Published online Dec 19, 2025. doi: 10.5498/wjp.v15.i12.112655
Revised: September 23, 2025
Accepted: October 29, 2025
Published online: December 19, 2025
Processing time: 100 Days and 1.1 Hours
Patients who undergo radical cervical cancer surgery often experience sexual dysfunction and psychological distress, which seriously affects their quality of life. This study aimed to evaluate the clinical effectiveness of mindfulness-based stress reduction (MBSR) therapy for psychosexual adaptation in patients after radical cervical cancer surgery.
To systematically evaluate the clinical effectiveness of MBSR therapy on psychosexual adaptation in patients following radical cervical cancer surgery.
A multicenter retrospective study design was used to analyze the clinical data of 280 patients who underwent radical cervical cancer surgery between January 2021 and August 2024 at Lishui Central Hospital, The Fifth Hospital Affiliated to Wenzhou Medical University, Lishui Hospital of Zhejiang University and Wen
After intervention, patients in the MBSR intervention group showed significant improvement in anxiety and depression levels (anxiety: 5.8 ± 1.2 vs 8.3 ± 1.7, P < 0.001; depression: 6.2 ± 1.4 vs 9.1 ± 1.8, P < 0.001). The proportion of patients with clinically significant anxiety decreased from 69.3% to 21.4% (control group: 67.9%-52.9%, P < 0.001). The intervention group showed significantly better Female Sexual Function Index total scores (23.5 ± 3.6 vs 17.8 ± 3.2, P < 0.001) and scores in all dimensions than the control group, with a significantly lower incidence of sexual dysfunction (42.9% vs 67.9%, P < 0.001). Regarding sexual relationship satisfaction, both patients in the intervention group (78.3 ± 6.5 vs 65.2 ± 7.8, P < 0.001) and their partners (76.9 ± 7.1 vs 63.6 ± 8.3, P < 0.001) showed significantly improved scores. Age-stratified analysis showed that MBSR was most effective in younger patients (≤ 45 years, 46-55 years; P < 0.001), with relatively less benefit in older patients (> 55 years; P = 0.032). Multivariate regression analysis confirmed that MBSR intervention [odds ratios (OR) = 2.86, 95% confidence interval (95%CI): 1.75-4.68, P < 0.001] and partner support (OR = 1.92, 95%CI: 1.28-2.87, P = 0.002) were independent positive predictive factors for improving patients' psychosexual adaptation.
MBSR therapy can effectively improve anxiety and depression in patients after radical cervical cancer surgery and significantly enhance sexual function and sexual relationship satisfaction, with the effects being more pronounced in younger patients. This study demonstrated that MBSR, as an integrative intervention approach, has independent positive effects on psychosexual adaptation in post-operative cervical cancer patients and is worthy of promotion in clinical practice.
Core Tip: This multicenter retrospective study investigated the impact of mindfulness-based stress reduction (MBSR) on psychological sexual adaptation in patients after radical cervical cancer surgery. MBSR significantly improved anxiety, depression, sexual function, and sexual relationship satisfaction compared to standard care. Both patients and their partners reported enhanced intimacy and emotional connections. Younger patients benefited more than older patients. Multivariate analysis confirmed that MBSR and partner support are independent predictors of psychosexual recovery. The findings support MBSR as an effective integrative intervention for improving postoperative quality of life in cervical cancer survivors.
- Citation: Sun QQ, Ke FF, Zhou HY, Zhou SJ, Lu J, Gao M. Mindfulness-based stress reduction for sexual psychological recovery after radical cervical cancer surgery: A retrospective study. World J Psychiatry 2025; 15(12): 112655
- URL: https://www.wjgnet.com/2220-3206/full/v15/i12/112655.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i12.112655
Cervical cancer is the fourth most common malignant tumor among women worldwide, with approximately 570000 new cases and 310000 deaths annually, 80% of which occur in developing countries. In China, the incidence of cervical cancer has shown a trend toward a younger age, seriously threatening women's health. With advancements in early screening and treatment technologies, the five-year survival rate of patients with cervical cancer has significantly improved, exceeding 70%. However, while radical cervical cancer surgery (including total hysterectomy and pelvic lymph node dissection, etc.) effectively controls disease progression, it often leads to a series of physiological and psychological problems, especially sexual dysfunction and related psychological distress, which severely affects patients' postoperative quality of life and partner relationships[1-7].
After radical cervical cancer surgery, approximately 60%-80% of patients experience varying degrees of sexual dysfunction, mainly manifested as decreased libido, difficulty with sexual arousal, inadequate vaginal lubrication, painful intercourse, and orgasmic disorders. These physiological changes stem from pelvic nerve damage, vaginal morphological changes, and endocrine dysfunction caused by the surgery. Simultaneously, patients often experience negative emotional states, such as anxiety, depression, low self-esteem, body image disorders, and fear. Research shows that the incidence of anxiety in post-cervical cancer surgery patients is 32.6%-68.3%, and the incidence of depression is 25.8%-53.7%, which is significantly higher than that in healthy women of the same age. This dual predicament forms a "vicious cycle": Sexual dysfunction exacerbates psychological distress, while psychological problems further worsen sexual dysfunction, leading to a continuous decline in patients' sexual quality of life, decreased marital satisfaction, and even family crises[8-10].
Traditional interventions often focus on either physiological sexual function rehabilitation or simple psychological support such as pelvic floor muscle training, vaginal dilator use guidance, sexual education, and routine psychological counseling. However, these interventions often separate the intrinsic connection between sexual dysfunction and psychological problems, lacking an integrative perspective and with limited clinical effectiveness. Research shows that among post-cervical cancer surgery patients receiving routine sexual health guidance, 45%-60% still report persistent sexual dissatisfaction, and 30%-40% of patients' psychological distress derived from sexual problems remains unresolved. Therefore, exploring more effective integrative intervention programs has become a current research focus[11-13].
Mindfulness-based stress reduction (MBSR), founded by the American molecular biologist Jon Kabat-Zinn in 1979, is an eight-week structured intervention program that combines Eastern meditation and modern psychological concepts. This therapy guides patients to perceive their current physical and mental experiences in a non-judgmental, fully accepting manner, gradually changing their cognitive patterns toward stressors and enhancing psychological regulation capabilities. Recently, MBSR has demonstrated significant psychological intervention effects in patients with chronic pain, cancer, anxiety, depression, and other chronic diseases. Meta-analyses showed that MBSR can effectively reduce anxiety levels [SMD = -0.75, 95% confidence interval (95%CI): -0.95 to -0.54] and depressive symptoms (SMD = -0.73, 95%CI: -0.94 to -0.52) in cancer patients, improving their quality of life[14-16].
Notably, the core concepts of MBSR—cultivating sensitivity to bodily sensations, improving concentration, accepting current experiences, and reducing self-judgment—highly align with key elements of sexual and psychological health. Preliminary studies have indicated that mindfulness training helps improve female sexual function, especially in enh
Given the complexity of psychological sexual problems in patients after radical cervical cancer surgery and the limitations of traditional intervention measures, exploring the effects of MBSR on psychological sexual adaptation in this special population has important clinical significance. This study aimed to systematically evaluate the impact of MBSR on anxiety and depression, sexual function, and sexual relationship satisfaction in patients after radical cervical cancer surgery through a retrospective analysis of a larger sample of clinical data, providing evidence-based support for clinical practice and helping comprehensive rehabilitation and quality of life improvement for cervical cancer patients.
