Published online Oct 19, 2025. doi: 10.5498/wjp.v15.i10.106705
Revised: June 18, 2025
Accepted: August 4, 2025
Published online: October 19, 2025
Processing time: 132 Days and 23.5 Hours
Hip fracture in elderly patients, particularly those with comorbid post-traumatic stress disorder (PTSD), presents a significant clinical challenge. In addition to the physiological stress of surgery, these patients often endure psychological burdens that may adversely affect postoperative recovery. The potential benefits of targeted perioperative psychological interventions have not been fully elucidated in this special population. This study hypothesized that a structured perioperative psychological program would improve recovery outcomes, including postope
To evaluate the impact of perioperative psychological intervention on postopera
Between January 1, 2022, and December 31, 2024, medical records of 50 elderly hip fracture patients (age ≥ 65) with PTSD who underwent surgical fixation at our center were retrospectively reviewed. Patients were divided into an intervention (n = 25; standardized psychological care) and control (n = 25; usual care) groups. Data collected included de
The groups had comparable demographic and clinical characteristics. The intervention group demonstrated significantly lower pain scores on postoperative days 3 and 7 (P < 0.01), fewer moderate-to-severe depressive symptoms (P < 0.05), and a greater reduction in PTSD severity (P < 0.01) compared with the control group. Furthermore, the intervention group exhibited improved activities of daily living scores at 4 weeks post-surgery and a lower postoperative complication rate (16% vs 32%, P = 0.14). The average length of hospital stay was shorter in the intervention group (11.5 ± 2.0 days vs 13.1 ± 2.6 days, P < 0.05).
In elderly hip fractures patients with comorbid PTSD, perioperative psychological interventions improved pain control, functional recovery, and PTSD symptoms, supporting its value in holistic perioperative management and outcome enhancement.
Core Tip: Elderly hip fracture patients with comorbid post-traumatic stress disorder face unique recovery challenges. This retrospective study highlights the benefits of structured perioperative psychological intervention, demonstrating significant improvements in pain management, functional recovery, and post-traumatic stress disorder symptom reduction. Patients receiving psychological support reported lower pain scores, fewer depressive symptoms, enhanced activities of daily living, and shorter hospital stays. These findings suggest that integrating psychological care into perioperative management may optimize outcomes and overall patient well-being in this vulnerable population.
- Citation: Liu YD, Ma JY, Wang JH, Sun T, Han ZY. Effect of perioperative psychological intervention on recovery in elderly hip fracture patients with comorbid post-traumatic stress disorder. World J Psychiatry 2025; 15(10): 106705
- URL: https://www.wjgnet.com/2220-3206/full/v15/i10/106705.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i10.106705
Elderly hip fractures are a major public health concern worldwide, with high incidence rates and substantial morbidity[1]. Although complications such as infections, delirium, and malunion are commonly addressed, less attention has been given to comorbid post-traumatic stress disorder (PTSD) in elderly patients following trauma. Older adults often present with complex medical and psychological profiles that can complicate perioperative care. PTSD, originally conceptualized in the context of combat experiences, may also be triggered by falls, accidents, or life-threatening injuries[2].
The presence of PTSD can result in hyperarousal, intrusive recollections, avoidance, and negative mood states[3]. These psychological stressors may exacerbate the stress response to surgery, hindering physical rehabilitation, increasing pain perception, and prolonging hospital stays[4]. Conventional surgical pathways may not adequately address the specific anxieties and altered coping mechanisms of patients with PTSD, particularly in geriatric populations. Older individuals with PTSD often exhibit compromised psychological resilience, which can impair adherence to postoperative protocols[5,6]. The potential synergy between PTSD and hip fracture is particularly concerning, as unmanaged mental health may adversely affect clinical outcomes.
Growing attention has been directed toward holistic perioperative care, recognizing the interplay between emotional well-being and physiological recovery[7,8]. Standard interventions, such as pain control, mobilization exercises, nutritional support, are vital but may not sufficiently address the psychological dimension. Evidence from other surgical contexts demonstrate that psychological support can mitigate anxiety, reduce analgesic consumption, and improve patient satisfaction[9]. Nevertheless, data specific to geriatric hip fracture patients with PTSD remain limited. This retrospective study aimed to compare postoperative recovery outcomes between elderly hip fracture patients with comorbid PTSD who received standardized psychological intervention and those who received usual care. It was hypothesized that structured perioperative psychological support would reduce pain, enhance functional recovery, shorten hospital stays, and improve PTSD symptom control. These findings could pave the way for more integrated mental health interventions within geriatric orthopedic care pathways.
