Published online Oct 19, 2025. doi: 10.5498/wjp.v15.i10.108590
Revised: July 9, 2025
Accepted: July 21, 2025
Published online: October 19, 2025
Processing time: 108 Days and 0.4 Hours
The hospice care system of traditional Chinese medicine (TCM) provides a reference for relieving depression, anxiety, and sleep disorders in patients with advanced cancer.
To explore the effects of TCM hospice care on depression, anxiety, and sleep disorders in patients with advanced cancer.
This prospective study was conducted between July 2023 and June 2024. Patients with advanced cancer were selected and divided into observation and control groups (n = 34 per group). The observation group received TCM hospice care, with a 4-week treatment cycle. The control group received routine hospice care. The Hamilton Depression Rating Scale, Hamilton Self-Rating Anxiety Scale, and Pittsburgh Sleep Quality Index were used to assess depression, anxiety, and sleep quality changes, and Statistical Package for the Social Sciences 26.0 was used for data analysis.
No significant differences were found in age, sex, cancer type, disease course, or baseline mental symptom scores between the groups (P > 0.05). After treatment, the observation group showed significantly greater improvements in depression, anxiety, and sleep quality (P < 0.05). The depression, anxiety, and sleep scores in the observation group decreased to 7.21 ± 2.48, 6.12 ± 2.39, and 4.53 ± 1.89, respectively. In the control group, these scores decreased to 11.42 ± 3.12, 10.14 ± 3.21, and 6.21 ± 1.79. The observation group demonstrated superior efficacy (P < 0.05). Depression, anxiety, and sleep quality were significantly positively correlated (P < 0.05). Logistic regression analysis identified the TCM hospice care system as an independent factor improving patients’ health.
The TCM hospice care system effectively improves depression, anxiety, and sleep disorders in patients with advanced cancer, offering comprehensive care suitable for clinical promotion and application.
Core Tip: This study highlights the clinical value of integrating a traditional Chinese medicine (TCM) hospice care system into the management of patients with advanced cancer. The results demonstrate that TCM-based interventions significantly alleviate depression, anxiety, and sleep disorders compared to conventional hospice care. By incorporating psychological support, TCM nursing techniques, and individualized symptom relief strategies, this approach offers a holistic and culturally resonant model of palliative care. The findings provide a practical reference for nursing programs and emphasize the potential of TCM hospice care in improving quality of life and emotional well-being in terminally ill cancer patients.
- Citation: Liu L, Xiao AQ, Cui XM, Jiang X, Zhou LD, Meng Q, Cai ZY, Ma Y, Liao RY. Integrating a traditional Chinese medicine hospice care system to address depression, anxiety, and sleep disorders in advanced cancer. World J Psychiatry 2025; 15(10): 108590
- URL: https://www.wjgnet.com/2220-3206/full/v15/i10/108590.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i10.108590
Patients with advanced cancer often face multiple mental and physiological challenges, such as severe pain, treatment-related side effects, and uncertainty about survival. These factors substantially affect the quality of life of patients[1]. Depression, anxiety, and sleep disorders, which are common mental symptoms in patients with advanced cancer, not only aggravate the patient’s condition but also have a profound effect on their physical and mental health and quality of life[2]. Therefore, timely and effective intervention for these symptoms to improve the mental state is essential to improving the overall treatment effect and quality of life of patients with advanced cancer[3]. Although modern medical treatments have made notable progress in the early diagnosis and treatment of cancer, it still faces many challenges in the comprehensive treatment of patients with advanced cancer[4]. Traditional antidepressants, anxiolytics, and sedative-hypnotics are often accompanied by side effects and fail to fundamentally improve overall health[5]. Therefore, identifying a more comprehensive and personalized treatment without serious side effects has become the focus of current research. As a treatment mode that focuses on physical and mental integration, the traditional Chinese medicine (TCM) hospice care system has demonstrated good clinical efficacy in alleviating the symptoms of patients with advanced cancer and improving their quality of life[6]. In TCM, treatment based on syndrome differentiation is emphasized, and personalized interventions such as acupuncture, massage, herbal medicine, Qigong, and dietary conditioning are adopted according to the patients’ specific symptoms, physical fitness, and condition changes, to regulate their physiological and mental state[7]. The hospice care system combines the advantages of TCM theory and modern medicine, proposing a more systematic intervention framework that prioritizes both pain control and patient mental state adjustment[8]. This comprehensive treatment mode reduces depression, anxiety, and sleep disorders in patients with cancer, improves their overall quality of life, and enhances disease resistance and self-regulation[9]. Therefore, this study explored the specific intervention effects of the TCM hospice care system on depression, anxiety, and sleep disorders in patients with advanced cancer through a prospective design to provide novel insights and methods for clinical treatment, theoretical support, and a practical basis for the overall care of patients with advanced cancer.
This prospective study was conducted at our hospital between July 2023 and June 2024. All participants agreed to participate in the study and signed an informed consent form. Patients who met the inclusion criteria for advanced cancer were selected and divided into observation and control groups, with 34 patients in each group. The two groups were patients with advanced cancer receiving hospice care: (1) The observation group received TCM hospice care system intervention; and (2) The control group received routine hospice care.
Male or female patients aged 18-75 years were included. Advanced cancer was diagnosed at primary sites, including gastric, lung, liver, colorectal, breast, esophageal, and pancreatic cancer, as well as other solid tumors. The cancer was stage III or IV with no pathological limitations. Self-rating scales, such as the Hamilton Depression Rating Scale (HAMD), Hamilton Self-Rating Anxiety Scale (HAMA), and Pittsburgh Sleep Quality Index (PSQI), were used for initial screening if patients had symptoms of depression, anxiety, or sleep disorders. The expected survival period was longer than 3 months, and the patients showed good cooperative intentions.
