Published online Sep 19, 2022. doi: 10.5498/wjp.v12.i9.1204
Peer-review started: January 12, 2022
First decision: April 18, 2022
Revised: May 2, 2022
Accepted: August 26, 2022
Article in press: August 26, 2022
Published online: September 19, 2022
Processing time: 251 Days and 4.6 Hours
Lifetime psychotic symptoms are present in over half of the patients with bipolar disorder (BD) and can have an adverse effect on its course, outcome, and treatment. However, despite a considerable amount of research, the impact of psychotic symptoms on BD remains unclear, and there are very few systematic reviews on the subject.
To examine the extent of psychotic symptoms in BD and their impact on several aspects of the illness.
The Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines were followed. An electronic literature search of six English-language databases and a manual search was undertaken to identify published articles on psychotic symptoms in BD from January 1940 to December 2021. Combinations of the relevant Medical Subject Headings terms were used to search for these studies. Articles were selected after a screening phase, followed by a review of the full texts of the articles. Assessment of the methodological quality of the studies and the risk of bias was conducted using standard tools.
This systematic review included 339 studies of patients with BD. Lifetime psychosis was found in more than a half to two-thirds of the patients, while current psychosis was found in a little less than half of them. Delusions were more common than hallucinations in all phases of BD. About a third of the patients reported first-rank symptoms or mood-incongruent psychotic symptoms, particularly during manic episodes. Psychotic symptoms were more frequent in bipolar type I compared to bipolar type II disorder and in mania or mixed episodes compared to bipolar depression. Although psychotic symptoms were not more severe in BD, the severity of the illness in psychotic BD was consistently greater. Psychosis was usually associated with poor insight and a higher frequency of agitation, anxiety, and hostility but not with psychiatric comorbidity. Psychosis was consistently linked with increased rates and the duration of hospitalizations, switching among patients with depression, and poorer outcomes with mood-incongruent symptoms. In contrast, psychosis was less likely to be accompanied by a rapid-cycling course, longer illness duration, and heightened suicidal risk. There was no significant impact of psychosis on the other parameters of course and outcome.
Though psychotic symptoms are very common in BD, they are not always associated with an adverse impact on BD and its course and outcome.
Core Tip: This systematic review examined the extent and impact of psychosis in 339 studies of bipolar disorder (BD). The results endorsed the high rates of all types of psychotic symptoms in BD. However, psychosis was associated with an adverse impact only in a few domains of the illness including the severity of BD, the rate/duration of hospitalizations, switches to BD, and poorer outcomes with mood-incongruent symptoms. No consistent associations were found in other areas, suggesting that psychosis is not always associated with a negative impact on BD. This finding conformed to the current consensus in the literature on psychotic BD.
- Citation: Chakrabarti S, Singh N. Psychotic symptoms in bipolar disorder and their impact on the illness: A systematic review. World J Psychiatry 2022; 12(9): 1204-1232
- URL: https://www.wjgnet.com/2220-3206/full/v12/i9/1204.htm
- DOI: https://dx.doi.org/10.5498/wjp.v12.i9.1204
Psychosis in bipolar disorder (BD) is characterized by the presence of either delusions or hallucinations or both[1]. It is well known that over half of the patients with BD develop psychotic symptoms during their lifetimes[2,3]. Psychotic symptoms are more frequent in bipolar than in unipolar depression[3-5]. Rates of psychotic symptoms in BD may be comparable to schizophrenia, and there appears to be no qualitative distinction in psychotic symptoms found in BD or schizophrenia[6-8]. Psychotic symptoms are much more frequent during manic than depressive episodes[3,5,8]. Their rates are so high in mania that it is often indistinguishable from primary psychotic disorders[9]. All kinds of psychotic symptoms may occur among patients with BD, though grandiose, persecutory, and referential delusions, auditory verbal hallucinations or hearing voices, and visual hallucinations are particularly common[2,8,10]. Both mood-congruent and mood-incongruent psychotic symptoms as well as Schneiderian first-rank symptoms (FRS) also occur in BD[2,3,6,8].
Given their ubiquity, psychotic symptoms in BD have the potential to adversely affect its course, outcome, and response to treatment. Somewhat surprisingly, the impact of psychosis on the course and outcome of BD remains unclear despite extensive research on the subject. While some reviews regarding the impact of psychosis on BD have indicated that psychotic BD represents a more severe form of the illness with an adverse course and outcome[9,11,12], the majority of the others have not been able to find an association between psychotic symptoms and outcome in BD[2,3,5,8,13]. Nevertheless, the presence of psychotic symptoms in BD may be of some significance in determining its current nosology[12-14]. Moreover, the similarity of psychotic BD with schizophrenia on genetic, neurobiological, and cognitive aspects indicates common etiological underpinnings of these disorders[14-16]. In both aspects, BD seems to lie in an intermediate position between psychotic and non-psychotic disorders, leading to the hypothesis of a continuum of psychosis stretching from major depressive disorders with psychosis to psychotic BD and schizophrenia[15-18]. Finally, from the clinical perspective, psychotic symptoms have a considerable influence on the way BD is diagnosed and treated. The high prevalence of psychotic symptoms in BD often results in a mistaken diagnosis of schizophrenia. This can lead to inappropriate treatment and can have negative social and economic consequences for those with BD[2,6,8,19]. Moreover, the best way to manage psychotic BD is not clear. Though guidelines emphasize the role of antipsychotics or electroconvulsive therapy, research on adjunctive psychosocial interventions for psychotic symptoms is limited[8,14].
Over the years there have been many reviews of psychotic symptoms in BD including the seminal ones by Goodwin and Jamison[3,5] and by other authors[2,6,9,14,20]. However, there have been very few systematic reviews on the subject. Only three such systematic reviews could be identified. Two of them were primarily focused on hallucinations in BD, unipolar depression, or other disorders[10,21]. Only one systematic review had examined the phenomenology of auditory verbal hallucinations and delusions along with their clinical and cognitive correlates in 32 studies of BD[8].
The current systematic review was specifically intended to address the gaps in the literature regarding psychotic symptoms and their impact on BD. It attempted to comprehensively examine the extent of psychotic symptoms in BD with a particular emphasis on the associations of psychotic symptoms with the course and outcome of BD. For this purpose, it focused on four groups of studies including those of BD [type I (BP I) and type II (BP II) disorders], studies of mania, bipolar depression, and mixed episodes. Four types of psychotic symptoms were examined including delusions, hallucinations, mood-congruent and mood-incongruent symptoms, and FRS. Mood-congruent and incongruent symptoms and FRS were examined separately because these symptoms usually indicate a more severe form of BD and may have a greater impact on its outcome. The impact of psychotic symptoms was determined by exploring the demographic correlates of psychotic symptoms, their clinical correlates, and the influence of psychotic symptoms on different parameters of the course and outcome of BD.
This systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines[22]. Supplementary Table 1 includes the PRISMA 2009 Checklist.
The search for the studies was carried out in 2021. A comprehensive literature search was undertaken using six English-language databases, MEDLINE, PubMed, PsycINFO, EMBASE, Cochrane, and Google, to identify published articles on psychotic symptoms in BD from January 1940 to December 2021. The Reference Citation Analysis (https://www.referencecitationanalysis.com/) was also used to search these databases. The year 1940 was chosen as the inception point because the initial search revealed that very few studies of psychotic symptoms in BD had been conducted before that year. Only two studies from 1931 identified by the manual search were included in the final list of studies.
The following Medical Subject Headings search terms or combinations of these terms were used to search for the relevant studies: BD, mania, depression, psychosis, psychotic, delusions, hallucinations, FRS, mood-congruent symptoms, mood-incongruent symptoms, prevalence, course, and outcome. Supplementary Table 1 includes a list of the search strings used and the results retrieved from the PubMed search.
During the screening phase, all relevant original research articles were identified based on their titles and abstracts. At this stage, articles with no relevant information on the subject, those not in English, reviews, case reports/series, conference abstracts, editorials, and viewpoints were excluded. Full texts of the articles derived from the screening phase were reviewed to determine whether they met the selection criteria. These full texts were also searched manually to identify additional studies.
Inclusion criteria: Studies were included if they: (1) Had examined psychotic symptoms in BD; psychosis was defined as the presence of delusions and/or hallucinations; (2) Had a patient sample that included adult subjects (> 18 years of age); and (3) Had provided information on the relevant aspects of psychotic symptoms in BD including the rates and types of psychotic symptoms, clinical and demographic correlates, or the association with different parameters of outcome.
Exclusion criteria: The following were excluded: (1) Studies providing only qualitative data; (2) Studies where data on psychotic symptoms were not provided separately for BD; (3) Studies of child and adolescent subjects with BD; (4) Studies conducted exclusively among subjects with schizophrenia, schizoaffective disorder, and unipolar depression; and (5) Studies exclusively reporting neurocognitive outcomes of psychosis in BD (these studies were excluded because there are already several systematic reviews and meta-analyses on the subject).
The following data were extracted for each study included in the final list: Authors, year of study, sample size, assessment procedures, results related to the areas of interest, and any indices that estimated the strength of associations, e.g., odds or hazard ratios. The mean, median, and range were estimated for the rates of psychosis and different types of psychotic symptoms. The relationship of psychotic symptoms with the clinical and demographic correlates and outcome parameters was determined based on studies reporting either positive or negative associations. Other aspects, such as the difference between BP I and BP II disorders or between mania, mixed episodes, and depression were also examined.
The STROBE Checklist for cohort, case-control, and cross-sectional studies (combined) was used to rate the quality of studies included in this review[23]. Additional considerations included a sample size of 200 patients (determined by power calculations based on the included studies), the use of standardized interviews to ascertain the diagnosis, the use of validated operational criteria, and the use of validated scales to measure outcomes. Based on these criteria, the studies included in the review were judged to be of good, moderate, or poor quality. The Risk of Bias in Systematic Reviews tool was used to ascertain the risk of bias arising from the quality of included studies, or the methods of this review[24].
To reduce the selection bias arising from included studies as well as the bias in rating the quality of studies, these procedures were initially carried out independently by the two authors. Any discrepancies were resolved by joint consensus following the independent evaluations.
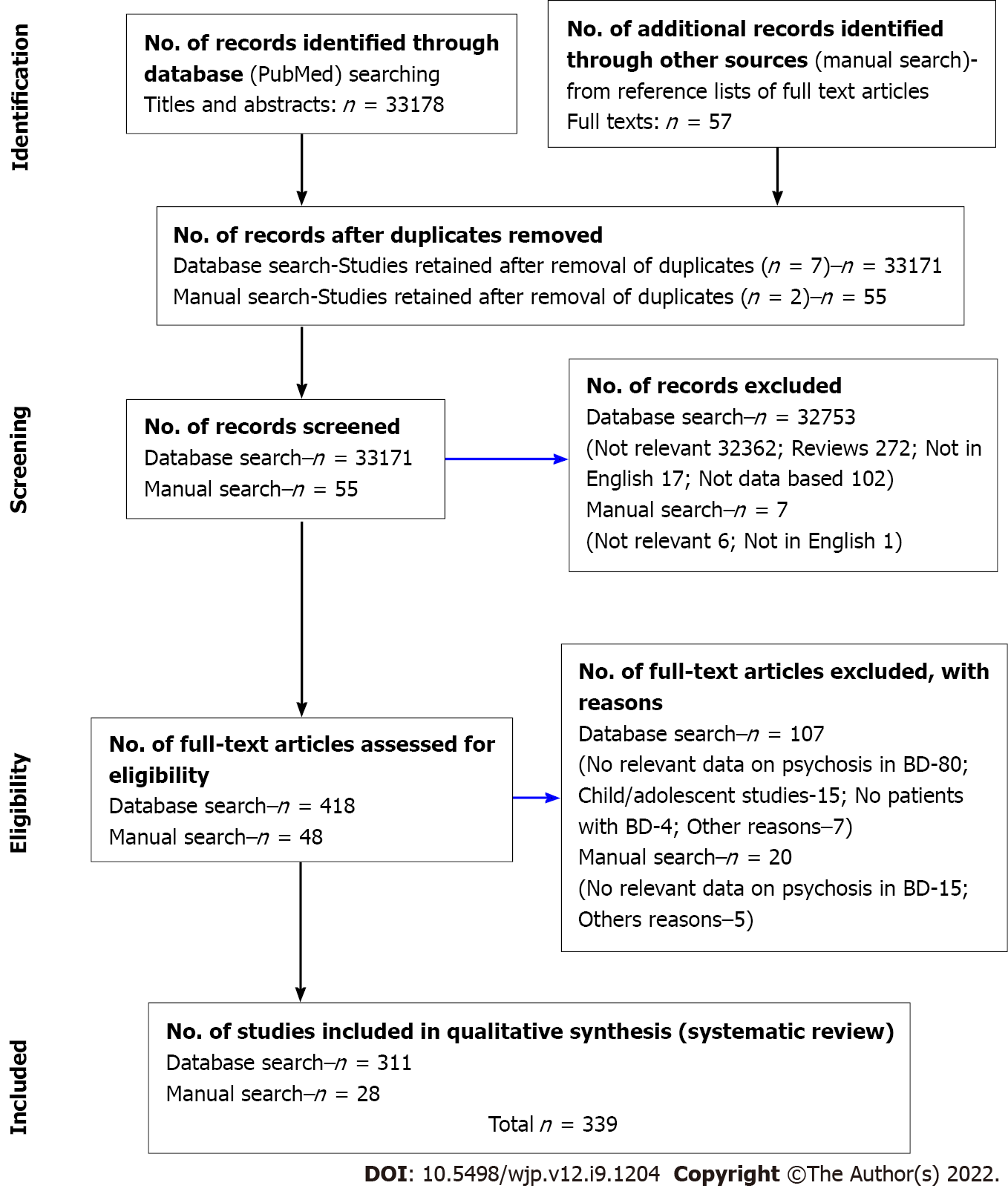
The final list of this review included 339 studies. (These have been cited from reference number 25 to 363[25-363]). Figure 1 shows how these studies were eventually selected. Supplementary Table 2 includes the complete list of these studies with their methodological details. The largest number of studies provided data on patients with current episodes of mania (n = 121), followed by the studies on lifetime psychosis among patients with BD (n = 113), current psychosis in patients with BD (n = 66), bipolar depression (n = 57), and mixed episodes (n = 43). Comparatively fewer studies had provided lifetime data among patients with mania (n = 29), bipolar depression (n = 21), and mixed episodes (n = 8).