This retrospective study focused on elderly patients who were diagnosed with both hip fractures and PTSD at our hospital. The study period spanned from January 1, 2022, to December 31, 2024, during which consecutive patient records were systematically reviewed. Prior to the study, ethical approval was obtained from the Institutional Ethics Committee of Yantaishan Hospital of Yantai, and informed consent was secured from all patients. Data collection and analysis procedures strictly adhered to institutional privacy protocols and regulatory requirements. The study protocol was approved by the Yantaishan Hospital of Yantai.
The study population was defined through comprehensive inclusion and exclusion criteria. Eligible participants were aged ≥ 65 years with an acute hip fracture, specifically including femoral neck, intertrochanteric, or subtrochanteric fractures necessitating surgical intervention. A confirmed diagnosis of PTSD according to Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition criteria, either pre-existing or established during the initial hospital admission, was required. Additionally, medical stability for surgical intervention, as determined by a multidisciplinary team, was also necessary.
Several exclusion criteria were applied to maintain data quality and ensure reliable outcomes assessment. Patients with severe cognitive impairment, particularly those with advanced dementia that could compromise self-reporting accuracy, were excluded. Patients with terminal illnesses or a projected life expectancy of less than six months were also excluded, as such conditions could significantly confound study outcomes. In addition, patients unable or unwilling to participate in postoperative assessments were excluded to ensure completeness of follow-up data. An initial screening identified 60 patients who meet the basic eligibility criteria. Following rigorous quality checks and verification of medical documen
Patient allocation into study groups was determined through systematic review of departmental record system, which documented the delivery of specialized perioperative psychological support. The final sample was evenly divided into two groups of 25 patients each. The intervention group received a standardized perioperative psychological intervention program, whereas the control group received standard routine care without structured psychological support.
Standard routine care: All study participants, regardless of group assignment, received comprehensive standard perioperative care in accordance with established institutional protocols. The surgical approach was individualized based on fracture characteristics and patient-specific factors, with options including dynamic hip screw placement, intramedullary nail fixation, or arthroplasty. The specific surgical technique was selected at the discretion of the attending surgeon, taking into consideration factors such as fracture pattern, bone quality, and patient activity level.
Perioperative analgesia included intravenous acetaminophen 1 g every 6 hours, with or without celecoxib 200 mg twice daily, and rescue morphine 2 mg intravenous as needed. Pain management followed a multimodal approach combining regional anesthesia techniques with systemic analgesics. Nutritional optimization was achieved through dietary con
Structured psychological intervention: The intervention group received an intensive, evidence-based psychological program administered by qualified mental health professionals, including clinical psychologists and psychiatrists trained in trauma-informed care. This comprehensive intervention commenced immediately upon admission and continued throughout the hospital stay, with several key components carefully integrated into the patient’s daily routine.
Preoperative assessment and counseling constituted the foundation of the intervention, comprising detailed psy
Daily relaxation and mindfulness exercises were structured as 20-minute guided sessions, specifically designed to address trauma-related triggers and flashbacks commonly experienced in the hospital setting. These sessions incor
Postoperative coping sessions focused on cognitive restructuring techniques to help patients reframe negative thoughts related to their recovery process. These sessions aimed to enhance self-efficacy in the rehabilitation process while acknowledging and working through PTSD-related challenges that could impact recovery. Mental health professionals collaborated with physical therapists to ensure psychological support was integrated with physical rehabilitation goals.
Family involvement was recognized as a crucial component of the intervention. Family members received structured education on PTSD symptoms and their potential impact on recovery. Training included specific techniques to support the patient's emotional needs, recognize and respond to PTSD triggers, and encourage participation in rehabilitation activities. Regular family conferences were scheduled to address concerns and adjust support strategies as needed.
Baseline parameters: Data were extracted from electronic medical records using a standardized protocol. Demographic variables included age, sex, educational level, living situation, and indicators of socioeconomic status. Comorbidities were documented comprehensively, detailing both the presence and severity and duration of conditions including hypertension, diabetes, coronary artery disease, and other relevant medical conditions, assessed using the Charlson Comorbidity Index.
Fracture characteristics were documented in detail, including exact anatomical location, fracture pattern classification, mechanism of injury, and time from injury to hospital presentation. PTSD severity was assessed using the Clinician-Administered PTSD Scale (CAPS), which provides a comprehensive evaluation of symptom frequency and intensity. When available, historical data on the original trauma, duration of PTSD symptoms, and previous treatment approaches were also collected.