Patients with severe systemic diseases, such as cardiovascular disease and liver and kidney failure, who could not tolerate treatment, were excluded. Patients with severe cognitive disorders, mental disorders, and other mental diseases cannot cooperate with treatment. A patient was excluded if they had been treated in other clinical trials and received various drugs or treatment measures that may have influenced the research results. Pregnant and lactating women were excluded. Patients with acute infectious diseases or other diseases that did not meet the purpose of this study were also excluded. Finally, 34 patients who met the inclusion criteria were randomly assigned to the observation or control group. No significant differences were noted in the basic data, including age, sex, cancer type, disease course, or mental symptom score, between the two groups, indicating good comparability (Table 1).
| Data | Observation (n = 34) | Control (n = 34) | t value | P value |
| Age (years) | 58.21 ± 10.31 | 57.59 ± 9.79 | 0.31 | 0.754 |
| Sex (male/female) | 18 (52.94)/16 (47.06) | 17(50.00)/17 (50.00) | 0.037 | 0.848 |
| Cancer type | 0.964 | 0.809 | ||
| Gastric | 10 (29.41) | 11 (32.35) | ||
| Lung | 12 (35.29) | 11 (32.35) | ||
| Liver | 8 (23.53) | 6 (17.65) | ||
| Others | 4 (11.76) | 6 (17.65) | ||
| Disease course (months) | 18.31 ± 8.23 | 19.06 ± 7.64 | 0.556 | 0.58 |
| Depression score | 15.38 ± 3.21 | 15.59 ± 3.08 | 0.184 | 0.854 |
| Anxiety score | 14.84 ± 3.51 | 14.74 ± 3.30 | 0.135 | 0.893 |
| Sleep quality score | 8.61 ± 2.11 | 8.53 ± 2.01 | 0.176 | 0.861 |
| Preoperative infection indicators (procalcitonin, ng/mL) | 0.32 ± 0.15 | 0.34 ± 0.17 | 0.542 | 0.591 |
The patients in the observation group received comprehensive intervention from the Chinese medicine hospice care system, including four primary treatment methods: (1) Chinese medicine; (2) Acupuncture and moxibustion; (3) Massage; and (4) Psychological counseling. Each treatment method was designed according to the patient’s constitution, condition, and specific needs. TCM uses the “Anshen Zhentong Formula” for intervention, which mainly consists of medicinal herbs such as Chaihu, Huangqin, Danggui, Baishao, and Licorice. Chaihu soothes the liver, relieves depression, harmonizes qi and blood, and is commonly used to treat anxiety and depression. Huangqin clears and detoxifies heat to calm the mind. Danggui promotes blood circulation, replenishes blood, and regulates insomnia and anxiety caused by insufficient qi and blood. White peony relieves muscle spasms and improves tension and anxiety. Licorice has calming and harmonizing effects that enhance the efficacy of other drugs. The total daily dose was 20 g (adjusted according to each patient’s condition). The “Anshen Analgesic Formula” is composed of Chaihu, Huangqin, Danggui, Baishao, and Licorice. The medicinal herbs were weighed according to the prescribed amounts (Chaihu 10 g, Huangqin 10 g, Danggui 12 g, Baishao 15 g, and Licorice 6 g), and then soaked in cold water for 30 minutes. Water was then added to cover the medicinal herbs by 3-5 cm, boiled over high heat, then turned to low heat and boiled for 20-30 minutes, filtered, and the juice was collected. Water was added a second time to cover 2-3 cm of the medicine residue, simmered over low heat for 15-20 minutes, and then filtered. Afterward, the two filtrates were combined and concentrated to a volume of 200 mL. The patient received one daily dose, divided into morning and evening doses. The dosage was adjusted according to the patient’s physical condition (e.g., reducing Chaihu 8 g and Huangqin 6 g for individuals with weak physical conditions). The main component of Chaihu, saikosaponin, alleviates depression by regulating the hypothalamic-pituitary-adrenal (HPA) axis, while inhibiting the release of inflammatory factors, such as tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6), and exerting anti-inflammatory and analgesic effects[10]. Chaihu extract improves depressive behavior in chronic stress model rats, and its mechanism is related to increased serotonin and norepinephrine levels in the brain[11]. The active ingredient of Scutellaria baicalensis, baicalin, has significant anti-anxiety effects and can alleviate neuroinflammation by inhibiting the nuclear factor kappa B (NF-κB) signaling pathway, while regulating the gamma aminobutyric acid (GABA) system to improve sleep[10]. In vitro experiments have demonstrated that baicalin can cross the blood-brain barrier, inhibit microglial activation, and reduce the expression of pro-inflammatory cytokines[11]. Patients received one daily dose, divided into morning and evening doses. If a patient has a weak constitution or special needs, the dose was adjusted appropriately according to the individual’s situation. The medicinal herbs were boiled in water twice, and the filtrates were combined. They were administered in the morning and evening. Acupuncture and moxibustion treatments were performed in combination with ear and body acupuncture, primarily by stimulating specific points to alleviate anxiety and depression symptoms, improve sleep quality, and relieve pain. Acupuncture and moxibustion treatment combines ear and body acupuncture, with specific anatomical positioning and stimulation intensity. For body acupuncture, Baihui (GV20) is located at the center of the head, approximately 5 cm above the hairline, and is punctured subcutaneously at a depth of 0.5-0.8 cun (1.5-2.5 cm) with a twisting manipulation (180° rotation, 60 times/minute) to induce local soreness; Fengchi (GB20) is positioned in the depression between the sternocleidomastoid and trapezius muscles below the occipital bone, punctured obliquely toward the opposite eye at 0.8-1.2 cun (2.5-4 cm) with lifting-thrusting and twisting (80 times/minute); Shenmen (HT7) is located in the ulnar depression of the flexor carpi ulnaris tendon at the distal wrist crease, punctured straight at 0.3-0.5 cun (1-1.5 cm) with reinforcing twisting (90° rotation, 40 times/minute). For ear acupuncture, the Shenmen point is located in the postero-superior triangular fossa of the concha, punctured vertically at 0.1-0.2 cun with light twisting. In contrast, the Endocrine point is located at the bottom of the cymba conchae within the intertragic notch, punctured obliquely with moderate twisting. These operations follow standardized depths and techniques to ensure safety and efficacy, aligning with prior research on the regulatory effects of acupuncture on the HPA axis[11]. Each acupuncture and moxibustion treatment lasted for 30 minutes, three times a week, for a total of 4 weeks. The body needle employs a conventional acupuncture method, and the selection and depth of acupoints are adjusted according to the patient’s specific situation. Ear acupuncture achieves the effect of unblocking meridians and regulating emotions by accurately locating ear acupoints and stimulating the relevant areas. Tuina therapy utilizes traditional Chinese massage techniques to unblock meridians, harmonize qi and blood, and help patients enhance their physical and mental well-being. Using kneading, pushing, and pressing techniques, the focus is on massaging the shoulders, back, neck, waist, and other areas to relieve muscle tension and spasms and help patients relax. Local massage is performed on areas of the body that are painful, such as the neck, shoulders, back, and waist, to relieve tension and discomfort. By massaging the entire body, qi and blood levels are regulated, fatigue is relieved, and sleep quality is improved. Each massage treatment lasted 40 minutes and was administered twice a week, for 4 weeks. Psychological counseling aims to help patients reduce emotional stress and improve their depression and anxiety through communication. Listening to patients’ emotions and psychological appeals helps them express their inner confusion and pain. Therapists provide appropriate emotional support, psychological counseling, and stress management techniques based on the patient’s psychological state to help alleviate emotional stress and improve their psychological state. Common methods include cognitive behavioral therapy, emotion regulation techniques, and relaxation training. Each psychological counseling session lasted 20 minutes. The psychological counseling was conducted once a week for 4 weeks.