Supplementary Table 2 also includes the quality ratings for individual studies. According to these ratings, 97 studies were of good quality, 168 were of moderate quality, and 74 were poor quality studies. Since the majority of studies were of moderate quality, the risk of bias from studies included in this review was moderate to high.
The lifetime and current rates of psychosis for BD, and manic, depressive, and mixed episodes are shown in Table 1. Supplementary Table 3 includes the complete details of these studies.
| Study groups | Lifetime rates | Current rates |
| BD | n = 40, mean 57%; Median 56%; Range: 17%-93% | n = 32, mean 46%; Median 44%; Range: 11%-99% |
| BD I | n = 32, mean 61%; Median 64%; Range: 30%-90% | n = 10, mean 43%; Median 40%; Range: 12%-75% |
| BD II | n = 12, mean 22%; Median 20%; Range: 1%-49% | n = 6, mean 19%; Median 18%; Range: 9%-29% |
| Mania | BD-n = 5, mean 43%; Median 48%; Range: 19%-63% | BD-n = 201, mean 60%; Median 58%; Range: 25%-90% |
| BP I-n = 4, mean 60%; Median 56%; Range: 44%-86% | BP I-n = 51, mean 56%; Median 56%; Range: 8%-91% | |
| Bipolar depression | BD-n = 10, mean 21%; Median 19%; Range: 8%-42% | BD-n = 242, mean 24%; Median 19%; Range: 10%-80% |
| BP I-n = 11, mean 27%; Median 27%; Range: 6%-55% | BP I-n = 12, mean 18%; Median 19%; Range: 3%-28% | |
| BP II-n = 6, mean 15%; Median 10%; Range: 7%-30% | BP II-n = 11, mean 11%; Median 8%; Range: 5%-28% | |
| Mixed episodes | BD-n = 2, mean 50%; Median 50%; Range: 34%-66% | BD-n = 14, mean 47%; Median 40%; Range: 8%-97% |
| BP I-n = 3, mean 43%; Median 33%; Range: 10%-86% | BP I-n = 143, mean 52%; Median 50%; Range: 15%-89% | |
| BP II-n = 2, mean 11%; Median 11%; Range: 7%-15% |
More than half of the patients with BD and about two-thirds of those with BP I disorder had psychotic symptoms during their lifetimes. The lifetime rates of psychosis were about 40%-60% in mania and mixed episodes but only about 20% in the episodes of bipolar depression. The current rates of psychosis were somewhat lower but still in the range of 40%-60% for BD, BP I disorder, mania, and mixed episodes. The current rates of psychosis were less than 20% for bipolar depression. Both the lifetime and current rates of psychosis were about two to three times higher in BP I compared to BP II disorder; this difference was more marked for mixed episodes where the current rates of psychosis in BP I disorder were about five times that of BP II disorder. Lifetime rates of psychosis were about twice as common in mania than in bipolar depression, while the current rates of psychosis were about three times higher in mania compared to bipolar depression. On the other hand, both the lifetime and current rates of psychosis were similar in mania and mixed episodes. Finally, about 60 studies had compared the rates of psychosis in bipolar and unipolar depression. In all but 12 of them, the rates of psychosis were higher in BD than in unipolar disorder. In contrast, 18 of the 20 studies that had compared BD with schizophrenia found much higher rates among patients with schizophrenia. An obvious problem in obtaining an accurate picture of the rates of psychosis was that the average rates tended to get skewed as the number of available studies declined. Though relying on median rates and excluding outliers resolved the problem to an extent, this did not completely correct the imbalance. Thus, the only reliable rates were those for BD, BP I disorder, and the current rates of psychosis in mania.
The lifetime and current rates of the different psychotic symptoms for BD, mania, bipolar depression, and mixed episodes are shown in Table 2. Supplementary Table 4 includes the complete details of these studies.
| Study groups | Delusions | Hallucinations | First-rank symptoms | Mood congruent symptoms | Mood incongruent symptoms |
| Lifetime BD (n = 6-16) | Mean = 69%; Median = 71%; Range: 29%-100% | Mean = 37%; Median = 32%; Range: 13%-100% | Mean = 17%; Median = 11%; Range: 4%-44% | Mean = 49%; Median = 47%; Range: 18%-90% | Mean = 37%; Median = 40%; Range: 3%-76% |
| Lifetime BP I (n = 4-8) | Mean = 55%; Median = 71%; Range: 25%-82% | Mean = 32%; Median = 32%; Range: 23%-43% | Mean = 22%; Median = 25%; Range: 1%-38% | Mean = 37%; Median = 34%; Range: 11%-70% | Mean = 36%; Median = 30%; Range: 19%-66% |
| Lifetime BP II (n = 0-1) | Mean = 4%; Median = 4%; Range: 4% | Mean = 1%; Median = 1%; Range: 1% | - | - | - |
| Current BD (n = 2-13) | Mean = 54%; Median = 49%; Range: 16%-99% | Mean = 26%; Median = 19%; Range: 10%-58% | Mean = 26%; Median = 24%; Range: 5%-49% | Mean = 39%; Median = 39% Range: 24%-35% | Mean = 42%; Median = 46%; Range: 8%-75% |
| Current BP I (n = 1) | - | - | - | Mean = 68%; Median = 68%; Range: 68% | Mean = 32%; Median = 32%; Range: 32% |
| Current BP II | - | - | - | - | - |
| Lifetime mania (n = 1-5) | BD and BP I Mean = 77%; Median = 77%; Range: 33%-98% | BD and BP I Mean = 83%; Median = 83%; Range: 55%-100% | Only BP I Mean = 45%; Median = 45%; Range: 34%-59% | Only BD Mean = 87%; Median = 87%; Range: 87% | Only BP I Mean = 74%; Median = 74% Range: 74% |
| Current mania (n = 8-25) | BD and BP I Mean = 57%; Median = 62%; Range: 11%-87% | BD and BP I Mean = 35%; Median = 41%; Range: 10%-55% | BD and BP I Mean = 28%; Median = 32%; Range: 6%-48% | BD and BP I Mean = 41%; Median = 36%; Range: 20%-87% | BD and BP I Mean = 34%; Median = 36%; Range: 9%-64% |
| Lifetime bipolar depression (n = 1-3) | BD and BP I Mean = 16%; Median = 16%; Range: 10%-20% | BD and BP I Mean = 25%; Median = 25%; Range: 4%-73% | Only BP I Mean = 18%; Median = 18%; Range: 18% | Only BD Mean = 100%; Median = 100%; Range: 100% | - |
| Current bipolar depression (n = 2-13)1 | BD and BP I Mean = 28%; Median = 22%; Range: 6%-97% | BD and BP I Mean = 14%; Median = 9%; Range: 7%-73% | Only BD Mean = 14%; Median = 14%; Range: 8%-20% | BD and BP I Mean = 54%; Median = 54%; Range: 7%-100% | BD and BP I Mean = 7%; Median = 6%; Range: 0-32% |
| Lifetime mixed episodes (n = 0-3) | Only BD Mean = 66%; Median = 66%; Range: 33%-100% | Only BD Mean = 55%; Median = 55%; Range: 10%-100% | - | BD and BP I Mean = 64%; Median = 64%; Range: 28%-100% | Only BP I Mean = 72%; Median = 72%; Range: 72% |
| Current mixed episodes (n = 2- 8) | BD and BP I Mean = 55%; Median = 53%; Range: 19%-90% | BD and BP I Mean = 38%; Median = 38%; Range: 23%-67% | Only BP I Mean = 32%; Median = 32%; Range: 16%-49% | BD and BP I Mean = 27%; Median = 28%; Range: 14%-37% | BD and BP I Mean = 41%; Median = 39%; Range: 22%-63% |
Predictably, there was greater variability in the rates of the four types of psychotic symptoms. The number of studies from which these rates were derived was also smaller, ranging from 1 to 25. However, certain consistent trends could still be made out.
The average rates of delusions ranged from 44%-87% (median: 43%-87%) with the highest rates being obtained for a lifetime and current psychosis in BD, BP I disorder, mania, and mixed episodes. The average rates of delusions in bipolar depression were much less, ranging from 12%-20% in a lifetime and current episodes. In contrast, hallucinations were reported only in about a third of the patients, except for those with lifetime episodes of mania and mixed states where rates ranged from 55%-100%. However, the high rates in these two groups were probably because of the small number of studies involved. The number of studies was also small for bipolar depression, and the average rates were about 22% (median: 19%), with greater variability across individual studies. The lifetime rates of delusions and hallucinations in patients with BP I disorder far exceeded the rates among those with BP II disorder.
The rates of FRS were high, particularly for the studies of lifetime mania (mean and median: 45%, range up to 59%), current mania (mean: 28%, median: 32%, range up to 48%), and current mixed episodes (mean and median: 32%, range up to 49%). About a fifth of the patients with BD and BP I disorder also reported FRS during psychotic episodes, whereas the average rates in bipolar depression were somewhat lower. None of the studies of patients with BP II disorder reported FRS. However, apart from the current mania group, the number of studies was too small in the other groups to obtain an accurate estimate of the rates.
Mood-congruent psychotic symptoms were far more frequent and were present in about a third to half of the patients. Though some groups such as patients with current BP I disorder, lifetime depression, and lifetime mixed episodes reported very high rates of mood congruence, the number of studies was too small for these rates to be reliable. Mood-incongruent psychotic symptoms were usually reported by about a third of the patients (mean: 33%; median: 37%) apart from two exceptions. Rates were very high (72%-74%) for the lifetime mania and mixed groups, but these were based only on one or two studies. On the other hand, the rates in six studies of current bipolar depression were less than 10%. No studies of BP II disorder reported mood-congruent or incongruent symptoms. Finally, the difficulties of ascertaining mood congruence were reflected by the fact that nine studies had found that about 14% of the patients (range 2%-55%) had both types of symptoms simultaneously.
The different types of delusions, hallucinations, and FRS found in BD are shown in Tables 3-5. Supplementary Tables 5-7 include the complete details of these studies.
