Published online Oct 19, 2025. doi: 10.5498/wjp.v15.i10.109502
Revised: June 19, 2025
Accepted: August 6, 2025
Published online: October 19, 2025
Processing time: 136 Days and 5.4 Hours
The coronavirus disease 2019 pandemic has left an indelible mark on global mental health, with widespread psychological consequences that persist beyond the acute phase of the virus. This review synthesizes current evidence on the post-pandemic mental health burden across diverse populations, highlighting elevated rates of depression, anxiety, posttraumatic stress, and substance use disorders linked to prolonged social isolation, economic instability, and grief. We examine disparities in psychological outcomes among vulnerable groups (e.g., healthcare workers, survivors, marginalized communities) and identify key challenges in addressing these issues, including fragmented healthcare systems, stigma, and the limited scalability of interventions. Emerging evidence on resilience factors (e.g., social support and adaptive coping) is also discussed. Finally, we propose critical priorities for future research, including longitudinal studies on the chronic mental health effects, the development of culturally tailored interventions, and the integration of digital mental health solutions. This review distinctively addresses enduring post-pandemic mental health challenges, integrating neurobiological insights, equity-focused interventions, and critical perspectives on digital so
Core Tip: The coronavirus disease 2019 (COVID-19) pandemic has exacerbated global mental health disparities, disproportionately affecting vulnerable groups (e.g., healthcare workers, youth, and marginalized communities). Unique pandemic stressors (e.g., social isolation, economic instability, and long COVID-related neuropsychiatric symptoms) have created new risk pathways. Systemic barriers such as fragmented care, stigma, and digital inequities limit intervention scalability, especially in low-resource settings. Evidence highlights resilience factors (social support, adaptive coping) and urgent priorities: Longitudinal research on chronic outcomes, culturally adapted interventions, and policy reforms integrating mental health into primary care and digital platforms. This crisis demands equity-focused, multidisciplinary action to mitigate long-term consequences.
- Citation: Ding W, Zhang Y, Wang MZ, Wang S. Post-pandemic mental health: Understanding the global psychological burden and charting future research priorities. World J Psychiatry 2025; 15(10): 109502
- URL: https://www.wjgnet.com/2220-3206/full/v15/i10/109502.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i10.109502
The coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been one of the most disruptive global health crises in modern history, with profound and lasting impacts that extend far beyond its immediate medical consequences[1-3]. While much attention has been devoted to understanding the virological and immunological aspects of SARS-CoV-2[4,5], the psychological repercussions of the pandemic have emerged as a parallel public health emergency[6,7], with increasing evidence suggesting that the mental health toll may persist for years to come[8,9]. Even as the acute phase of infection subsides, societies worldwide continue to experience elevated rates of depression, anxiety, posttraumatic stress disorder (PTSD)[10,11], and other psychiatric conditions, exacerbated by prolonged social isolation, economic instability, and collective grief[6,12,13]. The unique combination of mass morbidity, mortality, and sustained public health restrictions during and after the COVID-19 pandemic has created an unprecedented mental health burden, necessitating urgent scholarly and policy attention[13-15].
The psychological aftermath of the pandemic has not been uniformly distributed, with significant disparities observed across demographic and socioeconomic groups[16,17]. Unlike pre-pandemic mental health challenges, the COVID-19 crisis introduced unique stressors such as mass morbidity, sustained public health restrictions, and collective grief, which exacerbated existing conditions and triggered new forms of psychological distress (e.g., pandemic-related PTSD)[18-20]. Frontline healthcare workers, COVID-19 survivors, individuals with preexisting mental health conditions, and economically vulnerable populations have been disproportionately affected, highlighting the role of structural inequities in shaping mental health outcomes[21-24]. Furthermore, the pandemic has exposed critical weaknesses in mental healthcare systems globally, including insufficient resources, fragmented service delivery, and persistent stigma surrounding mental illness[22,25,26]. Despite the growing recognition of these challenges, there remains a pressing need to consolidate existing research, identify gaps in knowledge, and establish a cohesive framework for future intervention strategies[26,27].
This review seeks to address these gaps by providing a comprehensive synthesis of the post-pandemic mental health landscape. Specifically, we aim to assess the magnitude and scope of psychological distress across different populations; examine the underlying biological, social, and economic determinants of these outcomes; and propose actionable research priorities to guide policymakers, clinicians, and researchers in mitigating long-term mental health consequences. While existing reviews catalogued acute-phase distress, our work uniquely analyzes longitudinal data on chronicity (> 24 months post-outbreak), bridges neuropsychiatric (e.g., viral persistence) and social determinants (e.g., pandemic-driven inequities), and evaluates scalable interventions post-2022, including low-cost artificial intelligence (AI) tools and policy reforms for low- and middle-income countries (LMICs)[23,28,29]. We synthesized evidence from English-language literature published between 2019 and 2025, retrieved from databases including PubMed, Web of Science, and PsycINFO. Key search terms included combinations of “post-pandemic mental health”, “COVID-19”, “psychological burden”, “mental health outcomes”, and “global mental health”. Priority was given to peer-reviewed articles, meta-analyses, and longitudinal studies addressing post-pandemic psychological effects. Grey literature and non-English publications were excluded to maintain focus on high-impact, widely accessible research. While this is not a systematic review, the selection aimed to represent diverse populations, geographic regions, and methodological approaches to ensure comprehensive coverage of the topic. By integrating findings from epidemiological studies, clinical reports, and public health analyses, this review underscores the necessity of a multidisciplinary approach to effectively respond to what has been termed the “shadow pandemic” of mental health deterioration.
While depression and anxiety existed pre-pandemic, their prevalence surged post-COVID-19 due to pandemic-specific drivers (e.g., economic instability, healthcare system strain), with meta-analyses showing a 20%-30% increase in cases compared to baseline rates[13,30,31]. The Global Burden of Disease Study 2021 highlights significant trends in mental health, with depressive and anxiety disorders ranking as the second and sixth leading causes of years lived with disability globally[32,33]. Between 2010 and 2021, age-standardized disability-adjusted life-years increased by 16.4% for depressive disorders and 16.7% for anxiety disorders, underscoring their growing burden[11,32,33]. Depression and generalized anxiety disorder have emerged as two of the most commonly reported conditions, affecting approximately 25%-30% of the surveyed populations in multiple countries[34-36]. Notably, PTSD symptoms linked to pandemic-related experiences have been documented in 15%-20% of individuals, with healthcare workers and COVID-19 survivors exhibiting particularly high vulnerability[18,19,37]. Substance use disorders, including alcohol misuse and opioid dependence, have also increased, reflecting maladaptive coping mechanisms in response to prolonged stress and social disruption[38,39].
Critically, pre-pandemic mental health burdens (e.g., chronic depression linked to socioeconomic status) persisted independently of COVID-19. However, pandemic-specific stressors, such as social isolation[40] or long COVID-related cognitive impairment[41], created new risk pathways not observed in earlier data. This divergence underscores the importance of disaggregating enduring inequities from acute pandemic effects. In addition, the psychological toll extends beyond clinically diagnosable conditions, encompassing subthreshold distress that nevertheless impairs daily functioning[42]. Insomnia, fatigue, and emotional dysregulation have become widespread and often co-occur with more severe disorders[43-45]. The pandemic’s mental health consequences are further compounded by delays in help-seeking behavior, as many individuals avoid clinical settings due to fear of infection or perceived stigma[46-48]. This treatment gap underscores the need for proactive mental health screening and accessible interventions[49,50].
The COVID-19 pandemic exacerbated mental health burdens in specific populations, though the magnitude varied across demographics and pre-existing conditions. While pooled estimates indicate a 25%-30% rise in depression and anxiety globally [95% confidence interval (CI): 22%-34%][10,11,13,51], certain groups such as particularly women, youth, and frontline workers experienced disproportionate rises in psychiatric morbidity due to pandemic-specific stressors (e.g., caregiving burdens, educational disruptions)[6,24,52-54]. Notably, some general population studies found stable or only transiently elevated distress post-COVID-19, underscoring the need for subgroup-specific analyses[11,55]. Vulnerable populations bear a disproportionate share of this burden. For example, frontline healthcare workers exhibit PTSD rates comparable to those observed in military combat veterans, driven by exposure to patient deaths, moral injury, and workplace exhaustion[21,56,57]. COVID-19 survivors, particularly those with long-term physical symptoms (“long COVID”), frequently report cognitive impairments (“brain fog”) and emotional lability, suggesting a bidirectional relationship between viral infection and mental health deterioration[41,58-61]. Economic disparities further stratify risk: Low-income households, ethnic minorities, and informal laborers face heightened psychological distress due to job loss, housing insecurity, and limited healthcare access[34,53,62,63]. Pooled data indicate a 25%-30% relative increase in depression and anxiety for women, especially caregivers (vs 10%-15% in men), linked to gendered caregiving roles and economic precarity[6,11,52,64,65]. The COVID-19 pandemic exacerbated mental health challenges, particularly among youth, due to social restrictions and educational disruptions rather than direct viral effects[14,54,66]. Adolescents showed significantly higher risk of suicidal ideation post-pandemic compared to pre-pandemic baselines[53,67], conversely, older adults, while initially assumed to be at the highest risk, demonstrate surprising resilience in some cohorts, possibly due to greater life experience and coping skills[11,52,65,68]. A concerning trend is the rise in suicidal ideation, especially among young adults and adolescents, with studies attributing this to disrupted education, social isolation, and economic precarity[69-72].
Geographical variations in mental health outcomes highlight the role of structural and cultural factors[73,74]. High-income countries with robust mental health infrastructures, such as those in Western Europe, still face service overload and unmet demand[75-78]. While high-income nations with robust safety nets (e.g., Germany, Australia) saw transient distress spikes (SMD = 0.15-0.30)[75,79,80], LMICs faced sustained elevations (SMD = 0.45-0.60), mediated by healthcare gaps[53,73,81], highlighting the moderating role of policy. The stigma surrounding mental illness remains a pervasive barrier in many LMICs, while high-income nations face challenges in equitable service distribution[75-78,82,83]. Emerging longitudinal studies (2023-2024) reveal that 25%-40% of long COVID patients in LMICs develop persistent depression or cognitive impairment[84,85]. In Brazil and India, socioeconomic disparities exacerbate these outcomes, with low-income survivors reporting 2.3-fold higher PTSD rates than high-income cohorts[19,86]. Post-2022 studies highlight divergent recovery trajectories. while high-income nations show stabilization[55], LMICs face compounding crises. In sub-Saharan Africa[73], pandemic-related job losses correlated with a 32% rise in depression prevalence, double pre-pandemic rates. South Asian studies[87] report escalating adolescent suicidality linked to school closures and child labor resurgence, emphasizing the need for culturally grounded interventions. Cross-cultural studies also reveal differences in symptom expression: Somatic complaints (e.g., headaches, gastrointestinal distress) are more commonly reported in Asian and Latin American populations than overt psychological symptoms are emphasized in Western populations[88,89].
The cumulative evidence highlights a picture of a global mental health emergency that transcends national borders and healthcare systems. While acute pandemic measures may have receded, their psychological aftershocks persisted, demanding urgent, coordinated responses[3,18,19,36].
This section focuses exclusively on risk and resilience factors amplified or uniquely triggered by the COVID-19 pandemic, supported by longitudinal studies comparing pre- and post-pandemic data. General mental health determinants (e.g., genetic predisposition) are noted only where they interact with pandemic-specific stressors (e.g., SARS-CoV-2 neurotropism exacerbating pre-existing depression).
The mental health repercussions of the COVID-19 pandemic stem from a complex interplay of biological, psychological, and socioeconomic factors. Understanding these multifaceted determinants is crucial for developing targeted interventions and mitigating long-term consequences. Emerging research highlights several key mechanisms through which the pandemic has exacerbated psychological distress while also identifying protective factors that foster resilience amid adversity.
The unprecedented nature of COVID-19 has introduced unique stressors that have profoundly disrupted daily life. Prolonged social isolation, a hallmark of public health measures, erodes support networks and increases feelings of loneliness, particularly among older adults and young people[10,34,40,90-92]. Economic instability, including job losses, business closures, and financial insecurity, has emerged as a major predictor of anxiety and depression, with studies showing that individuals facing unemployment are twice as likely to report suicidal ideation as those with stable incomes[93,94]. Bereavement, compounded by restrictions on traditional mourning practices, further intensifies grief-related mental health challenges, with many individuals experiencing prolonged or complicated grief reactions[21,95,96].
Healthcare systems themselves have become sources of trauma, particularly for frontline workers[97,98]. Moral injury is widespread among clinicians forced to ration care or witness preventable deaths[21,23,99]. Media saturation and misinformation amplify fear and uncertainty, contributing to “pandemic fatigue” and a pervasive sense of helplessness[100,101]. Additionally, the virus’s direct neurological effects, including neuroinflammation and hypoxia, may exacerbate psychiatric symptoms in COVID-19 survivors, particularly those with preexisting mental health conditions[102-104].
Despite these challenges, research has also identified factors that buffer against psychological distress. Social support, whether from family, friends, or online communities, significantly mitigates the effects of isolation, particularly when individuals maintain regular virtual contact[105,106]. Adaptive coping strategies, such as mindfulness, physical exercise, and structured routines, are associated with lower levels of anxiety and depression[107-110]. Compared with more fragmented societies, communities with strong social cohesion have better mental health outcomes[111,112].
Individual differences in resilience also play a critical role. Personality traits such as optimism, emotional regulation skills, and a sense of purpose are linked to lower levels of psychological distress, even in high-stress environments[113-115]. Access to mental health resources, including teletherapy and crisis hotlines, provides critical lifelines for those in need, although disparities in access remain a persistent issue[116,117]. Interestingly, some studies suggest that prior exposure to adversity (e.g., natural disasters, economic recessions) may confer psychological resilience in certain populations, enabling them to navigate pandemic-related stressors more effectively[10,118-120].