This study employed a multicenter retrospective cohort study design and collected clinical data from patients who underwent radical cervical cancer surgery between January 2021 and August 2024 at the gynecological oncology centers of two tertiary hospitals: Lishui Central Hospital, The Fifth Hospital Affiliated to Wenzhou Medical University, Lishui Hospital of Zhejiang University (hereafter referred to as Lishui Central) and Wenzhou Central Hospital. The study included patients aged 20-65 years, pathologically diagnosed with cervical cancer (clinical stage IA2-IIA, FIGO 2018 staging) and underwent radical surgery (type I or type II radical hysterectomy and pelvic lymph node dissection), with expected survival > 12 months, stable sexual partners with normal sexual life before surgery, and elementary school education or above. Exclusion criteria included patients with other malignant tumors or terminal chronic diseases, previous history of psychiatric disorders or current use of psychiatric medications, pre-existing clear sexual dysfunction [Female Sexual Function Index (FSFI) score < 23], serious complications within 3 months post-surgery, pre- or post-operative cognitive dysfunction, and patients lost to follow-up or with extremely poor compliance (participation in intervention < 30%).
Finally, 280 patients meeting the criteria were included, with Lishui Central collecting 140 cases (70 in the intervention group and 70 in the control group) and Wenzhou Central Hospital collecting 140 cases (70 in the intervention group and 70 in the control group). Based on different post-operative rehabilitation protocols, the patients were divided into a control group (n = 140) and an intervention group (n = 140). The control group received routine care and sexual health guidance, including general post-operative complication management, basic sexual health education, routine psychological support, and sexual life guidance, implemented by specially trained oncology nurses through one-on-one health consultations and distribution of educational materials, with monthly follow-ups for 6 consecutive months. The intervention group, in addition to routine care and sexual health guidance, participated in an 8-week MBSR intervention led by professionally trained and certified MBSR psychotherapists, following standard MBSR protocols including weekly 90-minute group mindfulness sessions (8-12 people per group), daily 45-minute home practice, and specially designed targeted psychological adaptation content (such as accepting body changes, sexual pleasure mindfulness training, partner communication practice, etc.). MBSR intervention began 3 months post-surgery and lasted 8 weeks, followed by monthly 60-minute reinforcement training for 4 consecutive months. The study protocol was approved by the Ethics Committee of Wenzhou Central Hospital (approval No. L2025-06-021), and all participants provided written informed consent.
All assessments were conducted before the intervention (3 months after surgery), after the intervention (6 months after surgery), and during follow-up (12 months after surgery) by researchers blinded to group allocation. This study est
The FSFI was used to assess sexual function (including desire, arousal, lubrication, orgasm, satisfaction, and pain, 19 items in total, total score 2-36 points, < 23 points defined as sexual dysfunction).
The Sexual Satisfaction Scale for Women (SSSW) was used to assess sexual relationship quality (25 items in total, total score 25-100 points, both the patients and their partners completed the assessment). The secondary assessment indicators included quality of life (using the EORTC QLQ-C30 scale), intervention compliance, and adverse event recording. The primary endpoint was set as FSFI total score ≥ 23 points after intervention (6 months after surgery), representing sexual function recovery; secondary endpoints included HADS anxiety and depression subscale scores < 8 points after int
SPSS software (version 25.0) was used for the data analysis. Measurement data were expressed as mean ± SD, and an independent sample t-test was used for between-group comparisons. Count data were expressed as number of cases (percentage), and χ² test or Fisher's exact probability method was used for between-group comparisons. Multifactor analysis used multivariate logistic regression models, calculating odds ratios (OR) and 95%CI; P < 0.05, considered statistically significant. Sample size estimation was based on changes in the FSFI total score, setting effect size d = 0.4, α = 0.05, β = 0.1, considering a 15% dropout rate, and finally determining that at least 142 patients were needed in each group.
The results showed good homogeneity between the intervention (n = 140) and control groups (n = 140). Regarding demographic characteristics, the intervention group's average age was 51.3 ± 6.8 years, control group 52.1 ± 7.2 years (P = 0.732), body mass index indices were 23.2 ± 3.1 kg/m2 and 23.6 ± 3.3 kg/m2 respectively (P = 0.634). Sociodemographic indicators showed a similar educational level distribution between groups (junior high school and below: 42.1% vs 40.0%; high school/technical secondary school: 39.3% vs 41.4%; college and above: Approximately 18%, P = 0.872), and marital status was predominantly married (88.6% vs 87.1%, P = 0.657). Clinical characteristics showed laparoscopic surgery rates slightly higher than open surgery (intervention group 56.4% vs 43.6%, control group 57.1% vs 42.9%, P = 0.885), FIGO staging predominantly IB1 (approximately 42%, P = 0.939), pathological types predominantly squamous cell carcinoma (approximately 79%), adenocarcinoma (approximately 16%), and adenosquamous carcinoma (approximately 5%; P = 0.951). Baseline assessment scores showed no significant differences in FSFI total score (28.7 ± 3.3 vs 28.4 ± 3.5, P = 0.823), Hospital Anxiety Scale (HADS-A; 9.6 ± 1.8 vs 9.4 ± 1.9, P = 0.425) and Hospital Depression Scale (HADS-D; 10.1 ± 2.1 vs 9.9 ± 2.0, P = 0.533). Treatment-related indicators showed that approximately 53% of patients did not receive adjuvant therapy, approximately 15% received radiotherapy alone, approximately 32% received chemoradiotherapy (P = 0.862), and there was a balanced distribution of pre- and post-menopausal patients (P = 0.724), similar surgical time, and intraoperative blood loss. Comorbidities (hypertension approximately 23%, diabetes approximately 13%, cardiovascular disease approximately 7%), tumor size (2.6 ± 1.1 cm vs 2.8 ± 1.2 cm, P = 0.376) and lymph node metastasis rate (10.7% vs 12.9%, P = 0.546) showed no statistical differences. All P values were > 0.05, providing a reliable research foundation for evaluating the effects of MBSR therapy on psychosexual adaptation in patients after radical cervical cancer surgery (Table 1).