| Delusions | Grandiose | Referential | Persecutory | Erotomanic | Jealousy | Somatic | Depressive | Religious |
| Lifetime BD and BP I (n = 11) | Mean (n = 7) 52%; Median 61%; Range: 24%-69% | Mean (n = 3) 59%; Median 61%; Range: 54%-62% | Mean (n = 9) 40%; Median 40%; Range: 16%-56% | - | Mean (n = 2) 8%; Median 8%; Range: 3%-13% | - | Mean (n = 2) 13%; Median 13%; Range: 12%-15% | Mean (n = 1) 35%; Median 35%; Range: 35% |
| Current BD (n = 9) | Mean (n = 9) 36%; Median 39%; Range: 4%-75% | Mean (n = 3) 42%; Median 5%; Range: 5%-75% | Mean (n = 8) 35%; Median 30%; Range: 7%-71% | Mean (n = 2) 4%; Median 4%; Range: 4% | - | Mean (n = 3) 16%; Median 11%; Range: 7%-31% | Mean (n = 7) 9%; Median 6%; Range: 3%-36% | Mean (n = 2) 5%; Median 5%; Range: 5% |
| Lifetime mania (N = 3) | Mean (n = 3) 66%; Median 69%; Range: 41%-88% | - | Mean (n = 3) 21%; Median 21%; Range: 12%-30% | - | Mean (n = 1) 2%; Median 2%; Range: 2% | Mean (n = 2) 16%; Median 16%; Range: 16% | Mean (n = 2) 10%; Median 7%; Range: 7%-13% | Mean (n =1) 3%; Median 3%; Range: 3% |
| Current mania (n = 23) | Mean (n = 17) 57%; Median 59%; Range: 20%-80% | Mean (n = 7) 43%; Median 41%; Range: 14%-69% | Mean (n = 20) 46%; Median 47%; Range: 8%-90% | Mean (n = 4) 29%; Median 24%; Range: 9%-61% | Mean (n = 1) 3%; Median 3%; Range: 3% | Mean (n = 5) 15%; Median 13%; Range: 1%-35% | Mean (n = 3) 10%; Median 10%; Range: 6%-14% | Mean (n = 7) 27%; Median 27%; Range: 22%-31% |
| Lifetime depression (n = 2) | - | - | Mean (n = 2) 17%; Median 17%; Range: 15%-20 | - | - | - | - | - |
| Current depression (n = 5) | - | Mean (n = 2) 32%; Median 32%; Range: 32%-33% | Mean (n = 4) 37%; Median 39%; Range: 1%-7% | - | Mean (n = 1) 20%; Median 20%; Range: 20% | Mean (n = 1) 17%; Median 17%; Range: 17% | Mean (n = 3) 12%; Median 7%; Range: 3%-30% | - |
| Lifetime mixed (n = 1) | - | - | Mean (n = 1) 33%; Median 33%; Range: 33% | - | Mean (n = 1) 33%; Median 33%; Range: 33% | - | - | - |
| Current mixed (n = 4) | Mean (n = 3) 42%; Median 41%; Range: 19%-66% | Mean (n = 2) 71%; Median 71%; Range: 56%-86% | Mean (n = 4) 46%; Median 31%; Range: 16%-90% | - | - | Mean (n = 3) 7%; Median 10%; Range: 7%-13% | Mean (n = 2) 19%; Median 19%; Range: 6%-33% | - |
| Overall rates | Mean (n = 39) 51%; Median 54%; Range: 4%-88% | Mean (n = 17) 49%; Median 42%; Range: 5%-86% | Mean (n = 52) 34%; Median 32%; Range: 1%-90% | Mean (n = 6) 16%; Median 14%; Range: 4%-61% | Mean (n = 6) 13%; Median 13%; Range: 3%-33% | Mean (n = 14) 14%; Median 13%; Range: 1%-35% | Mean (n = 19) 12%; Median 10%; Range: 3%-36% | Mean (n = 11)18%; Median 17%; Range: 3%-42% |
| Hallucinations | Auditory/AVH | Visual | Tactile | Olfactory | Gustatory | Somatic | Others |
| Lifetime BD and BP I (n = 13) | Mean (n = 13) 26%; Median 24%; Range: 3%-52% | Mean (n = 10) 23%; Median 23%; Range: 9%-47% | Mean (n = 1) 16%; Median 16%; Range: 16% | - | - | - | Mean (n = 3) Median 12%; 9%; Range: 3%-13% |
| Current BD (n = 3) | Mean (n = 3) 17%; Median 17%; Range: 8%-17% | Mean (n = 2) 6%; Median 6%; Range: 3%-9% | Mean (n = 1) 0.3%; Median 0.3%; Range: 0.3% | Mean (n = 2) 1%; Median 1%; Range: 1% | Mean (n = 2) 1%; Median 1%; Range: 1% | Mean (n = 2) 2%; Median 2%; Range: 0.4%-3% | - |
| Lifetime mania (n = 3) | Mean (n = 3) 40%; Median 39%; Range: 22%-52% | Mean (n = 1) 25%; Median 25%; Range: 25% | - | - | - | Mean (n = 1) 11%; Median 11%; Range: 11% | - |
| Current mania (n = 18) | Mean (n = 17) 33%; Median 41%; Range: 12%-57% | Mean (n = 8) 20%; Median 17%; Range: 2%-61% | Mean (n =2) 4%; Median 4%; Range: 3%-5% | Mean (n = 2) 8%; Median 8%; Range: 6%-13% | - | Mean (n = 2) 11%; Median 11%; Range: 1%-21% | Mean (n = 5) 27%; Median 28%; Range: 7%-46% |
| Lifetime depression (n = 2) | Mean (n = 2) 40%; Median 40%; Range: 13%-67% | Mean (n = 1) 7%; Median 7%; Range: 7% | - | - | - | - | Mean (n = 2) 18%; Median 18%; Range: 4%-33% |
| Current depression (n = 6) | Mean (n = 6) 16%; Median 9%; Range: 4%-50% | Mean (n = 3) 5%; Median 3%; Range: 1%-11% | - | Mean (n = 1) 0.5%; Median 0.5%; Range: 0.5% | Mean (n = 1) 0.5%; Median 0.5%; Range: 0.5% | - | Mean (n = 1) 2%; Median 2%; Range: 2% |
| Lifetime mixed (n = 1) | Mean (n = 1) 33%; Median 33%; Range: 33% | - | - | - | - | - | - |
| Current mixed (n = 3) | Mean (n = 3) 37%; Median 41%; Range: 4%-67% | Mean (n = 3) 13%; Median 18%; Range: 2%-20% | Mean (n = 1) 5%; Median 5%; Range: 5% | - | Mean (n = 1) 0.5%; Median 0.5%; Range: 0.5% | Mean (n = 1) 2%; Median 2%; Range: 2% | Mean (n = 1) 6%; Median 6%; Range: 6% |
| Overall rates | Mean (n = 48) 30%; Median 30%; Range: 3%-67% | Mean (n = 28) 14%; Median 13%; Range: 3%-47% | Mean (n = 1) 6%; Median 6%; Range: 0.3%- 16% | Mean (n = 5) 3%; Median 3%; Range: 1%- 16% | Mean (n = 4) 1%; Median 1%; Range: 0.5%-1% | Mean (n = 5) 8%; Median 8%; Range: 0.4%- 47% | Mean (n = 10) 12%; Median 1%; Range: 1%- 46% |
| Study groups | Passivity/control | Delusional perception | Somatic passivity | Thought broadcast | Thought insertion | Thought withdrawal | Running commentary | Two or more voices conversing | Thought echo |
| Lifetime BD and BP I (n = 9) | Mean (n = 4) 10%; Median 11%; Range: 4%-16% | Mean (n = 1) 20%; Median 20%; Range: 20% | - | Mean (n = 3) 11%; Median 14%; Range: 3%-17% | Mean (n = 1) 20%; Median 20%; Range: 20% | Mean (n = 1) 4%; Median 4%; Range: 4% | Mean (n = 4) 17%; Median 17%; Range: 10%-27% | Mean (n = 4) 16%; Median 17%; Range: 5%-27% | Mean (n = 1) 13%; Median 13%; Range: 13% |
| Current BD (n = 4) | Mean (n = 2) 36%; Median 36%; Range: 18%-49% | Mean (n = 2) 6%; Median 6%; Range: 2%-10% | Mean (n = 1) 7%; Median 7%; Range: 7% | Mean (n = 3) 14%; Median 5%; Range: 5%-18% | Mean (n = 1) 5%; Median 5%; Range: 5% | Mean (n = 1) 2%; Median 2%; Range: 2% | Mean (n = 2) 20%; Median 20%; Range: 4%-37% | Mean (n = 2)12%; Median 12%; Range: 4%-20% | Mean (n = 1) 4%; Median 4%; Range: 4% |
| Lifetime mania (n = 2) | Mean (n = 2) 27%; Median 27%; Range: 3%-52% | - | - | Mean (n = 1) 6%; Median 6%; Range: 6% | Mean (n = 1) 4%; Median 4%; Range: 4% | Mean (n = 1) 3%; Median 3%; Range: 3% | Mean (n = 1) 1%; Median 1%; Range: 1% | Mean (n = 1) 1%; Median 1%; Range: 1% | Mean (n = 2) 14%; Median 14%; Range: 14%-15% |
| Current mania (n = 8) | Mean (n = 8) 23%; Median 20%; Range: 5%-48% | - | - | Mean (n = 5) 12%; Median 14%; Range: 2%-21% | Mean (n = 3) 9%; Median 7%; Range: 1%-18% | Mean (n = 3) 9%; Median 3%; Range: 3%-13% | Mean (n = 3) 9%; Median 3%; Range: 2%-14% | Mean (n = 3) 5%; Median 3%; Range: 2%-6% | Mean (n = 3) 5%; Median 2%; Range: 1%-12% |
| Lifetime depression (n = 1) | Mean (n = 1) 1%; Median 1%; Range: 1% | - | - | Mean (n = 1) 1%; Median 1%; Range: 1% | Mean (n = 1) 1%; Median 1%; Range: 1% | Mean (n = 1) 4%; Median 4%; Range: 4% | - | - | Mean (n = 1) 10%; Median 10%; Range: 10% |
| Current depression (n = 1) | - | - | - | - | - | - | - | Mean (n = 1) 17%; Median 17% | - |
| Current mixed (n = 1) | Mean (n = 1) 49%; Median 49%; Range: 49% | - | - | - | - | - | - | - | |
| Overall rates | Mean (n = 18) 24%; Median 24%; Range: 1%-49% | Mean (n = 3) 13%; Median 13%; Range: 2%-20% | Mean (n = 1) 7%; Median 7%; Range: 7% | Mean (n = 17) 9%; Median 8%; Range: 1%-18% | Mean (n = 7) 8%; Median 7%; Range: 1%-20% | Mean (n = 7) 4%; Median 3%; Range: 2%-13% | Mean (n = 10) 12%; Median 10%; Range: 1%-20% | Mean (n = 11) 10%; Median 10%; Range: 1%-27% | Mean (n = 8) 9%; Median 9%; Range: 4%-15% |
The number of studies from which these rates were derived was generally small, apart from certain exceptions such as those reporting grandiose and persecutory delusions and auditory and visual hallucinations. Very few studies had examined the different types of FRS.
Nevertheless, it appeared that both grandiose and referential delusions were equally common in BD, particularly among patients with mania. Persecutory delusions were present in about a third of the patients with BD and were almost equally common in the groups with mania, depression, or mixed episodes. Other common delusions included religious and erotomanic delusions; both were more common in mania and mixed episodes. Somatic delusions, delusional jealousy, and depressive delusions, particularly delusions of guilt were found in all phases. Auditory hallucinations, especially auditory verbal hallucinations, were the most frequent types of hallucinations reported in BD and were equally common across all the groups. Visual hallucinations were much less common and found more frequently in mania. Other types of hallucinations were rare including somatic, tactile, olfactory, and gustatory hallucinations. Among the FRS, passivity delusions were the most common, followed by delusional perception, “running commentary” type of hallucinations, “voices conversing,” thought echo, thought broadcast, thought insertion, somatic passivity, and thought withdrawal. As expected, the rates of all FRS were more common in mania, BD, and BP I disorders.
Demographic correlates of psychosis in BD are included in Table 6. Supplementary Table 8 includes the complete details of these studies. The results showed that there were very few consistent associations of psychotic symptoms with sociodemographic variables in BD. Many studies (n = 27) had not found significant relationships between psychotic BD and any of the demographic characteristics. Moreover, when significant associations were found with demographic parameters in some of the studies, an equal number of studies usually reported contrary results. Finally, the number of studies that had failed to find significant associations of psychosis with individual demographic parameters far outweighed the studies that had found positive associations.
| Correlates | Studies showing positive association with psychosis | Studies showing inverse association or no association with psychosis1 |
| Younger age | n = 14 | n = 48 |
| Female sex | n = 16 | n = 51 |
| Single status | n = 11 | n = 14 |
| Lower educational levels | n = 9 | n = 26 |
| Low income or unemployment | n = 6 | n = 14 |
| Ethnic minority status | n = 4 | n = 10 |
| Severity of psychotic symptoms in bipolar disorder | ||
| Studies showing that psychotic symptoms are less severe in bipolar disorder | Studies showing that psychotic symptoms are more severe in bipolar disorder | |
| n = 20 | n = 20 | |
| Severity of illness/mood symptoms in psychotic bipolar disorder | ||
| Studies showing that the illness/mood symptoms are not more severe in psychotic bipolar disorder | Studies showing that severity of illness/mood symptoms is greater in psychotic bipolar disorder | |
| n = 16 | n = 34 | |
| Insight and psychotic symptoms in bipolar disorder | ||
| Studies showing that psychosis is associated with lack of insight in bipolar disorder | Studies showing that psychosis is not associated with lack of insight in bipolar disorder | |
| n = 15 | n = 9 | |
| Agitation, aggression and anxiety in psychotic bipolar disorder | ||
| Studies showing that agitation, aggression and anxiety are associated with psychosis in bipolar disorder | Studies showing that agitation, aggression and anxiety are not associated with psychosis in bipolar disorder | |
| n = 13 | n = 2 | |
| Comorbidity and psychotic symptoms in bipolar disorder | ||
| Studies showing that psychosis associated with greater comorbidity in bipolar disorder | Studies showing that psychosis is not associated with greater comorbidity in bipolar disorder | |
| n = 21 | n = 27 | |
Clinical correlates of psychosis in BD are also shown in Table 6. Supplementary Table 9 includes the complete details of these studies.
(1) The severity of psychosis and severity of illness in psychotic BD. Whether psychotic BD represents a more severe form of the illness has been examined by three groups of studies. The first group examined the severity of psychosis in BD relative to schizophrenia and unipolar depression. The number of studies showing that psychotic symptoms were either less or more severe in BD was exactly equal suggesting that the severity of psychotic symptoms in BD was no different from the other patient groups with psychosis. The second group of studies focused on the association between psychotic symptoms and the overall severity of BD or the severity of manic and depressive symptoms. Here, the number of studies showing that the severity of illness or mood symptoms was greater in psychotic BD outnumbered those that did not find a difference. This indicated that the overall severity of the illness and severity of acute episodes was greater in psychotic BD. However, about a third of these studies had found this to be true only for the severity of manic symptoms. Therefore, the association between severe mood symptoms and psychotic BD was largely applicable to patients with current manic episodes. The third group of studies had examined the severity of BD with psychosis in terms of its impact on the course and outcome of the disorder. These are discussed later.
(2) Other indicators of severity. There was some evidence that psychotic BD was associated with poorer insight and a higher frequency of symptoms of agitation, aggression, and anxiety. Then again, this finding was also derived from the studies of mania, where agitation, violence, lack of insight, and psychosis often co-occurred. On the other hand, the rates of psychiatric comorbidity did not appear to be greater in those with psychotic BD.