At the biological level, chronic stress from the pandemic likely dysregulated hypothalamic-pituitary-adrenal axis function, contributing to increased cortisol levels and inflammatory responses linked to mood disorders[121-123]. Emerging evidence highlights that SARS-CoV-2 infection triggers neuroinflammatory cascades, including microglial activation, blood-brain barrier disruption, and elevated pro-inflammatory cytokines (e.g., interleukin-6, tumor necrosis factor-α), which correlate with persistent depression, anxiety, and cognitive dysfunction in long COVID patients[59,84,102]. Notably, recent studies identify biomarkers such as glial fibrillary acidic protein and neurofilament light chain as predictors of neuropsychiatric sequelae, suggesting axonal injury and astrocyte activation as underlying mechanisms[84,85,103].
Furthermore, viral persistence in neural tissues and mitochondrial dysfunction may exacerbate oxidative stress, while autoantibodies targeting neural antigens [e.g., anti-N-methyl-D-aspartic acid (NMDA) receptors] could contribute to psychiatric symptoms independently of infection severity[59,104]. These findings underscore the need for targeted immunomodulatory therapies (e.g., interleukin-6 inhibitors, NMDA antagonists) and neuroprotective strategies in post-COVID mental health care, which is a paradigm shift from traditional monoamine-based treatments. Psychosocially, the erosion of daily structure and loss of meaningful activities (e.g., work, social gatherings) undermined a sense of control, a known protective factor against anxiety[124-126]. Sleep disturbances, which are prevalent during lockdowns, further disrupt neurobiological processes, exacerbating emotional instability[60,123]. Psychosocially, the erosion of daily structure and loss of meaningful activities (e.g., work, social gatherings) undermined a sense of control, a known protective factor against anxiety[124-126].
Identifying these drivers and moderators is not merely an academic exercise. This study has direct implications for mental health strategies. Interventions must account for the diverse pathways through which COVID-19 has affected psychological well-being, from economic policies that reduce financial strain to community-based programs that strengthen social ties[124,127]. Future research should prioritize longitudinal studies to track how these factors interact over time, particularly in understudied populations such as children, refugees, and rural communities[52,128-130]. By dissecting these mechanisms, we move closer to a nuanced understanding of post-pandemic mental health that recognizes both the vulnerabilities exposed by COVID-19 and the resilience that persists despite it.
The COVID-19 pandemic has exposed and exacerbated systemic weaknesses in global mental health care systems, creating formidable barriers to effective intervention[131,132]. Despite growing recognition of the psychological crisis, multiple intersecting challenges continue to hinder adequate response efforts, leaving large populations without necessary support[105,106]. While mental health systems faced significant challenges before the pandemic, COVID-19 served as both a stress test and a catalyst for transformation. This section examines how these systemic issues have evolved in the post-pandemic era, highlighting both deteriorations and innovations across. These obstacles range from structural deficiencies in healthcare delivery to deeply rooted societal attitudes that perpetuate stigma[131,132]. The pandemic’s legacy includes both deepened vulnerabilities and unexpected opportunities for reform. Sustaining positive changes while addressing new inequities (e.g., digital divides) represents the central challenge for post-pandemic mental health systems.
Mental health services worldwide were ill-prepared to handle the surge in demand caused by the pandemic. Many countries, particularly LMICs, entered a crisis with preexisting shortages of mental health professionals a gap that became critically apparent as needs escalated[73,81]. The World Health Organization estimates that nearly 75% of people with mental disorders in these regions receive no treatment whatsoever[133,134]. Even in high-income countries with relatively robust systems, psychiatric services struggle with overwhelmed capacities, resulting in prolonged wait times and rushed consultations[75,80]. The pandemic further disrupted care continuity as facilities repurposed resources for the COVID-19 response, inadvertently deprioritizing mental health needs[75,131,135]. This systemic fragmentation is particularly detrimental for vulnerable groups requiring specialized care, such as trauma survivors or individuals with severe mental illnesses[128,136-138]. In addition, the diversion of resources to acute COVID-19 care significantly worsened existing fragmentation. In LMICs, 68% of community mental health programs experienced budget cuts or closures[131], while high-income countries saw 30% longer wait times due to staff redeployment[135]. The pandemic also created new forms of fragmentation, with “long COVID” clinics often operating separately from mental health services despite overlapping patient needs[139].
Despite decades of anti-stigma campaigns, negative attitudes toward mental illness remain deeply entrenched in many societies[140]. Cultural narratives framing psychological distress as personal weakness rather than legitimate health concerns continue to deter help-seeking behaviors[141-143]. In collectivist cultures, where mental health issues may be viewed as family shame, individuals often avoid professional treatment to prevent social ostracization[144-146]. The workplace presents another arena of stigma, with employees fearing career repercussions for disclosing mental health struggles[79,147-149]. These barriers are compounded by generational divides: Older populations frequently exhibit lower mental health literacy and greater reluctance to engage with psychological services than younger, more psychiatrically aware demographics do[11,52,65,68].
While telehealth emerged as a crucial alternative during lockdowns, its implementation revealed significant digital divides[150,151]. Elderly patients, low-income individuals, and rural communities often lack reliable internet access or technological literacy to benefit from virtual care[150,152,153]. Privacy concerns in crowded living situations further limit the effectiveness of teletherapy for many people[116,154]. Paradoxically, the same digital solutions meant to improve access created new barriers for already marginalized groups[152]. Additionally, the rapid shift to remote care occurred without established protocols for quality control, raising questions about treatment efficacy and patient safety in unsupervised settings[116,153].
The mental health care workforce itself became a casualty of the pandemic[21,79]. Clinicians reported unprecedented levels of exhaustion as they confronted both professional demands and personal pandemic stresses[18,21,23,56,79,147]. Frontline mental health workers faced unprecedented burnout, with 45% considering career changes after the COVID-19 pandemic[146]. This burnout phenomenon has led to early retirements and career changes among mental health professionals, further straining systems already operating with insufficient staffing[132]. The problem is particularly acute in child psychiatry and geriatric mental health, where specialist shortages were severe even before the pandemic[155-157]. Training pipelines for new professionals remain inadequate to meet growing needs, suggesting that this crisis will persist for years without substantial investment in education and recruitment[158-160].
Significant disparities exist between research knowledge and real-world applications. While studies have identified numerous evidence-based interventions, few have been adapted for diverse cultural contexts or scaled effectively[124,148,161-163]. The use of implementation science in the study of how to translate research into practice remains underfunded and undervalued[164-166]. Furthermore, most mental health research continues to focus on Western, educated, industrialized, rich, and democratic populations, limiting the generalizability of findings to global majority communities[28,62,167,168]. This research bias perpetuates a cycle where interventions developed for specific cultural contexts are applied inappropriately to dissimilar populations with poor results[169-171].
Mental health funding consistently lags behind physical health investments, with many governments allocating less than 2% of their health budgets to psychiatric care[160,172-174]. The economic aftermath of the pandemic has intensified fiscal pressures, making new mental health initiatives politically challenging to justify[53]. Insurance coverage limitations create additional financial barriers for patients, particularly for long-term therapy or innovative treatments not yet included in standard formularies[175,176]. At the policy level, mental health is frequently siloed from broader public health planning, resulting in disjointed responses that fail to address social determinants of psychological wellbeing[160,172].
These challenges, while daunting, are not insurmountable. Addressing them requires coordinated action across multiple sectors, from healthcare redesign and workforce expansion to anti-stigma education and policy reform[82,131,132]. The next section outlines concrete research priorities and intervention strategies that can help overcome these barriers, emphasizing innovative approaches that leverage lessons from the pandemic experience[6,26]. Only by confronting these systemic obstacles can societies hope to mitigate the long-term psychological consequences of COVID-19 effectively[177,178].
The post-pandemic mental health landscape demands a reconceptualization of research paradigms and intervention strategies to address persistent gaps in knowledge and service delivery. While the challenges outlined in the previous sections are substantial, they also present opportunities for innovation and systemic improvement. This section prioritizes research directions based on empirical evidence of post-COVID-19 intervention outcomes. We evaluate feasibility and effectiveness across settings, with particular attention to disparities between high-income countries and LMICs.
The long-term psychological consequences of COVID-19 remain poorly understood, particularly for high-risk groups such as survivors of severe infection, frontline workers, and bereaved individuals[6,84,179]. Prospective cohort studies with extended follow-ups (5-10 years) must integrate policy-relevant endpoints (e.g., healthcare utilization costs, return-to-work outcomes) to inform national mental health budgeting and disability insurance frameworks[20,180,181]. Special attention should be given to delayed-onset disorders, which may emerge years after initial trauma exposure[182,183]. Additionally, research must investigate the interplay between long COVID-19 and mental health, including potential neurobiological mechanisms linking persistent physical symptoms to cognitive and emotional dysfunction[85,139].
Current evidence-based treatments often fail to account for cultural variations in symptom expression, help-seeking behaviors, and treatment preferences[184,185]. There is an urgent need for implementation research that tests the effectiveness of Western-developed psychotherapies [e.g., cognitive behavioral therapy (CBT)] when adapted for diverse cultural contexts, particularly in low-resource settings where mental health infrastructure is limited[186-188]. Community-based participatory research methods should be prioritized to codesign interventions with local populations, ensuring their relevance and acceptability[87,189,190]. Furthermore, studies must evaluate task-shifting approaches that train nonspecialists (e.g., community health workers, religious leaders) to deliver basic mental health care in regions with psychiatrist shortages[168,191-193]. Culturally adapted CBT shows promising but heterogeneous effects across settings: Meta-analyses report pooled effect sizes of 0.52 (95%CI: 0.34-0.70) for depression in high-income countries[186] vs 0.29 (0.12-0.46) in LMICs[188], with grading of recommendations, assessment, development and evaluation (GRADE) confidence ratings downgraded to “low” for LMICs due to task-shifting challenges and fidelity concerns. Key barriers include stigma[185] and underfunded training pipelines[193], highlighting the need for contextual adaptation frameworks.
The pandemic starkly revealed disparities in mental health care capacity between LMICs and high-income countries, demanding tailored research priorities[73]. In LMICs, task-shifting emerged as a critical strategy, with community health workers delivering 80% of mental health services in Kenya[188], though sustainability remains challenged by unpaid labor[193]. Low-tech solutions like short message services (SMS) interventions achieved 60% adherence in India[193], outperforming app-based tools that faced 40% attrition due to digital divides[152]. Structural barriers persist, however, with only 12% of LMICs increasing mental health funding post-pandemic vs 52% of high-income countries[172], exacerbating pre-existing inequities. Recent LMIC adaptations demonstrate promise: Kenya’s peer-delivered CBT achieved 60% remission in depression (vs 35% in standard care) via community health workers[188], while Guatemala’s radio-based counseling reduced anxiety symptoms by 45% in indigenous populations[194]. However, sustainability remains challenged by funding shortages[172]. Culturally adapted, non-stigmatizing platforms, such as radio-based counseling in rural Guatemala[194], showed particular promise, suggesting that LMIC-focused research must prioritize context over technology transfer.
The COVID-19 pandemic has significantly accelerated the adoption of digital mental health interventions, yet several critical issues regarding their implementation and impact remain unresolved[195,196]. While these technological solutions have demonstrated potential in expanding access to care, rigorous research is still needed to comprehensively evaluate their efficacy compared with traditional face-to-face therapies across different psychiatric conditions[197-200]. The pandemic also accelerated preexisting trends, such as digital reliance on mental health care. While teletherapy improved accessibility for some, it also highlighted disparities in technological literacy and internet access, particularly among older and low-income populations[116,150,152,153]. These findings underscore the need for interventions that address both individual vulnerabilities and systemic inequities. Particular attention should be given to developing AI-based screening tools with appropriate safeguards against inherent algorithmic biases, as well as investigating optimal strategies to enhance patient engagement and retention in digital therapeutic platforms[198,201,202]. Furthermore, the widening digital divide poses substantial challenges to equitable implementation, potentially exacerbating existing mental health disparities among socioeconomically disadvantaged populations[53,195,196,203].
While digital tools (e.g., chatbots, teletherapy) improved accessibility during the pandemic, disparities persist across socioeconomic and geographic lines. It reported that chatbots reduced depression symptoms by 22% in high-income countries[198], but LMIC trials showed 40% attrition due to low digital literacy[125]. However, AI-based risk algorithms also exhibited racial bias[204], limiting scalability. Recent meta-analyses of digital mental health interventions[196,198] demonstrate moderate efficacy for reducing depression (SMD = -0.45, 95%CI: -0.62 to -0.28) and anxiety (SMD = -0.38) during the pandemic, though effect sizes vary by platform type (chatbots > self-help apps). GRADE assessments indicate moderate-quality evidence for CBT-based tools but low quality for AI-driven solutions due to high attrition rates (40% in LMICs) and algorithmic bias[204]. Scalability remains limited by digital literacy gaps, particularly among older and rural populations[152]. In addition, cultural barriers compound these issues: Western-developed apps often lack linguistic adaptation or fail to address local stigma (e.g., somatic symptom presentation in Asian cultures)[185,194]. Conversely, low-tech solutions (e.g., SMS-based counseling in India, radio programs in Guatemala) show higher adherence (60%-80%) by aligning with existing infrastructure[193,194]. To advance equity, we urge co-designing tools with LMIC stakeholders, subsidizing internet/data costs, and tiered interventions (e.g., hybrid SMS/clinic models). Policymakers must treat digital access as a mental health determinant.
In summary, these technological advancements must be accompanied by parallel developments in ethical frameworks to ensure robust protection for patient confidentiality, appropriate informed consent procedures, and equitable distribution of these innovative mental healthcare solutions[203-207]. In addition, digital tools require tiered implementation as high-resource settings can validate AI chatbots, while LMICs prioritize low-tech hybrids (SMS + community hubs) to bypass internet barriers. Policy action should mandate that mental health apps meet World Health Organization’s digital adaptation kits for cultural/Linguistic adaptation[195].
