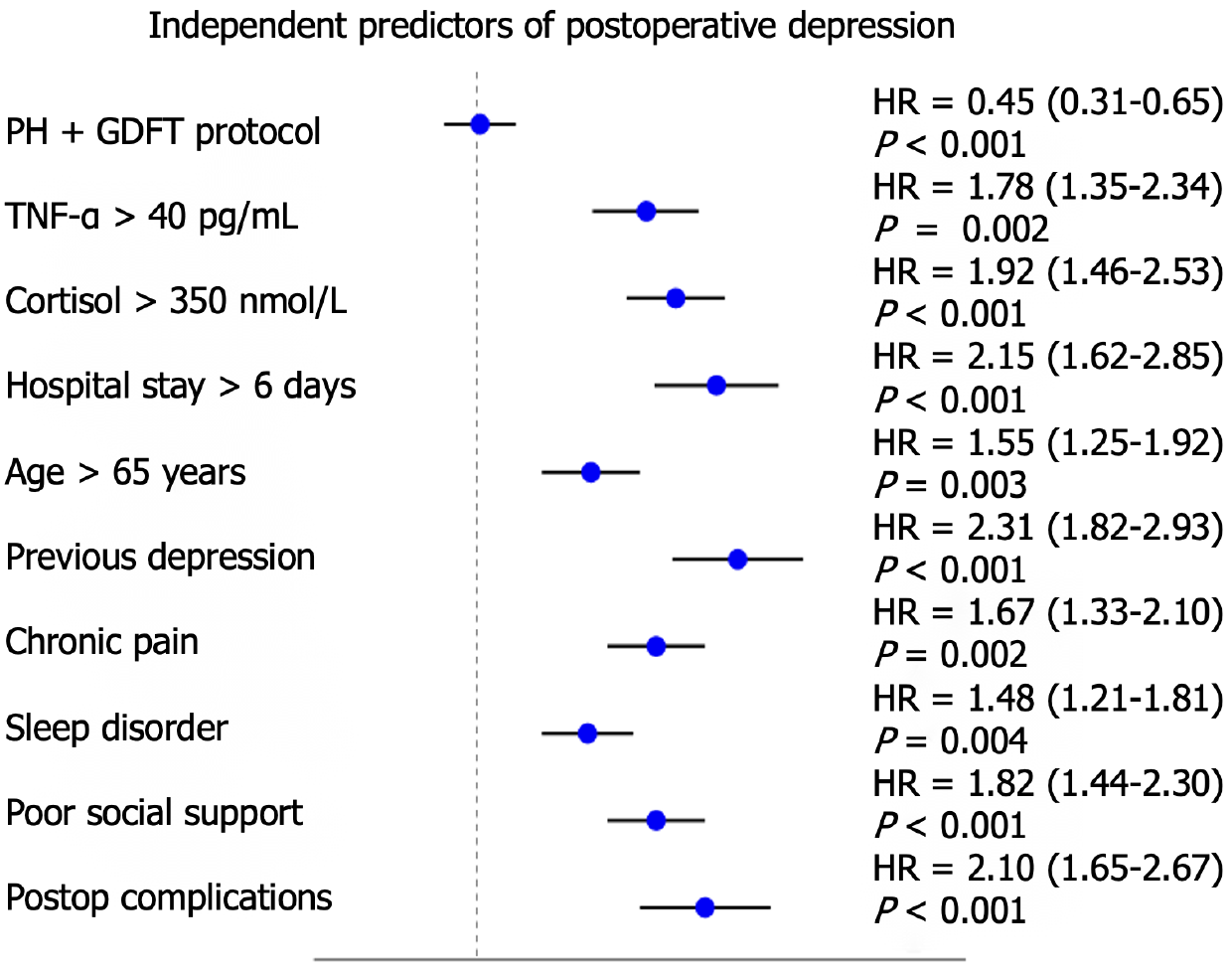
A study on independent predictors of postoperative depression shows that the PH + GDFT protocol is the only protective factor (HR = 0.45, P < 0.001), reducing the risk of postoperative depression by 55%. Of the risk factors identified for postoperative depression, the following had the most influence: Previous history of depression (HR = 2.31, P = 0.001), length of hospital stay greater than 6 days (HR = 2.15, P = 0.001), and postoperative complications (HR = 2.10, P = 0.001). Among the inflammatory, endocrine and psychological indicators, TNF-α > 40 pg/mL and cortisol > 350 nmol/L significantly influenced the occurrence of postoperative pulmonary dysfunction, which increased the risk of peripheral inflammatory factors and endocrine factors for postoperative pulmonary dysfunction by 78% and 92%, respectively. Older age (≥ 65 years) (HR = 1.55), chronic pain (HR = 1.67), and sleep disorders (HR = 1.48) were other factors associated with increased risk of postoperative depression. As an important social factor, poor social support (HR = 1.82) significantly increased the patients' risk of postoperative depression. Physiological, psychological, and social factors contribute to postoperative depression, highlighting that this debilitating condition is multifactorial in nature. These results constitute an impactful addition to the clinical practice framework, highlighting not only the preventive value of the PH + GDFT protocol itself but also the implicit necessity to pay attention to patients at risk in the form of clusters of risk factors and design tailored prevention strategies (Figure 1).