| Characteristics | Intervention group (n = 140) | Control group (n = 140) | Statistics | P value |
| Demographic characteristics | ||||
| Age (years, mean ± SD) | 51.3 ± 6.8 | 52.1 ± 7.2 | t = -0.343 | 0.732 |
| BMI (kg/m2, mean ± SD) | 23.2 ± 3.1 | 23.6 ± 3.3 | t = -0.477 | 0.634 |
| Sociodemographic characteristics | ||||
| Education level | χ² = 0.274 | 0.872 | ||
| Junior high school and below | 59 (42.1) | 56 (40.0) | ||
| High school/technical secondary school | 55 (39.3) | 58 (41.4) | ||
| College and above | 26 (18.6) | 26 (18.6) | ||
| Marital status | χ² = 0.198 | 0.657 | ||
| Married | 124 (88.6) | 122 (87.1) | ||
| Others | 16 (11.4) | 18 (12.9) | ||
| Clinical characteristics | ||||
| Surgical approach | χ² = 0.021 | 0.885 | ||
| Laparoscopic surgery | 79 (56.4) | 80 (57.1) | ||
| Open surgery | 61 (43.6) | 60 (42.9) | ||
| FIGO stage | χ² = 0.406 | 0.939 | ||
| IA2 | 21 (15.0) | 20 (14.3) | ||
| IB1 | 59 (42.1) | 59 (42.1) | ||
| IB2 | 38 (27.1) | 39 (27.9) | ||
| IIA | 22 (15.8) | 22 (15.7) | ||
| Pathological type | χ² = 0.103 | 0.951 | ||
| Squamous cell carcinoma | 110 (78.6) | 111 (79.3) | ||
| Adenocarcinoma | 23 (16.4) | 22 (15.7) | ||
| Adenosquamous carcinoma | 7 (5.0) | 7 (5.0) | ||
| Baseline assessment scores | ||||
| FSFI total score (mean ± SD) | 28.7 ± 3.3 | 28.4 ± 3.5 | t = 0.223 | 0.823 |
| HADS-A (mean ± SD) | 9.6 ± 1.8 | 9.4 ± 1.9 | t = 0.800 | 0.425 |
| HADS-D (mean ± SD) | 10.1 ± 2.1 | 9.9 ± 2.0 | t = 0.625 | 0.533 |
| Treatment-related indicators | ||||
| Adjuvant therapy | χ² = 0.297 | 0.862 | ||
| No adjuvant therapy | 74 (52.9) | 75 (53.6) | ||
| Radiotherapy alone | 21 (15.0) | 21 (15.0) | ||
| Chemoradiotherapy | 45 (32.1) | 44 (31.4) | ||
| Menopausal status | χ² = 0.125 | 0.724 | ||
| Premenopausal | 61 (43.6) | 63 (45.0) | ||
| Postmenopausal | 79 (56.4) | 77 (55.0) | ||
| Other indicators | ||||
| Comorbidities | ||||
| Hypertension | 32 (22.9) | 32 (22.9) | χ² = 0.000 | 0.989 |
| Diabetes | 18 (12.9) | 18 (12.9) | χ² = 0.006 | 0.936 |
| Cardiovascular disease | 10 (7.1) | 10 (7.1) | χ² = 0.026 | 0.872 |
| Tumor size (cm, mean ± SD) | 2.6 ± 1.1 | 2.8 ± 1.2 | t = -0.887 | 0.376 |
| Lymph node metastasis | 15 (10.7) | 18 (12.9) | χ² = 0.365 | 0.546 |
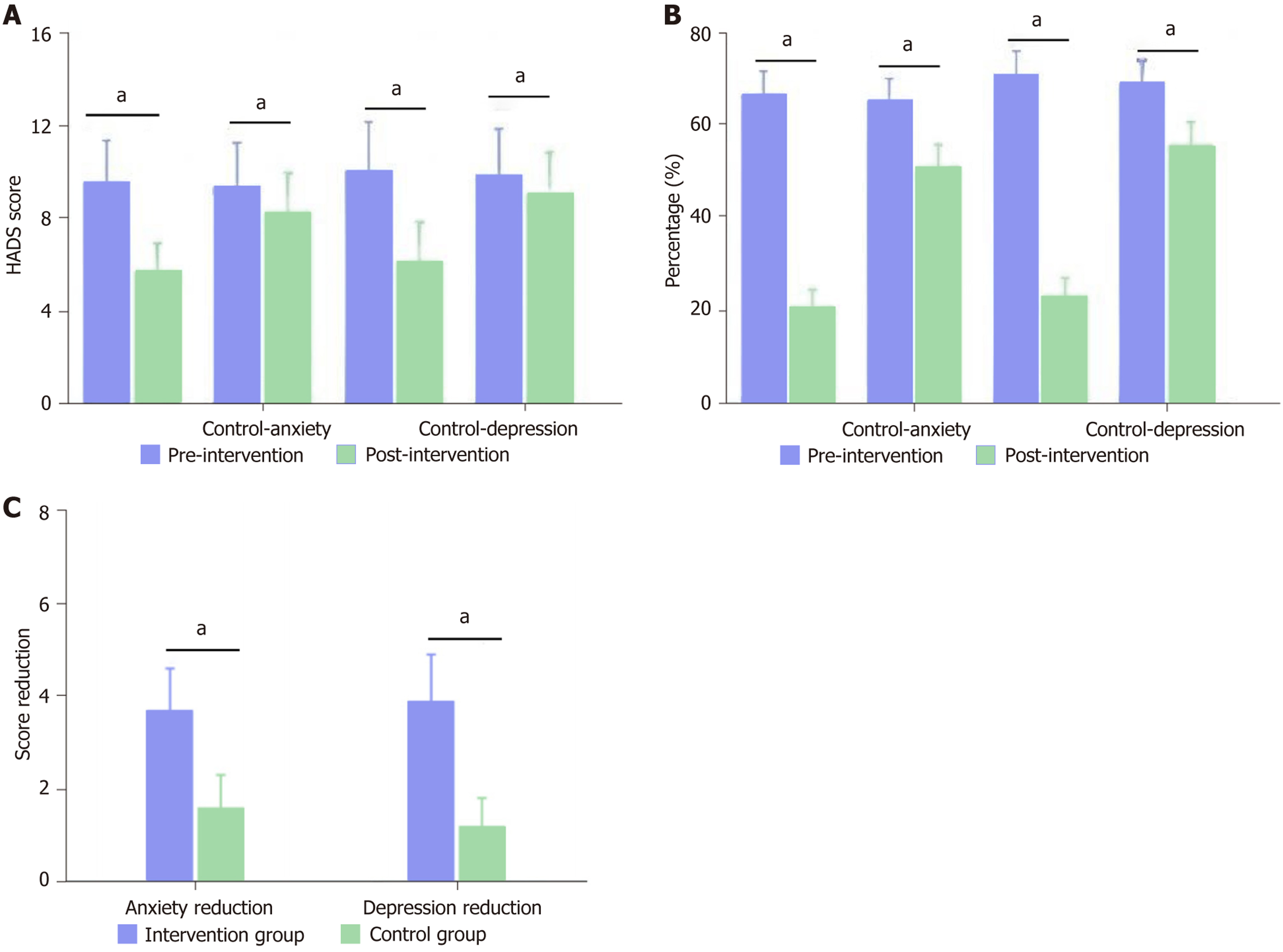
With regard to anxiety and depression outcomes, MBSR intervention showed significant clinical benefits. Compared to the control group, the intervention group had significantly lower HADS scores after intervention (anxiety: 5.8 ± 1.2 vs 8.3 ± 1.7, P < 0.001; depression: 6.2 ± 1.4 vs 9.1 ± 1.8, t = -16.47, P < 0.001). Pre-post intervention difference analysis showed that the intervention group's anxiety scores decreased by an average of 3.8 ± 0.9 points, while the control group only decreased by 1.1 ± 0.7 points (t = 24.19, P < 0.001), and depression scores decreased by 3.9 ± 1.0 points, while the control group decreased by 0.8 ± 0.6 points (P < 0.001). The proportion of patients with clinically significant anxiety (HADS-A ≥ 8) in the intervention group decreased from 69.3% to 21.4%, while that in the control group decreased from 67.9% to 52.9% (χ² = 35.86, P < 0.001). Similarly, the incidence of clinical depression (HADS-D ≥ 8) in the intervention group decreased from 73.6% to 24.3%, whereas that in the control group decreased from 71.4% to 57.9% (P < 0.001). The standardized effect sizes (Cohen's d) for MBSR on anxiety and depression were 1.68 (95%CI: 1.42-1.94) and 1.83 (95%CI: 1.56-2.10) respectively, indicating large treatment effects. These findings suggest that, compared to standard care, MBSR intervention significantly reduced psychological distress in post-operative cervical cancer patients (Figure 1).