Reactive approaches to mental health care are insufficient to address the post-pandemic burden[208,209]. Research must identify modifiable risk factors (e.g., childhood adversity, social determinants) that can be targeted through population-level prevention strategies[6,210-212]. School-based programs must embed mental health literacy into core curricula[213], while workplaces adopt “mental health leave” policies tied to screening[214]. Cost-effectiveness analyses should compare universal prevention vs high-risk targeting[67,213,215,216]. Additionally, biomarker research (e.g., investigations of inflammatory markers and epigenetic changes) may enable early identification of high-risk individuals before clinical symptoms emerge[217-220].
The COVID-19 pandemic has revealed fundamental deficiencies in mental health service delivery systems worldwide, necessitating comprehensive health system research to develop effective solutions[135,221]. Key areas requiring investigation include determining optimal models for integrating mental health services into primary care settings, establishing sustainable financing mechanisms for long-term program viability, and developing workforce expansion strategies that address both training pipelines and retention incentives[222-226]. Additionally, rigorous policy evaluation studies are needed to assess the effectiveness of mental health parity laws and insurance reforms implemented during the crisis[29,214,227]. Cross-national comparative research represents a particularly valuable approach, as systematic analysis of countries that successfully maintained mental health services throughout the pandemic could yield transferable best practices and innovative care delivery models[29,228,229]. These research initiatives must account for varying healthcare system architectures and resource availability across different national contexts while maintaining a focus on equitable access to quality mental healthcare[29,228-230].
Future studies must move beyond broad demographic categories to investigate how intersecting identities (e.g., race, gender, disability, and socioeconomic status) compound mental health risks[6,10,13,231]. Participatory action research with marginalized communities, including refugees, indigenous populations, and lesbian, gay, bisexual, transgender, and queer + individuals, is essential for developing tailored interventions that address unique stressors and resilience factors[86,194,232-236].
The COVID-19 mental health crisis presents both a formidable challenge and a historic opportunity to reimagine mental healthcare delivery[6,53,230,237]. By investing in these research priorities, the global community can build more equitable, evidence-based systems capable of mitigating not only the aftermath of this pandemic but also future crises[26,238,239]. Addressing these priorities will require unprecedented collaboration between researchers, clinicians, policymakers, and community stakeholders[240,241]. International consortia should be established to harmonize measurement tools, share data, and accelerate discovery[242-244]. In addition, funding agencies must prioritize mental health research with the same urgency according to infectious disease and biomedical research during the pandemic’s peak[9,29,227,245].
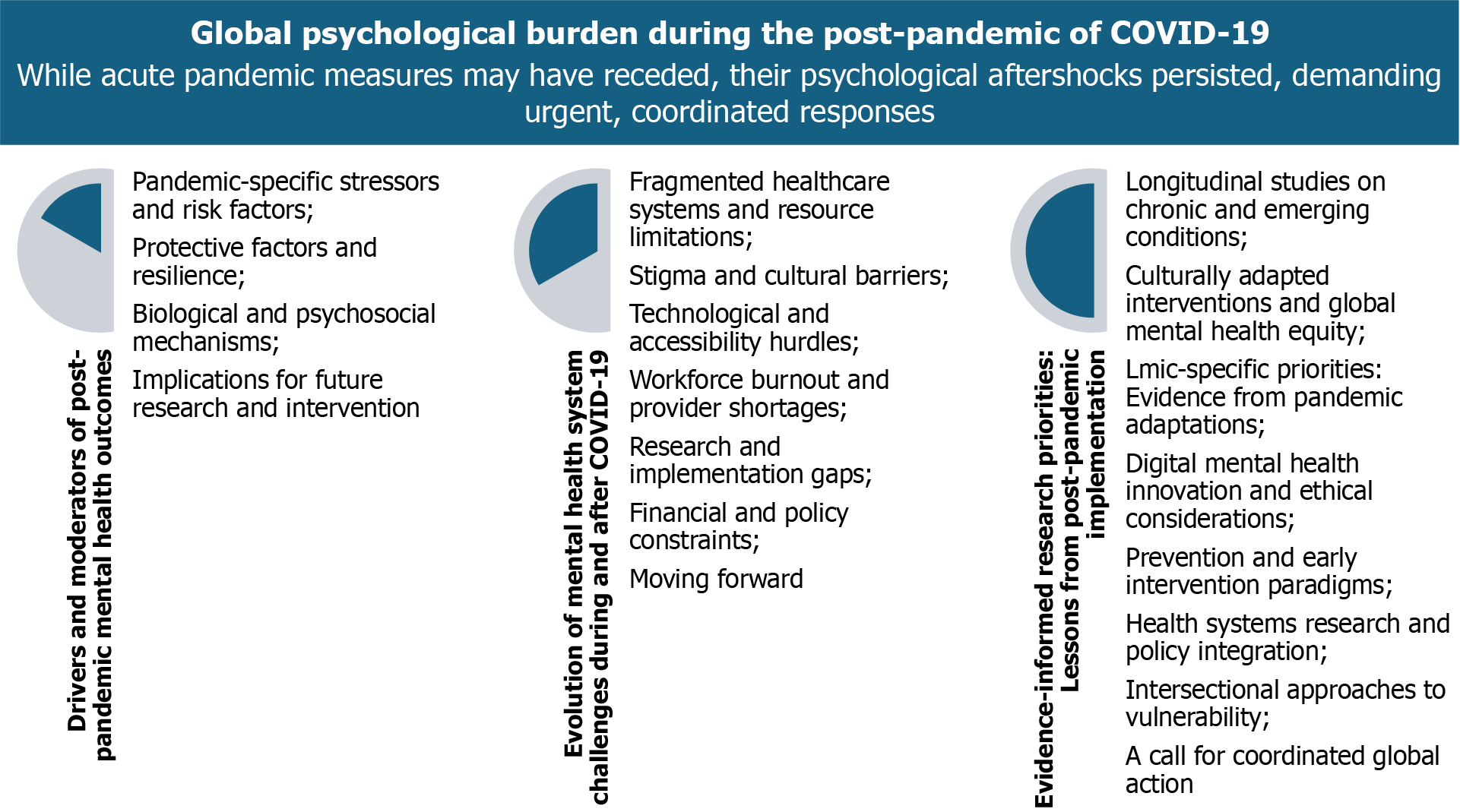
The COVID-19 pandemic has precipitated a lasting global mental health crisis that demands urgent, multifaceted solutions. This review underscores the disproportionate psychological burden borne by vulnerable populations and highlights critical areas for intervention: Integrating mental health into primary care systems, developing culturally adapted treatments, leveraging digital tools while addressing accessibility gaps, and implementing policy reforms to ensure sustainable funding (Figure 1). The pandemic has revealed both the fragility of existing mental healthcare systems and opportunities for transformative change. By synthesizing evidence on chronic outcomes and innovative solutions, this review fills critical gaps between acute-pandemic reports and emerging next-phase challenges, offering a roadmap for research prioritization. Moving forward, we must capitalize on this momentum by adopting evidence-based, equity-focused approaches that not only address current needs but also build resilience against future crises. The scale of this challenge calls for immediate, coordinated action across research, clinical practice, and policymaking to create mental healthcare systems capable of supporting population wellbeing in the post-pandemic era and beyond. To translate these research priorities into practice, we propose a three-tiered action framework: (1) Policy advocacy: Governments and World Health Organization should integrate mental health into pandemic preparedness plans, with dedicated funding for LMIC-specific interventions (e.g., task-shifting programs); (2) Researcher collaboration: Establish an international consortium to harmonize metrics (e.g., standardized long COVID neuropsychiatric assessments) and share datasets via platforms like the Global Mental Health Databank; and (3) Community engagement: Co-design interventions with marginalized groups (e.g., refugees, indigenous communities) using participatory methods. The post-COVID-19 mental health crisis demands a coordinated response, requiring researchers, policymakers, and communities must act now to avert a generational catastrophe.
| 1. | Davis HE, McCorkell L, Vogel JM, Topol EJ. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. 2023;21:133-146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1688] [Cited by in RCA: 2529] [Article Influence: 843.0] [Reference Citation Analysis (0)] |
| 2. | Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA. 2020;324:782-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2691] [Cited by in RCA: 3243] [Article Influence: 540.5] [Reference Citation Analysis (0)] |
| 3. | Ceban F, Ling S, Lui LMW, Lee Y, Gill H, Teopiz KM, Rodrigues NB, Subramaniapillai M, Di Vincenzo JD, Cao B, Lin K, Mansur RB, Ho RC, Rosenblat JD, Miskowiak KW, Vinberg M, Maletic V, McIntyre RS. Fatigue and cognitive impairment in Post-COVID-19 Syndrome: A systematic review and meta-analysis. Brain Behav Immun. 2022;101:93-135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 841] [Cited by in RCA: 983] [Article Influence: 245.8] [Reference Citation Analysis (0)] |
| 4. | Wu CT, Lidsky PV, Xiao Y, Cheng R, Lee IT, Nakayama T, Jiang S, He W, Demeter J, Knight MG, Turn RE, Rojas-Hernandez LS, Ye C, Chiem K, Shon J, Martinez-Sobrido L, Bertozzi CR, Nolan GP, Nayak JV, Milla C, Andino R, Jackson PK. SARS-CoV-2 replication in airway epithelia requires motile cilia and microvillar reprogramming. Cell. 2023;186:112-130.e20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 136] [Article Influence: 45.3] [Reference Citation Analysis (0)] |
| 5. | Moss P. The T cell immune response against SARS-CoV-2. Nat Immunol. 2022;23:186-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 766] [Cited by in RCA: 923] [Article Influence: 230.8] [Reference Citation Analysis (0)] |
| 6. | Penninx BWJH, Benros ME, Klein RS, Vinkers CH. How COVID-19 shaped mental health: from infection to pandemic effects. Nat Med. 2022;28:2027-2037. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 252] [Article Influence: 63.0] [Reference Citation Analysis (1)] |
| 7. | Taylor S. The Psychology of Pandemics. Annu Rev Clin Psychol. 2022;18:581-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 71] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 8. | COVID-19 Excess Mortality Collaborators. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020-21. Lancet. 2022;399:1513-1536. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 430] [Cited by in RCA: 1069] [Article Influence: 267.3] [Reference Citation Analysis (3)] |
| 9. | Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, Ballard C, Christensen H, Cohen Silver R, Everall I, Ford T, John A, Kabir T, King K, Madan I, Michie S, Przybylski AK, Shafran R, Sweeney A, Worthman CM, Yardley L, Cowan K, Cope C, Hotopf M, Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547-560. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3158] [Cited by in RCA: 3300] [Article Influence: 550.0] [Reference Citation Analysis (0)] |
| 10. | Wang S, Zhang Y, Ding W, Meng Y, Hu H, Liu Z, Zeng X, Wang M. Psychological distress and sleep problems when people are under interpersonal isolation during an epidemic: A nationwide multicenter cross-sectional study. Eur Psychiatry. 2020;63:e77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 85] [Article Influence: 14.2] [Reference Citation Analysis (4)] |
| 11. | COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398:1700-1712. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2518] [Cited by in RCA: 3085] [Article Influence: 617.0] [Reference Citation Analysis (0)] |
| 12. | Luo D, Mei B, Wang P, Li X, Chen X, Wei G, Kuang F, Li B, Su S. Prevalence and risk factors for persistent symptoms after COVID-19: a systematic review and meta-analysis. Clin Microbiol Infect. 2024;30:328-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 79] [Article Influence: 39.5] [Reference Citation Analysis (0)] |
| 13. | Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav Immun. 2020;89:531-542. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2189] [Cited by in RCA: 1956] [Article Influence: 326.0] [Reference Citation Analysis (0)] |
| 14. | Cullen W, Gulati G, Kelly BD. Mental health in the COVID-19 pandemic. QJM. 2020;113:311-312. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 508] [Cited by in RCA: 533] [Article Influence: 88.8] [Reference Citation Analysis (0)] |
| 15. | Usher K, Durkin J, Bhullar N. The COVID-19 pandemic and mental health impacts. Int J Ment Health Nurs. 2020;29:315-318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 302] [Cited by in RCA: 316] [Article Influence: 52.7] [Reference Citation Analysis (0)] |
| 16. | McElroy E, Patalay P, Moltrecht B, Shevlin M, Shum A, Creswell C, Waite P. Demographic and health factors associated with pandemic anxiety in the context of COVID-19. Br J Health Psychol. 2020;25:934-944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 98] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 17. | Breslau J, Finucane ML, Locker AR, Baird MD, Roth EA, Collins RL. A longitudinal study of psychological distress in the United States before and during the COVID-19 pandemic. Prev Med. 2021;143:106362. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 100] [Cited by in RCA: 158] [Article Influence: 31.6] [Reference Citation Analysis (0)] |
| 18. | Wang X, Fu F, Gan A, Wu Y, Pan W, Zhou X, Zhang X. Psychological status of healthcare workers in the post-COVID 19 period in China: a retrospective multicentric cross-sectional study. Front Psychiatry. 2025;16:1520361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 19. | Santoro A, Bai F, Greco MF, Rovito R, Sala M, Borghi L, Piscopo K, Vegni E, de Morais Caporali JF, Marinho CC, Leite AS, Santoro MM, Silberstein FC, Iannetta M, Juozapaite D, Strumiliene E, Almeida A, Toscano C, Quinones JAR, Carioti L, Mommo C, Fanti I, Incardona F, Marchetti G; EuCARE POSTCOVID study. Short and long-term trajectories of the post COVID-19 condition: Results from the EuCARE POSTCOVID study. BMC Infect Dis. 2025;25:625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 20. | Bourmistrova NW, Solomon T, Braude P, Strawbridge R, Carter B. Long-term effects of COVID-19 on mental health: A systematic review. J Affect Disord. 2022;299:118-125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 215] [Article Influence: 53.8] [Reference Citation Analysis (0)] |
| 21. | Ding W, Wang MZ, Zeng XW, Liu ZH, Meng Y, Hu HT, Zhang Y, Guan YG, Meng FG, Zhang JG, Wang S. Mental health and insomnia problems in healthcare workers after the COVID-19 pandemic: A multicenter cross-sectional study. World J Psychiatry. 2024;14:704-714. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (1)] |
| 22. | Masters GA, Asipenko E, Bergman AL, Person SD, Brenckle L, Moore Simas TA, Ko JY, Robbins CL, Byatt N. Impact of the COVID-19 pandemic on mental health, access to care, and health disparities in the perinatal period. J Psychiatr Res. 2021;137:126-130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 71] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 23. | Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020;88:901-907. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1812] [Cited by in RCA: 2324] [Article Influence: 387.3] [Reference Citation Analysis (2)] |
| 24. | Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, Wu J, Du H, Chen T, Li R, Tan H, Kang L, Yao L, Huang M, Wang H, Wang G, Liu Z, Hu S. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open. 2020;3:e203976. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5313] [Cited by in RCA: 4449] [Article Influence: 741.5] [Reference Citation Analysis (10)] |
| 25. | Thomeer MB, Moody MD, Yahirun J. Racial and Ethnic Disparities in Mental Health and Mental Health Care During The COVID-19 Pandemic. J Racial Ethn Health Disparities. 2023;10:961-976. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 179] [Article Influence: 59.7] [Reference Citation Analysis (0)] |
| 26. | Moreno C, Wykes T, Galderisi S, Nordentoft M, Crossley N, Jones N, Cannon M, Correll CU, Byrne L, Carr S, Chen EYH, Gorwood P, Johnson S, Kärkkäinen H, Krystal JH, Lee J, Lieberman J, López-Jaramillo C, Männikkö M, Phillips MR, Uchida H, Vieta E, Vita A, Arango C. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7:813-824. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1107] [Cited by in RCA: 987] [Article Influence: 164.5] [Reference Citation Analysis (0)] |