The impact of psychosis on the different aspects of the course and outcome of BD is summarized in Table 7. Supplementary Table 10 includes the complete details of these studies.
| Outcome measure | Studies with positive association with psychosis in bipolar disorder | Studies with negative or no association with psychosis in bipolar disorder |
| Poor overall outcome | n = 38 | n = 39 |
| Earlier age of onset | n = 30 | n = 36 |
| Persistent or chronic course of illness | n = 23 | n = 18 |
| Lack of remission or lack of recovery | n = 12 | n = 15 |
| More frequent relapses or recurrences | n =5 | n = 5 |
| Greater number of mood episodes | n = 13 | n = 19 |
| Lower proportion with rapid cycling | n = 6 | n = 6 |
| Longer duration of illness | n = 5 | n = 23 |
| Manic polarity of illness | n = 9 | n = 6 |
| Seasonal pattern of illness | n = 2 | n = 2 |
| More frequent hospitalizations or longer hospital stays | n =26 | n = 15 |
| Poor functioning, poor quality of life, or poor functional outcome | n = 45 | n = 46 |
| More frequent suicidal attempts or heightened suicidal behavior | n = 14 | n = 35 |
| Good response to lithium treatment | n = 5 | n = 10 |
| Switch to diagnosis of bipolar disorder | n = 10 | - |
| Poorer outcome with mood-incongruent psychotic symptoms | n = 21 | n = 13 |
| Poorer outcome with first-rank symptoms | n = 3 | n = 9 |
The overall conclusion from these studies was that psychotic BD was not inevitably associated with a more adverse course and poorer outcome of BD. While several studies had found psychosis was associated with a poorer overall outcome, the number of those that had failed to find such an association was almost the same or even more. This trend also appeared to be true for several individual measures of outcome including earlier age of onset, a persistent or chronic course of the illness, lack of remission or recovery, more frequent relapses or recurrences, a greater number of lifetime mood episodes, poor functioning, poor quality of life, and poor functional outcome. Since a large number of studies with reasonable methodological quality had examined these outcome parameters, this lent further support to the notion that psychosis was not always associated with poor outcomes in BD. Moreover, studies that had estimated odds or hazard ratios also showed that psychotic symptoms were not associated with earlier age of onset, poorer functional, or poorer overall outcomes[51,159,256,313,355]. Though some of the studies based on similar estimations of risk had found adverse outcomes in psychotic BD[103,104,137,157], the positive association of psychosis with poor outcomes in these studies was usually found only in a few outcome measures and not in others[64,250,288,342].
Additionally, negative associations between psychosis and outcome were reported in other domains such as the manic polarity of BD, a seasonal pattern of the illness, the response to lithium treatment, and a poorer outcome with FRS. However, these findings were uncertain because of the small number of studies involved.
Finally, psychosis appeared to be linked to better outcomes in three other areas including a lower proportion of rapid cycling, a shorter duration of illness, and a lowered suicidal risk. The negative association with suicidal behavior appeared to be particularly strong based on the number of studies and estimations of risk[40,57,105,306].
Nevertheless, psychosis appeared to be more consistently linked with adverse outcomes in some of the other areas. The rate and the duration of hospitalizations were consistently higher among patients with psychotic BD. Some studies had found the risk of hospitalization to be about one and a half times in psychotic BD[209]. Patients with depression were more likely to switch to BD if they had psychotic symptoms. Though this finding was based on only ten studies, some of them had estimated the risk to be between one and a half to two times based on odds ratios[186,216,222]. Lastly, the number of studies that found mood-incongruent psychotic symptoms to be associated with a poorer outcome was considerably more than those that had not found such an association.
The current systematic review examined the extent of psychotic symptoms in BD and their impact on the course and outcome of BD based on the 339 studies that were selected. Before focusing on its findings, it is imperative to understand the strengths and weaknesses of the studies included in this review.
This review showed that there is no dearth of studies on the subject of psychotic symptoms in BD. Moreover, almost every aspect such as the prevalence of psychotic symptoms, their correlates, and the impact of psychosis on the course and outcome of BD have been systematically assessed by a number of these studies. However, the existing literature has several methodological shortcomings that often make it difficult to reach firm conclusions.
The studies covered a period from 1940 to 2021, during which the definition of BD has undergone many changes. Thus, there may be some difficulty in equating labels such as manic-depressive psychoses and BD. However, there were only minor differences between the definitions in older studies and the current definitions of the disorder. Moreover, leaving out studies conducted before the 1980s would have resulted in a significant loss of data. Psychosis has usually been defined as the presence of delusions and/or hallucinations by most studies. Though this definition fits the current standards and is easily established by using structured interviews[364], a few studies have included formal thought disorder as a part of the definition[142]. This complicates matters since thought disorder is relatively non-specific and more difficult to ascertain. Nevertheless, the broader definition seems to be commonly used[365], while the narrower one has its critics[366]. The method of assessment also had a bearing on the results of the studies. Although the majority of the studies had used structured interviews and validated scales to assess psychotic symptoms, some especially the older ones had not. However, rather than the assessment method, the inadequate sample size of most of the studies compromised their methodological adequacy. Moreover, almost all studies included hospital-based patients. The lack of community studies hinders the generalization of these findings to patients with BD in real-world settings. These lacunae in the quality of most of the studies included in the review raise the possibility of a moderate to high risk of bias in the findings of this review. The variability in results could also result from the lack of control for potential confounders such as age[159,321], sex[357,367], mood state[8], comorbidity[162], and chronicity of the illness[46]. Although multivariate statistics have been used in many studies to control for these factors, risk estimates are only offered by a few of them, and the estimation of the strength of associations by calculating effect sizes is rare. Finally, there was a lack of studies examining the descriptive and subjective aspects of psychotic symptoms in BD[8].
As a consequence of the methodological variability across the studies, some of the findings of this review were more reliable than the others.
One of the more reliable findings was the very high rates of psychotic symptoms in BD. In keeping with the earlier reviews, more than half of the patients with BD, mania, or mixed episodes developed such symptoms during their lifetimes[2,3,5,14,89]. Current rates of psychosis were also high and found in a little less than half of these patients. In contrast, earlier reviews have reported that about a third of the patients have psychotic symptoms during their current episodes[6,368].
Like the earlier reports, psychosis was much more common in mania and mixed episodes than in bipolar depression[3,5,8]. Psychosis was about twice as common in BP I compared to BP II disorder. Despite the smaller number of studies of patients with BP II disorder, this has been a consistent finding in the existing literature[3]. This could be because psychosis can be present only during depressive episodes in BP II disorder according to the current definitions or because of the lower severity of illness in this subtype[44,62]. In agreement with the earlier reviews[3-5], a large number of studies found the rates of psychosis to be much higher in bipolar compared to unipolar depression. However, the rates of psychosis were usually lower than those found in schizophrenia[6-8].
The rates of different types of psychotic symptoms were somewhat less reliable, principally because of the smaller number of studies involved. Nevertheless, the trends were similar to the existing reports. Thus, delusions were far more frequent than hallucinations in all phases of BD[2,3,5,8,10]. The higher rates in mania compared to bipolar depression and BP I compared to BP II disorder were also in keeping with the previous reviews[3,8-10,368]. Though based on the smallest number of studies, about a third of the patients reported experiencing FRS, particularly during acute manic episodes. This was almost equal to the rates of FRS reported in the existing literature[2,3,8,10]. Similar to the earlier reports, mood-congruent psychotic symptoms were more common among patients with BD[2,3,6,8,10]. As found in these reviews, mood-incongruent symptoms were reported in about a third of the patients with BD, and the rates were highest for those with mania. However, because of the small number of studies and the difficulties in ascertaining mood congruence, the validity of these findings is questionable. Similarly, the findings regarding the different types of delusions, hallucinations, and FRS were also based on very few studies but conformed to what has been reported earlier[3,5,8,10,89].
One of the principal objectives of this review was to examine the impact of psychosis on the course, outcome, clinical correlates, and demographic profile of BD. The findings of this aspect of the current review proved to be the most reliable since they were based on the largest number of studies, which were of moderate to good quality. Moreover, taken together these studies had carried out a comprehensive examination of different facets of BD that could be impacted by the presence of psychosis. The overall conclusion of this section of the review was that psychotic BD is not always associated with a negative impact on the illness. This reflected the continuing debate about the prognostic implications of psychosis in BD, with some reviews concluding that psychosis is associated with a poorer prognosis[9,11,12,89], whereas the majority have found an uncertain impact of psychosis on BD[2,3,5,8,46].
In line with the other reviews[3,8,10], the current one found few consistent associations of psychotic symptoms in BD with sociodemographic variables. Thus, the case for psychosis being associated with an adverse demographic profile[89] was not proven. The findings concerning the clinical correlates were more equivocal. As reported earlier[3,10,13], psychotic symptoms were not more severe in BD, particularly when compared to schizophrenia. On the other hand and in keeping with the existing evidence[2,3,12,89], the severity of the illness in psychotic BD appeared to be consistently greater. However, this finding was largely based on manic symptom severity, which tends to be inevitably higher than the other phases of BD[2]. Moreover, the genesis of psychotic symptoms is likely to be only partly mediated by clinical severity and partly by other factors such as early-onset, shorter duration of illness, comorbid conditions, and sex[8]. Psychosis was associated with a lack of insight, particularly during severe manic episodes. Then again, because most patients regain insight once mania resolves, the extent of impaired insight was less among patients with psychotic mania compared to those with schizophrenia[61,161]. Psychosis was also associated with a more frequent occurrence of agitation, anxiety, and hostility, but this association could be a consequence rather than the cause of psychosis in BD[8]. Finally, comorbid disorders were less common in psychotic BD, which was in agreement with the other reviews[3].
There was greater uncertainty about the impact of psychosis on the other parameters of course and outcome. The number of studies reporting poorer overall outcomes in psychotic BD was no different from those that failed to find such a relationship. Moreover, there was no consistent association between psychotic symptoms and earlier age of onset, lack of remission and recovery, more frequent relapses and recurrences, the persistence of psychosis, poorer functional outcomes, and lithium response. Lastly, psychosis was less likely to be associated with a rapid-cycling course, longer duration of illness, and heightened suicidal behavior. This emulated the uncertainty in the existing literature regarding the associations of psychosis in BD with an earlier age of onset[2,89,369-371], a poorer long-term course[2,3,8,46,89], impaired functioning[88,367,372,373], more frequent suicide attempts[3,374,375], more frequent rapid-cycling course[46], predominant manic polarity[376], and lithium response[2,6,89,377]. The lack of impact on functioning was surprising but not unexpected. The existing literature suggests that though a significant proportion of the patients with BD have impaired functional and social outcomes, this does not appear to be mediated by the presence of psychotic symptoms[83,141].
Nevertheless, psychosis was associated with poor outcomes in three domains. Psychosis was associated with a higher risk of switching to BD, which is known to occur in about a fifth of the patients with depression[8]. Psychotic symptoms were also associated with more frequent hospitalizations and longer hospital stays, which has been noted by other reviews[9]. Finally, mood-incongruent symptoms appeared to be associated with poorer overall outcomes. Most of the earlier reviews have reported both positive and negative associations of mood-congruent symptoms with outcome[2,3,6,46,250]. However, the most comprehensive review on the subject found that though mood-incongruent symptoms were associated with poor outcomes, the differences between psychotic and non-psychotic BD were small and rarely significant[378]. Moreover, in line with the existing evidence, the current review also found that psychotic BD had a better outcome than schizophrenia[7,11].
The current systematic review has shown that there is no paucity of evidence on the subject of psychotic symptoms in BD. However, because of methodological shortcomings of the evidence, there are few consistent and reliable findings. One of them was the high prevalence of psychotic symptoms and the other was the lack of an adverse impact of psychosis on several domains of BD, including its course and outcome. These findings together with the genetic, neurobiological, and neurocognitive evidence suggest that psychotic BD lies on a continuum between non-psychotic forms of the disorder and schizophrenia[379-382]. Mood-incongruent psychotic BD, which is a severe form of BD overlaps with schizophrenia, whereas non-psychotic BD is similar to unipolar disorders[17,18,79,383]. The evidence from this review thus supports the current classification of BD as lying in an intermediate position between unipolar depression and schizophrenia[1]. Finally, from the clinicians’ perspective, this review suggests that greater awareness and understanding of this subject is needed so that psychotic BD can be properly diagnosed and adequately treated in routine practice.
Psychotic symptoms are very common in bipolar disorder (BD) and have the potential to adversely affect its course, outcome, and treatment. However, despite the considerable amount of research and several reviews on the subject, the impact of psychotic symptoms on the course and outcome of BD remains unclear. Moreover, there are very few systematic reviews on the impact of psychosis in BD.
The lack of information about the impact of psychotic symptoms in BD in existing literature prompted the current systematic review. Moreover, it was prompted by the possibility that the presence of such symptoms in BD and their impact on the illness may have significant etiological, nosological, and clinical implications.
The current systematic review was specifically intended to address the gaps in the literature regarding psychotic symptoms in BD. Therefore, it aimed to examine psychotic symptoms in BD and their impact on several domains of BD. This review focused on four groups of studies and four types of psychotic symptoms. The impact of psychotic symptoms was determined by exploring demographic correlates of psychotic symptoms, their clinical correlates, and the influence of psychotic symptoms on different parameters of course and outcome of BD.
This systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines. It undertook an electronic search supplemented by a manual one. Articles were selected in two phases: Screening of abstracts and review of full texts. The methodological quality of the studies and the risk of bias were ascertained by standard tools.
This systematic review included 339 studies of BD. The results endorsed the high rates of all types of psychotic symptoms found in BD. More than a half to two-thirds of the patients experienced psychosis during their lifetimes. Current psychosis was found in a little less than half of these patients. Delusions were more common than hallucinations. About a third of the patients had first-rank symptoms or mood-incongruent psychotic symptoms. Psychotic symptoms were more frequent in bipolar type I disorder, and in mania or mixed episodes. However, psychosis was associated with an adverse impact only in a few domains of the illness including the severity of BD, lack of insight, more frequent occurrence of agitation, anxiety, and hostility, the rate of and the duration of hospitalizations, switch to BD among patients with depression, and poorer outcomes with mood-incongruent symptoms. No consistent associations were found in other areas, suggesting that psychosis is not always associated with a negative impact on BD. This finding conformed to the current consensus in the literature on psychotic BD.
Though psychotic symptoms are very common in BD, they are not always associated with an adverse impact on BD and its course and outcome.