Preoperative psychological status was evaluated using standardized instruments. The Geriatric Depression Scale (GDS) was used to assess depressive symptoms, whereas the Hamilton Anxiety Rating Scale measured anxiety levels. Cognitive function was evaluated using the Mini-Mental State Examination, supplemented by the Montreal Cognitive Assessment when more detailed cognitive assessment was warranted.
Surgical and perioperative data: Surgical data were comprehensively documented, including procedure type, with specific attention to surgical approach, fixation method, and any additional procedures performed. Anesthesia records included the primary method (spinal, epidural, or general) and any supplementary techniques used such as nerve blocks or local infiltration.
Operative parameters were meticulously recorded, including precise operative time, estimated blood loss, fluid administration, and any intraoperative complications or challenges. The expertise level of the primary surgeon and any specific technical considerations influencing the surgical approach were also noted. Length of hospital stay was calculated from admission to discharge, with detailed documentation of factors contributing to prolonged hospitalization.
Outcome assessment followed a comprehensive, multi-dimensional protocol. Pain scores were recorded using the Numerical Rating Scale at standardized intervals: Every 4 hours during the first 24 hours post-surgery, then three times daily until postoperative day 7. Pain assessment included both rest and movement-related pain scores, alongside docu
PTSD symptom severity was reassessed using the CAPS on postoperative days 7 and 14, with particular attention to any surgery-related exacerbation of symptoms. Additional measures included assessment of sleep quality, nightmare frequency, and flashback episodes. Depressive symptoms were monitored using both the GDS and Hamilton Depression Rating Scale (HDRS) at regular intervals during the postoperative period.
Functional recovery was evaluated using a multi-faceted approach that included Timed-Up-and-Go test. The activities of daily living assessment and Barthel Index were completed at 4 weeks post-surgery, supplemented by objective measures of physical function including gait speed and grip strength, with the Timed-Up-and-Go test administered when appropriate. Participation in and adherence to physical therapy sessions were also documented.
Complications were systematically monitored and recorded, including both medical (infection, pressure ulcers, pneumonia, delirium) and psychological complications. Each adverse event was classified according to severity and its relationship to the surgical procedure or PTSD status. Readmission rates were tracked for 30 days post-discharge, with detailed documentation of readmission causes.
Patient satisfaction was evaluated using a comprehensive 5-point Likert scale covering multiple domains of the care experience, including pain management, psychological support, physical therapy, and overall care coordination. Additional qualitative feedback was collected through structured interviews at discharge and follow-up visits.
Data were analyzed using SPSS version 26.0 (IBM, Armonk, NY, United States), and groups were balanced using 1:1 propensity-score matching (C-statistic = 0.71). Descriptive statistics summarized baseline variables; mean ± SD or medians (interquartile range) were reported as appropriate. Categorical data are expressed as frequencies and percen
A total of 50 elderly patients with hip fractures and comorbid PTSD were included, evenly divided into the intervention group (n = 25) and the control group (n = 25). Table 1 summarizes the baseline demographics and clinical characteristics. No significant differences were observed between groups in age (mean 78.2 ± 5.1 years vs 77.8 ± 6.2 years, P = 0.73), sex distribution (56% female in the intervention group vs 60% female in the control group, P = 0.77), fracture type (P = 0.82), or comorbidity profiles (P > 0.05). Baseline PTSD symptom severity scores (CAPS) did not differ significantly (P = 0.66). Mean Mini-Mental State Examination scores were comparable, indicating equivalent baseline cognitive status.
| Characteristics | Intervention group (n = 25) | Control group (n = 25) | P value |
| Demographics | |||
| Age (year), mean ± SD | 78.2 ± 5.1 | 77.8 ± 6.2 | 0.73 |
| Female sex | 14 (56) | 15 (60) | 0.77 |
| Living situation | |||
| Independent | 16 (64) | 15 (60) | 0.85 |
| With family | 7 (28) | 8 (32) | 0.82 |
| Assisted living | 2 (8) | 2 (8) | 1.00 |
| Clinical parameters | |||
| BMI, kg/m2, mean ± SD | 25.3 ± 4.2 | 24.9 ± 3.8 | 0.68 |
| MMSE score, mean ± SD | 26.8 ± 2.1 | 26.5 ± 2.3 | 0.71 |
| CAPS score, mean ± SD | 45.6 ± 12.4 | 44.8 ± 11.9 | 0.66 |
| Comorbidities | |||
| Hypertension | 18 (72) | 17 (68) | 0.82 |
| Diabetes mellitus | 8 (32) | 9 (36) | 0.77 |
| Coronary artery disease | 6 (24) | 7 (28) | 0.75 |
| Chronic pulmonary disease | 5 (20) | 4 (16) | 0.71 |
| Fracture type | |||
| Femoral neck | 12 (48) | 11 (44) | 0.82 |
| Intertrochanteric | 9 (36) | 10 (40) | 0.78 |
| Subtrochanteric | 4 (16) | 4 (16) | 1.00 |
| Preoperative status | |||
| ASA score, mean ± SD | 2.8 ± 0.6 | 2.7 ± 0.5 | 0.69 |
| Hemoglobin, g/dL, mean ± SD | 12.1 ± 1.4 | 12.3 ± 1.3 | 0.74 |
| Albumin, g/dL, mean ± SD | 3.8 ± 0.4 | 3.7 ± 0.5 | 0.68 |
| Time from injury to surgery (hours), mean ± SD | 28.4 ± 8.2 | 29.1 ± 7.8 | 0.65 |
The distribution of surgical procedures, intramedullary nailing (n = 22), hemiarthroplasty (n = 18), and dynamic hip screw (n = 10), was comparable between groups (P = 0.49). Mean operative time was 90 ± 20 minutes in the intervention group and 93 ± 18 minutes in the control group. No differences were observed in the type of anesthesia administered or estimated blood loss (P > 0.05).