Aim This study aimed to determine the effects of PH in conjunction with GDFT on postoperative recovery and anxiety-depression status in elderly patients following laparoscopic surgery. This study is especially relevant as surgical indications expand into an older patient demographic with higher baseline risks for postoperative complications and psychological distress.
Over the past several years, perioperative management strategies have evolved to facilitate recovery and reduce complications. Abstract PH, GDFT two strategies have shown improvement in patient outcome. PH is a ventilator management strategy that augments arterial CO2 pressure in an effort to minimize ventilator-induced lung injury while sparing systemic perfusion. Conversely, GDFT adjusts fluid control according to haemodynamic indicators, allowing proper tissue perfusion while avoiding excessive fluid volume. Utilizing both strategies together may aid not only in physical recovery but also in alleviating some of the psychological trauma of surgery[21-24].
The gastric cancer patients 794 found that the rates of postoperative anxiety and depression among colorectal cancer patients is prevalent, which is primarily related to factors such as surgical trauma, chemotherapy drugs, doubts about prognosis, and a lack of social support[25-27]. In patients with colorectal cancer following surgical procedures who underwent chemotherapy, the rates of anxiety and depression were reported as 30%-45% and 25%-35%, respectively. These psychological morbidities affect patients’ quality of life and can also result in delayed wound healing, complications, and prolonged hospitalization.
Allowing CO2 retention in patients under mechanical ventilation, this management technique known as PH seeks to minimize the ventilator-induced lung injury by permitting a moderate increase in arterial CO2 pressure (PaCO2). Nevertheless, the effects of hypercapnia on the mental state are still not completely elucidated[28]. Other research indicates that hypercapnia can influence patients’ emotional state, via its impact on neurotransmitters and the autonomic nervous system.
During postoperative recovery, the combination of hypercapnia and GDFT has been proven to significantly improve patients' postoperative recovery. This combined treatment strategy not only reduces the incidence of postoperative complications but also shortens hospital stays and improves patients' quality of life. Furthermore, this treatment strategy may indirectly alleviate patients’ anxiety and depression through reducing inflammatory responses and improving tissue perfusion.
Although hypercapnia shows certain advantages in postoperative recovery, its direct effects on anxiety and depression require further research[28]. Some studies indicate that hypercapnia may positively affect patients' psychological state by improving tissue perfusion and reducing inflammatory responses. However, other studies suggest that hypercapnia might trigger anxiety by activating the autonomic nervous system.
Elderly patients are particularly vulnerable to postoperative anxiety and depression. The incidence of these psychological issues can be as high as 45% for anxiety and 35% for depression in this population. These conditions can significantly impair recovery by delaying wound healing, increasing the risk of complications, and prolonging hospital stays[7]. Moreover, the interplay between physical and psychological health can create a vicious cycle, where poor mental health exacerbates physical recovery and vice versa. Therefore, interventions that address both physical and psychological aspects of recovery are crucial.
The study highlights the significant role of inflammatory markers in postoperative psychological outcomes. Elevated levels of cytokines such as IL-6 and TNF-α have been shown to influence mood regulation by affecting neurotransmitter metabolism and activating the hypothalamic-pituitary-adrenal axis. The findings suggest that reducing inflammatory responses through optimized perioperative management can have a positive impact on psychological well-being. This aligns with previous research indicating that inflammation is a key mediator in the development of postoperative anxiety and depression.
Enhanced recovery after surgery protocols have gained traction in recent years, emphasizing the importance of multimodal interventions to improve patient outcomes. The combination of PH and GDFT in this study can be seen as an extension of enhanced recovery after surgery principles, focusing on optimizing physiological parameters to enhance recovery. The results demonstrate significant improvements in postoperative recovery indicators, such as shorter time to first flatus, ambulation, and hospital stay. These findings underscore the potential of integrating PH and GDFT into clinical practice to achieve better overall outcomes.
Failure to adequately control for potential confounding factors such as preoperative mental health status, social support, and individual coping strategies; although inflammatory markers were measured, the exact mechanisms by which PH + GDFT improves psychological outcomes are not fully elucidated; the single-center design and focus solely on elderly patients undergoing laparoscopic colorectal cancer surgery limit the generalizability of the results. Future research will expand the sample population and further explore the mechanisms of action to validate the effectiveness of PH + GDFT in broader clinical settings.