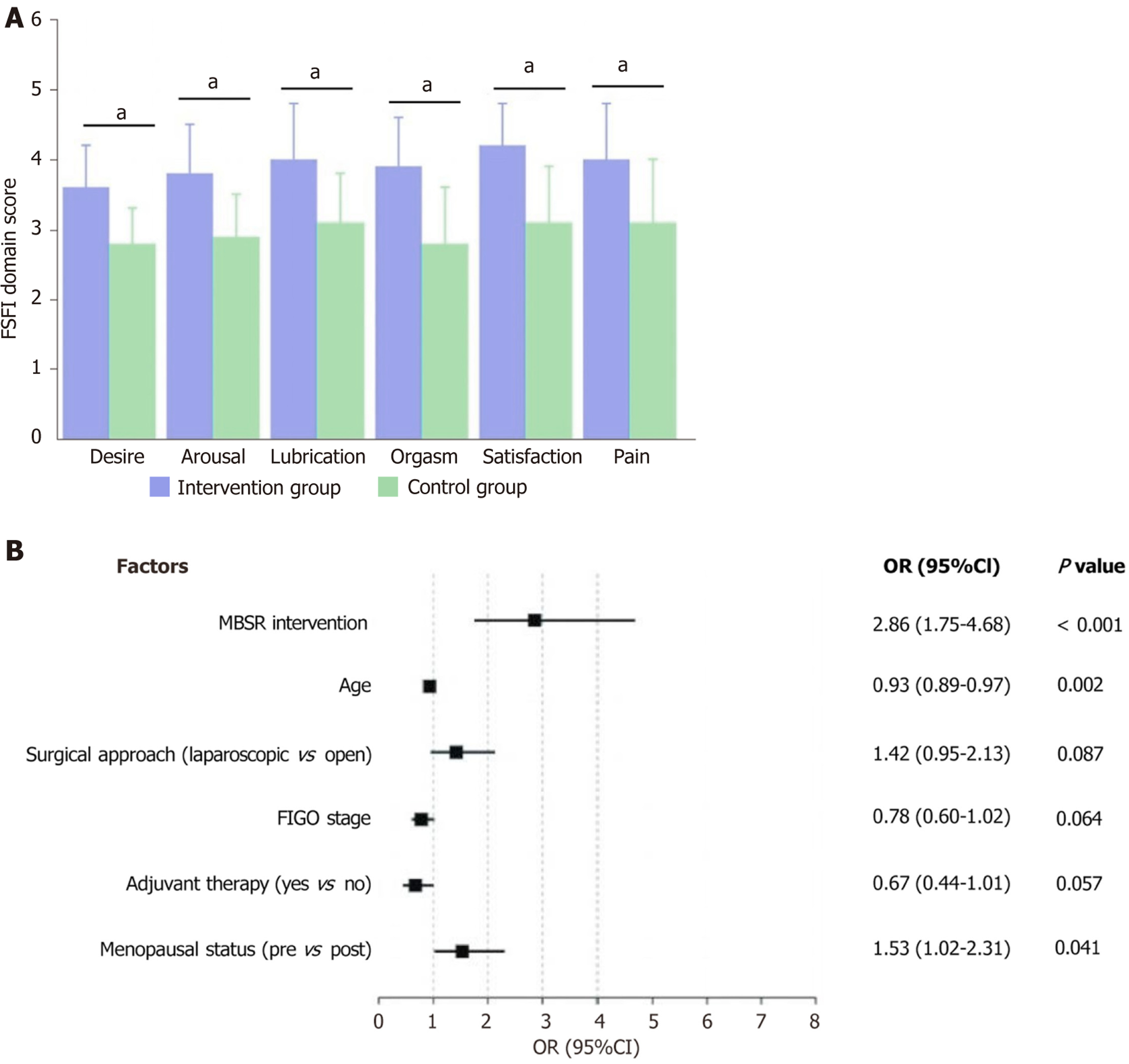
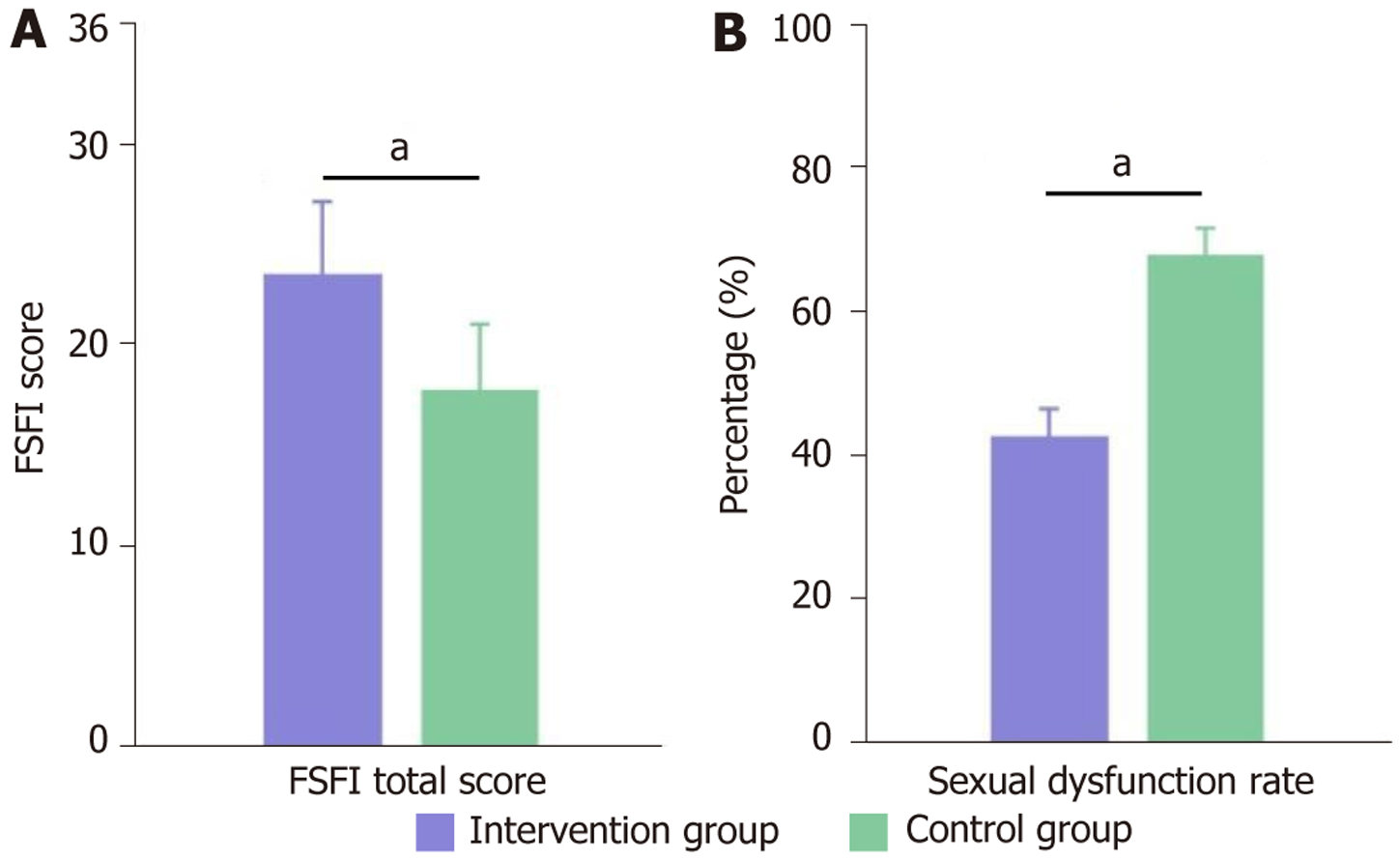
The sexual function assessment results showed that MBSR intervention significantly improved sexual function in patients with post-operative cervical cancer. After intervention (6 months post-surgery), the intervention group's FSFI total score (23.5 ± 3.6) was significantly higher than that of the control group (17.8 ± 3.2), with statistically significant differences (t = 15.27, P < 0.001). According to the criterion of sexual dysfunction defined as FSFI < 23 points, the incidence of sexual dysfunction in the intervention group was 42.9% (60/140), which was significantly lower than the control group's 67.9% (95/140; χ² = 21.36, P < 0.001), with an absolute risk difference of 25.0% (95%CI: 15.1%-34.9%) between the two groups. Further analysis of dimensional scores showed that the intervention group was superior to the control group in all six dimensions: Sexual desire (3.6 ± 0.6 vs 2.8 ± 0.5, t = 13.41, P < 0.001), sexual arousal (3.8 ± 0.7 vs 2.9 ± 0.6, t = 12.88, P < 0.001), vaginal lubrication (4.0 ± 0.8 vs 3.1 ± 0.7, t = 11.25, P < 0.001), orgasm (3.9 ± 0.7 vs 2.8 ± 0.8, t = 13.54, P < 0.001), sexual satisfaction (4.2 ± 0.6 vs 3.1 ± 0.8, t = 14.38, P < 0.001), and pain (4.0 ± 0.8 vs 3.1 ± 0.9, t = 9.74, P < 0.001). Multivariate analysis showed that after adjusting for factors such as age, surgical approach, staging, and adjuvant therapy, MBSR intervention was an independent protective factor for improving post-operative cervical cancer sexual function (OR = 2.86, 95%CI: 1.75-4.68, P < 0.001). Follow-up to 12 months post-surgery showed that the intervention group's FSFI total score continued to improve to 25.8 ± 3.9, with sexual dysfunction incidence decreasing to 29.3% (41/140), while the control group showed 19.2 ± 3.5 and 61.4% (86/140), respectively, with statistically significant differences maintained between the groups (P < 0.001). These results indicate that MBSR intervention can effectively improve sexual function in patients after radical cervical cancer surgery, and this improvement can last for at least 9 months (Figure 2).