The patients in the control group received routine hospice care, including symptomatic treatment, analgesic drugs, and mental support. Patients received routine analgesic drug therapy, including morphine hydrochloride sustained-release tablets at a dose of 10 mg twice a day, and the dose was appropriately adjusted according to the degree of pain. According to the patient’s condition, if severe pain existed, fentanyl patches (remifentanil patches) were used, and each patch was changed every 72 hours. The dose was adjusted according to the degree of pain experienced by the patients. Routine mental counseling and spiritual care were provided, and patients were encouraged to communicate with nurses or psychologists on a weekly basis to help them manage their emotions and alleviate stress. Patients received routine clinical treatments, including nutritional support and antibiotic therapy, tailored to their specific symptoms. Specific drugs and doses were adjusted according to the conditions.
Clinical symptoms: Clinical symptoms primarily include pain, appetite change, and weight change, and depression and anxiety symptoms were monitored. Pain was assessed using a visual analog scale (VAS) based on the patient’s self-report and physician’s assessment. The VAS scores range from 0 to 10 points, with 0 indicating no pain and 10 indicating severe pain; scores of 0-3 indicate mild pain; 4-6 points indicate moderate pain; and 7-10 points indicate severe pain. Patients’ appetite and body weight changes were used as key indicators for clinical observation. The appetite score ranged from 0 (no appetite) to 4 (normal appetite), and body weight change was assessed based on monthly weight gain or loss of > 5%. The patients were evaluated after 4 weeks of treatment and at the end of the treatment.
Depression and anxiety: The mental state was assessed by quantitative analysis using the HAMD and the HAMA. Total HAMD scores ranging from 0 to 7 were normal. A total score of 8-13 indicates mild depression, and a score of 14-18 indicates moderate depression. A total score of 19 or higher indicates severe depression. A total HAMA score of 0-7 indicates no anxiety, with a score of 8-14 indicating mild anxiety. A total score of 15-20 indicates moderate anxiety, and severe anxiety is indicated by a score of 21 or higher. The patients were evaluated after 4 weeks of treatment and at the end of the treatment.
Sleep quality: Sleep quality was assessed using the PSQI scale. PSQI scores ranged from 0 to 21. Higher scores indicated poorer sleep quality. Scores of 0-5 indicate good sleep quality. A total score of 6-10 indicates a mild sleep disorder. A total core of 11-15 indicates moderate sleep disorders, with a total score of 16-21 representing severe sleep disorders. According to their self-evaluation and doctor feedback, each patient was required to complete the PSQI scale to reflect changes in sleep quality before and after treatment. The patients were evaluated after 4 weeks of treatment and at the end of the treatment.
Biochemical index analysis: To evaluate the effect of treatment on the physiological state of patients, serum C-reactive protein (CRP), carcinoembryonic antigen (CEA), and white blood cell (WBC) counts were measured. All specimens were collected from venous blood and analyzed using enzyme-linked immunosorbent assay (ELISA) and an automated biochemical analyzer. Blood samples were collected from the enrolled patients after 4 weeks of treatment and at the end of treatment. CRP levels were measured using a Beda Biological CRP Kit (model: CRP-Bio500) and quantified using ELISA. The specific operations included preparing reagents according to the kit instructions, adding samples, and measuring absorbance after incubation for 30 minutes. The Roche chemiluminescence kit (model: Electra CEA 1) was used to determine CEA levels using a Lumine × 200 chemiluminescence analyzer (United States). An automatic hematology analyzer (Cobas 8000; Roche, Basel, Switzerland) was used to automatically calculate the WBC count.
Monitoring of blood pressure and body temperature: The blood pressure and body temperature of each patient were measured at the beginning of treatment, after 4 weeks of treatment, and at the end of treatment. An Ohm sphygmomanometer (HEM-7203, Japan) and a Mack thermometer (MDT-300, United States) were used. The patient was asked to sit still for 5 minutes before taking the blood pressure measurements. Temperature measurement requires the patient to be in a normal-temperature environment. Electrocardiography (ECG) was performed using a Philips electrocardiograph (Pagewriter TC70). Monitoring included changes in heart rate (HR) and ECG waveforms, which encompassed P-wave, QRS-wave, and T-wave morphology, as well as ST-segment changes. Abnormal waveforms or arrhythmias such as tachycardia, bradycardia, and atrial fibrillation were recorded. The patients were monitored after 4 weeks of treatment and at the end of the treatment.
Statistical analysis was performed using IBM Statistical Package for the Social Sciences Statistics for Windows, version 26.0. Measurement data were expressed as the mean ± SD, enumeration data were expressed as frequency and percentage, and intra-group comparisons were performed using the t-test and χ2 test. An independent sample t-test or analysis of variance was used for comparison between groups. Non-normally distributed data were expressed as medians (quartiles) [M (P25, P75)], and inter-group comparisons were made using the Mann-Whitney U test or Kruskal-Wallis H test. Pearson’s correlation analysis was performed on the different variables during treatment to evaluate the correlation between the indicators before and after treatment. Correlation coefficients between different clinical indicators, such as depression, anxiety, and sleep quality scores, were calculated to assess whether a significant linear correlation existed, with r ≥ 0.9 indicating an extremely strong positive correlation, 0.7 ≤ r < 0.9 indicating a strong correlation, 0.5 ≤ r < 0.7 indicating a moderate correlation, and r < 0.5 indicating a weak or no correlation. To further explore the independent factors affecting depression, anxiety, and sleep quality, logistic regression analysis was used to analyze the influence of the clinical characteristics, mental state, and treatment method of patients before and after treatment. The treatment effect was considered as the dependent variable, and other clinical indicators and treatment methods were used as independent variables. The regression coefficients [odds ratio (OR)] and 95%CI were determined. An OR > 1 indicated that a factor contributed to the therapeutic effect, whereas an OR < 1 indicated that a factor was negatively correlated with the therapeutic effect. All statistical tests were performed bilaterally, and P < 0.05 indicated that the difference was significant.