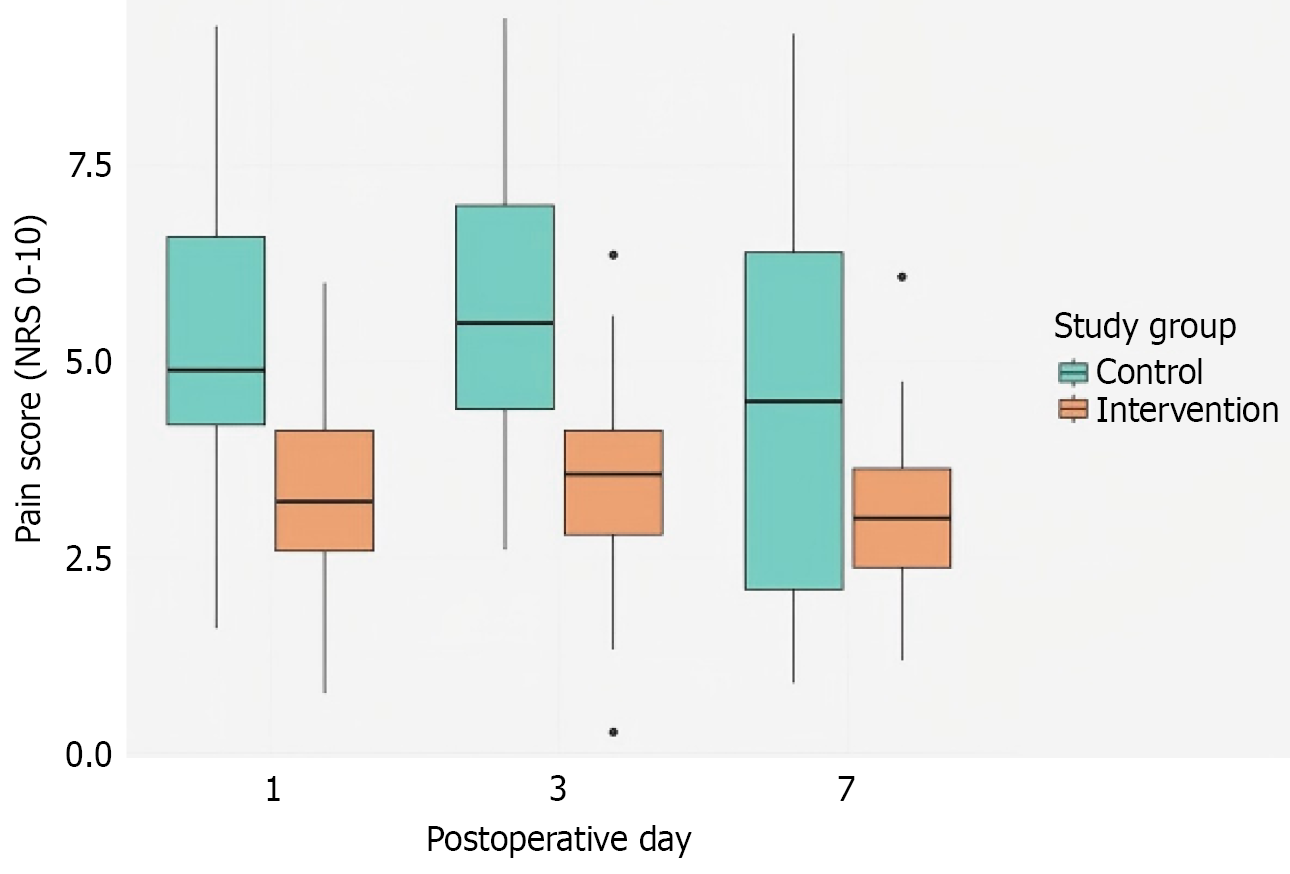
Figure 1 presents the Numerical Rating Scale pain scores on postoperative days (POD) 1, 3, and 7. POD 1: Both groups reported moderate-to-severe pain (intervention group: 6.0 ± 1.2; control group: 6.3 ± 1.1, P = 0.42). POD 3: Pain scores were significantly lower in the intervention group (4.2 ± 1.1) compared with the control group (5.1 ± 1.2, P = 0.01). POD 7: This trend persisted, with the intervention group reporting lower pain levels (2.9 ± 0.8) than the control group (3.8 ± 1.0, P < 0.01). These findings indicate that, from POD 3 onward, the intervention group reported significantly lower pain levels compared with the control group.