The ongoing debate about the impact of psychosis in BD is yet to be resolved. Studies with more improved methodology are needed to ascertain the true impact of psychotic symptoms in several domains of BD.
| 1. | American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Association, 2013: 152. |
| 2. | Dunayevich E, Keck PE Jr. Prevalence and description of psychotic features in bipolar mania. Curr Psychiatry Rep. 2000;2:286-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 136] [Article Influence: 5.2] [Reference Citation Analysis (1)] |
| 3. | Goodwin FK, Jamison KR. Manic-Depressive illness: bipolar disorder and recurrent depression. New York: Oxford University Press, 2007: 29-118. |
| 4. | Dubovsky SL, Ghosh BM, Serotte JC, Cranwell V. Psychotic Depression: Diagnosis, Differential Diagnosis, and Treatment. Psychother Psychosom. 2021;90:160-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 123] [Article Influence: 24.6] [Reference Citation Analysis (0)] |
| 5. | Goodwin FK, Jamison KR. Manic-depressive illness. New York: Oxford University Press, 1990. |
| 6. | Pope HG Jr, Lipinski JF Jr. Diagnosis in schizophrenia and manic-depressive illness: a reassessment of the specificity of 'schizophrenic' symptoms in the light of current research. Arch Gen Psychiatry. 1978;35:811-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 398] [Cited by in RCA: 320] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 7. | Ketter TA, Wang PW, Becker OV, Nowakowska C, Yang Ys. Psychotic bipolar disorders: dimensionally similar to or categorically different from schizophrenia? J Psychiatr Res. 2004;38:47-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 52] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 8. | Smith LM, Johns LC, Mitchell R. Characterizing the experience of auditory verbal hallucinations and accompanying delusions in individuals with a diagnosis of bipolar disorder: A systematic review. Bipolar Disord. 2017;19:417-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Fountoulakis KN, Young A, Yatham L, Grunze H, Vieta E, Blier P, Moeller HJ, Kasper S. The International College of Neuropsychopharmacology (CINP) Treatment Guidelines for Bipolar Disorder in Adults (CINP-BD-2017), Part 1: Background and Methods of the Development of Guidelines. Int J Neuropsychopharmacol. 2017;20:98-120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Toh WL, Thomas N, Rossell SL. Auditory verbal hallucinations in bipolar disorder (BD) and major depressive disorder (MDD): A systematic review. J Affect Disord. 2015;184:18-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 72] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 11. | Kempf L, Hussain N, Potash JB. Mood disorder with psychotic features, schizoaffective disorder, and schizophrenia with mood features: trouble at the borders. Int Rev Psychiatry. 2005;17:9-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 56] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Vieta E, Phillips ML. Deconstructing bipolar disorder: a critical review of its diagnostic validity and a proposal for DSM-V and ICD-11. Schizophr Bull. 2007;33:886-892. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 103] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 13. | Colom F, Vieta E. The road to DSM-V. Bipolar disorder episode and course specifiers. Psychopathology. 2009;42:209-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 14. | Henry C, Etain B. New ways to classify bipolar disorders: going from categorical groups to symptom clusters or dimensions. Curr Psychiatry Rep. 2010;12:505-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 47] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 15. | Bora E. Neurocognitive features in clinical subgroups of bipolar disorder: A meta-analysis. J Affect Disord. 2018;229:125-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 144] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 16. | Bora E, Yücel M, Pantelis C. Cognitive impairment in affective psychoses: a meta-analysis. Schizophr Bull. 2010;36:112-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 93] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 17. | Carpenter WT, Bustillo JR, Thaker GK, van Os J, Krueger RF, Green MJ. The psychoses: cluster 3 of the proposed meta-structure for DSM-V and ICD-11. Psychol Med. 2009;39:2025-2042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 62] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 18. | Goldberg DP, Andrews G, Hobbs MJ. Where should bipolar disorder appear in the meta-structure? Psychol Med. 2009;39:2071-2081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 19. | Meyer F, Meyer TD. The misdiagnosis of bipolar disorder as a psychotic disorder: some of its causes and their influence on therapy. J Affect Disord. 2009;112:174-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 69] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 20. | Akiskal HS, Puzantian VR. Psychotic forms of depression and mania. Psychiatr Clin North Am. 1979;2:419-439. [RCA] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 46] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Waters F, Fernyhough C. Hallucinations: A Systematic Review of Points of Similarity and Difference Across Diagnostic Classes. Schizophr Bull. 2017;43:32-43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 199] [Cited by in RCA: 202] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 22. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52948] [Cited by in RCA: 48670] [Article Influence: 2862.9] [Reference Citation Analysis (3)] |
| 23. | Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M; STROBE initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Ann Intern Med. 2007;147:W163-W194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 849] [Cited by in RCA: 1450] [Article Influence: 76.3] [Reference Citation Analysis (0)] |
| 24. | Whiting P, Savović J, Higgins JP, Caldwell DM, Reeves BC, Shea B, Davies P, Kleijnen J, Churchill R; ROBIS group. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225-234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 718] [Cited by in RCA: 1469] [Article Influence: 133.5] [Reference Citation Analysis (0)] |
| 25. | Rennie TA. Prognosis in manic-depressive psychoses. Am J Psychiatry. 1942;98:801-814. [DOI] [Full Text] |
| 26. | Astrup C, Fossum A, Holmboe R. Outcome of the disease in manic-depressive psychoses. Acta Psychiatr Scand. 1959;34 (Suppl 135):13-24. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 27. | Rosenthal NE, Rosenthal LN, Stallone F, Fleiss J, Dunner DL, Fieve RR. Psychosis as a predictor of response to lithium maintenance treatment in bipolar affective disorder. J Affect Disord. 1979;1:237-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | Rosenthal NE, Rosenthal LN, Stallone F, Dunner DL, Fieve RR. Toward the validation of RDC schizoaffective disorder. Arch Gen Psychiatry. 1980;37:804-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 43] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 29. | Rosen LN, Rosenthal NE, Van Dusen PH, Dunner DL, Fieve RR. Age at onset and number of psychotic symptoms in bipolar I and schizoaffective disorder. Am J Psychiatry. 1983;140:1523-1524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 43] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 30. | Rosen LN, Rosenthal NE, Dunner DL, Fieve RR. Social outcome compared in psychotic and nonpsychotic bipolar I patients. J Nerv Ment Dis. 1983;171:272-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 31. | Winokur G. Psychosis in bipolar and unipolar affective illness with special reference to schizo-affective disorder. Br J Psychiatry. 1984;145:236-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 24] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 32. | Winokur G, Scharfetter C, Angst J. Stability of psychotic symptomatology (delusions, hallucinations), affective syndromes, and schizophrenic symptoms (thought disorder, incongruent affect) over episodes in remitting psychoses. Eur Arch Psychiatry Neurol Sci. 1985;234:303-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 31] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 33. | Endicott J, Nee J, Coryell W, Keller M, Andreasen N, Croughan J. Schizoaffective, psychotic, and nonpsychotic depression: differential familial association. Compr Psychiatry. 1986;27:1-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 34. | Dell'Osso L, Placidi GF, Nassi R, Freer P, Cassano GB, Akiskal HS. The manic-depressive mixed state: familial, temperamental and psychopathologic characteristics in 108 female inpatients. Eur Arch Psychiatry Clin Neurosci. 1991;240:234-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 77] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 35. | Vieta E, Gastó C, Otero A, Nieto E, Vallejo J. Differential features between bipolar I and bipolar II disorder. Compr Psychiatry. 1997;38:98-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 141] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 36. | Gonzalez-Pinto A, Gutierrez M, Mosquera F, Ballesteros J, Lopez P, Ezcurra J, Figuerido JL, de Leon J. First episode in bipolar disorder: misdiagnosis and psychotic symptoms. J Affect Disord. 1998;50:41-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 60] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 37. | Kirov G, Murray RM. Ethnic differences in the presentation of bipolar affective disorder. Eur Psychiatry. 1999;14:199-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 34] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 38. | Perugi G, Micheli C, Akiskal HS, Madaro D, Socci C, Quilici C, Musetti L. Polarity of the first episode, clinical characteristics, and course of manic depressive illness: a systematic retrospective investigation of 320 bipolar I patients. Compr Psychiatry. 2000;41:13-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 134] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 39. | Benabarre A, Vieta E, Colom F, Martínez-Arán A, Reinares M, Gastó C. Bipolar disorder, schizoaffective disorder and schizophrenia: epidemiologic, clinical and prognostic differences. Eur Psychiatry. 2001;16:167-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 73] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 40. | Lopez P, Mosquera F, de Leon J, Gutierrez M, Ezcurra J, Ramurez F, Gonzalez-Pinto A. Suicide attempts in bipolar patients. J Clin Psychiatry. 2001;62:963-966. [RCA] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 99] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 41. | Suppes T, Leverich GS, Keck PE, Nolen WA, Denicoff KD, Altshuler LL, McElroy SL, Rush AJ, Kupka R, Frye MA, Bickel M, Post RM. The Stanley Foundation Bipolar Treatment Outcome Network. II. Demographics and illness characteristics of the first 261 patients. J Affect Disord. 2001;67:45-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 315] [Cited by in RCA: 310] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 42. | Tsai SM, Chen C, Kuo C, Lee J, Lee H, Strakowski SM. 15-year outcome of treated bipolar disorder. J Affect Disord. 2001;63:215-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 43. | Judd LL, Akiskal HS, Schettler PJ, Endicott J, Maser J, Solomon DA, Leon AC, Rice JA, Keller MB. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry. 2002;59:530-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1361] [Cited by in RCA: 1390] [Article Influence: 57.9] [Reference Citation Analysis (0)] |
| 44. | Serretti A, Mandelli L, Lattuada E, Cusin C, Smeraldi E. Clinical and demographic features of mood disorder subtypes. Psychiatry Res. 2002;112:195-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 45. | Hammersley P, Dias A, Todd G, Bowen-Jones K, Reilly B, Bentall RP. Childhood trauma and hallucinations in bipolar affective disorder: preliminary investigation. Br J Psychiatry. 2003;182:543-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 144] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 46. | Keck PE Jr, McElroy SL, Havens JR, Altshuler LL, Nolen WA, Frye MA, Suppes T, Denicoff KD, Kupka R, Leverich GS, Rush AJ, Post RM. Psychosis in bipolar disorder: phenomenology and impact on morbidity and course of illness. Compr Psychiatry. 2003;44:263-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 137] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 47. | Yildiz A, Sachs GS. Age onset of psychotic versus non-psychotic bipolar illness in men and in women. J Affect Disord. 2003;74:197-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 48. | Cassano GB, Rucci P, Frank E, Fagiolini A, Dell'Osso L, Shear MK, Kupfer DJ. The mood spectrum in unipolar and bipolar disorder: arguments for a unitary approach. Am J Psychiatry. 2004;161:1264-1269. [PubMed] |
| 49. | Ernst CL, Goldberg JF. Clinical features related to age at onset in bipolar disorder. J Affect Disord. 2004;82:21-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 63] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 50. | Mantere O, Suominen K, Leppämäki S, Valtonen H, Arvilommi P, Isometsä E. The clinical characteristics of DSM-IV bipolar I and II disorders: baseline findings from the Jorvi Bipolar Study (JoBS). Bipolar Disord. 2004;6:395-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 103] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 51. | Perlis RH, Miyahara S, Marangell LB, Wisniewski SR, Ostacher M, DelBello MP, Bowden CL, Sachs GS, Nierenberg AA; STEP-BD Investigators. Long-term implications of early onset in bipolar disorder: data from the first 1000 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD). Biol Psychiatry. 2004;55:875-881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 581] [Cited by in RCA: 600] [Article Influence: 27.3] [Reference Citation Analysis (6)] |
| 52. | Angst J, Angst F, Gerber-Werder R, Gamma A. Suicide in 406 mood-disorder patients with and without long-term medication: a 40 to 44 years' follow-up. Arch Suicide Res. 2005;9:279-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 199] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 53. | Perlis RH, Delbello MP, Miyahara S, Wisniewski SR, Sachs GS, Nierenberg AA, STEP-BD investigators. Revisiting depressive-prone bipolar disorder: polarity of initial mood episode and disease course among bipolar I Systematic Treatment Enhancement Program for Bipolar Disorder Participants. Biol Psychiatry. 2005;58:549-553. [RCA] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 62] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 54. | Daban C, Colom F, Sanchez-Moreno J, García-Amador M, Vieta E. Clinical correlates of first-episode polarity in bipolar disorder. Compr Psychiatry. 2006;47:433-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 108] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 55. | Engh JA, Friis S, Birkenaes AB, Jónsdóttir H, Ringen PA, Ruud T, Sundet KS, Opjordsmoen S, Andreassen OA. Measuring cognitive insight in schizophrenia and bipolar disorder: a comparative study. BMC Psychiatry. 2007;7:71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 63] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 56. | Selva G, Salazar J, Balanzá-Martínez V, Martínez-Arán A, Rubio C, Daban C, Sánchez-Moreno J, Vieta E, Tabarés-Seisdedos R. Bipolar I patients with and without a history of psychotic symptoms: do they differ in their cognitive functioning? J Psychiatr Res. 2007;41:265-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 78] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 57. | Valtonen HM, Suominen K, Haukka J, Mantere O, Leppämäki S, Arvilommi P, Isometsä ET. Differences in incidence of suicide attempts during phases of bipolar I and II disorders. Bipolar Disord. 2008;10:588-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 88] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 58. | Hamshere ML, Schulze TG, Schumacher J, Corvin A, Owen MJ, Jamra RA, Propping P, Maier W, Orozco y Diaz G, Mayoral F, Rivas F, Jones I, Jones L, Kirov G, Gill M, Holmans PA, Nöthen MM, Cichon S, Rietschel M, Craddock N. Mood-incongruent psychosis in bipolar disorder: conditional linkage analysis shows genome-wide suggestive linkage at 1q32.3, 7p13 and 20q13.31. Bipolar Disord. 2009;11:610-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 59. | Suominen K, Mantere O, Valtonen H, Arvilommi P, Leppämäki S, Isometsä E. Gender differences in bipolar disorder type I and II. Acta Psychiatr Scand. 2009;120:464-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 50] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 60. | Derks EM, Allardyce J, Boks MP, Vermunt JK, Hijman R, Ophoff RA; GROUP. Kraepelin was right: a latent class analysis of symptom dimensions in patients and controls. Schizophr Bull. 2012;38:495-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 61. | Hammersley P, Taylor K, McGovern J, Kinderman P. Attributions for hallucinations in bipolar affective disorder. Behav Cogn Psychother. 2010;38:221-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 62. | Mazzarini L, Colom F, Pacchiarotti I, Nivoli AM, Murru A, Bonnin CM, Cruz N, Sanchez-Moreno J, Kotzalidis GD, Girardi P, Tatarelli R, Vieta E. Psychotic versus non-psychotic bipolar II disorder. J Affect Disord. 2010;126:55-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 42] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 63. | Ozyildirim I, Cakir S, Yazici O. Impact of psychotic features on morbidity and course of illness in patients with bipolar disorder. Eur Psychiatry. 2010;25:47-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 64. | Solomon DA, Leon AC, Coryell WH, Endicott J, Li C, Fiedorowicz JG, Boyken L, Keller MB. Longitudinal course of bipolar I disorder: duration of mood episodes. Arch Gen Psychiatry. 2010;67:339-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 104] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 65. | Souery D, Zaninotto L, Calati R, Linotte S, Sentissi O, Amital D, Moser U, Kasper S, Zohar J, Mendlewicz J, Serretti A. Phenomenology of psychotic mood disorders: lifetime and major depressive episode features. J Affect Disord. 2011;135:241-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 66. | Simonsen C, Sundet K, Vaskinn A, Birkenaes AB, Engh JA, Faerden A, Jónsdóttir H, Ringen PA, Opjordsmoen S, Melle I, Friis S, Andreassen OA. Neurocognitive dysfunction in bipolar and schizophrenia spectrum disorders depends on history of psychosis rather than diagnostic group. Schizophr Bull. 2011;37:73-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 233] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 67. | Baldessarini RJ, Tondo L, Vazquez GH, Undurraga J, Bolzani L, Yildiz A, Khalsa HM, Lai M, Lepri B, Lolich M, Maffei PM, Salvatore P, Faedda GL, Vieta E, Tohen M. Age at onset versus family history and clinical outcomes in 1,665 international bipolar-I disorder patients. World Psychiatry. 2012;11:40-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 146] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 68. |
Eissa MF, ElGhoniemy S, Hamed D, Omar A-N, Morsy M.