| 27. | Loeb TB, Ebor MT, Smith-Clapham AM, Chin D, Novacek DM, Hampton-Anderson JN, Norwood-Scott E, Hamilton AB, Brown AF, Wyatt GE. How Mental Health Professionals Can Address Disparities in the Context of the COVID-19 Pandemic. Traumatology (Tallahass Fla). 2021;27:60-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 28. | Kelly MP, Brayne C, Kinmonth AL, Kriznik N, Ford J, Fletcher PC. Inequalities in mental health: predictive processing and social life. Curr Opin Psychiatry. 2021;34:171-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 29. | Aknin LB, Andretti B, Goldszmidt R, Helliwell JF, Petherick A, De Neve JE, Dunn EW, Fancourt D, Goldberg E, Jones SP, Karadag O, Karam E, Layard R, Saxena S, Thornton E, Whillans A, Zaki J. Policy stringency and mental health during the COVID-19 pandemic: a longitudinal analysis of data from 15 countries. Lancet Public Health. 2022;7:e417-e426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 140] [Article Influence: 35.0] [Reference Citation Analysis (0)] |
| 30. | Hossain MM, Tasnim S, Sultana A, Faizah F, Mazumder H, Zou L, McKyer ELJ, Ahmed HU, Ma P. Epidemiology of mental health problems in COVID-19: a review. F1000Res. 2020;9:636. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 536] [Cited by in RCA: 590] [Article Influence: 98.3] [Reference Citation Analysis (0)] |
| 31. | Dong L, Bouey J. Public Mental Health Crisis during COVID-19 Pandemic, China. Emerg Infect Dis. 2020;26:1616-1618. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 289] [Cited by in RCA: 359] [Article Influence: 59.8] [Reference Citation Analysis (0)] |
| 32. | GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403:2133-2161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2282] [Cited by in RCA: 2750] [Article Influence: 1375.0] [Reference Citation Analysis (0)] |
| 33. | The Lancet Psychiatry. Global Burden of Disease 2021: mental health messages. Lancet Psychiatry. 2024;11:573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 38] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 34. | Wang S, Zhang Y, Guan Y, Ding W, Meng Y, Hu H, Liu Z, Zeng X, Wang M. A nationwide evaluation of the prevalence of and risk factors associated with anxiety, depression and insomnia symptoms during the return-to-work period of coronavirus disease 2019 in China. Soc Psychiatry Psychiatr Epidemiol. 2021;56:2275-2286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 35. | Deng J, Zhou F, Hou W, Silver Z, Wong CY, Chang O, Huang E, Zuo QK. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann N Y Acad Sci. 2021;1486:90-111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 402] [Cited by in RCA: 473] [Article Influence: 94.6] [Reference Citation Analysis (0)] |
| 36. | Wang S, Quan L, Chavarro JE, Slopen N, Kubzansky LD, Koenen KC, Kang JH, Weisskopf MG, Branch-Elliman W, Roberts AL. Associations of Depression, Anxiety, Worry, Perceived Stress, and Loneliness Prior to Infection With Risk of Post-COVID-19 Conditions. JAMA Psychiatry. 2022;79:1081-1091. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 108] [Cited by in RCA: 242] [Article Influence: 60.5] [Reference Citation Analysis (0)] |
| 37. | Mohammad PJ, Hama Amin DS, Mohammed PF, Hussein HA, Abdullah OS. PTSS in COVID-19 survivors peritraumatic stress symptoms among COVID-19 survivors in Iraq. Curr Psychol. 2023;1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 38. | Izudi J, Nasuuna EM, Appeli S, Bajunirwe F. Effect of COVID-19 pandemic on smoking, alcohol consumption, and substance use in persons aged 15 years and older in Uganda. Sci Rep. 2025;15:14817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 39. | Beygui NC, Duross E, Cheng CI, Mesaros K, Gawronski K, Perzhinsky J. The Effect of the COVID-19 Pandemic on Prescribing Medications for Opioid Use Disorder in the Mid-Michigan Region. J Prim Care Community Health. 2025;16:21501319251331322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 40. | Martínez-Garcia M, Sansano-Sansano E, Castillo-Hornero A, Femenia R, Roomp K, Oliver N. Social isolation during the COVID-19 pandemic in Spain: a population study. Sci Rep. 2022;12:12543. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 41. | Zawilska JB, Kuczyńska K. Psychiatric and neurological complications of long COVID. J Psychiatr Res. 2022;156:349-360. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 94] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 42. | Tarsitani L, Vassalini P, Koukopoulos A, Borrazzo C, Alessi F, Di Nicolantonio C, Serra R, Alessandri F, Ceccarelli G, Mastroianni CM, d'Ettorre G. Post-traumatic Stress Disorder Among COVID-19 Survivors at 3-Month Follow-up After Hospital Discharge. J Gen Intern Med. 2021;36:1702-1707. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 91] [Cited by in RCA: 96] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 43. | Sagherian K, Steege LM, Cobb SJ, Cho H. Insomnia, fatigue and psychosocial well-being during COVID-19 pandemic: A cross-sectional survey of hospital nursing staff in the United States. J Clin Nurs. 2023;32:5382-5395. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 139] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 44. | Gong K, Garneau J, Grenier S, Vasiliadis HM, Dang-Vu TT, Dialahy IZ, Gouin JP. Insomnia symptoms among older adults during the first year of the COVID-19 pandemic: A longitudinal study. Sleep Health. 2023;9:560-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 45. | Sagherian K, Cho H, Steege LM. The insomnia, fatigue, and psychological well-being of hospital nurses 18 months after the COVID-19 pandemic began: A cross-sectional study. J Clin Nurs. 2024;33:273-287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 28] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 46. | Aldalaykeh M, Al-Hammouri MM, Rababah J, Al-Dwaikat T. COVID-19 Help-Seeking Behaviors: Application of the Theory of Planned Behavior. Psychol Belg. 2021;61:391-400. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 47. | Yonemoto N, Kawashima Y. Help-seeking behaviors for mental health problems during the COVID-19 pandemic: A systematic review. J Affect Disord. 2023;323:85-100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 41] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 48. | Guenthner L, Baldofski S, Kohls E, Schuhr J, Brock T, Rummel-Kluge C. Differences in Help-Seeking Behavior among University Students during the COVID-19 Pandemic Depending on Mental Health Status: Results from a Cross-Sectional Survey. Behav Sci (Basel). 2023;13:885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 49. | Evans RA, McAuley H, Harrison EM, Shikotra A, Singapuri A, Sereno M, Elneima O, Docherty AB, Lone NI, Leavy OC, Daines L, Baillie JK, Brown JS, Chalder T, De Soyza A, Diar Bakerly N, Easom N, Geddes JR, Greening NJ, Hart N, Heaney LG, Heller S, Howard L, Hurst JR, Jacob J, Jenkins RG, Jolley C, Kerr S, Kon OM, Lewis K, Lord JM, McCann GP, Neubauer S, Openshaw PJM, Parekh D, Pfeffer P, Rahman NM, Raman B, Richardson M, Rowland M, Semple MG, Shah AM, Singh SJ, Sheikh A, Thomas D, Toshner M, Chalmers JD, Ho LP, Horsley A, Marks M, Poinasamy K, Wain LV, Brightling CE; PHOSP-COVID Collaborative Group. Physical, cognitive, and mental health impacts of COVID-19 after hospitalisation (PHOSP-COVID): a UK multicentre, prospective cohort study. Lancet Respir Med. 2021;9:1275-1287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 382] [Cited by in RCA: 436] [Article Influence: 87.2] [Reference Citation Analysis (0)] |
| 50. | Borrescio-Higa F, Droller F, Valenzuela P. Financial Distress and Psychological Well-Being During the COVID-19 Pandemic. Int J Public Health. 2022;67:1604591. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 51. | Wu T, Jia X, Shi H, Niu J, Yin X, Xie J, Wang X. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J Affect Disord. 2021;281:91-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 812] [Cited by in RCA: 751] [Article Influence: 150.2] [Reference Citation Analysis (0)] |
| 52. | Patel K, Robertson E, Kwong ASF, Griffith GJ, Willan K, Green MJ, Di Gessa G, Huggins CF, McElroy E, Thompson EJ, Maddock J, Niedzwiedz CL, Henderson M, Richards M, Steptoe A, Ploubidis GB, Moltrecht B, Booth C, Fitzsimons E, Silverwood R, Patalay P, Porteous D, Katikireddi SV. Psychological Distress Before and During the COVID-19 Pandemic Among Adults in the United Kingdom Based on Coordinated Analyses of 11 Longitudinal Studies. JAMA Netw Open. 2022;5:e227629. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 129] [Cited by in RCA: 137] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 53. | Kim S, Hwang J, Lee JH, Park J, Kim HJ, Son Y, Oh H, Smith L, Kang J, Fond G, Boyer L, Rahmati M, Tully MA, Pizzol D, Udeh R, Lee J, Lee H, Lee S, Yon DK. Psychosocial alterations during the COVID-19 pandemic and the global burden of anxiety and major depressive disorders in adolescents, 1990-2021: challenges in mental health amid socioeconomic disparities. World J Pediatr. 2024;20:1003-1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 37] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 54. | Oliveira JMD, Butini L, Pauletto P, Lehmkuhl KM, Stefani CM, Bolan M, Guerra E, Dick B, De Luca Canto G, Massignan C. Mental health effects prevalence in children and adolescents during the COVID-19 pandemic: A systematic review. Worldviews Evid Based Nurs. 2022;19:130-137. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 80] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 55. | Reutter M, Hutterer K, Gründahl M, Gall D, Dannlowski U, Domschke K, Leehr EJ, Lonsdorf TB, Lueken U, Reif A, Schiele MA, Zwanzger P, Pauli P, Hein G, Gamer M. Mental health improvement after the COVID-19 pandemic in individuals with psychological distress. Sci Rep. 2024;14:5685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 56. | Zahiriharsini A, Gilbert-Ouimet M, Langlois L, Biron C, Pelletier J, Beaulieu M, Truchon M. Associations between psychosocial stressors at work and moral injury in frontline healthcare workers and leaders facing the COVID-19 pandemic in Quebec, Canada: A cross-sectional study. J Psychiatr Res. 2022;155:269-278. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 57. | AlJaberi M, Elshatarat RA, Sawalha MA, Al Hmaimat N, AlBlooshi H, Alshehhi M, Ibrahim AM, Zaghamir DE, Saleh ZT, Saifan AR. The psychological impact of COVID-19 on front-line healthcare providers in the United Arab Emirates: A cross-sectional study. J Educ Health Promot. 2024;13:335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 58. | Jafri MR, Zaheer A, Fatima S, Saleem T, Sohail A. Mental health status of COVID-19 survivors: a cross sectional study. Virol J. 2022;19:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 59. | Monje M, Iwasaki A. The neurobiology of long COVID. Neuron. 2022;110:3484-3496. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 287] [Article Influence: 71.8] [Reference Citation Analysis (0)] |
| 60. | Mazza MG, De Lorenzo R, Conte C, Poletti S, Vai B, Bollettini I, Melloni EMT, Furlan R, Ciceri F, Rovere-Querini P; COVID-19 BioB Outpatient Clinic Study group, Benedetti F. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav Immun. 2020;89:594-600. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 967] [Cited by in RCA: 1062] [Article Influence: 177.0] [Reference Citation Analysis (0)] |
| 61. | van der Feltz-Cornelis C, Turk F, Sweetman J, Khunti K, Gabbay M, Shepherd J, Montgomery H, Strain WD, Lip GYH, Wootton D, Watkins CL, Cuthbertson DJ, Williams N, Banerjee A. Prevalence of mental health conditions and brain fog in people with long COVID: A systematic review and meta-analysis. Gen Hosp Psychiatry. 2024;88:10-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 62. | Bambra C, Riordan R, Ford J, Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health. 2020;74:964-968. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 395] [Cited by in RCA: 778] [Article Influence: 129.7] [Reference Citation Analysis (0)] |
| 63. | Yuan J, Dong M, Wong IOL, Cowing BJ, Lam WWT, Ni MY, Liao Q. Can psychological distress account for the associations between COVID-19 vaccination acceptance and socio-economic vulnerability? Appl Psychol Health Well Being. 2023;15:1583-1602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 64. | Robinson E, Sutin AR, Daly M, Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J Affect Disord. 2022;296:567-576. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 673] [Cited by in RCA: 678] [Article Influence: 169.5] [Reference Citation Analysis (0)] |
| 65. | Kunzler AM, Röthke N, Günthner L, Stoffers-Winterling J, Tüscher O, Coenen M, Rehfuess E, Schwarzer G, Binder H, Schmucker C, Meerpohl JJ, Lieb K. Mental burden and its risk and protective factors during the early phase of the SARS-CoV-2 pandemic: systematic review and meta-analyses. Global Health. 2021;17:34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 155] [Cited by in RCA: 149] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 66. | Panchal U, Salazar de Pablo G, Franco M, Moreno C, Parellada M, Arango C, Fusar-Poli P. The impact of COVID-19 lockdown on child and adolescent mental health: systematic review. Eur Child Adolesc Psychiatry. 2023;32:1151-1177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 432] [Cited by in RCA: 471] [Article Influence: 157.0] [Reference Citation Analysis (0)] |
| 67. | Marraccini ME, Griffard MKR, Whitcomb CE, Wood C, Griffin DC, Pittleman C, Sartain L. School-based Mental Health Supports During COVID-19: School Professional Perspectives. Psychol Sch. 2023;60:2460-2482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 68. | Racine N, McArthur BA, Cooke JE, Eirich R, Zhu J, Madigan S. Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19: A Meta-analysis. JAMA Pediatr. 2021;175:1142-1150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1353] [Cited by in RCA: 1537] [Article Influence: 307.4] [Reference Citation Analysis (0)] |