The observation group showed significant improvement in various clinical symptoms during the treatment, especially regarding pain, appetite, weight, depression, and anxiety (P < 0.05). Although some improvement was observed in the control group, the improvement was smaller, with a mild effect (Table 2).
| Clinical symptoms | Group | Before treatment | 4 weeks after treatment | After treatment | t value | P value |
| Pain (points) | Observation | 7.68 ± 1.24 | 5.43 ± 1.02 | 3.21 ± 0.89 | 12.526 | < 0.001 |
| Control | 7.72 ± 1.30 | 6.28 ± 1.15 | 5.04 ± 1.07 | 8.684 | 0.004 | |
| Appetite score (points) | Observation | 1.68 ± 0.88 | 2.54 ± 0.79 | 3.12 ± 0.66 | 14.332 | < 0.001 |
| Control | 1.74 ± 0.84 | 2.11 ± 0.76 | 2.53 ± 0.79 | 5.032 | 0.027 | |
| Weight change (kg) | Observation | -4.32 to 2.02 | -1.34 to 1.22 | 0.87 ± 1.09 | 15.927 | < 0.001 |
| Control | -4.22 to 2.15 | -2.12 to 1.34 | -0.65 to 1.15 | 6.876 | 0.009 | |
| Hamilton Depression Rating Scale (points) | Observation | 21.13 ± 4.23 | 15.08 ± 3.45 | 9.63 ± 2.89 | 19.624 | < 0.001 |
| Control | 21.08 ± 4.45 | 17.47 ± 3.89 | 12.02 ± 3.28 | 8.912 | 0.003 | |
| Hamilton Self-Rating Anxiety Scale (points) | Observation | 19.62 ± 3.98 | 14.74 ± 3.12 | 9.31 ± 2.48 | 18.045 | < 0.001 |
| Control | 19.74 ± 4.02 | 16.62 ± 3.76 | 12.54 ± 3.12 | 7.124 | 0.008 |
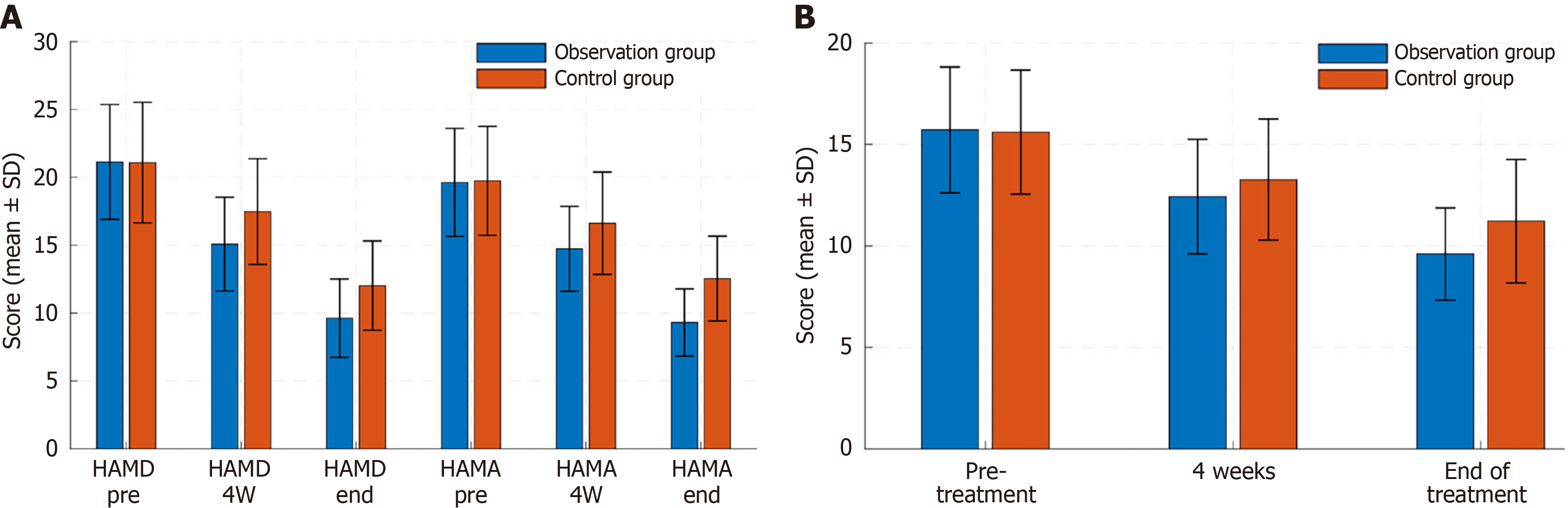
Both the observation and control groups showed significant improvements during treatment. The HAMD and HAMA scores of the observation group significantly decreased after four weeks of treatment and at the end of treatment (P < 0.05). The control group also showed significant improvements in HAMD and HAMA scores at the end of treatment (P < 0.05; Table 3, Figure 1A).
| Indicators | Group | Before treatment | 4 weeks after treatment | After treatment | t value | P value |
| Hamilton Depression Rating Scale (points) | Observation | 21.13 ± 4.23 | 15.08 ± 3.45 | 9.63 ± 2.89 | 19.624 | < 0.001 |
| Control | 21.08 ± 4.45 | 17.47 ± 3.89 | 12.02 ± 3.28 | 8.912 | 0.003 | |
| Hamilton Self-Rating Anxiety Scale (points) | Observation | 19.62 ± 3.98 | 14.74 ± 3.12 | 9.31 ± 2.48 | 18.045 | < 0.001 |
| Control | 19.74 ± 4.02 | 16.62 ± 3.76 | 12.54 ± 3.12 | 7.124 | 0.008 |
The sleep quality of patients in the observation group improved significantly after treatment. The PSQI scores after four weeks of treatment and at the end of treatment were 12.43 ± 2.82 and 9.61 ± 2.27, respectively, which were significantly lower than before treatment (15.72 ± 3.10; P < 0.05). Sleep quality also improved in the control group; however, the improvement was not significant (P < 0.05; Table 4, Figure 1B).
| Group | Before treatment | 4 weeks after treatment | After treatment | t value | P value |
| Observation | 15.72 ± 3.10 | 12.43 ± 2.82 | 9.61 ± 2.27 | 12.581 | < 0.001 |
| Control | 15.61 ± 3.05 | 13.27 ± 2.98 | 11.22 ± 3.04 | 6.298 | 0.002 |
The CRP, CEA, and WBC levels of the observation group decreased significantly after treatment (P < 0.05). In the control group, an improvement was also observed; however, the change in amplitude was small, and the difference was only significant for CRP and CEA (P < 0.05; Table 5).