First, we will include more diverse patient populations, including patients of different age groups and surgical types, to validate the generalizability of our results. Second, we will incorporate patient-reported outcome measures to gain deeper insight into patients' subjective experiences of the treatment. Third, we plan to further explore the specific mechanisms by which PH + GDFT improves psychological health, particularly its regulatory effects on neuroinflammatory pathways. Finally, we will work to develop individualized risk assessment tools to identify high-risk patients who are most likely to benefit from PH + GDFT, thereby achieving precision medicine. These directions will help us establish more comprehensive and individualized perioperative management strategies, ultimately improving postoperative recovery quality and psychological health levels in elderly patients.
In conclusion, the study highlights the importance of optimizing perioperative management strategies to improve both physical and psychological recovery in elderly patients undergoing laparoscopic surgery. It is demonstrated that the combination of PH and GDFT can significantly enhance postoperative recovery and mitigate the risk of postoperative anxiety and depression. This research contributes to a growing body of evidence advocating for the incorporation of advanced perioperative protocols into clinical practice to improve patient outcomes.
| 1. | Cavalcante AN, Gurrieri C, Sprung J, Schroeder DR, Weingarten TN. Isoflurane and postoperative respiratory depression following laparoscopic surgery: A retrospective propensity-matched analysis. Bosn J Basic Med Sci. 2018;18:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Dai J, Lu Y, Zou Z, Wu Z. Optimizing esketamine administration for postoperative depression: a comprehensive study on laparoscopic bariatric surgery patients. Psychopharmacology (Berl). 2025;242:285-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 3. | Turgut DN, Tuncel E, Palta A, Tektas M, Balci M, Guzel O, Keten T, Aslan Y, Tuncel A. Job satisfaction, depression severity and quality of life ratings of perioperative nurses in robotic-assisted and laparoscopic surgery. J Robot Surg. 2024;18:19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Aldobekhi FSS. Efficacy of Virtual Reality as a Treatment Modality on Preoperative vs Postoperative Patient Anxiety: A Systematic Review. J Pharm Bioallied Sci. 2024;16:S3827-S3830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 5. | Huang Y, Gao RJ, Mao SM, Yao JL, He HY, Wang Y, Feng JY. Effect of estazolam plus remimazolam on attenuating preoperative anxiety and remifentanil-induced postoperative hyperalgesia in elective gynecological laparoscopic surgery: a randomized clinical trial. Minerva Anestesiol. 2025;91:164-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Kirtil İ, Aydin E. Relationship Between Preoperative Fasting Duration and Anxiety Levels With Postoperative Pain, Nausea-Vomiting, and Sleep Quality in Orthopedic Surgical Patients: A Cross-Sectional Study. Nurs Health Sci. 2025;27:e70048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Momtaz D, Jahn J, Eskenazi J, Peterson B, Lawand J, Ghali A, Hosseinzadeh P. The Impact of Anxiety and Depression on Postoperative Pain Management and Emergency Room Visits in Pediatric Patients With Surgically Treated Lower Extremity Fractures: A Propensity-matched Cohort Analysis. J Pediatr Orthop. 2025;45:251-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 8. | Ai AL, Huang B, Nash V, Stouffer GA. Optimism mitigated impacts of pre-operative depression and anxiety on post-operative distress in cardiac patients. Psychol Health Med. 2025;30:460-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Sharif-Nia H, Froelicher ES, Marôco J, Hoseinzadeh E, Hejazi S, Fatehi R, Nowrozi P, Mohammadi B. Psychometric properties of the pain anxiety symptom scale among postoperative patients in Amol, Iran. Front Psychiatry. 2024;15:1422346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 10. | Tong K, Song YT, Jing SQ, You Y, Wang SJ, Wu T, Xu H, Zhang JW, Liu L, Hao JR, Sun N, Cao JL, Gao C. Reactive astrocytes mediate postoperative surgery-induced anxiety through modulation of GABAergic signalling in the zona incerta of mice. Br J Anaesth. 2025;134:111-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 11. | Qin J, Cheng M, He C, Shen X, Zhu Z. An imidazo-pyridin derivative as fluorescent probe for the peroxynitrite detection in pulmonary permissive hypercapnia. Anal Sci. 2025;41:457-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Xi YZ, Wei XL, Xie L, Jia XY, Li ZP, Zhou QH. Impact of Permissive Hypercapnia on Postoperative Early Plasma Neurofilament Light Chain in Elderly Patients Undergoing Laparoscopic Surgery: A Prospective, Randomized Controlled Trial. Ther Clin Risk Manag. 