| 69. | Farooq S, Tunmore J, Wajid Ali M, Ayub M. Suicide, self-harm and suicidal ideation during COVID-19: A systematic review. Psychiatry Res. 2021;306:114228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 122] [Cited by in RCA: 226] [Article Influence: 45.2] [Reference Citation Analysis (0)] |
| 70. | Dobrin-De Grace R, Carvalho D, Courtney DB, Aitken M. Suicidal behaviour and ideation among adolescents during the COVID-19 pandemic. Curr Opin Psychol. 2023;52:101650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 71. | Zhu Y, Li Y, Xu X. Suicidal ideation and suicide attempts in psychiatric patients during the COVID-19: A systematic review and meta-analysis. Psychiatry Res. 2022;317:114837. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 72. | García-Iglesias JJ, Gómez-Salgado J, Fernández-Carrasco FJ, Rodríguez-Díaz L, Vázquez-Lara JM, Prieto-Callejero B, Allande-Cussó R. Suicidal ideation and suicide attempts in healthcare professionals during the COVID-19 pandemic: A systematic review. Front Public Health. 2022;10:1043216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 23] [Reference Citation Analysis (0)] |
| 73. | Aksunger N, Vernot C, Littman R, Voors M, Meriggi NF, Abajobir A, Beber B, Dai K, Egger D, Islam A, Kelly J, Kharel A, Matabaro A, Moya A, Mwachofi P, Nekesa C, Ochieng E, Rahman T, Scacco A, van Dalen Y, Walker M, Janssens W, Mobarak AM. COVID-19 and mental health in 8 low- and middle-income countries: A prospective cohort study. PLoS Med. 2023;20:e1004081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 74. | Hall LR, Sanchez K, da Graca B, Bennett MM, Powers M, Warren AM. Income Differences and COVID-19: Impact on Daily Life and Mental Health. Popul Health Manag. 2022;25:384-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 75. | Stepanova E, Thompson A, Yu G, Fu Y. Changes in mental health services in response to the COVID-19 pandemic in high-income countries: a rapid review. BMC Psychiatry. 2024;24:103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 19] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 76. | Passavanti M, Argentieri A, Barbieri DM, Lou B, Wijayaratna K, Foroutan Mirhosseini AS, Wang F, Naseri S, Qamhia I, Tangerås M, Pelliciari M, Ho CH. The psychological impact of COVID-19 and restrictive measures in the world. J Affect Disord. 2021;283:36-51. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 91] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 77. | Marchi M, Magarini FM, Chiarenza A, Galeazzi GM, Paloma V, Garrido R, Ioannidi E, Vassilikou K, de Matos MG, Gaspar T, Guedes FB, Primdahl NL, Skovdal M, Murphy R, Durbeej N, Osman F, Watters C, van den Muijsenbergh M, Sturm G, Oulahal R, Padilla B, Willems S, Spiritus-Beerden E, Verelst A, Derluyn I. Experience of discrimination during COVID-19 pandemic: the impact of public health measures and psychological distress among refugees and other migrants in Europe. BMC Public Health. 2022;22:942. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 78. | Kendrick K, Isaac M. Overview of behavioural and psychological consequences of COVID 19. Curr Opin Psychiatry. 2021;34:477-484. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 79. | Moro MF, Calamandrei G, Poli R, Di Mattei V, Perra A, Kurotschka PK, Restrepo A, Romano F, La Torre G, Preti E, Mascayano F, Picardi A, Chiarotti F, Rapisarda V, Urban A, Alvarado R, Susser E, Carta MG. The Impact of the COVID-19 Pandemic on the Mental Health of Healthcare Workers in Italy: Analyzing the Role of Individual and Workplace-Level Factors in the Reopening Phase After Lockdown. Front Psychiatry. 2022;13:867080. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 80. | Gutwinski S, Schreiter S, Deutscher K, Fazel S. The prevalence of mental disorders among homeless people in high-income countries: An updated systematic review and meta-regression analysis. PLoS Med. 2021;18:e1003750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 160] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 81. | Kola L, Kohrt BA, Hanlon C, Naslund JA, Sikander S, Balaji M, Benjet C, Cheung EYL, Eaton J, Gonsalves P, Hailemariam M, Luitel NP, Machado DB, Misganaw E, Omigbodun O, Roberts T, Salisbury TT, Shidhaye R, Sunkel C, Ugo V, van Rensburg AJ, Gureje O, Pathare S, Saxena S, Thornicroft G, Patel V. COVID-19 mental health impact and responses in low-income and middle-income countries: reimagining global mental health. Lancet Psychiatry. 2021;8:535-550. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 476] [Cited by in RCA: 446] [Article Influence: 89.2] [Reference Citation Analysis (0)] |
| 82. | Zhou M. COVID-19-related stigma and its impact on psychological distress: A cross-sectional study in Wuhan, China. Health Sci Rep. 2022;5:e758. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 83. | Fujii K, Hashimoto H. Socio-psychological factors associated with anticipated stigma toward COVID-19: a cross-sectional study in Japan. BMC Public Health. 2023;23:1245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 84. | Li Z, He J, Wang Y, Bai M, Zhang Y, Chen H, Li W, Cai Y, Chen S, Qu M, Wang J. A cross-sectional study on the mental health of patients with COVID-19 1 year after discharge in Huanggang, China. Eur Arch Psychiatry Clin Neurosci. 2023;273:301-310. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 85. | Rahmati M, Udeh R, Yon DK, Lee SW, Dolja-Gore X, McEVoy M, Kenna T, Jacob L, López Sánchez GF, Koyanagi A, Shin JI, Smith L. A systematic review and meta-analysis of long-term sequelae of COVID-19 2-year after SARS-CoV-2 infection: A call to action for neurological, physical, and psychological sciences. J Med Virol. 2023;95:e28852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 77] [Reference Citation Analysis (0)] |
| 86. | Jumaa JA, Bendau A, Ströhle A, Heinz A, Betzler F, Petzold MB. Psychological distress and anxiety in Arab refugees and migrants during the COVID-19 pandemic in Germany. Transcult Psychiatry. 2023;60:62-73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 87. | Saha I, Majumder J, Bagepally BS, Ray S, Saha A, Chakrabarti A. Burden of mental health disorders and synthesis of community-based mental health intervention measures among adolescents during COVID-19 pandemic in low middle-income countries: A systematic review and meta-analysis. Asian J Psychiatr. 2023;89:103790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 88. | Liu X, Li X, Sun T, Qin H, Zhou Y, Zou C, Cao J, Zhang H. East-West differences in clinical manifestations of COVID-19 patients: A systematic literature review and meta-analysis. J Med Virol. 2021;93:2683-2693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 89. | Banerjee D, Viswanath B. Neuropsychiatric manifestations of COVID-19 and possible pathogenic mechanisms: Insights from other coronaviruses. Asian J Psychiatr. 2020;54:102350. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 58] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 90. | Cosco TD, Fortuna K, Wister A, Riadi I, Wagner K, Sixsmith A. COVID-19, Social Isolation, and Mental Health Among Older Adults: A Digital Catch-22. J Med Internet Res. 2021;23:e21864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 91. | Naidu SC, Persaud M, Sheikhan NY, Sem G, O'Driscoll V, Diamond L, Pitch N, Dhingra N, Nowak DA, Kuluski K. Student-senior isolation prevention partnership: a Canada-wide programme to mitigate social exclusion during the COVID-19 pandemic. Health Promot Int. 2022;37:daab118. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 92. | Pietromonaco PR, Overall NC. Implications of social isolation, separation, and loss during the COVID-19 pandemic for couples' relationships. Curr Opin Psychol. 2022;43:189-194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 45] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 93. | Mathieu S, Treloar A, Hawgood J, Ross V, Kõlves K. The Role of Unemployment, Financial Hardship, and Economic Recession on Suicidal Behaviors and Interventions to Mitigate Their Impact: A Review. Front Public Health. 2022;10:907052. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 94. | Faria M, Santos MR, Sargento P, Branco M. The role of social support in suicidal ideation: a comparison of employed vs. unemployed people. J Ment Health. 2020;29:52-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 95. | Fisher JE, Rice AJ, Zuleta RF, Cozza SJ. Bereavement during the COVID-19 Pandemic: Impact on Coping Strategies and Mental Health. Psychiatry. 2022;85:354-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 96. | Eisma MC, Tamminga A. COVID-19, natural, and unnatural bereavement: comprehensive comparisons of loss circumstances and grief severity. Eur J Psychotraumatol. 2022;13:2062998. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 97. | Danet Danet A. Psychological impact of COVID-19 pandemic in Western frontline healthcare professionals. A systematic review. Med Clin (Barc). 2021;156:449-458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 84] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 98. | Teo WZY, Yap ES, Yip C, Ong L, Lee CT. The psychological impact of COVID-19 on 'hidden' frontline healthcare workers. Int J Soc Psychiatry. 2021;67:284-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 99. | Li Y, Fan R, Lu Y, Li H, Liu X, Kong G, Wang J, Yang F, Zhou J, Wang J. Prevalence of psychological symptoms and associated risk factors among nurses in 30 provinces during the COVID-19 pandemic in China. Lancet Reg Health West Pac. 2023;30:100618. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 29] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 100. | Rodriguez-Besteiro S, Beltran-Velasco AI, Tornero-Aguilera JF, Martínez-González MB, Navarro-Jiménez E, Yáñez-Sepúlveda R, Clemente-Suárez VJ. Social Media, Anxiety and COVID-19 Lockdown Measurement Compliance. Int J Environ Res Public Health. 2023;20:4416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 101. | Latikka R, Koivula A, Oksa R, Savela N, Oksanen A. Loneliness and psychological distress before and during the COVID-19 pandemic: Relationships with social media identity bubbles. Soc Sci Med. 2022;293:114674. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 38] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 102. | Ünlü B, Simsek R, Köse SBE, Yirün A, Erkekoglu P. Neurological Effects of SARS-CoV-2 and Neurotoxicity of Antiviral Drugs Against COVID-19. Mini Rev Med Chem. 2022;22:213-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 103. | Hogberg HT, Tsaioun K, Breidenbach JD, Elmore B, Filipovska J, Garcia-Reyero N, Hargreaves AJ, Joshi O, Omeragic E, Plant S, Ram R, Virmani I, Waspe J, Macmillan DS. A systematic scoping review of the neurological effects of COVID-19. Neurotoxicology. 2024;103:16-26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 104. | Ren AL, Digby RJ, Needham EJ. Neurological update: COVID-19. J Neurol. 2021;268:4379-4387. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 105. | Labrague LJ. Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: A systematic review of quantitative studies. J Nurs Manag. 2021;29:1893-1905. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 324] [Article Influence: 64.8] [Reference Citation Analysis (0)] |
| 106. | Zysberg L, Zisberg A. Days of worry: Emotional intelligence and social support mediate worry in the COVID-19 pandemic. J Health Psychol. 2022;27:268-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 55] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 107. | Marks DF. Psychological homeostasis and protective behaviours in the COVID-19 pandemic. J Health Psychol. 2022;27:1275-1287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 108. | Riedel B, Horen SR, Reynolds A, Hamidian Jahromi A. Mental Health Disorders in Nurses During the COVID-19 Pandemic: Implications and Coping Strategies. Front Public Health. 2021;9:707358. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 55] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 109. | Sepúlveda-Loyola W, Rodríguez-Sánchez I, Pérez-Rodríguez P, Ganz F, Torralba R, Oliveira DV, Rodríguez-Mañas L. Impact of Social Isolation Due to COVID-19 on Health in Older People: Mental and Physical Effects and Recommendations. J Nutr Health Aging. 2020;24:938-947. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 100] [Cited by in RCA: 149] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 110. | Tandon PS, Zhou C, Johnson AM, Gonzalez ES, Kroshus E. Association of Children's Physical Activity and Screen Time With Mental Health During the COVID-19 Pandemic. JAMA Netw Open. 2021;4:e2127892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 114] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 111. | Hajek A, Kretzler B, Walther C, Aarabi G, Zwar L, König HH. Neighbourhood cohesion, loneliness and perceived social isolation prior and during the COVID-19 pandemic. Longitudinal evidence from the German Ageing Survey. Soc Psychiatry Psychiatr Epidemiol. 2023;58:1411-1420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 112. | Kingsbury M, Clayborne Z, Colman I, Kirkbride JB. The protective effect of neighbourhood social cohesion on adolescent mental health following stressful life events. Psychol Med. 2020;50:1292-1299. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 75] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 113. | Meng X, D'Arcy C. Coping strategies and distress reduction in psychological well-being? A structural equation modelling analysis using a national population sample. Epidemiol Psychiatr Sci. 2016;25:370-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 114. | Puig-Perez S, Cano-López I, Martínez P, Kozusznik MW, Alacreu-Crespo A, Pulopulos MM, Duque A, Almela M, Aliño M, Garcia-Rubio MJ, Pollak A, Kożusznik B. Optimism as a protective factor against the psychological impact of COVID-19 pandemic through its effects on perceived stress and infection stress anticipation. Curr Psychol. 2022;1-15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 115. | Bakalova D, Nacheva I, Panchelieva T. Psychological Predictors of COVID-19-Related Anxiety in Vulnerable Groups. Eur J Investig Health Psychol Educ. 2023;13:1815-1830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 116. | Gangamma R, Walia B, Luke M, Lucena C. Continuation of Teletherapy After the COVID-19 Pandemic: Survey Study of Licensed Mental Health Professionals. JMIR Form Res. 2022;6:e32419. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 117. | Taylor CB, Fitzsimmons-Craft EE, Graham AK. Digital technology can revolutionize mental health services delivery: The COVID-19 crisis as a catalyst for change. Int J Eat Disord. 2020;53:1155-1157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 101] [Cited by in RCA: 114] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 118. | Lei MK, Klopack ET. Social and psychological consequences of the COVID-19 outbreak: The experiences of Taiwan and Hong Kong. Psychol Trauma. 2020;12:S35-S37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 119. | Zenba Y, Kobayashi A, Imai T. Psychological distress is affected by fear of COVID-19 via lifestyle disruption and leisure restriction among older adults in Japan: a cross-sectional study. Front Public Health. 2023;11:1264088. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 120. | Prizmić-Larsen Z, Vujčić MT, Lipovčan LK. Fear of COVID-19 and Fear of Earthquake: Multiple Distressing Events and Well-Being in Croatia. Psychol Rep. 2025;128:435-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 121. | Wang S, Guan YG, Zhu YH, Wang MZ. Role of high mobility group box protein 1 in depression: A mechanistic and therapeutic perspective. World J Psychiatry. 2022;12:779-786. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (10)] |