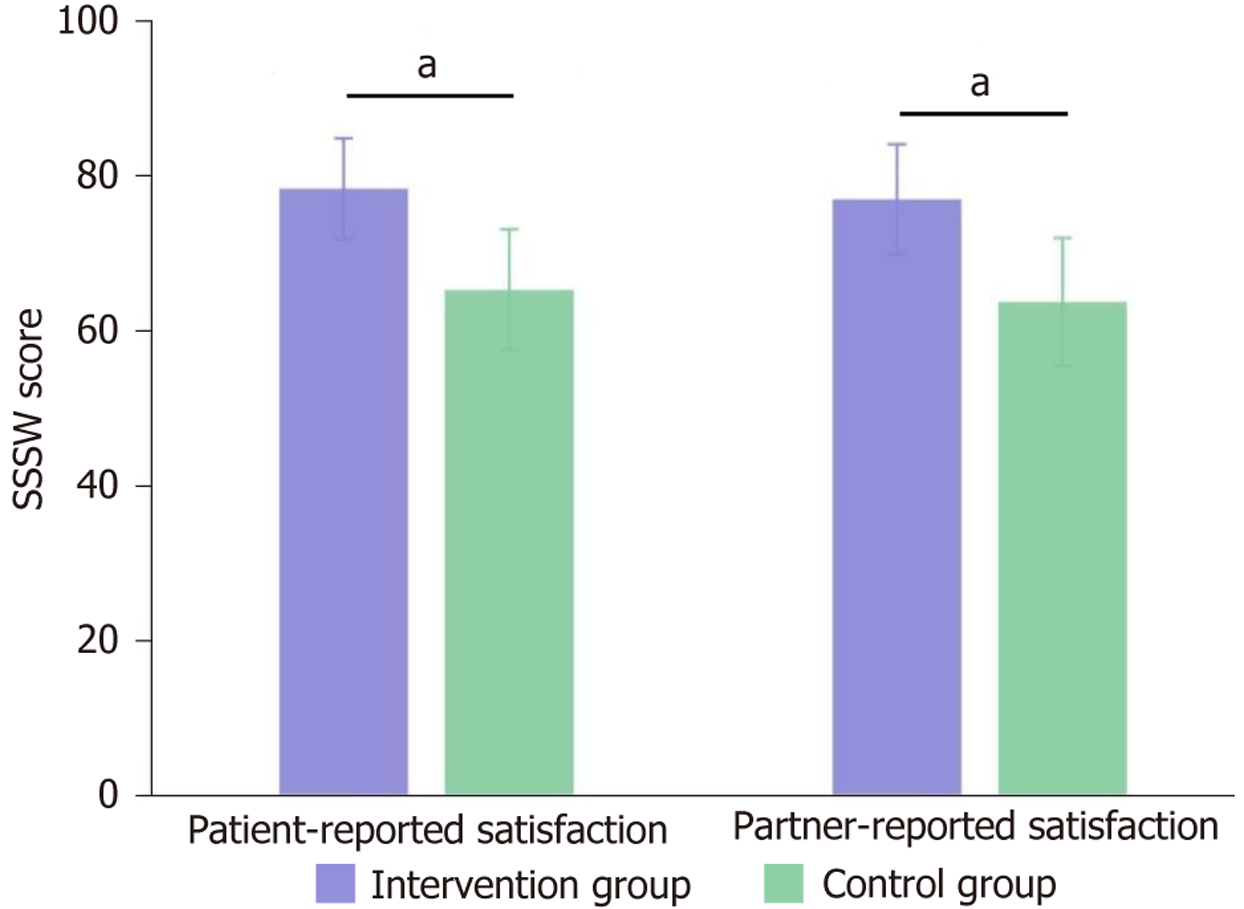
The sexual relationship satisfaction assessment results further validated the comprehensive effect of MBSR intervention in improving the sexual quality of life of post-cervical cancer surgery patients. According to the SSSW scores, the inter
Age-stratified analysis revealed age-related differential patterns in MBSR intervention effects, providing an important reference for individualized treatment in clinical practice. The study divided 280 patients into three age groups: ≤ 45 years (n = 95), 46-55 years (n = 121), and > 55 years (n = 64), and evaluated the improvement effects of MBSR intervention on sexual function in each age group. Results showed clear age gradients in intervention effects: In the ≤ 45 years group, the intervention group's FSFI total score was on average 6.8 points higher than the control group (24.6 ± 3.2 vs 17.8 ± 3.0), with 38.2% improvement amplitude and extremely significant statistical differences (P < 0.001); in the 46-55 years group, intervention effects were also significant, with FSFI total scores improving by 5.9 points (23.9 ± 3.4 vs 18.0 ± 3.1), representing 32.8% improvement (P < 0.001); in the > 55 years group, although intervention still produced positive effects, the degree of improvement was relatively weaker, with FSFI total scores improving by only 3.7 points (21.5 ± 3.8 vs 17.8 ± 3.5), representing 20.8% improvement, with statistical differences present but reduced significance(P = 0.032, Figure 4).