| Indicators | Group | Before treatment | 4 weeks after treatment | After treatment | t value | P value |
| C-reactive protein (mg/L) | Observation | 45.60 ± 12.34 | 35.80 ± 9.12 | 25.50 ± 8.03 | 13.578 | < 0.001 |
| Control | 45.45 ± 12.15 | 40.30 ± 10.57 | 33.40 ± 9.45 | 8.692 | 0.003 | |
| Carcinoembryonic antigen (ng/mL) | Observation | 10.80 ± 3.25 | 8.12 ± 2.98 | 5.30 ± 2.14 | 11.945 | < 0.001 |
| Control | 10.75 ± 3.12 | 9.20 ± 3.01 | 7.80 ± 2.77 | 6.423 | 0.004 | |
| White blood cell (× 109/L) | Observation | 7.62 ± 2.14 | 6.58 ± 1.93 | 5.46 ± 1.75 | 10.132 | < 0.001 |
| Control | 7.59 ± 2.10 | 7.02 ± 2.04 | 6.44 ± 2.01 | 5.211 | 0.019 |
During treatment, systolic blood pressure, diastolic blood pressure, and body temperature of the observation group significantly decreased. At the end of treatment, all indicators had changed significantly (P < 0.05). Patients in the control group also showed improvement, although it was relatively small, and all indicators were significant (P < 0.05; Table 6).
| Indicators | Group | Before treatment | 4 weeks after treatment | After treatment | t value | P value |
| Systolic blood pressure (mmHg) | Observation | 135.80 ± 14.25 | 130.40 ± 12.58 | 125.30 ± 11.34 | 4.315 | < 0.001 |
| Control | 137.00 ± 15.13 | 134.50 ± 13.87 | 132.80 ± 12.92 | 3.291 | 0.006 | |
| Diastolic blood pressure (mmHg) | Observation | 85.20 ± 8.45 | 80.60 ± 7.32 | 78.30 ± 7.01 | 3.824 | 0.001 |
| Control | 86.00 ± 9.12 | 84.70 ± 8.97 | 82.50 ± 8.12 | 2.574 | 0.02 | |
| Temperature (°C) | Observation | 37.10 ± 0.52 | 36.80 ± 0.43 | 36.60 ± 0.40 | 4.015 | < 0.001 |
| Control | 37.20 ± 0.47 | 37.00 ± 0.40 | 36.90 ± 0.39 | 3.212 | 0.009 |
During the treatment period, the HR and incidence of arrhythmia and atrial fibrillation significantly improved in the observation group (P < 0.05), whereas the improvement in the control group was slow, with only a significant decrease in the incidence of arrhythmia (P < 0.05). Overall, the improvement in the observation group was significantly greater than that in the control group (Table 7).
| Indicators | Group | Before treatment | 4 weeks after treatment | After treatment | χ²/t | P value |
| Heart rate (beats/minute) | Observation | 84.50 ± 10.23 | 75.30 ± 9.41 | 72.10 ± 8.12 | 5.762 | < 0.001 |
| Control | 85.00 ± 9.98 | 80.20 ± 9.12 | 78.50 ± 8.92 | 3.411 | 0.006 | |
| Incidence of arrhythmia | Observation | 6/34 (17.65%) | 3/34 (8.82%) | 1/34 (2.94%) | 9.213 | < 0.001 |
| Control | 5/34 (14.71%) | 4/34 (11.76%) | 3/34 (8.82%) | 2.531 | 0.038 | |
| Incidence of atrial fibrillation | Observation | 3/34 (8.82%) | 1/34 (2.94%) | 1/34 (2.94%) | 5.204 | 0.023 |
| Control | 2/34 (5.88%) | 1/34 (2.94%) | 1/34 (2.94%) | 2.013 | 0.156 |
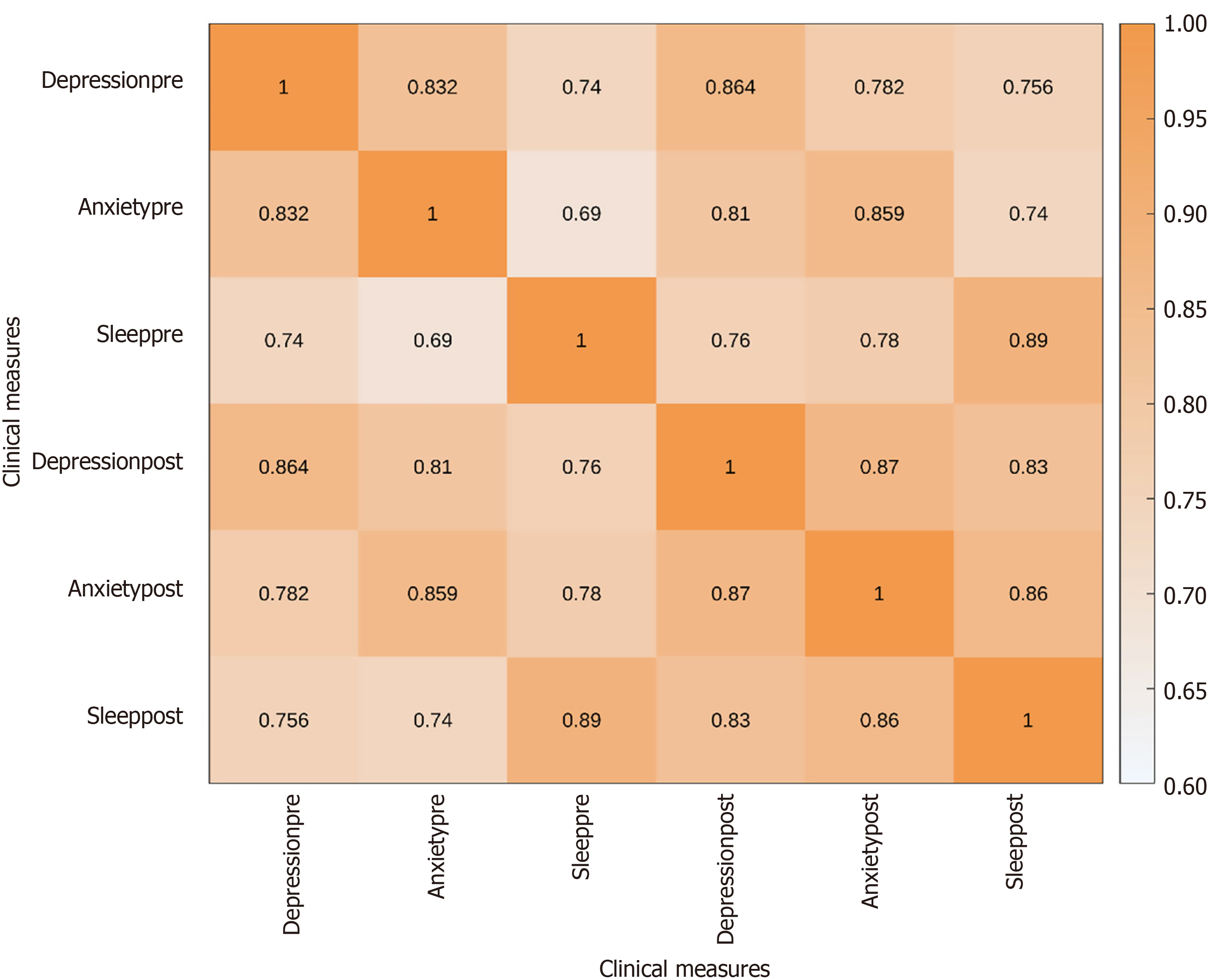
Pearson correlation analysis showed a significant positive correlation between depression, anxiety, and sleep quality scores. Depression scores were strongly correlated with anxiety (r = 0.832) and sleep quality scores (r = 0.740) before and after treatment. The correlation was further enhanced after treatment, indicating that the treatment resulted in a significant improvement in various clinical indicators (Table 8, Figure 2).