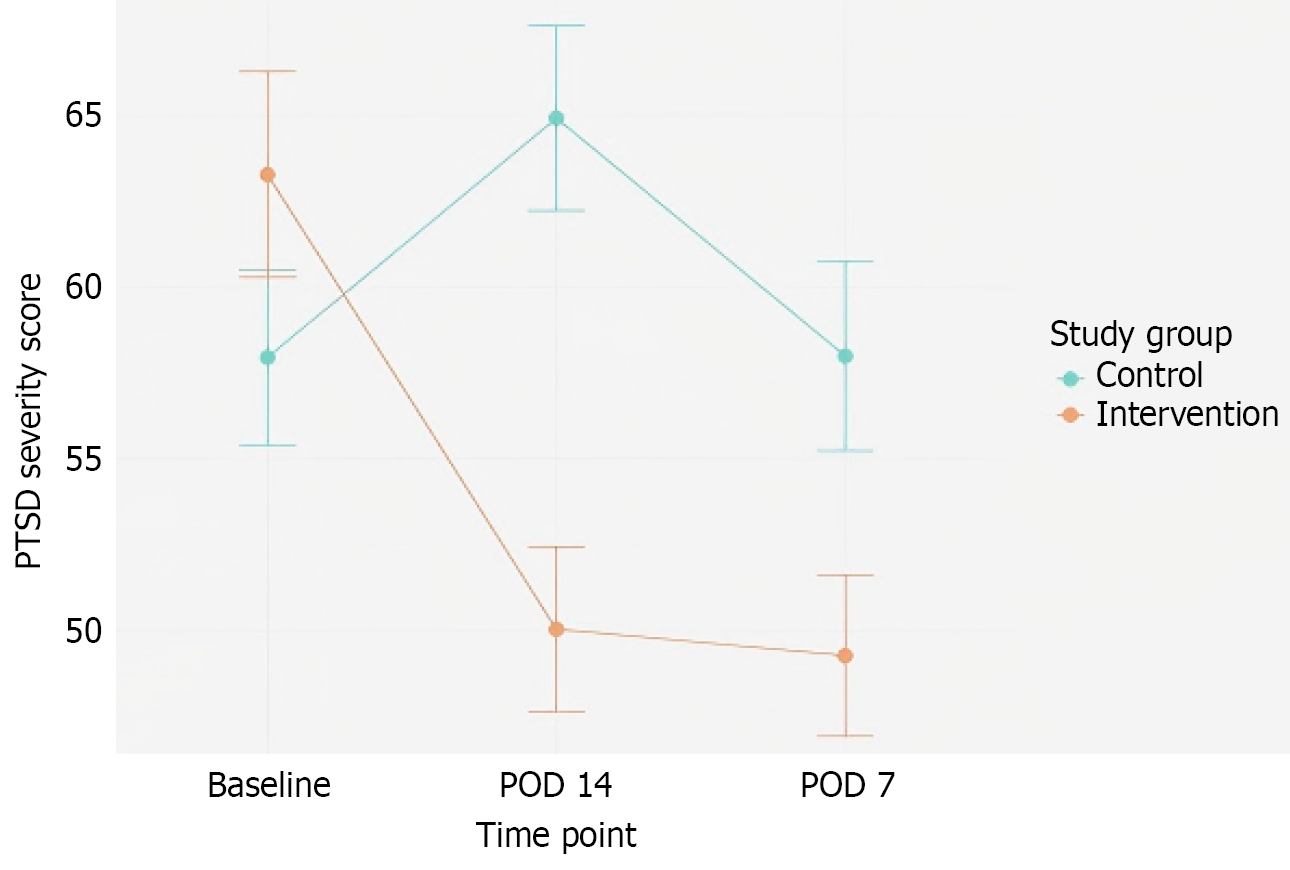
Figure 2 illustrates the mean changes in PTSD severity, assessed using the CAPS or a similar validated scale, from baseline to postoperative days 7 and 14. Both groups demonstrated improvements, likely due to partial symptom resolution post-surgery; however, the intervention group exhibited significantly greater reductions: Day 7: -8.2 points (intervention) vs -4.6 points (control), P < 0.01. Day 14: -10.5 points (intervention) vs -6.5 points (control), P < 0.01.