| 122. | Durcan E, Hacioglu A, Karaca Z, Unluhizarci K, Gonen MS, Kelestimur F. Hypothalamic-Pituitary Axis Function and Adrenal Insufficiency in COVID-19 Patients. Neuroimmunomodulation. 2023;30:215-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 123. | Elder GJ, Altena E, Palagini L, Ellis JG. Stress and the hypothalamic-pituitary-adrenal axis: How can the COVID-19 pandemic inform our understanding and treatment of acute insomnia? J Sleep Res. 2023;32:e13842. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 124. | He J, Lin J, Sun W, Cheung T, Cao Y, Fu E, Chan SHW, Tsang HWH. The effects of psychosocial and behavioral interventions on depressive and anxiety symptoms during the COVID-19 pandemic: a systematic review and meta-analysis. Sci Rep. 2023;13:19094. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 125. | Dubey S, Biswas P, Ghosh R, Chatterjee S, Dubey MJ, Chatterjee S, Lahiri D, Lavie CJ. Psychosocial impact of COVID-19. Diabetes Metab Syndr. 2020;14:779-788. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1000] [Cited by in RCA: 969] [Article Influence: 161.5] [Reference Citation Analysis (0)] |
| 126. | Richmond J, Sanderson M, Shrubsole MJ, Holowatyj AN, Schlundt DG, Aldrich MC. Psychosocial impact of COVID-19 among adults in the southeastern United States. Prev Med. 2022;163:107191. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 127. | Huh MK, Fitzpatrick K, Harris C, Niño M. Social and psychological resources and COVID-19 related fear, threat and worry. Anxiety Stress Coping. 2023;36:710-726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 128. | Pan KY, Kok AAL, Eikelenboom M, Horsfall M, Jörg F, Luteijn RA, Rhebergen D, Oppen PV, Giltay EJ, Penninx BWJH. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three Dutch case-control cohorts. Lancet Psychiatry. 2021;8:121-129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 301] [Cited by in RCA: 363] [Article Influence: 72.6] [Reference Citation Analysis (0)] |
| 129. | Fancourt D, Steptoe A, Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. 2021;8:141-149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 504] [Cited by in RCA: 694] [Article Influence: 138.8] [Reference Citation Analysis (0)] |
| 130. | Varga TV, Bu F, Dissing AS, Elsenburg LK, Bustamante JJH, Matta J, van Zon SKR, Brouwer S, Bültmann U, Fancourt D, Hoeyer K, Goldberg M, Melchior M, Strandberg-Larsen K, Zins M, Clotworthy A, Rod NH. Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: A longitudinal analysis of 200,000 Western and Northern Europeans. Lancet Reg Health Eur. 2021;2:100020. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 166] [Cited by in RCA: 146] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 131. | Zobi M, Abrokwa SK, Dordoye E, Phuti A. A mixed method study on the impact of COVID-19 on mental healthcare in Ghana: rethinking mental health service delivery. Int J Equity Health. 2024;23:56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 132. | Arevian AC, Jones F, Moore EM, Goodsmith N, Aguilar-Gaxiola S, Ewing T, Siddiq H, Lester P, Cheung E, Ijadi-Maghsoodi R, Gabrielian S, Sugarman OK, Bonds C, Benitez C, Innes-Gomberg D, Springgate B, Haywood C, Meyers D, Sherin JE, Wells K. Mental Health Community and Health System Issues in COVID-19: Lessons from Academic, Community, Provider and Policy Stakeholders. Ethn Dis. 2020;30:695-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 133. | Javed A, Lee C, Zakaria H, Buenaventura RD, Cetkovich-Bakmas M, Duailibi K, Ng B, Ramy H, Saha G, Arifeen S, Elorza PM, Ratnasingham P, Azeem MW. Reducing the stigma of mental health disorders with a focus on low- and middle-income countries. Asian J Psychiatr. 2021;58:102601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 145] [Article Influence: 29.0] [Reference Citation Analysis (0)] |
| 134. | Rebello TJ, Marques A, Gureje O, Pike KM. Innovative strategies for closing the mental health treatment gap globally. Curr Opin Psychiatry. 2014;27:308-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 135. | Thome J, Deloyer J, Coogan AN, Bailey-Rodriguez D, da Cruz E Silva OAB, Faltraco F, Grima C, Gudjonsson SO, Hanon C, Hollý M, Joosten J, Karlsson I, Kelemen G, Korman M, Krysta K, Lichterman B, Loganovsky K, Marazziti D, Maraitou M, Mertens deWilmars S, Reunamen M, Rexhaj S, Sancaktar M, Sempere J, Tournier I, Weynant E, Vis C, Lebas MC, Fond-Harmant L. The impact of the early phase of the COVID-19 pandemic on mental-health services in Europe. World J Biol Psychiatry. 2021;22:516-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 136. | Okuyama J, Izumi SI, Funakoshi S, Seto S, Sasaki H, Ito K, Imamura F, Willgerodt M, Fukuda Y. Supporting adolescents' mental health during COVID-19 by utilising lessons from the aftermath of the Great East Japan Earthquake. Humanit Soc Sci Commun. 2022;9:332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 137. | Levaj S, Medved S, Grubišin J, Tomašić L, Brozić K, Shields-Zeeman L, Bolinski F, Rojnic Kuzman M. The impact of the COVID-19 pandemic and earthquake on mental health of persons with severe mental illness: A survey study among people receiving community mental health care versus treatment as usual in Croatia. Int J Soc Psychiatry. 2023;69:653-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 138. | Sukut O, Ayhan Balik CH. The impact of COVID-19 pandemic on people with severe mental illness. Perspect Psychiatr Care. 2021;57:953-956. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 139. | Li J, Zhou Y, Ma J, Zhang Q, Shao J, Liang S, Yu Y, Li W, Wang C. The long-term health outcomes, pathophysiological mechanisms and multidisciplinary management of long COVID. Signal Transduct Target Ther. 2023;8:416. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 72] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 140. | Kassem AM, Witte TK, Nett RJ, Carter KK. Characteristics associated with negative attitudes toward mental illness among US veterinarians. J Am Vet Med Assoc. 2019;254:979-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 141. | Berry C, Michelson D, Othman E, Tan JC, Gee B, Hodgekins J, Byrne RE, Ng ALO, Marsh NV, Coker S, Fowler D. Views of young people in Malaysia on mental health, help-seeking and unusual psychological experiences. Early Interv Psychiatry. 2020;14:115-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 142. | Basri T, Radhakrishnan K, Rolin D. Barriers to and Facilitators of Mental Health Help-Seeking Behaviors Among South Asian American College Students. J Psychosoc Nurs Ment Health Serv. 2022;60:32-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 143. | Husain W. Barriers in Seeking Psychological Help: Public Perception in Pakistan. Community Ment Health J. 2020;56:75-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 144. | Robertson JJ, Long B. Medicine's Shame Problem. J Emerg Med. 2019;57:329-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 145. | Thi LM, Manzano A, Ha BTT, Vui LT, Quynh-Chi NT, Duong DTT, Lakin K, Kane S, Mirzoev T, Trang DTH. Mental health stigma and health-seeking behaviors amongst pregnant women in Vietnam: a mixed-method realist study. Int J Equity Health. 2024;23:163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 146. | Kotera Y, Mayer CH, Vanderheiden E. Self-compassion, mental health shame and work motivation in German and Japanese employees. Int Rev Psychiatry. 2023;35:113-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 147. | Oyat FWD, Oloya JN, Atim P, Ikoona EN, Aloyo J, Kitara DL. The psychological impact, risk factors and coping strategies to COVID-19 pandemic on healthcare workers in the sub-Saharan Africa: a narrative review of existing literature. BMC Psychol. 2022;10:284. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 23] [Reference Citation Analysis (0)] |
| 148. | Gray NS, Davies H, Brad R, Snowden RJ. Reducing sickness absence and stigma due to mental health difficulties: a randomised control treatment trial (RCT) of a low intensity psychological intervention and stigma reduction programme for common mental disorder (Prevail). BMC Public Health. 2023;23:1324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 149. | Hampson ME, Watt BD, Hicks RE. Impacts of stigma and discrimination in the workplace on people living with psychosis. BMC Psychiatry. 2020;20:288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 150. | Tajan N, Devès M, Potier R. Tele-psychotherapy during the COVID-19 pandemic: a mini-review. Front Psychiatry. 2023;14:1060961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 151. | Schmidt SA. Teletherapy Used to Breakdown Access Barriers. Telemed J E Health. 2024;30:1491-1494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 152. | Gamoran J, Xu Y, Buinewicz SAP, Liu J, Mowrey W, Goldentyer G, Gabbay V, Pimentel SS. An examination of depression severity and treatment adherence among racially and ethnically minoritized, low-income individuals during the COVID-19 transition to telehealth. Psychiatry Res. 2024;342:116221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 153. | Davis KA, Zhao F, Janis RA, Castonguay LG, Hayes JA, Scofield BE. Therapeutic alliance and clinical outcomes in teletherapy and in-person psychotherapy: A noninferiority study during the COVID-19 pandemic. Psychother Res. 2024;34:589-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 154. | Chan S, Parish M, Yellowlees P. Telepsychiatry Today. Curr Psychiatry Rep. 2015;17:89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 53] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 155. | Naqvi SSB, Davis J, Pickles RW, Loewenthal MR. Concerns and psychological well-being of healthcare workers during the COVID-19 pandemic in a tertiary care hospital in New South Wales. Intern Med J. 2021;51:1407-1413. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 156. | Chevance A, Gourion D, Hoertel N, Llorca PM, Thomas P, Bocher R, Moro MR, Laprévote V, Benyamina A, Fossati P, Masson M, Leaune E, Leboyer M, Gaillard R. Ensuring mental health care during the SARS-CoV-2 epidemic in France: A narrative review. Encephale. 2020;46:193-201. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 187] [Cited by in RCA: 158] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 157. | O'Brien L, Tighe J, Doroud N, Barradell S, Dowling L, Pranata A, Ganderton C, Lovell R, Hughes R. "Burnout felt inevitable": Experiences of university staff in educating the nursing and allied health workforce during the first COVID-19 waves. Front Public Health. 2023;11:1082325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 158. | Luo Z, Gardiner JC, Smith RC. Costs of a Train-the-Trainer Program to Teach Primary Care Faculty Mental Health Care. Med Care. 2021;59:970-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 159. | Watanabe-Galloway S, Madison L, Watkins KL, Nguyen AT, Chen LW. Recruitment and retention of mental health care providers in rural Nebraska: perceptions of providers and administrators. Rural Remote Health. 2015;15:3392. [PubMed] |
| 160. | Maalouf FT, Alamiri B, Atweh S, Becker AE, Cheour M, Darwish H, Ghandour LA, Ghuloum S, Hamze M, Karam E, Khoury B, Khoury SJ, Mokdad A, Meho LI, Okasha T, Reed GM, Sbaity E, Zeinoun P, Akl EA. Mental health research in the Arab region: challenges and call for action. Lancet Psychiatry. 2019;6:961-966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 59] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 161. | Obschonka M, Gewirtz AH, Zhu L. Psychological implications of the COVID-19 pandemic around the world: Introduction to the special issue. Int J Psychol. 2021;56:493-497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 162. | Gálvez-Herrer M, Via-Clavero G, Ángel-Sesmero JA, Heras-La Calle G. Psychological crisis and emergency intervention for frontline critical care workers during the COVID-19 pandemic. J Clin Nurs. 2022;31:2309-2323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 163. | Wang Q, An S, Shao Z. Psychological intervention for negative emotions aroused by COVID-19 pandemic in university students: A systematic review and meta-analysis. PLoS One. 2023;18:e0283208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 164. | Bauer MS, Kirchner J. Implementation science: What is it and why should I care? Psychiatry Res. 2020;283:112376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 655] [Article Influence: 109.2] [Reference Citation Analysis (0)] |