The quality of life in patients with bipolar disorder who have achieved remission in an Egyptian sample: |
| 69. | Finseth PI, Morken G, Andreassen OA, Malt UF, Vaaler AE. Risk factors related to lifetime suicide attempts in acutely admitted bipolar disorder inpatients. Bipolar Disord. 2012;14:727-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 70. | Aminoff SR, Hellvin T, Lagerberg TV, Berg AO, Andreassen OA, Melle I. Neurocognitive features in subgroups of bipolar disorder. Bipolar Disord. 2013;15:272-283. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 71. | Prieto ML, McElroy SL, Hayes SN, Sutor B, Kung S, Bobo WV, Fuentes ME, Cuellar-Barboza AB, Crow S, Ösby U, Chauhan M, Westman J, Geske JR, Colby CL, Ryu E, Biernacka JM, Frye MA. Association between history of psychosis and cardiovascular disease in bipolar disorder. Bipolar Disord. 2015;17:518-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 72. | Upthegrove R, Chard C, Jones L, Gordon-Smith K, Forty L, Jones I, Craddock N. Adverse childhood events and psychosis in bipolar affective disorder. Br J Psychiatry. 2015;206:191-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 54] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 73. | Gesi C, Carmassi C, Miniati M, Benvenuti A, Massimetti G, Dell'Osso L. Psychotic spectrum symptoms across the lifespan are related to lifetime suicidality among 147 patients with bipolar I or major depressive disorder. Ann Gen Psychiatry. 2016;15:15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 74. | Perlman G, Kotov R, Fu J, Bromet EJ, Fochtmann LJ, Medeiros H; Genomic Psychiatry Cohort Consortium; Pato MT, Pato CN. Symptoms of psychosis in schizophrenia, schizoaffective disorder, and bipolar disorder: a comparison of African Americans and Caucasians in the Genomic Psychiatry Cohort. Am J Med Genet B Neuropsychiatr Genet. 2016;171:546-555. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 75. | de Silva LFAL, Loureiro JC, Franco SCR, Santos ML, Secolin R, Lopes-Cendes I, Dantas CR, Banzato CEM. Assessing treatment response to prophylactic lithium use in patients with bipolar disorder. J Bras Psiquiatr. 2016;65:9-16. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 76. | Dell'Osso B, Camuri G, Cremaschi L, Dobrea C, Buoli M, Ketter TA, Altamura AC. Lifetime presence of psychotic symptoms in bipolar disorder is associated with less favorable socio-demographic and certain clinical features. Compr Psychiatry. 2017;76:169-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 77. | Serafini G, Geoffroy PA, Aguglia A, Adavastro G, Canepa G, Pompili M, Amore M. Irritable temperament and lifetime psychotic symptoms as predictors of anxiety symptoms in bipolar disorder. Nord J Psychiatry. 2018;72:63-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 78. | Tondo L, Vázquez GH, Baldessarini RJ. Depression and Mania in Bipolar Disorder. Curr Neuropharmacol. 2017;15:353-358. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 116] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 79. | Allardyce J, Leonenko G, Hamshere M, Pardiñas AF, Forty L, Knott S, Gordon-Smith K, Porteous DJ, Haywood C, Di Florio A, Jones L, McIntosh AM, Owen MJ, Holmans P, Walters JTR, Craddock N, Jones I, O'Donovan MC, Escott-Price V. Association Between Schizophrenia-Related Polygenic Liability and the Occurrence and Level of Mood-Incongruent Psychotic Symptoms in Bipolar Disorder. JAMA Psychiatry. 2018;75:28-35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 91] [Cited by in RCA: 86] [Article Influence: 10.8] [Reference Citation Analysis (1)] |
| 80. | Altamura AC, Buoli M, Cesana B, Dell'Osso B, Tacchini G, Albert U, Fagiolini A, de Bartolomeis A, Maina G, Sacchetti E. Socio-demographic and clinical characterization of patients with Bipolar Disorder I vs II: a Nationwide Italian Study. Eur Arch Psychiatry Clin Neurosci. 2018;268:169-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 81. | Belteczki Z, Rihmer Z, Ujvari J, Lamis DA, Dome P. Differences in clinical characteristics between bipolar patients with current psychotic symptoms and those who have never been psychotic. Psychiatr Danub. 2018;30:183-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 82. | Bowie CR, Best MW, Depp C, Mausbach BT, Patterson TL, Pulver AE, Harvey PD. Cognitive and functional deficits in bipolar disorder and schizophrenia as a function of the presence and history of psychosis. Bipolar Disord. 2018;20:604-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 83. | Burton CZ, Ryan KA, Kamali M, Marshall DF, Harrington G, McInnis MG, Tso IF. Psychosis in bipolar disorder: Does it represent a more "severe" illness? Bipolar Disord. 2018;20:18-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 84. | Markota M, Coombes BJ, Larrabee BR, McElroy SL, Bond DJ, Veldic M, Colby CL, Chauhan M, Cuellar-Barboza AB, Fuentes M, Kung S, Prieto ML, Rummans TA, Bobo WV, Frye MA, Biernacka JM. Association of schizophrenia polygenic risk score with manic and depressive psychosis in bipolar disorder. Transl Psychiatry. 2018;8:188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 85. | Sanchez-Moreno J, Bonnin CM, González-Pinto A, Amann BL, Solé B, Balanzá-Martinez V, Arango C, Jiménez E, Tabarés-Seisdedos R, Garcia-Portilla MP, Ibáñez A, Crespo JM, Ayuso-Mateos JL, Martinez-Aran A, Torrent C, Vieta E; CIBERSAM Functional Remediation Group. Factors associated with poor functional outcome in bipolar disorder: sociodemographic, clinical, and neurocognitive variables. Acta Psychiatr Scand. 2018;138:145-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 86. | Sánchez-Morla EM, López-Villarreal A, Jiménez-López E, Aparicio AI, Martínez-Vizcaíno V, Roberto RJ, Vieta E, Santos JL. Impact of number of episodes on neurocognitive trajectory in bipolar disorder patients: a 5-year follow-up study. Psychol Med. 2019;49:1299-1307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 87. | Altamura AC, Buoli M, Cesana BM, Fagiolini A, de Bartolomeis A, Maina G, Bellomo A, Dell'Osso B; ISBD Italian Chapter Epidemiological Group. Psychotic versus non-psychotic bipolar disorder: Socio-demographic and clinical profiles in an Italian nationwide study. Aust N Z J Psychiatry. 2019;53:772-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 88. | Bonnín CM, Jiménez E, Solé B, Torrent C, Radua J, Reinares M, Grande I, Ruíz V, Sánchez-Moreno J, Martínez-Arán A, Vieta E. Lifetime Psychotic Symptoms, Subthreshold Depression and Cognitive Impairment as Barriers to Functional Recovery in Patients with Bipolar Disorder. J Clin Med. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 89. | van Bergen AH, Verkooijen S, Vreeker A, Abramovic L, Hillegers MH, Spijker AT, Hoencamp E, Regeer EJ, Knapen SE, Riemersma-van der Lek RF, Schoevers R, Stevens AW, Schulte PFJ, Vonk R, Hoekstra R, van Beveren NJ, Kupka RW, Sommer IEC, Ophoff RA, Kahn RS, Boks MPM. The characteristics of psychotic features in bipolar disorder. Psychol Med. 2019;49:2036-2048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 90. | Drakopoulos J, Sparding T, Clements C, Pålsson E, Landén M. Executive functioning but not IQ or illness severity predicts occupational status in bipolar disorder. Int J Bipolar Disord. 2020;8:7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 91. | Bowman KM, Raymond AF. A statistical study of delusions in the manic-depressive psychoses. Am J Psychiatry. 1931;88:111-121. [DOI] [Full Text] |
| 92. | Bowman KM, Raymond AF. A statistical study of hallucinations in the manic-depressive psychoses. Am J Psychiatry. 1931;88:299-309. [DOI] [Full Text] |
| 93. | Blumenthal RL, Egeland JA, Sharpe L, Nee J, Endicott J. Age of onset in bipolar and unipolar illness with and without delusions or hallucinations. Compr Psychiatry. 1987;28:547-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 94. | Guze SB, Woodruff RA Jr, Clayton PJ. The significance of psychotic affective disorders. Arch Gen Psychiatry. 1975;32:1147-1150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 64] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 95. | Jones BE, Robinson WM, Parson EB, Gray BA. The clinical picture of mania in manic-depressive black patients. J Natl Med Assoc. 1982;74:553-557. [PubMed] |
| 96. | Jørgensen P. Manic-depressive patients with delusions. Clinical and diagnostic course. Acta Psychiatr Scand. 1985;72:364-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 97. | Black DW, Winokur G, Bell S, Nasrallah A, Hulbert J. Complicated mania. Comorbidity and immediate outcome in the treatment of mania. Arch Gen Psychiatry. 1988;45:232-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 58] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 98. | Mitterauer B, Leibetseder M, Pritz WF, Sorgo G. Comparisons of psychopathological phenomena of 422 manic-depressive patients with suicide-positive and suicide-negative family history. Acta Psychiatr Scand. 1988;77:438-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 99. | Black DW, Nasrallah A. Hallucinations and delusions in 1,715 patients with unipolar and bipolar affective disorders. Psychopathology. 1989;22:28-34. [RCA] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 48] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 100. | Lenzi A, Rinaldi A, Bianco I, Balestri C, Marazziti D. Psychotic symptoms in mood disorders: Evaluation of 159 inpatients. Eur Psychiatry. 1996;11:396-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 101. | Coryell W, Turvey C, Endicott J, Leon AC, Mueller T, Solomon D, Keller M. Bipolar I affective disorder: predictors of outcome after 15 years. J Affect Disord. 1998;50:109-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 88] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 102. | Wylie ME, Mulsant BH, Pollock BG, Sweet RA, Zubenko GS, Begley AE, Gregor M, Frank E, Reynolds CF 3rd, Kupfer DJ. Age at onset in geriatric bipolar disorder. Effects on clinical presentation and treatment outcomes in an inpatient sample. Am J Geriatr Psychiatry. 1999;7:77-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 103. | Tohen M, Hennen J, Zarate CM Jr, Baldessarini RJ, Strakowski SM, Stoll AL, Faedda GL, Suppes T, Gebre-Medhin P, Cohen BM. Two-year syndromal and functional recovery in 219 cases of first-episode major affective disorder with psychotic features. Am J Psychiatry. 2000;157:220-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 346] [Cited by in RCA: 346] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 104. | Tohen M, Strakowski SM, Zarate C Jr, Hennen J, Stoll AL, Suppes T, Faedda GL, Cohen BM, Gebre-Medhin P, Baldessarini RJ. The McLean-Harvard first-episode project: 6-month symptomatic and functional outcome in affective and nonaffective psychosis. Biol Psychiatry. 2000;48:467-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 108] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 105. | Grunebaum MF, Oquendo MA, Harkavy-Friedman JM, Ellis SP, Li S, Haas GL, Malone KM, Mann JJ. Delusions and suicidality. Am J Psychiatry. 2001;158:742-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 51] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 106. | Pini S, Cassano GB, Dell'Osso L, Amador XF. Insight into illness in schizophrenia, schizoaffective disorder, and mood disorders with psychotic features. Am J Psychiatry. 2001;158:122-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 150] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 107. | Dell'Osso L, Pini S, Cassano GB, Mastrocinque C, Seckinger RA, Saettoni M, Papasogli A, Yale SA, Amador XF. Insight into illness in patients with mania, mixed mania, bipolar depression and major depression with psychotic features. Bipolar Disord. 2002;4:315-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 81] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 108. | Judd LL, Akiskal HS, Schettler PJ, Coryell W, Endicott J, Maser JD, Solomon DA, Leon AC, Keller MB. A prospective investigation of the natural history of the long-term weekly symptomatic status of bipolar II disorder. Arch Gen Psychiatry. 2003;60:261-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 813] [Cited by in RCA: 821] [Article Influence: 35.7] [Reference Citation Analysis (3)] |
| 109. | Appelbaum PS, Robbins PC, Roth LH. Dimensional approach to delusions: comparison across types and diagnoses. Am J Psychiatry. 1999;156:1938-1943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 110. | Depp CA, Jin H, Mohamed S, Kaskow J, Moore DJ, Jeste DV. Bipolar disorder in middle-aged and elderly adults: is age of onset important? J NervMent Dis. 2004;192:796-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 41] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 111. | Baethge C, Baldessarini RJ, Freudenthal K, Streeruwitz A, Bauer M, Bschor T. Hallucinations in bipolar disorder: characteristics and comparison to unipolar depression and schizophrenia. Bipolar Disord. 2005;7:136-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 119] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 112. | Johnson SL, McMurrich SL, Yates M. Suicidality in bipolar I disorder. Suicide Life Threat Behav. 2005;35:681-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 113. | Patel NC, Delbello MP, Keck PE Jr, Strakowski SM. Phenomenology associated with age at onset in patients with bipolar disorder at their first psychiatric hospitalization. Bipolar Disord. 2006;8:91-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 114. | Carlson GA, Kotov R, Chang SW, Ruggero C, Bromet EJ. Early determinants of four-year clinical outcomes in bipolar disorder with psychosis. Bipolar Disord. 2012;14:19-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 115. | Grande I, Goikolea JM, de Dios C, González-Pinto A, Montes JM, Saiz-Ruiz J, Prieto E, Vieta E; PREBIS group. Occupational disability in bipolar disorder: analysis of predictors of being on severe disablement benefit (PREBIS study data). Acta Psychiatr Scand. 2013;127:403-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 116. | Levy B, Medina AM, Weiss RD. Cognitive and psychosocial functioning in bipolar disorder with and without psychosis during early remission from an acute mood episode: a comparative longitudinal study. Compr Psychiatry. 2013;54:618-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 117. | Owoeye O, Kingston T, Scully PJ, Baldwin P, Browne D, Kinsella A, Russell V, O'Callaghan E, Waddington JL. Epidemiological and clinical characterization following a first psychotic episode in major depressive disorder: comparisons with schizophrenia and bipolar I disorder in the Cavan-Monaghan First Episode Psychosis Study (CAMFEPS). Schizophr Bull. 2013;39:756-765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 118. | Xiang YT, Zhang L, Wang G, Hu C, Ungvari GS, Dickerson FB, Kilbourne AM, Si TM, Fang YR, Lu Z, Yang HC, Lai KY, Lee EH, Hu J, Chen ZY, Huang Y, Sun J, Wang XP, Li HC, Zhang JB, Chiu HF. Sociodemographic and clinical features of bipolar disorder patients misdiagnosed with major depressive disorder in China. Bipolar Disord. 2013;15:199-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 119. | Soni A, Singh P, Shah R, Bagotia S. Impact of Cognition and Clinical Factors on Functional Outcome in Patients with Bipolar Disorder. East Asian Arch Psychiatry. 2017;27:26-34. [PubMed] |