At POD 7, a clinically relevant difference was observed in GDS or HDRS scores. The intervention group had significantly lower GDS or HDRS scores (10.2 ± 3.0) compared with the control group (12.1 ± 3.4, P = 0.03). Although both groups exhibited mild to moderate depressive symptoms, the psychological intervention may have mitigated acute stress responses.
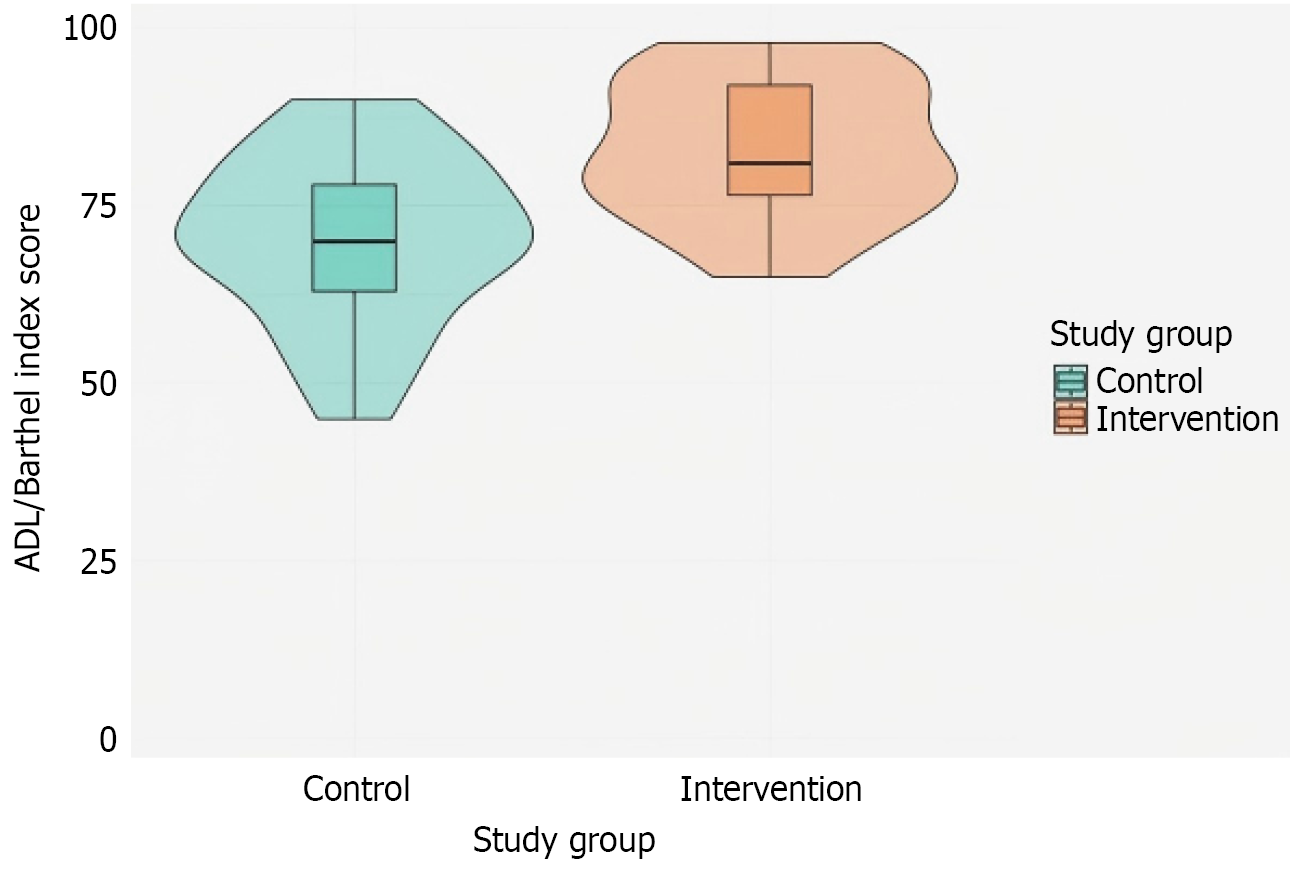
At 4 weeks postoperatively, functional independence, assessed via activities of daily living or Barthel Index, was significantly greater in the intervention group (74.5 ± 8.0) compared with the control group (67.2 ± 7.9, P = 0.01) (Figure 3). These findings suggests that addressing psychological distress may reinforce compliance with physiotherapy and self-care routines.