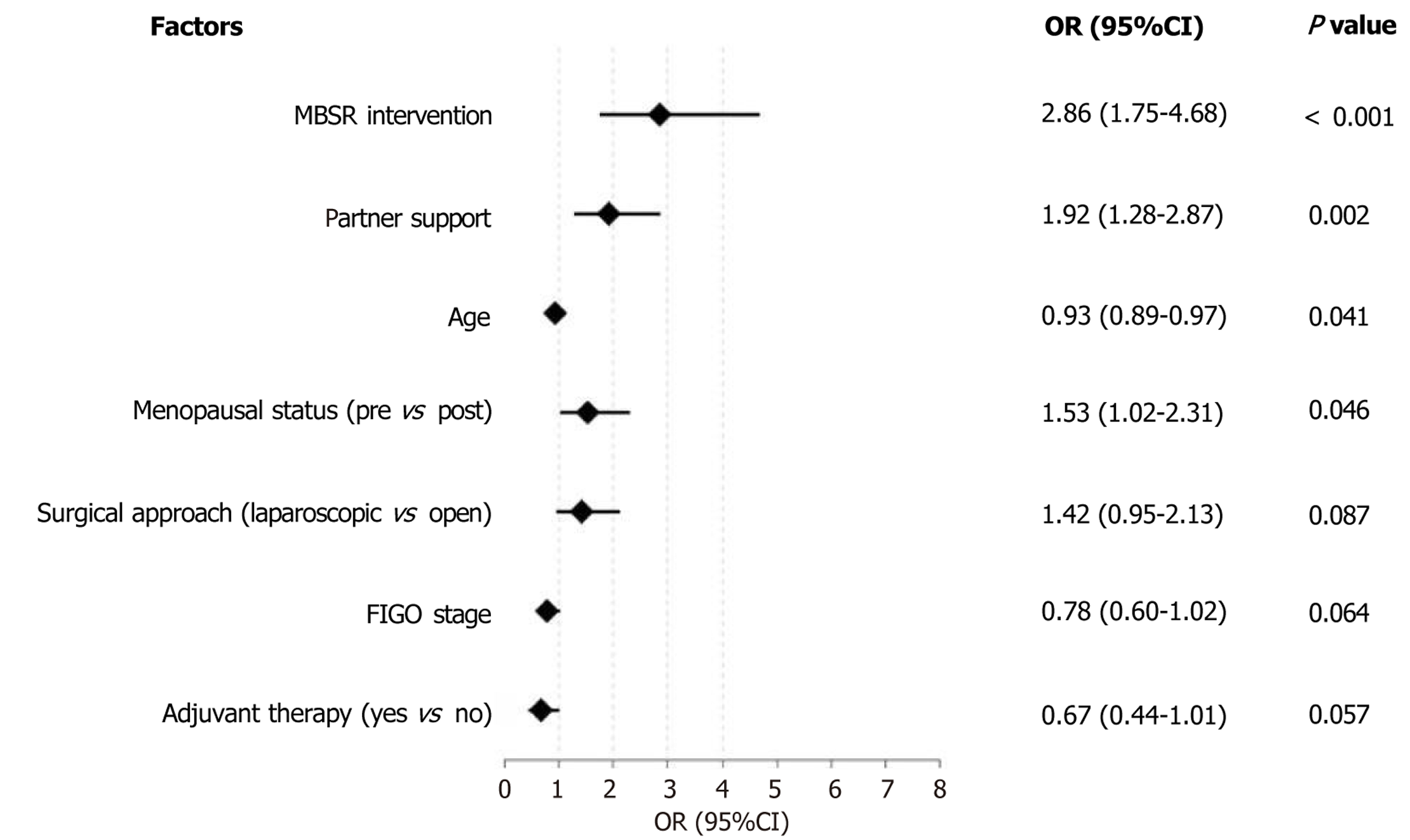
Multivariate logistic regression analysis further confirmed the independent value of MBSR intervention in the sexual psychological adaptation of patients post-cervical cancer surgery. After controlling for potential confounding factors such as age, education level, surgical approach, clinical staging, adjuvant therapy type, and marital status, MBSR intervention remained the strongest independent predictor of improving patients' sexual psychological adaptation status (OR = 2.86, 95%CI: 1.75-4.68, P < 0.001), indicating that patients receiving MBSR intervention were 2.86 times more likely to achieve good sexual psychological adaptation than those not receiving intervention. Partner support was also confirmed as another significant independent influencing factor (OR = 1.92, 95%CI: 1.28-2.87, P = 0.002), suggesting that high levels of partner support are associated with better sexual psychological adaptation outcomes. Other factors showing marginal statistical significance included age (OR = 0.93, 95%CI: 0.89-0.97, P = 0.041) and menopausal status (OR = 1.53, 95%CI: 1.02-2.31, P = 0.046), while education level, surgical approach, FIGO staging, adjuvant therapy type, and other factors were not statistically significant in the multivariate model (all P > 0.05; Figure 5).
This study systematically evaluated the impact of MBSR therapy on psychosexual adaptation through a retrospective analysis of clinical data from 280 patients after radical cervical cancer surgery[20]. The research results indicate that MBSR has significant effects in improving anxiety and depression, sexual function, and sexual relationship satisfaction in patients after radical cervical cancer surgery[21]. These effects maintain independence after controlling for potential confounding factors, providing important evidence for clinical practice.
Cervical cancer is a common malignant tumor in women. With the advancement of early screening and treatment technologies, the five-year survival rate has significantly improved; however, radical surgery, although effectively controlling disease progression, often leads to a series of physiological and psychological problems. Research shows that approximately 60%-80% of post-cervical cancer surgery patients experience varying degrees of sexual dysfunction, manifested as decreased libido, difficulty with sexual arousal, inadequate vaginal lubrication, painful intercourse, and orgasmic disorders, which stem from pelvic nerve damage, vaginal morphological changes, and endocrine dysfunction caused by surgery[22]. Simultaneously, patients often experience negative emotions such as anxiety, depression, low self-esteem, body image disorders, and fear, with research showing that the incidence of anxiety in post-cervical cancer surgery patients is 32.6%-68.3%[23,24], and the incidence of depression is 25.8%-53.7%[25,26], which is significantly higher than that in healthy women of the same age.
Traditional interventions often focus on either physiological sexual function rehabilitation or simple psychological support such as pelvic floor muscle training, vaginal dilator use guidance, sexual education, and routine psychological counseling. However, these interventions often separate the intrinsic connection between sexual dysfunction and psychological problems, lacking an integrative perspective and with limited clinical effectiveness[27,28]. Among post-cervical cancer surgery patients receiving routine sexual health guidance, 45%-60% still report persistent sexual dissatisfaction, and 30%-40% of patients' psychological distress due to sexual problems remains unresolved[29].
MBSR guides patients to perceive their current physical and mental experiences in a non-judgmental, fully accepting manner, gradually changing their cognitive patterns toward stressors, and enhancing psychological regulation capa
The results of this study show that patients in the MBSR intervention group achieved significant improvements in emotional state, sexual function, and sexual relationship satisfaction. Anxiety and depression scores and the incidence of clinically significant emotional disorders were significantly reduced compared to the control group, indicating that MBSR helps alleviate negative emotions in post-cervical cancer surgery patients[34]. This may be related to the emphasis on accepting current experiences and reducing self-judgment in MBSR, helping patients more positively face body changes and sexual dysfunction, and reducing related psychological pressure[35]. Additionally, body scanning, breath awareness, and other exercises in MBSR training can promote parasympathetic nervous system activity, reduce physiological anxiety responses, and alleviate anxiety and depression symptoms[36].
Regarding sexual function assessment, the intervention group's FSFI total score improved from 17.8 ± 3.2 to 23.5 ± 3.6, representing a clinically meaningful advancement along the sexual recovery trajectory. While the post-intervention score of 23.5 remained close to the sexual dysfunction cutoff (FSFI < 23), this improvement represents significant clinical progress that warrants careful interpretation. The transition from severe sexual dysfunction (17.8) to borderline normal function (23.5) constitutes a 32% improvement that translates into tangible benefits for patients' quality of life and intimate relationships.
It is important to emphasize that MBSR should be viewed as part of a comprehensive rehabilitation approach rather than as a standalone cure for sexual dysfunction. The intervention group (57.1%) who achieved an FSFI ≥ 23 (compared to 32.1% in controls) demonstrated that a substantial proportion of patients achieved functional sexual recovery through MBSR intervention. For the remaining patients who continued to experience some degree of dysfunction, the imp
The concept of "sexual recovery trajectory" is crucial for understanding these results. Postsurgical sexual dysfunction typically follows a gradual recovery pattern, and even modest improvements can significantly impact patients' con
Regarding sexual function assessment, the intervention group's FSFI total score and scores in all six dimensions were significantly higher than those of the control group, with a markedly lower incidence of sexual dysfunction. This result aligns with the core mechanisms of MBSR: By enhancing sensitivity to bodily sensations and increasing the ability to focus on the present, patients can better perceive and enjoy positive sensations in sexual experiences, reduce excessive focus on pain and discomfort, and lower performance anxiety and negative self-evaluation in sexual activities, thereby improving physiological responses such as sexual arousal and lubrication as well as subjective experiences[37].