| 165. | Singla DR, Hollon SD. The importance of implementation science in scaling up psychological treatments. Behav Res Ther. 2020;130:103614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 166. | Wiltsey Stirman S, Beidas RS. Expanding the reach of psychological science through implementation science: Introduction to the special issue. Am Psychol. 2020;75:1033-1037. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 167. | Lombardo C, Guo L, Solomon S, Crepaz-Keay D, McDaid S, Thorpe L, Martin S, John A, Morton A, Davidson G, Kousoulis AA, Van Bortel T. Inequalities and mental health during the Coronavirus pandemic in the UK: a mixed-methods exploration. BMC Public Health. 2023;23:1830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 168. | Moitra M, Owens S, Hailemariam M, Wilson KS, Mensa-Kwao A, Gonese G, Kamamia CK, White B, Young DM, Collins PY. Global Mental Health: Where We Are and Where We Are Going. Curr Psychiatry Rep. 2023;25:301-311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 92] [Article Influence: 30.7] [Reference Citation Analysis (0)] |
| 169. | Uphoff E, Robertson L, Cabieses B, Villalón FJ, Purgato M, Churchill R, Barbui C. An overview of systematic reviews on mental health promotion, prevention, and treatment of common mental disorders for refugees, asylum seekers, and internally displaced persons. Cochrane Database Syst Rev. 2020;9:CD013458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 170. | Heinrich CJ, Colomer A, Hieronimus M. Minding the gap: Evidence, implementation and funding gaps in mental health services delivery for school-aged children. Child Youth Serv Rev. 2023;150:107023. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 171. | Wang S, Zhang Y, Wen Z, Yang Y, Zhang Y, Geng Y, Liu Y, Zhang J. Development, Evaluation, and impLemenTation for guideline adaptation: a quality improvement protocol for the DELTA study in global health practice. Health Res Policy Syst. 2023;21:114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 172. | Patel V, Saxena S, Lund C, Kohrt B, Kieling C, Sunkel C, Kola L, Chang O, Charlson F, O'Neill K, Herrman H. Transforming mental health systems globally: principles and policy recommendations. Lancet. 2023;402:656-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 80] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 173. | Evans-Lacko S, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, Benjet C, Bruffaerts R, Chiu WT, Florescu S, de Girolamo G, Gureje O, Haro JM, He Y, Hu C, Karam EG, Kawakami N, Lee S, Lund C, Kovess-Masfety V, Levinson D, Navarro-Mateu F, Pennell BE, Sampson NA, Scott KM, Tachimori H, Ten Have M, Viana MC, Williams DR, Wojtyniak BJ, Zarkov Z, Kessler RC, Chatterji S, Thornicroft G. Socio-economic variations in the mental health treatment gap for people with anxiety, mood, and substance use disorders: results from the WHO World Mental Health (WMH) surveys. Psychol Med. 2018;48:1560-1571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 410] [Article Influence: 51.3] [Reference Citation Analysis (0)] |
| 174. | Cortese S, Purper-Ouakil D, Apter A, Arango C, Baeza I, Banaschewski T, Buitelaar J, Castro-Fornieles J, Coghill D, Cohen D, Correll CU, Grünblatt E, Hoekstra PJ, James A, Jeppesen P, Nagy P, Pagsberg AK, Parellada M, Persico AM, Roessner V, Santosh P, Simonoff E, Stevanovic D, Stringaris A, Vitiello B, Walitza S, Weizman A, Wong ICK, Zalsman G, Zuddas A, Carucci S, Butlen-Ducuing F, Tome M, Bea M, Getin C, Hovén N, Konradsson-Geuken A, Lamirell D, Olisa N, Nafria Escalera B, Moreno C. Psychopharmacology in children and adolescents: unmet needs and opportunities. Lancet Psychiatry. 2024;11:143-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 24] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 175. | Mercado AE, Chesky KA, Panchamukhi AV, Boyd JW. US Medical Student Health Insurance Coverage for Mental Health Treatment After the COVID-19 Pandemic. JAMA Intern Med. 2023;183:1273-1275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 176. | Shoib S, Zaidi I, Saeed F, Banerjee D, Swed S, Chandradasa M. Mental health insurance reform in India. Lancet Psychiatry. 2023;10:660-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 177. | Milani SA, Kuo YF, Raji M. COVID-19 and mental health consequences: moving forward. Lancet Psychiatry. 2024;11:777-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 178. | Aknin LB, De Neve JE, Dunn EW, Fancourt DE, Goldberg E, Helliwell JF, Jones SP, Karam E, Layard R, Lyubomirsky S, Rzepa A, Saxena S, Thornton EM, VanderWeele TJ, Whillans AV, Zaki J, Karadag O, Ben Amor Y. Mental Health During the First Year of the COVID-19 Pandemic: A Review and Recommendations for Moving Forward. Perspect Psychol Sci. 2022;17:915-936. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 221] [Article Influence: 55.3] [Reference Citation Analysis (0)] |
| 179. | Clift AK, Ranger TA, Patone M, Coupland CAC, Hatch R, Thomas K, Hippisley-Cox J, Watkinson P. Neuropsychiatric Ramifications of Severe COVID-19 and Other Severe Acute Respiratory Infections. JAMA Psychiatry. 2022;79:690-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 180. | Lu ZA, Shi L, Que JY, Zheng YB, Wang QW, Liu WJ, Huang YT, Shi J, Bao YP, Lu L. Long-term psychological profile of general population following COVID-19 outbreak: symptom trajectories and evolution of psychopathological network. Epidemiol Psychiatr Sci. 2022;31:e69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 181. | Mazza MG, Palladini M, Poletti S, Benedetti F. Post-COVID-19 Depressive Symptoms: Epidemiology, Pathophysiology, and Pharmacological Treatment. CNS Drugs. 2022;36:681-702. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 127] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 182. | Bourgault Z, Ibrahim C, Le Foll B, Hassan AN. Comparing immediate- and delayed-onset posttraumatic stress disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). J Trauma Stress. 2022;35:1744-1755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 183. | Sumner JA, Rünger D, Robles TF, Lowe SR, Elashoff D, Shetty V. Understanding trajectories of underlying dimensions of posttraumatic psychopathology. J Affect Disord. 2021;284:75-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 184. | Holly LE. Cultural and Social Aspects of Anxiety Disorders. Psychiatr Clin North Am. 2024;47:775-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 185. | Fekih-Romdhane F, Jahrami H, Stambouli M, Alhuwailah A, Helmy M, Shuwiekh HAM, Lemine CMFM, Radwan E, Saquib J, Saquib N, Fawaz M, Zarrouq B, Naser AY, Obeid S, Hallit S, Saleh M, Haider S, Daher-Nashif S, Miloud L, Badrasawi M, Hamdan-Mansour A, Barbato M, Bakhiet A, Sayem N, Adawi S, Grein F, Cherif W, Chalghaf N, Husni M, Alrasheed MM, Cheour M. Cross-cultural comparison of mental illness stigma and help-seeking attitudes: a multinational population-based study from 16 Arab countries and 10,036 individuals. Soc Psychiatry Psychiatr Epidemiol. 2023;58:641-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 36] [Reference Citation Analysis (0)] |
| 186. | Goldsmith ES, Koffel E, Ackland PE, Hill J, Landsteiner A, Miller W, Stroebel B, Ullman K, Wilt TJ, Duan-Porter WD. Evaluation of Implementation Strategies for Cognitive Behavioral Therapy (CBT), Acceptance and Commitment Therapy (ACT), and Mindfulness-Based Stress Reduction (MBSR): a Systematic Review. J Gen Intern Med. 2023;38:2782-2791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 187. | Dorsey S, Gray CL, Wasonga AI, Amanya C, Weiner BJ, Belden CM, Martin P, Meza RD, Weinhold AK, Soi C, Murray LK, Lucid L, Turner EL, Mildon R, Whetten K. Advancing successful implementation of task-shifted mental health care in low-resource settings (BASIC): protocol for a stepped wedge cluster randomized trial. BMC Psychiatry. 2020;20:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 188. | Dorsey S, Lucid L, Martin P, King KM, O'Donnell K, Murray LK, Wasonga AI, Itemba DK, Cohen JA, Manongi R, Whetten K. Effectiveness of Task-Shifted Trauma-Focused Cognitive Behavioral Therapy for Children Who Experienced Parental Death and Posttraumatic Stress in Kenya and Tanzania: A Randomized Clinical Trial. JAMA Psychiatry. 2020;77:464-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 77] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 189. | Goodkind JR, Amer S, Christian C, Hess JM, Bybee D, Isakson BL, Baca B, Ndayisenga M, Greene RN, Shantzek C. Challenges and Innovations in a Community-Based Participatory Randomized Controlled Trial. Health Educ Behav. 2017;44:123-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 190. | Rodriguez Espinosa P, Verney SP. The Underutilization of Community-based Participatory Research in Psychology: A Systematic Review. Am J Community Psychol. 2021;67:312-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 191. | Hoeft TJ, Fortney JC, Patel V, Unützer J. Task-Sharing Approaches to Improve Mental Health Care in Rural and Other Low-Resource Settings: A Systematic Review. J Rural Health. 2018;34:48-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 309] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 192. | R Kottai S, Ranganathan S. Task-Shifting in Community Mental Health in Kerala: Tensions and Ruptures. Med Anthropol. 2020;39:538-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 193. | Aurizki GE, Wilson I. Nurse-led task-shifting strategies to substitute for mental health specialists in primary care: A systematic review. Int J Nurs Pract. 2022;28:e13046. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 194. | Alonzo D, Popescu M. A qualitative examination of the mental health impact of Covid-19 in marginalized communities in Guatemala: The Covid Care Calls survey. Int J Soc Psychiatry. 2022;68:1435-1444. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 195. | Strudwick G, Sockalingam S, Kassam I, Sequeira L, Bonato S, Youssef A, Mehta R, Green N, Agic B, Soklaridis S, Impey D, Wiljer D, Crawford A. Digital Interventions to Support Population Mental Health in Canada During the COVID-19 Pandemic: Rapid Review. JMIR Ment Health. 2021;8:e26550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 196. | Witteveen AB, Young S, Cuijpers P, Ayuso-Mateos JL, Barbui C, Bertolini F, Cabello M, Cadorin C, Downes N, Franzoi D, Gasior M, John A, Melchior M, McDaid D, Palantza C, Purgato M, Van der Waerden J, Wang S, Sijbrandij M. Remote mental health care interventions during the COVID-19 pandemic: An umbrella review. Behav Res Ther. 2022;159:104226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 46] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 197. | Liu XQ, Guo YX, Zhang XR, Zhang LX, Zhang YF. Digital interventions empowering mental health reconstruction among students after the COVID-19 pandemic. World J Psychiatry. 2023;13:397-401. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 198. | He Y, Yang L, Zhu X, Wu B, Zhang S, Qian C, Tian T. Mental Health Chatbot for Young Adults With Depressive Symptoms During the COVID-19 Pandemic: Single-Blind, Three-Arm Randomized Controlled Trial. J Med Internet Res. 2022;24:e40719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 61] [Reference Citation Analysis (0)] |
| 199. | Li X, Vanderloo LM, Keown-Stoneman CDG, Cost KT, Charach A, Maguire JL, Monga S, Crosbie J, Burton C, Anagnostou E, Georgiades S, Nicolson R, Kelley E, Ayub M, Korczak DJ, Birken CS. Screen Use and Mental Health Symptoms in Canadian Children and Youth During the COVID-19 Pandemic. JAMA Netw Open. 2021;4:e2140875. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 80] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 200. | Zhong S, Yang X, Pan Z, Fan Y, Chen Y, Yu X, Zhou L. The Usability, Feasibility, Acceptability, and Efficacy of Digital Mental Health Services in the COVID-19 Pandemic: Scoping Review, Systematic Review, and Meta-analysis. JMIR Public Health Surveill. 2023;9:e43730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 32] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 201. | Pham KT, Nabizadeh A, Selek S. Artificial Intelligence and Chatbots in Psychiatry. Psychiatr Q. 2022;93:249-253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 90] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 202. | Sun J, Dong QX, Wang SW, Zheng YB, Liu XX, Lu TS, Yuan K, Shi J, Hu B, Lu L, Han Y. Artificial intelligence in psychiatry research, diagnosis, and therapy. Asian J Psychiatr. 2023;87:103705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 65] [Article Influence: 21.7] [Reference Citation Analysis (0)] |
| 203. | Balcombe L, De Leo D. Digital Mental Health Challenges and the Horizon Ahead for Solutions. JMIR Ment Health. 2021;8:e26811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 59] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 204. | Benda N, Desai P, Reza Z, Zheng A, Kumar S, Harkins S, Hermann A, Zhang Y, Joly R, Kim J, Pathak J, Reading Turchioe M. Patient Perspectives on AI for Mental Health Care: Cross-Sectional Survey Study. JMIR Ment Health. 2024;11:e58462. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 17] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 205. | Patel S, Craigen G, Pinto da Costa M, Inkster B. Opportunities and Challenges for Digital Social Prescribing in Mental Health: Questionnaire Study. J Med Internet Res. 2021;23:e17438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 206. | Pretorius C, Chambers D, Coyle D. Young People's Online Help-Seeking and Mental Health Difficulties: Systematic Narrative Review. J Med Internet Res. 2019;21:e13873. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 107] [Cited by in RCA: 228] [Article Influence: 32.6] [Reference Citation Analysis (0)] |