The complication rates were lower in the intervention group (16%) compared with the control group (32%), although this difference did not reach statistical significance (P = 0.14), potentially due to limited sample size. However, length of hospital stay was significantly shorter in the intervention group (11.5 ± 2.0 days) than in the control group (13.1 ± 2.6 days, P < 0.05). Factors such as early mobilization, fewer analgesic requirements, and better emotional coping may have facilitated earlier discharge.
Patients in the intervention group reported significantly higher satisfaction scores on the 5-point Likert scale compared with the control group (4.2 ± 0.6 vs 3.7 ± 0.8, P < 0.01). Qualitative feedback highlighted feelings of reassurance, empower
This retrospective study investigated the role of perioperative psychological intervention in elderly patients with hip fracture and comorbid PTSD. The findings highlight the significant benefits of targeted mental health support in im
First, patients who received psychological intervention experienced significantly better pain relief compared with those receiving routine care. Specifically, on POD 3 and 7, the intervention group reported lower pain scores than the control group. This finding aligns with previous studies demonstrating that psychological intervention can alleviate pain by reducing anxiety, promoting emotional regulation, and improving self-efficacy, thereby optimizing postoperative reco
Second, PTSD symptoms showed significant improvement in the intervention group. Although both groups demon
Additionally, patients in the intervention group had a shorter hospital stay. Although the difference did not reach statistical significance, the reduced length of stay in the intervention group may be attributed to improved emotional adaptation, pain management, and prevention of postoperative complications. Previous studies have demonstrated that psychological interventions can attenuate the physiological stress response, promote early mobilization, and reduce complications, thereby contributing to shorter hospital stays[19-21].
However, despite the promising results, this study has some limitations. Its retrospective design introduces potential selection bias, and the relatively small sample size (n = 50) limits the statistical power of certain comparisons, such as complication rates. Additionally, the absence of long-term follow-up precludes assessment of the sustainability of psychological benefits over time. The single-center design may also limit the generalizability of the findings to broader health
Future research should focus on prospective, multicenter trials with larger sample sizes and extended follow-up periods. Such studies could help confirm the durability of psychological benefits observed in this study and explore whether booster sessions are required to sustain long-term improvements. Furthermore, refining psychological inter
Perioperative psychological intervention appears to offer significant benefits for elderly patients with hip fractures and PTSD, including improved pain management, reduction in PTSD symptoms, and enhanced functional recovery. Incor
| 1. | Sing CW, Lin TC, Bartholomew S, Bell JS, Bennett C, Beyene K, Bosco-Levy P, Bradbury BD, Chan AHY, Chandran M, Cooper C, de Ridder M, Doyon CY, Droz-Perroteau C, Ganesan G, Hartikainen S, Ilomaki J, Jeong HE, Kiel DP, Kubota K, Lai EC, Lange JL, Lewiecki EM, Lin J, Liu J, Maskell J, de Abreu MM, O'Kelly J, Ooba N, Pedersen AB, Prats-Uribe A, Prieto-Alhambra D, Qin SX, Shin JY, Sørensen HT, Tan KB, Thomas T, Tolppanen AM, Verhamme KMC, Wang GH, Watcharathanakij S, Wood SJ, Cheung CL, Wong ICK. Global Epidemiology of Hip Fractures: Secular Trends in Incidence Rate, Post-Fracture Treatment, and All-Cause Mortality. J Bone Miner Res. 2023;38:1064-1075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 317] [Article Influence: 105.7] [Reference Citation Analysis (0)] |
| 2. | Qassem T, Aly-ElGabry D, Alzarouni A, Abdel-Aziz K, Arnone D. Psychiatric Co-Morbidities in Post-Traumatic Stress Disorder: Detailed Findings from the Adult Psychiatric Morbidity Survey in the English Population. Psychiatr Q. 2021;92:321-330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 59] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 3. | Shalev A, Liberzon I, Marmar C. Post-Traumatic Stress Disorder. N Engl J Med. 2017;376:2459-2469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 394] [Cited by in RCA: 518] [Article Influence: 57.6] [Reference Citation Analysis (0)] |