Notably, both patients in the intervention group and their partners reported significantly higher sexual relationship satisfaction, with high consistency in their scores, indicating that the sexual relationship improvement brought about by MBSR is a real experience perceived by both parties, not a subjective preference of one side[38]. This may be related to MBSR's promotion of communication, enhancement of intimacy, and improvement in partner interaction patterns.
Age-stratified analysis showed clear age gradients in MBSR intervention effects, with more significant effects in younger patients, providing a reference for individualized treatment in clinical practice. The differential response pat
Multivariate regression analysis further confirmed that MBSR intervention remains an independent predictor of improved sexual psychological adaptation in post-cervical cancer surgery patients after controlling for multiple potential confounding factors while also finding that partner support level is another important influencing factor.
This result highlights the importance of implementing MBSR within a multidisciplinary care framework that includes gynecologic oncology, psychology, sexual health specialists, and couples’ therapy when appropriate. The synergistic effects of MBSR and partner support suggest that interventions should ideally involve both patients and their partners to maximize therapeutic benefits. Future research should explore the optimal timing, duration, and intensity of MBSR interventions as well as potential combination therapies with medical treatments (such as vaginal estrogen therapy, pelvic floor physiotherapy, or sexual aids). Long-term follow-up studies beyond 12 months are needed to understand the durability of treatment effects and to identify patients who may benefit from booster sessions or additional interventions.
This result highlights that in clinical practice, attention needs to be paid not only to individual psychological inter
While our study demonstrated the effectiveness of MBSR for psychosexual recovery, several limitations warrant consideration. The retrospective design limits causal inference, and the cultural context (Chinese healthcare settings) may affect generalizability to other populations. Additionally, the lack of active control groups (such as other psychotherapy modalities) prevents direct comparison of MBSR's relative effectiveness of MBSR. Future randomized controlled trials with active comparators and longer follow-up periods are needed to strengthen the evidence.
In conclusion, this study shows that MBSR, as an integrative mind-body intervention method, can effectively improve anxiety and depression, sexual function, and sexual relationship satisfaction in patients after radical cervical cancer surgery, with lasting effects that maintain independence after controlling for confounding factors, making it worth promoting in clinical practice as an important means for sexual psychological rehabilitation in post-cervical cancer surgery patients.
| 1. | Hayashi S, Kumai T, Michizuka T, Osaki T. Thyroid metastasis from cervical carcinoma. Braz J Otorhinolaryngol. 2023;89:101268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 2. | Kwok MM, Virk JS, Michael M, McKinley M, Magarey MJR. Cervical Nodal Metastatic Pituitary Carcinoma: A Case Report. Ear Nose Throat J. 2022;101:110-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 3. | Lahouti AH, Asiry S, Giampoli EJ. Pituitary carcinoma: A cytopathologic dilemma when metastatic to cervical lymph nodes. Diagn Cytopathol. 2023;51:E94-E97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Plotti F, Sansone M, Di Donato V, Antonelli E, Altavilla T, Angioli R, Panici PB. Quality of life and sexual function after type C2/type III radical hysterectomy for locally advanced cervical cancer: a prospective study. J Sex Med. 2011;8:894-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Rajendran S, McGivern U, Gonzalez D, McCluggage WG. Cervical Gastric-type Adenosquamous Carcinoma: Case Report of a Rare Neoplasm Associated With a BRCA1 Pathogenic Variant. Int J Gynecol Pathol. 2023;42:529-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Stolnicu S, Hoang L, Zhou Q, Iasonos A, Terinte C, Pesci A, Aviel-Ronen S, Kiyokawa T, Alvarado-Cabrero I, Oliva E, Park KJ, Soslow RA. Cervical Adenosquamous Carcinoma: Detailed Analysis of Morphology, Immunohistochemical Profile, and Outcome in 59 Cases. Int J Gynecol Pathol. 2023;42:259-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 7. | Zheng W, Jin F, Wang F, Wang L, Fu S, Pan Z, Long H. Analysis of eEF1A2 gene expression and copy number in cervical carcinoma. Medicine (Baltimore). 2023;102:e32559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Alzahrani AM, Hakami A, AlHadi A, Al-Maflehi N, Aljawadi MH, Alotaibi RM, Alzahrani MM, Alammari SA, Batais MA, Almigbal TH. The effectiveness of mindfulness training in improving medical students' stress, depression, and anxiety. PLoS One. 2023;18:e0293539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 9. | Burrowes SAB, Goloubeva O, Stafford K, McArdle PF, Goyal M, Peterlin BL, Haythornthwaite JA, Seminowicz DA. Enhanced mindfulness-based stress reduction in episodic migraine-effects on sleep quality, anxiety, stress, and depression: a secondary analysis of a randomized clinical trial. Pain. 2022;163:436-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 10. | Crovetto F, Crispi F, Casas R, Martín-Asuero A, Borràs R, Vieta E, Estruch R, Gratacós E; IMPACT BCN Trial Investigators. Effects of Mediterranean Diet or Mindfulness-Based Stress Reduction on Prevention of Small-for-Gestational Age Birth Weights in Newborns Born to At-Risk Pregnant Individuals: The IMPACT BCN Randomized Clinical Trial. JAMA. 2021;326:2150-2160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 80] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 11. | Crovetto F, Nakaki A, Arranz A, Borras R, Vellvé K, Paules C, Boutet ML, Castro-Barquero S, Freitas T, Casas R, Martín-Asuero A, Oller Guzmán T, Morilla I, Martínez-Àran A, Camacho A, Pasqual M, Izquierdo Renau M, Pozo ÓJ, Gomez-Gomez A, Estruch R, Vieta E, Crispi F, Gratacós E. Effect of a Mediterranean Diet or Mindfulness-Based Stress Reduction During Pregnancy on Child Neurodevelopment: A Prespecified Analysis of the IMPACT BCN Randomized Clinical Trial. JAMA Netw Open. 2023;6:e2330255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 25] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 12. | Ghawadra SF, Lim Abdullah K, Choo WY, Danaee M, Phang CK. The effect of mindfulness-based training on stress, anxiety, depression and job satisfaction among ward nurses: A randomized control trial. J Nurs Manag. 2020;28:1088-1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 62] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 13. | Javadzade N, Esmaeili SV, Omranifard V, Zargar F. Effect of mindfulness-based stress reduction (MBSR) program on depression, emotion regulation, and sleep problems: A randomized controlled trial study on depressed elderly. BMC Public Health. 2024;24:271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 22] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 14. | Young LA, Baime MJ. Mindfulness-Based Stress Reduction: Effect on Emotional Distress in Older Adults. Complement Health Pract Rev. 2010;15:59-64. [RCA] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Lensen JH, Stoltz SEMJ, Kleinjan M, Speckens AEM, Kraiss JT, Scholte RHJ. Mindfulness-based stress reduction intervention for elementary school teachers: a mixed method study. Trials. 2021;22:826. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Lenze EJ, Voegtle M, Miller JP, Ances BM, Balota DA, Barch D, Depp CA, Diniz BS, Eyler LT, Foster ER, Gettinger TR, Head D, Hershey T, Klein S, Nichols JF, Nicol GE, Nishino T, Patterson BW, Rodebaugh TL, Schweiger J, Shimony JS, Sinacore DR, Snyder AZ, Tate S, Twamley EW, Wing D, Wu GF, Yang L, Yingling MD, Wetherell JL. Effects of Mindfulness Training and Exercise on Cognitive Function in Older Adults: A Randomized Clinical Trial. JAMA. 2022;328:2218-2229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 91] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 17. | Liu L, Tian L, Jiang J, Zhang Y, Chi X, Liu W, Zhao YH, Sun P. Effect of an Online Mindfulness-Based Stress Reduction Intervention on Postpandemic Era Nurses' Subjective Well-being, Job Burnout, and Psychological Adaptation. Holist Nurs Pract. 2023;37:244-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Nakaki A, Crovetto F, Urru A, Piella G, Borras R, Comte V, Vellvé K, Paules C, Segalés L, Dacal M, Gomez Y, Youssef L, Casas R, Castro-Barquero S, Martín-Asuero A, Oller Guzmán T, Morilla I, Martínez-Àran A, Camacho A, Pascual Tutusaus M, Arranz A, Rebollo-Polo M, Gomez-Chiari M, Bargallo N, Pozo ÓJ, Gomez-Gomez A, Izquierdo Renau M, Eixarch E, Vieta E, Estruch R, Crispi F, Gonzalez-Ballester MA, Gratacós E. Effects of Mediterranean diet or mindfulness-based stress reduction on fetal and neonatal brain development: a secondary analysis of a randomized clinical trial. Am J Obstet Gynecol MFM. 2023;5:101188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 19. | Pérez V, Menéndez-Crispín EJ, Sarabia-Cobo C, de Lorena P, Fernández-Rodríguez A, González-Vaca J. Mindfulness-Based Intervention for the Reduction of Compassion Fatigue and Burnout in Nurse Caregivers of Institutionalized Older Persons with Dementia: A Randomized Controlled Trial. Int J Environ Res Public Health. 2022;19:11441. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 39] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 20. | Yang X, Huang L, Li C, Ji N, Zhu H. The effectiveness of mindfulness-based stress reduction intervention on alleviating anxiety and depression in postoperative patients with cervical cancer: A protocol for systematic review and meta-analysis. Medicine (Baltimore). 2022;101:e28706. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Banbury S, Chandler C, Lusher J. A Systematic Review Exploring the Effectiveness of Mindfulness for Sexual Functioning in Women with Cancer. Psych. 2023;5:194-208. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Shan X, Qian M, Wang L, Liu X. Prevalence of pelvic floor dysfunction and sexual dysfunction in cervical cancer survivors: a systematic review and meta-analysis. Int Urogynecol J. 2023;34:655-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 23. | Wang HZ, He RJ, Zhuang XR, Xue YW, Lu Y. Assessment of long-term sexual function of cervical cancer survivors after treatment: A cross-sectional study. J Obstet Gynaecol Res. 2022;48:2888-2895. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 24. | Tosic Golubovic S, Binic I, Krtinic D, Djordjevic V, Conic I, Gugleta U, Andjelkovic Apostolovic M, Stanojevic M, Kostic J. Risk Factors and Predictive Value of Depression and Anxiety in Cervical Cancer Patients. Medicina (Kaunas). 2022;58:507. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 23] [Reference Citation Analysis (0)] |
| 25. | Qian M, Wang L, Xing J, Shan X, Wu J, Liu X. Prevalence of sexual dysfunction in women with cervical cancer: a systematic review and meta-analysis. Psychol Health Med. 2023;28:494-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 26. | Membrilla-Beltran L, Cardona D, Camara-Roca L, Aparicio-Mota A, Roman P, Rueda-Ruzafa L. Impact of Cervical Cancer on Quality of Life and Sexuality in Female Survivors. Int J Environ Res Public Health. 2023;20:3751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 22] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 27. | Cyr MP, Jones T, Brennen R, Colombage U, Frawley HC. Effectiveness of Pelvic Floor Muscle and Education-Based Therapies on Bladder, Bowel, Vaginal, Sexual, Psychological Function, Quality of Life, and Pelvic Floor Muscle Function in Females Treated for Gynecological Cancer: A Systematic Review. Curr Oncol Rep. 2024;26:1293-1320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 28. | Araya-Castro P, Roa-Alcaino S, Celedón C, Cuevas-Said M, de Sousa Dantas D, Sacomori C. Barriers to and facilitators of adherence to pelvic floor muscle exercises and vaginal dilator use among gynecologic cancer patients: a qualitative study. Support Care Cancer. 2022;30:9289-9298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 29. | Tramacere F, Lancellotta V, Casà C, Fionda B, Cornacchione P, Mazzarella C, De Vincenzo RP, Macchia G, Ferioli M, Rovirosa A, Gambacorta MA, Colosimo C, Valentini V, Iezzi R, Tagliaferri L. Assessment of Sexual Dysfunction in Cervical Cancer Patients after Different Treatment Modality: A Systematic Review. Medicina (Kaunas). 2022;58:1223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 30. | Yavuz Sercekman M. Exploring the sustained impact of the Mindfulness-Based Stress Reduction program: a thematic analysis. Front Psychol. 2024;15:1347336. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 31. | Kogias N, Geurts DEM, Krause F, Speckens AEM, Hermans EJ. Study protocol for a randomised controlled trial investigating the effects of Mindfulness Based Stress Reduction on stress regulation and associated neurocognitive mechanisms in stressed university students: the MindRest study. BMC Psychol. 2023;11:194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 32. | Sánchez-Sánchez LC, Valderrama Rodríguez MF. [Mindfulness in the sexual health and psychological well-being of professionals and caregivers of people at risk of social exclusion]. Rev Int Androl. 2022;20:54-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 33. | Chayadi E, Baes N, Kiropoulos L. The effects of mindfulness-based interventions on symptoms of depression, anxiety, and cancer-related fatigue in oncology patients: A systematic review and meta-analysis. PLoS One. 2022;17:e0269519. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 73] [Reference Citation Analysis (0)] |
| 34. | Chang YC, Lin GM, Yeh TL, Chang YM, Yang CH, Lo C, Yeh CY, Hu WY. Impact of mindfulness-based stress reduction on female sexual function and mental health in patients with breast cancer. Support Care Cancer. 2022;30:4315-4325. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 35. | Guu SF, Chao YP, Huang FY, Cheng YT, Ng HH, Hsu CF, Chuang CH, Huang CM, Wu CW. Interoceptive awareness: MBSR training alters information processing of salience network. Front Behav Neurosci. 2023;17:1008086. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 36. | Juul L, Bonde EH, Fjorback LO. Altered self-reported resting state mediates the effects of Mindfulness-Based Stress Reduction on mental health: a longitudinal path model analysis within a community-based randomized trial with 6-months follow-up. Front Psychol. 2023;14:1154277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 37. | Brotto LA, Zdaniuk B, Chivers ML, Jabs F, Grabovac AD, Lalumière ML. Mindfulness and Sex Education for Sexual Interest/Arousal Disorder: Mediators and Moderators of Treatment Outcome. J Sex Res. 2023;60:508-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 38. | Beaulieu N, Bergeron S, Brassard A, Byers ES, Péloquin K. Toward an Integrative Model of Intimacy, Sexual Satisfaction, and Relationship Satisfaction: A Prospective Study in Long-Term Couples. J Sex Res. 2023;60:1100-1112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 39. | Marzola P, Melzer T, Pavesi E, Gil-Mohapel J, Brocardo PS. Exploring the Role of Neuroplasticity in Development, Aging, and Neurodegeneration. Brain Sci. 2023;13:1610. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 100] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/