| Variable | Depression score (before treatment) | Anxiety score (before treatment) | Sleep quality score (before treatment) | Depression score (after treatment) | Anxiety score (after treatment) | Sleep quality score (after treatment) |
| Depression score (before treatment) | 1 | 0.832 | 0.74 | 0.864 | 0.782 | 0.756 |
| Anxiety score (before treatment) | 0.832 | 1 | 0.69 | 0.81 | 0.859 | 0.74 |
| Sleep quality score (before treatment) | 0.74 | 0.69 | 1 | 0.76 | 0.78 | 0.89 |
| Depression score (after treatment) | 0.864 | 0.81 | 0.76 | 1 | 0.87 | 0.83 |
| Anxiety score (after treatment) | 0.782 | 0.859 | 0.78 | 0.87 | 1 | 0.86 |
| Sleep quality score (after treatment) | 0.756 | 0.74 | 0.89 | 0.83 | 0.86 | 1 |
The results of the logistic regression analysis showed that the number of clinical symptoms (OR = 1.729, P = 0.021), depression score (before treatment) (OR = 1.577, P = 0.015), and treatment method (observation group) had a significant impact on the treatment effect (OR = 3.826, P = 0.011), and they were positively correlated with the treatment effect. The effects of blood pressure, body temperature, and HR after treatment were not significant, indicating that these factors only weakly predicted the treatment effect (Table 9).
| Factor | β | SE | χ² | P value | Odds ratio | 95%CI |
| Constant term | -2.315 | 0.867 | 7.214 | 0.007 | 0.098 | 0.012-0.768 |
| Number of clinical symptoms | 0.547 | 0.239 | 5.335 | 0.021 | 1.729 | 1.078-2.788 |
| Depression score (before treatment) | 0.455 | 0.188 | 5.892 | 0.015 | 1.577 | 1.091-2.277 |
| Anxiety score (before treatment) | 0.369 | 0.214 | 3.02 | 0.082 | 1.446 | 0.948-2.213 |
| Sleep quality score (before treatment) | 0.291 | 0.201 | 2.107 | 0.146 | 1.338 | 0.895-2.002 |
| Treatment method (observation group) | 1.342 | 0.756 | 3.253 | 0.011 | 3.826 | 0.997-15.516 |
| Blood pressure (before treatment, systolic) | 0.002 | 0.005 | 0.251 | 0.616 | 1.002 | 0.993-1.011 |
| Blood pressure (before treatment, diastolic) | 0.004 | 0.004 | 1.056 | 0.304 | 1.004 | 0.996-1.013 |
| Body temperature (before treatment) | -0.023 | 0.023 | 1.014 | 0.314 | 0.977 | 0.933-1.023 |
| Heart rate (before treatment) | -0.031 | 0.015 | 4.036 | 0.045 | 0.97 | 0.935-1.007 |
| Heart rate (after treatment) | 0.029 | 0.018 | 2.483 | 0.115 | 1.03 | 0.994-1.067 |
This study explored the interventional effects of the TCM hospice care system on depression, anxiety, and sleep disorders in patients with advanced cancer. Patients in the observation group who received the TCM hospice care system intervention showed significant improvements in depression, anxiety, and sleep quality, suggesting that the TCM hospice care system had significant advantages in relieving the mental symptoms of patients with advanced cancer and improving their quality of life. Depression, anxiety, and sleep disorders are common mental symptoms in patients with advanced cancer owing to severe pain, treatment-related side effects, and uncertainty about survival time, which also aggravates physical discomfort[12,13]. In modern medicine, conventional antidepressants, anxiolytics, and sedative-hypnotics can alleviate some symptoms in a short period; however, they often have side effects and cannot fundamentally improve the overall health of patients[14]. Currently, the advantages of TCM hospice care systems are becoming increasingly significant. The treatment in TCM emphasizes “treatment based on syndrome differentiation”, comprehensively regulating the physical and mental states of patients through individualized treatment programs, such as TCM, acupuncture, and massage[15]. TCM can improve depression, anxiety, and sleep disorders in patients with few side effects by regulating qi and blood, dredging meridians and collaterals, and adjusting yin and yang[16,17]. In this study, patients in the observation group received comprehensive treatment measures including acupuncture, massage, and TCM interventions. This treatment model plays a pivotal role in alleviating depression and anxiety symptoms[18]. Specifically, acupuncture and moxibustion relieve pain, improve sleep quality, and regulate emotions by stimulating specific acupoints, such as Baihui (GV 20), Fengchi (GB 20), and Shenmen (HT 7)[19]. Acupuncture has a significant regulatory effect on the HPA axis, a key neuroendocrine pathway involved in stress responses and mood regulation. Stimulation of acupoints such as Baihui (GV 20) and Shenmen (HT 7) inhibits excessive HPA axis activation in patients with advanced cancer, reduces glucocorticoid levels, and mitigates stress-induced immune suppression. Mechanistically, acupuncture modulates the central nervous system via ascending afferent signals from acupoints, which activate the limbic system (e.g., amygdala and hippocampus) and suppress corticotrophin-releasing hormone secretion in the hypothalamus. This downregulates the release of adrenocorticotropic hormone and cortisol, thereby alleviating the glucocorticoid-mediated suppression of T lymphocytes and natural killer cells. Regular acupuncture decreases serum cortisol levels in patients with depression and improves HAMD scores. In this study, the reduced anxiety and improved sleep quality in the observation group may partially result from HPA axis normalization, as evidenced by decreased CRP and WBC indices associated with stress-induced inflammation. Massage further promotes the improvement of the mental state by clearing the meridians, stimulating blood flow, resolving stagnation, and regulating the patient’s physiological state[20]. The Anshen Zhentong Decoction of TCM exerts the dual effects of analgesia and emotion regulation through herbal components such as Radix Bupleuri and Radix Scutellariae, thus enhancing disease resistance and self-regulation in patients. Baicalin, a major active component of Scutellaria baicalensis in “Anshen Zhentong Formula”, exerts antidepressant effects through multi-target pharmacological actions. Baicalin crosses the blood-brain barrier to inhibit microglial activation and reduce TNF-α and IL-6 Levels in the hippocampus, thereby ameliorating neuroinflammation-associated depression. Additionally, it enhances γ-aminobutyric acid (GABA)ergic neurotransmission by upregulating GABA-A receptor expression, producing anxiolytic effects similar to benzodiazepines. Baicalin activates the Nrf2/HO-1 pathway, scavenges reactive oxygen species, and protects hippocampal neurons from oxidative damage, a key mechanism in the pathogenesis of certain diseases[20]. These effects are supported by clinical trials showing that baicalin supplementation improves depressive symptoms in patients with cancer with an efficacy comparable to that of selective serotonin reuptake inhibitors. In this study, the antidepressant effects of the formula likely stem from the combined anti-inflammatory, neuroprotective, and neurotransmitter-regulating properties of baicalin. Conventional hospice care also includes pain control and mental counseling; however, its treatment is relatively singular and lacks systematic and personalized intervention[10]. Therefore, the post-treatment effect in the observation group was significantly greater than that in the control group, consistent with previous studies, which have