| 120. | Picardi A, Fonzi L, Pallagrosi M, Gigantesco A, Biondi M. Delusional Themes Across Affective and Non-Affective Psychoses. Front Psychiatry. 2018;9:132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 121. | Buoli M, Cesana BM, Maina G, Conca A, Fagiolini A, Steardo L Jr, Altamura AC, Dell'Osso B; ISBD Italian Chapter Epidemiologic Group. Correlates of current rapid-cycling bipolar disorder: Results from the Italian multicentric RENDiBi study. Eur Psychiatry. 2019;62:82-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 122. | Gaudiano BA, Uebelacker LA, Miller IW. Course of illness in psychotic mania: is mood incongruence important? J Nerv Ment Dis. 2007;195:226-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 123. | Ostergaard SD, Bertelsen A, Nielsen J, Mors O, Petrides G. The association between psychotic mania, psychotic depression and mixed affective episodes among 14,529 patients with bipolar disorder. J Affect Disord. 2013;147:44-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 124. | Bjørklund LB, Horsdal HT, Mors O, Gasse C, Østergaard SD. Psychopharmacological treatment of psychotic mania and psychotic bipolar depression compared to non-psychotic mania and non-psychotic bipolar depression. Bipolar Disord. 2017;19:505-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 125. | Baek JH, Ha K, Kim Y, Cho YA, Yang SY, Choi Y, Jang SL, Park T, Ha TH, Hong KS. Psychopathologic structure of bipolar disorders: exploring dimensional phenotypes, their relationships, and their associations with bipolar I and II disorders. Psychol Med. 2019;49:2177-2185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 126. | Clayton PJ, Pitts FN Jr. Affect disorder. IV. Mania. Compr Psychiatry. 1965;6:313-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 54] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 127. | Carlson GA, Goodwin FK. The stages of mania. A longitudinal analysis of the manic episode. Arch Gen Psychiatry. 1973;28:221-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 186] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 128. | Taylor MA, Abrams R. The phenomenology of mania. A new look at some old patients. Arch Gen Psychiatry. 1973;29:520-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 120] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 129. | Abrams R, Taylor MA, Gaztanaga P. Manic-depressive illness and paranoid schizophrenia. A phenomenologic, family history, and treatment-response study. Arch Gen Psychiatry. 1974;31:640-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 42] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 130. | Taylor MA, Gaztanaga P, Abrams R. Manic-depressive illness and acute schizophrenia: a clinical, family history, and treatment-response study. Am J Psychiatry. 1974;131:678-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 52] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 131. | Taylor MA, Abrams R. Acute mania. Clinical and genetic study of responders and nonresponders to treatments. Arch Gen Psychiatry. 1975;32:863-865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 51] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 132. | Leff JP, Fischer M, Bertelsen A. A cross-national epidemiological study of mania. Br J Psychiatry. 1976;129:428-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 85] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 133. | Loudon JB, Blackburn IM, Ashworth CM. A study of the symptomatology and course of manic illness using a new scale. Psychol Med. 1977;7:723-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 134. | Dion GL, Tohen M, Anthony WA, Waternaux CS. Symptoms and functioning of patients with bipolar disorder six months after hospitalization. Hosp Community Psychiatry. 1988;39:652-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 31] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 135. | Chatterjee S, Kulhara P. Symptomatology, symptom resolution and short term course in mania. Indian J Psychiatry. 1989;31:213-218. [PubMed] |
| 136. | Chaturvedi SK, Sinha VK. Recurrence of hallucinations in consecutive episodes of schizophrenia and affective disorder. Schizophr Res. 1990;3:103-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 137. | Tohen M, Waternaux CM, Tsuang MT. Outcome in Mania. A 4-year prospective follow-up of 75 patients utilizing survival analysis. Arch Gen Psychiatry. 1990;47:1106-1111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 367] [Cited by in RCA: 320] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 138. | Grossman LS, Harrow M, Goldberg JF, Fichtner CG. Outcome of schizoaffective disorder at two long-term follow-ups: comparisons with outcome of schizophrenia and affective disorders. Am J Psychiatry. 1991;148:1359-1365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 42] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 139. | Sethi S, Khanna R. Phenomenology of mania in eastern India. Psychopathology. 1993;26:274-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 140. | Dilsaver SC, Chen YW, Swann AC, Shoaib AM, Krajewski KJ. Suicidality in patients with pure and depressive mania. Am J Psychiatry. 1994;151:1312-1315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 126] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 141. | Goldberg JF, Harrow M, Grossman LS. Course and outcome in bipolar affective disorder: a longitudinal follow-up study. Am J Psychiatry. 1995;152:379-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 219] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 142. | Dilsaver SC, Chen YW, Swann AC, Shoaib AM, Tsai-Dilsaver Y, Krajewski KJ. Suicidality, panic disorder and psychosis in bipolar depression, depressive-mania and pure-mania. Psychiatry Res. 1997;73:47-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 114] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 143. | Khess CR, Das J, Akhtar S. Four year follow-up of first episode manic patients. Indian J Psychiatry. 1997;39:160-165. [PubMed] |
| 144. | MacQueen GM, Young LT, Robb JC, Cooke RG, Joffe RT. Levels of functioning and well-being in recovered psychotic versus nonpsychotic mania. J Affect Disord. 1997;46:69-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 29] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 145. | McElroy SL, Strakowski SM, West SA, Keck PE Jr, McConville BJ. Phenomenology of adolescent and adult mania in hospitalized patients with bipolar disorder. Am J Psychiatry. 1997;154:44-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 60] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 146. | Perugi G, Akiskal HS, Micheli C, Musetti L, Paiano A, Quilici C, Rossi L, Cassano GB. Clinical subtypes of bipolar mixed states: validating a broader European definition in 143 cases. J Affect Disord. 1997;43:169-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 163] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 147. | Akiskal HS, Hantouche EG, Bourgeois ML, Azorin JM, Sechter D, Allilaire JF, Lancrenon S, Fraud JP, Châtenet-Duchêne L. Gender, temperament, and the clinical picture in dysphoric mixed mania: findings from a French national study (EPIMAN). J Affect Disord. 1998;50:175-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 195] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 148. | Cassidy F, Murry E, Forest K, Carroll BJ. Signs and symptoms of mania in pure and mixed episodes. J Affect Disord. 1998;50:187-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 130] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 149. | Peralta V, Cuesta MJ. Lack of insight in mood disorders. J Affect Disord. 1998;49:55-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 79] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 150. | Robinson AD. A century of delusions in south west Scotland. Br J Psychiatry. 1988;153:163-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 151. | Strakowski SM, Keck PE Jr, Sax KW, McElroy SL, Hawkins JM. Twelve-month outcome of patients with DSM-III-R schizoaffective disorder: comparisons to matched patients with bipolar disorder. Schizophr Res. 1999;35:167-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 152. | Strakowski SM, Williams JR, Fleck DE, Delbello MP. Eight-month functional outcome from mania following a first psychiatric hospitalization. J Psychiatr Res. 2000;34:193-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 153. | Coryell W, Leon AC, Turvey C, Akiskal HS, Mueller T, Endicott J. The significance of psychotic features in manic episodes: a report from the NIMH collaborative study. J Affect Disord. 2001;67:79-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 99] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 154. | Swann AC, Janicak PL, Calabrese JR, Bowden CL, Dilsaver SC, Morris DD, Petty F, Davis JM. Structure of mania: depressive, irritable, and psychotic clusters with different retrospectively-assessed course patterns of illness in randomized clinical trial participants. J Affect Disord. 2001;67:123-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 91] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 155. | Wright BM. Variation of intravenous infusion rates. Br Med J. 1975;2:69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 156. | Kauer-Sant'Anna M, Bond DJ, Lam RW, Yatham LN. Functional outcomes in first-episode patients with bipolar disorder: a prospective study from the Systematic Treatment Optimization Program for Early Mania project. Compr Psychiatry. 2009;50:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 55] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 157. | Tohen M, Zarate CA Jr, Hennen J, Khalsa HM, Strakowski SM, Gebre-Medhin P, Salvatore P, Baldessarini RJ. The McLean-Harvard First-Episode Mania Study: prediction of recovery and first recurrence. Am J Psychiatry. 2003;160:2099-2107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 317] [Cited by in RCA: 326] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 158. | Kennedy N, Boydell J, van Os J, Murray RM. Ethnic differences in first clinical presentation of bipolar disorder: results from an epidemiological study. J Affect Disord. 2004;83:161-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 159. | Kessing LV. Subtypes of manic episodes according to ICD-10-prediction of time to remission and risk of relapse. J Affect Disord. 2004;81:279-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 160. | Kessing LV. Gender differences in the phenomenology of bipolar disorder. Bipolar Disord. 2004;6:421-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 68] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 161. | Pini S, de Queiroz V, Dell'Osso L, Abelli M, Mastrocinque C, Saettoni M, Catena M, Cassano GB. Cross-sectional similarities and differences between schizophrenia, schizoaffective disorder and mania or mixed mania with mood-incongruent psychotic features. Eur Psychiatry. 2004;19:8-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 76] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 162. | Azorin JM, Akiskal H, Hantouche E. The mood-instability hypothesis in the origin of mood-congruent versus mood-incongruent psychotic distinction in mania: validation in a French National Study of 1090 patients. J Affect Disord. 2006;96:215-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 163. | Hantouche EG, Akiskal HS, Azorin JM, Châtenet-Duchêne L, Lancrenon S. Clinical and psychometric characterization of depression in mixed mania: a report from the French National Cohort of 1090 manic patients. J Affect Disord. 2006;96:225-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 49] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 164. | Haro JM, van Os J, Vieta E, Reed C, Lorenzo M, Goetz I; EMBLEM Advisory Board. Evidence for three distinct classes of 'typical', 'psychotic' and 'dual' mania: results from the EMBLEM study. Acta Psychiatr Scand. 2006;113:112-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 61] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 165. | Kessing LV. Gender differences in subtypes of late-onset depression and mania. Int Psychogeriatr. 2006;18:727-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 166. | Schwartzmann AM, Amaral JA, Issler C, Caetano SC, Tamada RS, Almeida KM, Soares MB, Dias Rda S, Rocca CC, Lafer B. A clinical study comparing manic and mixed episodes in patients with bipolar disorder. Braz J Psychiatry. 2007;29:130-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 167. | Azorin JM, Kaladjian A, Adida M, Hantouche E, Hameg A, Lancrenon S, Akiskal HS. Toward the delineation of mania subtypes in the French National EPIMAN-II Mille Cohort. Comparisons with prior cluster analytic investigations. Eur Arch Psychiatry Clin Neurosci. 2008;258:497-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 168. | Azorin JM, Kaladjian A, Adida M, Hantouche EG, Hameg A, Lancrenon S, Akiskal HS. Factors associated with rapid cycling in bipolar I manic patients: findings from a French national study. CNS Spectr. 2008;13:780-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 169. | Canuso CM, Bossie CA, Zhu Y, Youssef E, Dunner DL. Psychotic symptoms in patients with bipolar mania. J Affect Disord. 