| 207. | Teachman BA, Silverman AL, Werntz A. Digital Mental Health Services: Moving From Promise to Results. Cogn Behav Pract. 2022;29:97-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 208. | Rajkumar RP. Harnessing the Neurobiology of Resilience to Protect the Mental Well-Being of Healthcare Workers During the COVID-19 Pandemic. Front Psychol. 2021;12:621853. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 209. | Roy A, Singh AK, Mishra S, Chinnadurai A, Mitra A, Bakshi O. Mental health implications of COVID-19 pandemic and its response in India. Int J Soc Psychiatry. 2021;67:587-600. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 77] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 210. | Li N, Fan L, Wang Y, Wang J, Huang Y. Risk factors of psychological distress during the COVID-19 pandemic: The roles of coping style and emotional regulation. J Affect Disord. 2022;299:326-334. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 211. | Li N, Li S, Fan L. Risk Factors of Psychological Disorders After the COVID-19 Outbreak: The Mediating Role of Social Support and Emotional Intelligence. J Adolesc Health. 2021;69:696-704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 212. | Racine S, Miller A, Mehak A, Trolio V. Examining risk and protective factors for psychological health during the COVID-19 pandemic. Anxiety Stress Coping. 2022;35:124-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 213. | Stuenkel M, Koob C, Richardson E, Griffin SF, Sease KK. School-Based Mental Health Service Utilization Through the COVID-19 Pandemic and Beyond. J Sch Health. 2023;93:1000-1005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 214. | Kim DK, Lee I, Choi C, Park SU. Mental health and governmental response policy evaluation on COVID-19 based on vaccination status in Republic of Korea. BMC Public Health. 2023;23:1628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 215. | Bennett RJ, Cumming-Potvin E, Eikelboom RH, Manchiah V, Badcock JC, Swanepoel W. Changes in audiologists' mental wellbeing during the COVID-19 pandemic: the supportive role of professional associations, workplaces and hearing device manufacturers. Int J Audiol. 2023;62:533-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 216. | Sharma D, Singh J, Shah B, Ali F, AlZubi AA, AlZubi MA. Public mental health through social media in the post COVID-19 era. Front Public Health. 2023;11:1323922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 217. | Zhu C, Zhang T, Li Q, Chen X, Wang K. Depression and Anxiety During the COVID-19 Pandemic: Epidemiology, Mechanism, and Treatment. Neurosci Bull. 2023;39:675-684. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 79] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 218. | Khorasanchi Z, Rashidmayvan M, Hasanzadeh E, Moghadam MRSF, Afkhami N, Asadiyan-Sohan P, Fard MV, Mohammadhasani K, Varaste N, Sharifan P, Ferns G, Mobarhan MG. The association of hematological inflammatory markers and psychological function in COVID-19 patients: A cross-sectional study. Physiol Rep. 2023;11:e15889. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 219. | Scalabrini A, Palladini M, Mazza MG, Mucci C, Northoff G, Benedetti F. In Between the Psychological and Physiological Self - The Impact of Covid-19 Pandemic on the Neuro-Socio-Ecological and Inflammatory Mind-Body-Brain System. Clin Neuropsychiatry. 2023;20:342-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 220. | Villarreal-Zegarra D, Paredes-Angeles R, Mayo-Puchoc N, Vilela-Estada AL, Copez-Lonzoy A, Huarcaya-Victoria J. An explanatory model of depressive symptoms from anxiety, post-traumatic stress, somatic symptoms, and symptom perception: the potential role of inflammatory markers in hospitalized COVID-19 patients. BMC Psychiatry. 2022;22:638. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 221. | Duden GS, Gersdorf S, Stengler K. Global impact of the COVID-19 pandemic on mental health services: A systematic review. J Psychiatr Res. 2022;154:354-377. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 74] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 222. | Tanner LM, Wildman JM, Stoniute A, Still M, Bernard K, Green R, Eastaugh CH, Thomson KH, Sowden S. Non-pharmaceutical primary care interventions to improve mental health in deprived populations: a systematic review. Br J Gen Pract. 2023;73:e242-e248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 223. | Pouls KP, Koks-Leensen MC, Mastebroek M, Leusink GL, Assendelft WJ. Adults with intellectual disabilities and mental health disorders in primary care: a scoping review. Br J Gen Pract. 2022;72:e168-e178. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 224. | Toro-Devia O, Leyton G. COVID-19 pandemic and mental healthcare: Impact on health insurance with guaranteed universal access in Chile. Front Public Health. 2022;10:1005033. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 225. | Nair S, Kannan P, Mehta K, Raju A, Mathew J, Ramachandran P. The COVID-19 pandemic and its impact on mental health services: the provider perspective. J Public Health (Oxf). 2021;43:ii51-ii56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 226. | Wagner B, Snoubar Y, Mahdi YS. Access and efficacy of university mental health services during the COVID-19 pandemic. Front Public Health. 2023;11:1269010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 227. | Goldman ML, Druss BG, Horvitz-Lennon M, Norquist GS, Kroeger Ptakowski K, Brinkley A, Greiner M, Hayes H, Hepburn B, Jorgensen S, Swartz MS, Dixon LB. Mental Health Policy in the Era of COVID-19. Psychiatr Serv. 2020;71:1158-1162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 65] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 228. | Haber NA, Clarke-Deelder E, Feller A, Smith ER, Salomon JA, MacCormack-Gelles B, Stone EM, Bolster-Foucault C, Daw JR, Hatfield LA, Fry CE, Boyer CB, Ben-Michael E, Joyce CM, Linas BS, Schmid I, Au EH, Wieten SE, Jarrett B, Axfors C, Nguyen VT, Griffin BA, Bilinski A, Stuart EA. Problems with evidence assessment in COVID-19 health policy impact evaluation: a systematic review of study design and evidence strength. BMJ Open. 2022;12:e053820. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 229. | Villarreal-Zegarra D, Reátegui-Rivera CM, Sabastizagal-Vela I, Burgos-Flores MA, Cama-Ttito NA, Rosales-Rimache J. Policies on mental health in the workplace during the COVID-19 pandemic: A scoping review. PLoS One. 2022;17:e0272296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 230. | Cummings JR, Zhang X, Gandré C, Morsella A, Shields-Zeeman L, Winkelmann J, Allin S, Augusto GF, Cascini F, Cserháti Z, de Belvis AG, Eriksen A, Fronteira I, Jamieson M, Murauskienė L, Palmer WL, Ricciardi W, Samuel H, Scintee SG, Taube M, Vrangbæk K, van Ginneken E. Challenges facing mental health systems arising from the COVID-19 pandemic: Evidence from 14 European and North American countries. Health Policy. 2023;136:104878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 231. | Kim M, Yun B, Sim J, Cho A, Oh J, Kim J, Nambunmee K, Rozek LS, Yoon JH. Risk of psychological distress by decrease in economic activity, gender, and age due to COVID-19: A multinational study. Front Public Health. 2023;11:1056768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 232. | Lawal MA, Shalaby R, Chima C, Vuong W, Hrabok M, Gusnowski A, Surood S, Greenshaw AJ, Agyapong VIO. COVID-19 Pandemic: Stress, Anxiety, and Depression Levels Highest amongst Indigenous Peoples in Alberta. Behav Sci (Basel). 2021;11:115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 233. | Gonçalves Júnior J, Freitas JF, Cândido EL. COVID-19, mental health and Indigenous populations in Brazil: The epidemic beyond the pandemic. World J Psychiatry. 2022;12:766-769. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 234. | Garrido R, Paloma V, Benítez I, Skovdal M, Verelst A, Derluyn I. Impact of COVID-19 pandemic on the psychological well-being of migrants and refugees settled in Spain. Ethn Health. 2023;28:257-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 235. | Salerno JP, Boekeloo BO. LGBTQ Identity-Related Victimization During COVID-19 Is Associated with Moderate to Severe Psychological Distress Among Young Adults. LGBT Health. 2022;9:303-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 236. | Abreu RL, Barrita AM, Martin JA, Sostre J, Gonzalez KA. Latinx LGBTQ Youth, COVID-19, and Psychological Well-Being: A Systematic Review. J Clin Child Adolesc Psychol. 2024;53:98-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 237. | Ahmad A, Mueller C, Tsamakis K. Covid-19 pandemic: a public and global mental health opportunity for social transformation? BMJ. 2020;369:m1383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 238. | Nielsen M, Levkovich N. COVID-19 and mental health in America: Crisis and opportunity? Fam Syst Health. 2020;38:482-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 239. | Shim RS, Starks SM. COVID-19, Structural Racism, and Mental Health Inequities: Policy Implications for an Emerging Syndemic. Psychiatr Serv. 2021;72:1193-1198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 59] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 240. | Fountoulakis KN, Karakatsoulis G, Abraham S, Adorjan K, Ahmed HU, Alarcón RD, Arai K, Auwal SS, Berk M, Bjedov S, Bobes J, Bobes-Bascaran T, Bourgin-Duchesnay J, Bredicean CA, Bukelskis L, Burkadze A, Abud IIC, Castilla-Puentes R, Cetkovich M, Colon-Rivera H, Corral R, Cortez-Vergara C, Crepin P, De Berardis D, Zamora Delgado S, De Lucena D, De Sousa A, Stefano RD, Dodd S, Elek LP, Elissa A, Erdelyi-Hamza B, Erzin G, Etchevers MJ, Falkai P, Farcas A, Fedotov I, Filatova V, Fountoulakis NK, Frankova I, Franza F, Frias P, Galako T, Garay CJ, Garcia-Álvarez L, García-Portilla MP, Gonda X, Gondek TM, González DM, Gould H, Grandinetti P, Grau A, Groudeva V, Hagin M, Harada T, Hasan MT, Hashim NA, Hilbig J, Hossain S, Iakimova R, Ibrahim M, Iftene F, Ignatenko Y, Irarrazaval M, Ismail Z, Ismayilova J, Jacobs A, Jakovljević M, Jakšić N, Javed A, Kafali HY, Karia S, Kazakova O, Khalifa D, Khaustova O, Koh S, Kopishinskaia S, Kosenko K, Koupidis SA, Kovacs I, Kulig B, Lalljee A, Liewig J, Majid A, Malashonkova E, Malik K, Malik NI, Mammadzada G, Mandalia B, Marazziti D, Marčinko D, Martinez S, Matiekus E, Mejia G, Memon RS, Martínez XEM, Mickevičiūtė D, Milev R, Mohammed M, Molina-López A, Morozov P, Muhammad NS, Mustač F, Naor MS, Nassieb A, Navickas A, Okasha T, Pandova M, Panfil AL, Panteleeva L, Papava I, Patsali ME, Pavlichenko A, Pejuskovic B, Pinto Da Costa M, Popkov M, Popovic D, Raduan NJN, Ramírez FV, Rancans E, Razali S, Rebok F, Rewekant A, Flores ENR, Rivera-Encinas MT, Saiz P, de Carmona MS, Martínez DS, Saw JA, Saygili G, Schneidereit P, Shah B, Shirasaka T, Silagadze K, Sitanggang S, Skugarevsky O, Spikina A, Mahalingappa SS, Stoyanova M, Szczegielniak A, Tamasan SC, Tavormina G, Tavormina MGM, Theodorakis PN, Tohen M, Tsapakis EM, Tukhvatullina D, Ullah I, Vaidya R, Vega-Dienstmaier JM, Vrublevska J, Vukovic O, Vysotska O, Widiasih N, Yashikhina A, Prezerakos PE, Smirnova D. Results of the COVID-19 mental health international for the general population (COMET-G) study. Eur Neuropsychopharmacol. 2022;54:21-40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 94] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 241. | Silva-Valencia J, Lapadula C, Westfall JM, Gaona G, de Lusignan S, Kristiansson RS, Ling ZJ, Goh LH, Soto-Becerra P, Cuba-Fuentes MS, Wensaas KA, Flottorp S, Baste V, Chi-Wai Wong W, Pui Ng AP, Ortigoza A, Manski-Nankervis JA, Hallinan CM, Zingoni P, Scattini L, Heald A, Tu K; INTRePID. Effect of the COVID-19 pandemic on mental health visits in primary care: an interrupted time series analysis from nine INTRePID countries. EClinicalMedicine. 2024;70:102533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 14] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 242. | Bhugra D, Tasman A, Pathare S, Priebe S, Smith S, Torous J, Arbuckle MR, Langford A, Alarcón RD, Chiu HFK, First MB, Kay J, Sunkel C, Thapar A, Udomratn P, Baingana FK, Kestel D, Ng RMK, Patel A, Picker L, McKenzie KJ, Moussaoui D, Muijen M, Bartlett P, Davison S, Exworthy T, Loza N, Rose D, Torales J, Brown M, Christensen H, Firth J, Keshavan M, Li A, Onnela JP, Wykes T, Elkholy H, Kalra G, Lovett KF, Travis MJ, Ventriglio A. The WPA-Lancet Psychiatry Commission on the Future of Psychiatry. Lancet Psychiatry. 2017;4:775-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 221] [Article Influence: 24.6] [Reference Citation Analysis (0)] |
| 243. | Fitzgerald CA, Vaidyanathan B. Faith Leaders' Views on Collaboration with Mental Health Professionals. Community Ment Health J. 2023;59:477-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 244. | Cooper M, Evans Y, Pybis J. Interagency collaboration in children and young people's mental health: a systematic review of outcomes, facilitating factors and inhibiting factors. Child Care Health Dev. 2016;42:325-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 69] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 245. | Irarrazaval M, Norambuena P, Montenegro C, Toro-Devia O, Vargas B, Caqueo-Urízar A. Public Policy Responses to Address the Mental Health Consequences of the COVID-19 Pandemic: Evidence From Chile. Front Public Health. 2021;9:590335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/