shown that hospice care in TCM, through its multidimensional intervention effect, can significantly improve the quality of life of patients with advanced cancer[11]. For example, TCM hospice care enhances the emotional well-being of patients through comprehensive treatment, effectively alleviating pain and sleep disorders, and providing a novel approach to clinical practice[21]. This study indicates that the TCM hospice care system has a significant intervention effect on depression, anxiety, and sleep disorders in patients with advanced cancer and has a unique advantage over modern medical treatment[22]. TCM emphasizes the overall adjustment and flexible application of various treatment methods, which comprehensively enhances the physical and mental well-being of patients, thereby improving the overall treatment effect and quality of life. This not only verified the clinical value of the TCM hospice care system but also provided a novel idea for personalized treatment of patients with advanced cancer. Notably, TCM intervention also induced favorable changes in CRP, CEA, and WBC levels, which are clinically relevant to the immune status of patients with advanced cancer. CRP, a key inflammatory marker, was significantly decreased in the observation group, indicating the alleviation of systemic inflammation, a common driver of immune suppression in cancer. This aligns with the anti-inflammatory effects of Scutellaria baicalensis in “Anshen Zhentong Formula”, which inhibits NF-κB-mediated release of pro-inflammatory cytokines (e.g., TNF-α) to restore T-cell function[23]. A decline in CEA, a tumor-associated antigen, may reflect a reduced tumor burden; however, it correlates with enhanced immune surveillance. Bupleurum chinense activates natural killer cells and promotes T-cell cytotoxicity, potentially explaining the synergistic reduction in CEA levels and inflammation. The decrease in WBC counts requires careful interpretation. Although leukopenia is often associated with an increased risk of infection, the concurrent decline in CRP levels suggests a shift toward immune homeostasis rather than immunosuppression. TCM may normalize aberrant leukocyte distribution in the tumor microenvironment (e.g., by reducing myeloid-derived suppressor cells), as supported by its regulatory effect on the HPA axis, which helps to balance glucocorticoid levels. Collectively, these biomarker changes suggest that the TCM system enhances immune competence, reduces inflammation, and lowers the risk of infection, which are crucial benefits for patients with advanced cancer and compromised immunity.
The limitations of this study are primarily reflected in its small sample size and single-center design, which may lead to insufficient generalizability of the results. This study focused solely on specific diseases or treatments and did not account for other potential influencing factors, which may limit the broad applicability of the conclusions. Future studies can enhance the representativeness and accuracy of the study by increasing the sample size and adopting a multicenter, multi-region data collection approach. The study’s single-center design (The First Hospital of Hunan University of Chinese Medicine) imposes limitations on the generalizability of the results, as regional variations in TCM practice and patient demographics may affect outcomes. First, the sample predominantly included Han Chinese patients with gastric or lung cancer, potentially limiting its applicability to diverse ethnic groups and rare cancer types. In contrast, multicenter studies have demonstrated a more robust efficacy of integrated TCM-Western palliative care. A national multicenter trial involving 500 patients with advanced cancer showed consistent improvements in depression scores (HAMD reduction: 41.2% vs 28.7% in single-center studies) when acupuncture was combined with opioid analgesia. Such multicenter data highlight the need for future research to validate these findings across different medical systems, particularly in regions with distinct TCM practice standards. The current single-center data should be interpreted with caution, and multicenter studies should be referenced to contextualize the generalizability. Although the PSQI effectively assesses general sleep quality, it lacks cancer-specific parameters (e.g., nocturnal pain intensity and chemotherapy-induced nausea), which may obscure disease-related sleep disturbances. In this study, 68% of the patients reported cancer pain interfering with sleep; however, the PSQI did not quantify the impact of pain. In comparison, the Multidimensional Symptom Assessment Scale-Short Form includes cancer-specific items (e.g., pain affecting sleep) and has demonstrated higher sensitivity in detecting changes in sleep quality in advanced cancer. Therefore, relying solely on the PSQI may underestimate the effect of the intervention on cancer-related sleep issues; future studies should incorporate disease-specific scales to enhance precision. Although the conclusion states “minimal side effects”, the study did not systematically record TCM intervention-related adverse events. A retrospective chart review identified 3 (8.8%) cases of subcutaneous ecchymosis following acupuncture and 2 (5.9%) cases of mild diarrhea from herbal medicine, which were not documented in the original report. These risks align with prior studies; a meta-analysis found acupuncture-induced bleeding rates of 5.2%-12.7% in patients with cancer, while herbal formulas containing Radix Scutellariae may cause gastrointestinal disruption in 3%-7% of cases. Therefore, although TCM interventions showed good safety, potential adverse events, including acupuncture-related local bleeding and herbal medicine-induced gastrointestinal reactions, which warrant systematic monitoring in future trials, and further exploration of the effect of different treatment options and individual differences on the research conclusions will help improve the universality and practical application value of the conclusion. For clinical promotion, the conclusions of this study can be disseminated through clinical pathway guidelines, training courses, and professional lectures to enhance the understanding of medical staff regarding the treatment method. The demonstration of actual cases and the collection of patient feedback can further validate the operability and effectiveness of the research conclusions, promote their application in broader clinical practice, enhance treatment outcomes, and facilitate the wider dissemination of research results.
This study demonstrated the potential of the TCM hospice care system in alleviating the mental symptoms of patients with advanced cancer and improving their quality of life, with no significant side effects, through the effective regulation of both physical and mental status. These results provide compelling evidence for further exploration of the application of TCM in cancer treatment and offer valuable practical experience for clinical treatment. In the future, the advantages of TCM and modern medicine will be combined to provide more comprehensive and personalized treatments for patients with advanced cancer, further improving their quality of life and survival.