| 4. | Bisson JI, Baker A, Dekker W, Hoskins MD. Evidence-based prescribing for post-traumatic stress disorder. Br J Psychiatry. 2020;216:125-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Wainberg ML, Scorza P, Shultz JM, Helpman L, Mootz JJ, Johnson KA, Neria Y, Bradford JE, Oquendo MA, Arbuckle MR. Challenges and Opportunities in Global Mental Health: a Research-to-Practice Perspective. Curr Psychiatry Rep. 2017;19:28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 343] [Cited by in RCA: 428] [Article Influence: 47.6] [Reference Citation Analysis (0)] |
| 6. | Zuelzer DA, Weaver D, Zuelzer AP, Hessel EA. Current Strategies in Medical Management of the Geriatric Hip Fracture Patient. J Am Acad Orthop Surg. 2023;31:620-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 7. | Sepucha KR, Atlas SJ, Chang Y, Freiberg A, Malchau H, Mangla M, Rubash H, Simmons LH, Cha T. Informed, Patient-Centered Decisions Associated with Better Health Outcomes in Orthopedics: Prospective Cohort Study. Med Decis Making. 2018;38:1018-1026. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 8. | Suarez EC, Saab PG, Llabre MM, Kuhn CM, Zimmerman E. Ethnicity, gender, and age effects on adrenoceptors and physiological responses to emotional stress. Psychophysiology. 2004;41:450-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Kondylakis H, Giglioli IAC, Katehakis D, Aldemir H, Zikas P, Papagiannakis G, Hors-Fraile S, González-Sanz PL, Apostolakis K, Stephanidis C, Núñez-Benjumea FJ, Baños-Rivera RM, Fernandez-Luque L, Kouroubali A. Stress Reduction in Perioperative Care: Feasibility Randomized Controlled Trial. J Med Internet Res. 2025;27:e54049. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 10. | Hah JM, Nwaneshiudu CA, Cramer EM, Carroll IR, Curtin CM. Acute Pain Predictors of Remote Postoperative Pain Resolution After Hand Surgery. Pain Ther. 2021;10:1105-1119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Tassou A, Richebe P, Rivat C. Mechanisms of chronic postsurgical pain. Reg Anesth Pain Med. 2025;50:77-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 19] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 12. | Pai SL, Ladlie B, Locke K, Garcia Getting R. Patient-Centered Care for Ambulatory Surgery. Int Anesthesiol Clin. 2025;63:14-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 13. | Hetzel-Riggin MD. Evidence Based Treatments for Trauma-Related Psychological Disorders: A Practical Guide for Clinicians, edited by U. Schnyder and M. Cloitre. J Trauma Dissociation. 2016;17:520-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Merians AN, Spiller T, Harpaz-Rotem I, Krystal JH, Pietrzak RH. Post-traumatic Stress Disorder. Med Clin North Am. 2023;107:85-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 46] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 15. | Alisic E, Zalta AK, van Wesel F, Larsen SE, Hafstad GS, Hassanpour K, Smid GE. Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: meta-analysis. Br J Psychiatry. 2014;204:335-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 459] [Cited by in RCA: 514] [Article Influence: 46.7] [Reference Citation Analysis (0)] |
| 16. | Swarbrick CJ, Partridge JSL. Evidence-based strategies to reduce the incidence of postoperative delirium: a narrative review. Anaesthesia. 2022;77 Suppl 1:92-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 157] [Article Influence: 39.3] [Reference Citation Analysis (0)] |
| 17. | Maeng LY, Milad MR. Post-Traumatic Stress Disorder: The Relationship Between the Fear Response and Chronic Stress. Chronic Stress (Thousand Oaks). 2017;1:2470547017713297. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 18. | Ressler KJ, Berretta S, Bolshakov VY, Rosso IM, Meloni EG, Rauch SL, Carlezon WA Jr. Post-traumatic stress disorder: clinical and translational neuroscience from cells to circuits. Nat Rev Neurol. 2022;18:273-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 265] [Article Influence: 66.3] [Reference Citation Analysis (0)] |
| 19. | Oliveira P, Pires R, Silva R, Sequeira C. Design of a nursing psychoeducation program to reduce preoperative anxiety in adults. Front Public Health. 2024;12:1391764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 20. | Zale EL, Ring D, Vranceanu AM. The Future of Orthopaedic Care: Promoting Psychosocial Resiliency in Orthopaedic Surgical Practices. J Bone Joint Surg Am. 2018;100:e89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 21. | Conner KO, McKinnon SA, Ward CJ, Reynolds CF, Brown C. Peer education as a strategy for reducing internalized stigma among depressed older adults. Psychiatr Rehabil J. 2015;38:186-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/