2024;20:749-759. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 13. | Xiang B, Zhang W. Is permissive hypercapnia really pneumoprotective? Eur J Anaesthesiol. 2024;41:938-939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Zochios V, Yusuff H, Schmidt M. Personalizing Permissive Hypercapnia in Acute Severe Respiratory Failure. J Cardiothorac Vasc Anesth. 2025;39:355-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Abbruzzese L, Basagni B, Damora A, Salti G, Martinelli G, Gambarelli C, Maietti A, Scarselli C, Carlucci L, Zoccolotti P, Mancuso M. Psychological Distress in Patients Who Needed Invasive versus Non-Invasive Ventilation Following SARS-CoV-2 Viral Infection. Brain Sci. 2024;14:189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 16. | Annunziata A, Calabrese C, Simioli F, Coppola A, Pierucci P, Mariniello DF, Fiorentino G. Psychological Factors Influencing Adherence to NIV in Neuromuscular Patients Dependent on Non Invasive Mechanical Ventilation: Preliminary Results. J Clin Med. 2023;12:5866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 17. | Menza R, Howie-Esquivel J, Bongiovanni T, Tang J, Johnson JK, Leutwyler H. Personalized music for cognitive and psychological symptom management during mechanical ventilation in critical care: A qualitative analysis. PLoS One. 2024;19:e0312175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Aoki R, Maruyama S, Takii Y, Nogami H. Efficacy and safety of laparoscopic resection of colorectal cancer in non-elite cases. Surg Today. 2025;55:676-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 19. | Lin C, Xu Z, XinLiang, Wei H, Wang X. A randomized controlled trial to compare the effect of oxycodone and sufentanil on postoperative analgesia and immune function for laparoscopic resection of colorectal cancer. BMC Anesthesiol. 2025;25:58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 20. | Che L, Yu JW, Zhang YL, Xu L, Huang YG. Intraoperative Blood Pressure Lability Acts as a Key Mediator in the Impacts of Goal-Directed Fluid Therapy on Postoperative Complications in Patients Undergoing Major Spine Surgery. Chin Med Sci J. 2023;38:257-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Feng S, Xiao W, Zhang Y, Ma Y, Yang S, He T, Wang T. Effect of goal-directed fluid therapy based on both stroke volume variation and delta stroke volume on the incidence of composite postoperative complications among individuals undergoing meningioma resection. Chin Med J (Engl). 2023;136:1990-1992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 22. | Hoang TN, Musquiz BN, Tubog TD. Impact of Goal-Directed Fluid Therapy on Postoperative Outcomes in Colorectal Surgery: An Evidence-Based Review. J Perianesth Nurs. 2023;38:650-656.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 23. | Ma H, Li X, Wang Z, Qiao Q, Gao Y, Yuan H, Guan B, Guan Z. The effect of intraoperative goal-directed fluid therapy combined with enhanced recovery after surgery program on postoperative complications in elderly patients undergoing thoracoscopic pulmonary resection: a prospective randomized controlled study. Perioper Med (Lond). 2023;12:33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 24. | Hu Z, Zhang H, Wang J, Xiong H, Liu Y, Zhu Y, Chang Z, Hu H, Tang Q. Nomogram to Predict the Risk of Postoperative Anxiety and Depression in Colorectal Cancer Patients. Int J Gen Med. 2022;15:4881-4895. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 25. | Wada S, Inoguchi H, Hirayama T, Matsuoka YJ, Uchitomi Y, Ochiai H, Tsukamoto S, Shida D, Kanemitsu Y, Shimizu K. Yokukansan for the treatment of preoperative anxiety and postoperative delirium in colorectal cancer patients: a retrospective study. Jpn J Clin Oncol. 2017;47:844-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | Katznelson R, Djaiani G, Naughton F, Wasowicz M, Ragoonanan T, Duffin J, Fedorko L, Murphy J, Fisher JA. Post-operative hypercapnia-induced hyperpnoea accelerates recovery from sevoflurane anaesthesia: a prospective randomised controlled trial. Acta Anaesthesiol Scand. 2013;57:623-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 27. | Lin L, Zhang Q, Xu M, Xiao Z, Xu G, Mei Z. The impact of depression and anxiety disorders on postoperative outcomes for patients having total hip or knee arthroplasty: Protocol of a meta-analytic study from cohort studies. PLoS One. 2025;20:e0318067. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 28. | Sun M, Wang X, Lu Z, Yang Y, Lv S, Miao M, Chen WM, Wu SY, Zhang J. Chronic postsurgical pain increases postoperative depression risk. J Epidemiol Community Health. 2025;jech-2024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/