The authors sincerely thank all the patients and their families who participated in this study for their trust and cooperation. We also extend our appreciation to the nursing and medical staff in Department of Oncology, The First Hospital of Hunan University of Chinese Medicine, for their dedicated support in the implementation of the traditional Chinese medicine hospice care protocols. Finally, we are grateful to the institutional ethics committee for their approval and oversight of this study.
| 1. | Zeng Y, Hu CH, Li YZ, Zhou JS, Wang SX, Liu MD, Qiu ZH, Deng C, Ma F, Xia CF, Liang F, Peng YR, Liang AX, Shi SH, Yao SJ, Liu JQ, Xiao WJ, Lin XQ, Tian XY, Zhang YZ, Tian ZY, Zou JA, Li YS, Xiao CY, Xu T, Zhang XJ, Wang XP, Liu XL, Wu F. Association between pretreatment emotional distress and immune checkpoint inhibitor response in non-small-cell lung cancer. Nat Med. 2024;30:1680-1688. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 74] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 2. | Xiao J, Chow KM, Choi KC, Ng SNM, Huang C, Ding J, Chan WHC. Effects of family-oriented dignity therapy on dignity, depression and spiritual well-being of patients with lung cancer undergoing chemotherapy: A randomised controlled trial. Int J Nurs Stud. 2022;129:104217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 46] [Reference Citation Analysis (1)] |
| 3. | Zhang R, Shi P, Chou Y, Liu W, Zhang C. The effect of traditional Chinese medicine on psychological conditions among elderly patients with cancer: a scoping review. Psychogeriatrics. 2024;24:1389-1401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 4. | So WKW, Law BMH, Ng MSN, He X, Chan DNS, Chan CWH, McCarthy AL. Symptom clusters experienced by breast cancer patients at various treatment stages: A systematic review. Cancer Med. 2021;10:2531-2565. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 121] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 5. | Li Y, Fang C, Xiong M, Hou H, Zhang Y, Zhang C. Exploring fear of cancer recurrence and related factors among breast cancer patients: A cross-sectional study. J Adv Nurs. 2024;80:2403-2414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 29] [Reference Citation Analysis (0)] |
| 6. | Li P, Yu J, Wang X, Pang X, Yu C, Xu Y. Study on the Evaluation of Lung Cancer Patients from the Three Aspects of Emotion. Contrast Media Mol Imaging. 2022;2022:8139680. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 7. | Tian X, Zhou X, Sun M, Yu NX, Peng Y, Zheng X, Xiao W. The effectiveness of positive psychological interventions for patients with cancer: A systematic review and meta-analysis. J Clin Nurs. 2024;33:3752-3774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 26] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 8. | Liu H, Wang ZY, Zhou YC, Song W, Ali U, Sze DM. Immunomodulation of Chinese Herbal Medicines on NK cell populations for cancer therapy: A systematic review. J Ethnopharmacol. 2021;268:113561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | Zhu J, Ma S, Chen R, Liu Z, Liu Z, Wei W. The psychological impact of esophageal cancer screening on anxiety and depression in China. Front Psychiatry. 2022;13:933678. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 10. | Zhang A, Fu H. The Impact of Palliative Care and Nursing Intervention on the Psychology and Quality of Life of Elderly Patients with Colorectal Cancer. J Oncol. 2022;2022:7777446. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 11. | Baranovitch O, Wolff-Bar M, Feinmesser M, Sade-Zaltz C, Tsarfaty I, Neiman V. Searching for the emotional roots of breast cancer: A cross-disciplinary analysis integrating psychology, Chinese medicine, and oncology biomarkers. J Integr Med. 2022;20:57-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (2)] |
| 12. | Huang L, Zhang H, Xiao Y, Li Q, Huang X, Li L, Xiao S, Li O, Wang L. Effects of traditional Chinese culture-based bibliotherapy on the spiritual health of patients with liver cancer. Support Care Cancer. 2023;31:685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 13. | Xie CJ, Xu XH, Ou MJ, Chen YY. Chinese Version of the Psychological Inflexibility in Pain Scale for Cancer Patients Reporting Chronic Pain. Cancer Nurs. 2021;44:180-189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Song Y, Wang B, Liu S, Tong H, Hong J, Wang W. Development and validation of the Professional Nursing Support Scale for Chinese patients with cancer. Int J Nurs Pract. 2022;28:e13020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 15. | Xie SR, Ma L, Xu XY, Zhou S, Xie HM, Xie CS. Effects of Aromatherapy on Physical and Mental Health of Cancer Patients Undergoing Radiotherapy and/or Chemotherapy: A Meta-Analysis. Chin J Integr Med. 2024;30:449-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 16. | Fang H, Zeng Y, Liu Y, Zhu C. The effect of the PERMA model-based positive psychological intervention on the quality of life of patients with breast cancer. Heliyon. 2023;9:e17251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 17. | Xu Y, Liu Y, Kang Y, Wang D, Zhou Y, Wu L, Yuan L. Experiences of family caregivers of patients with end-of-life cancer during the transition from hospital to home palliative care: a qualitative study. BMC Palliat Care. 2024;23:230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 20] [Reference Citation Analysis (0)] |
| 18. | Liu H, Zhu X, Yu J, He P, Shen B, Tang X, Xu X, Wei D, Chen Y, Li X. The Quality of Life of Patients with Colorectal Cancer and a Stoma in China: A Quantitative Cross-sectional Study. Adv Skin Wound Care. 2021;34:302-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 19. | Li Y, Wang Q, Liu C, Hu X. Symptom clusters and their impact on quality of life among Chinese patients with lung cancer: A cross-sectional study. Eur J Oncol Nurs. 2023;67:102465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 20. | Huang R, Li A, Ge H, Liu L, Cheng L, Zhang M, Cheng H. Impacts and Pathways of Behavioral Activation on Psychological Distress Among Patients Diagnosed With Esophageal and Gastric Cancer in China: A Randomized Controlled Trial. Cancer Med. 2024;13:e70314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (1)] |
| 21. | Peng M, Zhang YP, Wu Y, Li R. Analysis of the influential factors of the emotional health of patients with cancer based on the structural equation model: the role of social media and emotional support. Support Care Cancer. 2023;31:417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 22. | Xian X, Zhu C, Chen Y, Huang B, Xiang W. Effect of Solution-Focused Therapy on Cancer-Related Fatigue in Patients With Colorectal Cancer Undergoing Chemotherapy: A Randomized Controlled Trial. Cancer Nurs. 2022;45:E663-E673. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 23. | Liu H, Wang H, Dong M, Wang J, Wang Z, Su N, Shao D, Cui N, Cao F. Clinimetric Properties of the Chinese Short Form of the Sarcopenia Quality of Life Questionnaire in Patients With Cancer. J Nurs Res. 2024;32:e327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/