2008;111:164-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 170. | Lindenmayer JP, Bossie CA, Kujawa M, Zhu Y, Canuso CM. Dimensions of psychosis in patients with bipolar mania as measured by the positive and negative syndrome scale. Psychopathology. 2008;41:264-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 171. | Picardi A, Battisti F, de Girolamo G, Morosini P, Norcio B, Bracco R, Biondi M. Symptom structure of acute mania: a factor study of the 24-item Brief Psychiatric Rating Scale in a national sample of patients hospitalized for a manic episode. J Affect Disord. 2008;108:183-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 172. | van Rossum I, Haro JM, Tenback D, Boomsma M, Goetz I, Vieta E, van Os J; EMBLEM Advisory Board. Stability and treatment outcome of distinct classes of mania. Eur Psychiatry. 2008;23:360-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 173. | Volpe FM, Tavares A, Del Porto JA. Seasonality of three dimensions of mania: psychosis, aggression and suicidality. J Affect Disord. 2008;108:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 174. | Bräunig P, Sarkar R, Effenberger S, Schoofs N, Krüger S. Gender differences in psychotic bipolar mania. Gend Med. 2009;6:356-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 175. | Prakash O, Kumar CN, Shivakumar PT, Bharath S, Varghese M. Clinical presentation of mania compared with depression: data from a geriatric clinic in India. Int Psychogeriatr. 2009;21:764-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 176. | Yatham LN, Kauer-Sant'Anna M, Bond DJ, Lam RW, Torres I. Course and outcome after the first manic episode in patients with bipolar disorder: prospective 12-month data from the Systematic Treatment Optimization Program For Early Mania project. Can J Psychiatry. 2009;54:105-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 78] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 177. | Salvatore P, Baldessarini RJ, Tohen M, Khalsa HM, Sanchez-Toledo JP, Zarate CA Jr, Vieta E, Maggini C. McLean-Harvard International First-Episode Project: two-year stability of ICD-10 diagnoses in 500 first-episode psychotic disorder patients. J Clin Psychiatry. 2011;72:183-193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 76] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 178. | de Sousa RT, Busnello JV, Forlenza OV, Zanetti MV, Soeiro-de-Souza MG, van de Bilt MT, Moreno RA, Zarate CA Jr, Gattaz WF, Machado-Vieira R. Early improvement of psychotic symptoms with lithium monotherapy as a predictor of later response in mania. J Psychiatr Res. 2012;46:1564-1568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 179. | Ryu V, Song DH, Ha R, Ha K, Cho HS. Prodromes and coping types in bipolar patients with nonpsychotic or psychotic mania. Compr Psychiatry. 2012;53:732-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 180. | Kumari R, Chaudhury S, Kumar S. Dimensions of hallucinations and delusions in affective and nonaffective illnesses. ISRN Psychiatry. 2013;2013:616304. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 181. | Michalak EE, Torres IJ, Bond DJ, Lam RW, Yatham LN. The relationship between clinical outcomes and quality of life in first-episode mania: a longitudinal analysis. Bipolar Disord. 2013;15:188-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 182. | Nakamura K, Iga J, Matsumoto N, Ohmori T. Risk of bipolar disorder and psychotic features in patients initially hospitalised with severe depression. Acta Neuropsychiatr. 2015;27:113-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 183. | Bhuyan D, Chaudhury PK. Nature and types of delusion in schizophrenia and mania – is there a difference? IOSR J Dental Med Sci. 2016;15:01-06. |
| 184. | Prabhavathy KS, Kuruvilla PK, Ravindren R, Ganesh KK, Midhun S. Treatment response in nonpsychotic vs psychotic manias - A follow up study from India. Asian J Psychiatr. 2017;26:104-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 185. | Nehme E, Obeid S, Hallit S, Haddad C, Salame W, Tahan F. Impact of psychosis in bipolar disorder during manic episodes. Int J Neurosci. 2018;128:1128-1134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 186. | Akiskal HS, Walker P, Puzantian VR, King D, Rosenthal TL, Dranon M. Bipolar outcome in the course of depressive illness. Phenomenologic, familial, and pharmacologic predictors. J Affect Disord. 1983;5:115-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 238] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 187. | Endicott J, Nee J, Andreasen N, Clayton P, Keller M, Coryell W. Bipolar II. Combine or keep separate? J Affect Disord. 1985;8:17-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 147] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 188. | Serretti A, Lattuada E, Cusin C, Gasperini M, Smeraldi E. Clinical and demographic features of psychotic and nonpsychotic depression. Compr Psychiatry. 1999;40:358-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 189. | Colom F, Vieta E, Daban C, Pacchiarotti I, Sánchez-Moreno J. Clinical and therapeutic implications of predominant polarity in bipolar disorder. J Affect Disord. 2006;93:13-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 225] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 190. | Goes FS, Sadler B, Toolan J, Zamoiski RD, Mondimore FM, Mackinnon DF, Schweizer B; Bipolar Disorder Phenome Group, Raymond Depaulo J Jr, Potash JB. Psychotic features in bipolar and unipolar depression. Bipolar Disord. 2007;9:901-906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 191. | Brugue E, Colom F, Sanchez-Moreno J, Cruz N, Vieta E. Depression subtypes in bipolar I and II disorders. Psychopathology. 2008;41:111-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 192. | Forty L, Smith D, Jones L, Jones I, Caesar S, Cooper C, Fraser C, Gordon-Smith K, Hyde S, Farmer A, McGuffin P, Craddock N. Clinical differences between bipolar and unipolar depression. Br J Psychiatry. 2008;192:388-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 98] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 193. | Souery D, Zaninotto L, Calati R, Linotte S, Mendlewicz J, Sentissi O, Serretti A. Depression across mood disorders: review and analysis in a clinical sample. Compr Psychiatry. 2012;53:24-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 194. | Parker G, Graham R, Hadzi-Pavlovic D, McCraw S, Hong M, Friend P. Differentiation of bipolar I and II disorders by examining for differences in severity of manic/hypomanic symptoms and the presence or absence of psychosis during that phase. J Affect Disord. 2013;150:941-947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 195. | Brockington IF, Altman E, Hillier V, Meltzer HY, Nand S. The clinical picture of bipolar affective disorder in its depressed phase. A report from London and Chicago. Br J Psychiatry. 1982;141:558-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 196. | Aronson TA, Shukla S, Gujavarty K, Hoff A, DiBuono M, Khan E. Relapse in delusional depression: a retrospective study of the course of treatment. Compr Psychiatry. 1988;29:12-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 197. | Mitchell P, Parker G, Jamieson K, Wilhelm K, Hickie I, Brodaty H, Boyce P, Hadzi-Pavlovic D, Roy K. Are there any differences between bipolar and unipolar melancholia? J Affect Disord. 1992;25:97-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 44] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 198. | Benazzi F. Gender differences in bipolar II and unipolar depressed outpatients: a 557-case study. Ann Clin Psychiatry. 1999;11:55-59. [PubMed] [DOI] [Full Text] |
| 199. | Benazzi F. Psychotic versus nonpsychotic bipolar outpatient depression. Eur Psychiatry. 1999;14:458-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 200. | Benazzi F. Early- versus late-onset bipolar II disorder. J Psychiatry Neurosci. 2000;25:53-57. [PubMed] |
| 201. | Parker G, Roy K, Wilhelm K, Mitchell P, Hadzi-Pavlovic D. The nature of bipolar depression: implications for the definition of melancholia. J Affect Disord. 2000;59:217-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 71] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 202. | Benazzi F, Akiskal HS. Delineating bipolar II mixed states in the Ravenna-San Diego collaborative study: the relative prevalence and diagnostic significance of hypomanic features during major depressive episodes. J Affect Disord. 2001;67:115-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 119] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 203. | Perugi G, Akiskal HS, Micheli C, Toni C, Madaro D. Clinical characterization of depressive mixed state in bipolar-I patients: Pisa-San Diego collaboration. J Affect Disord. 2001;67:105-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 122] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 204. | Benazzi F. Bipolar II disorder and major depressive disorder: continuity or discontinuity? World J Biol Psychiatry. 2003;4:166-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 205. | Akiskal HS, Benazzi F. Atypical depression: a variant of bipolar II or a bridge between unipolar and bipolar II? J Affect Disord. 2005;84:209-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 114] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 206. | Benazzi F. Bipolar family history of the hypomanic symptoms and dimensions of mixed depression. Compr Psychiatry. 2005;46:399-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 207. | Sato T, Bottlender R, Kleindienst N, Möller HJ. Irritable psychomotor elation in depressed inpatients: a factor validation of mixed depression. J Affect Disord. 2005;84:187-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 50] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 208. | Benazzi F. A continuity between bipolar II depression and major depressive disorder? Prog Neuropsychopharmacol Biol Psychiatry. 2006;30:1043-1050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 209. | Kessing LV, Jensen HM, Christensen EM. Differences in the ICD-10 diagnostic subtype of depression in bipolar disorder compared to recurrent depressive disorder. Psychopathology. 2008;41:141-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 210. | Mitchell PB, Frankland A, Hadzi-Pavlovic D, Roberts G, Corry J, Wright A, Loo CK, Breakspear M. Comparison of depressive episodes in bipolar disorder and in major depressive disorder within bipolar disorder pedigrees. Br J Psychiatry. 2011;199:303-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 65] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 211. | Hu C, Xiang YT, Ungvari GS, Dickerson FB, Kilbourne AM, Si TM, Fang YR, Lu Z, Yang HC, Chiu HF, Lai KY, Hu J, Chen ZY, Huang Y, Sun J, Wang XP, Li HC, Zhang JB, Wang G. Undiagnosed bipolar disorder in patients treated for major depression in China. J Affect Disord. 2012;140:181-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 212. | Song JY, Yu HY, Kim SH, Hwang SS, Cho HS, Kim YS, Ha K, Ahn YM. Assessment of risk factors related to suicide attempts in patients with bipolar disorder. J Nerv Ment Dis. 2012;200:978-984. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 213. | Holma KM, Haukka J, Suominen K, Valtonen HM, Mantere O, Melartin TK, Sokero TP, Oquendo MA, Isometsä ET. Differences in incidence of suicide attempts between bipolar I and II disorders and major depressive disorder. Bipolar Disord. 2014;16:652-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 133] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 214. | Frankland A, Cerrillo E, Hadzi-Pavlovic D, Roberts G, Wright A, Loo CK, Breakspear M, Mitchell PB. Comparing the phenomenology of depressive episodes in bipolar I and II disorder and major depressive disorder within bipolar disorder pedigrees. J Clin Psychiatry. 2015;76:32-8; quiz 39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 215. | Leonpacher AK, Liebers D, Pirooznia M, Jancic D, MacKinnon DF, Mondimore FM, Schweizer B, Potash JB, Zandi PP; NIMH Genetics Initiative Bipolar Disorder Consortium, Goes FS. Distinguishing bipolar from unipolar depression: the importance of clinical symptoms and illness features. Psychol Med. 2015;45:2437-2446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 216. | Nisha A, Sathesh V, Punnoose VP, Varghese PJ. A comparative study on psycho-socio-demographic and clinical profile of patients with bipolar versus unipolar depression. Indian J Psychiatry. 2015;57:392-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 217. | Caldieraro MA, Sylvia LG, Dufour S, Walsh S, Janos J, Rabideau DJ, Kamali M, McInnis MG, Bobo WV, Friedman ES, Gao K, Tohen M, Reilly-Harrington NA, Ketter TA, Calabrese JR, McElroy SL, Thase ME, Shelton RC, Bowden CL, Kocsis JH, Deckersbach T, Nierenberg AA. Clinical correlates of acute bipolar depressive episode with psychosis. J Affect Disord. 2017;217:29-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 218. | Divecha AH, Tiwari DS, Patel VK, Barot PJ, Vijapura M a. T. A comparative study of clinical features of major depressive episode in major depressive disorder and bipolar disorder at tertiary care centre of Saurashtra region. Int J Med Sci Public Health. 2019;8:70-77. [DOI] [Full Text] |
| 219. | Gosek P, Heitzman J, Stefanowski B, Antosik-Wójcińska AZ, Parnowski T. Symptomatic differences and symptoms stability in unipolar and bipolar depression. Medical charts review in 99 inpatients. Psychiatr Pol. 2019;53:655-672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 220. | Dell'Osso L, Akiskal HS, Freer P, Barberi M, Placidi GF, Cassano GB. Psychotic and nonpsychotic bipolar mixed states: comparisons with manic and schizoaffective disorders. Eur Arch Psychiatry Clin Neurosci. 1993;243:75-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 25] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 221. | Amin-Esmaeili M, Motevalian A, Rahimi-Movaghar A, Hajebi A, Sharifi V, Mojtabai R, Gudarzi SS. Bipolar features in major depressive disorder: Results from the Iranian mental health survey (IranMHS). J Affect Disord. 2018;241:319-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 222. | Othmer E, Desouza CM, Penick EC, Nickel EJ, Hunter EE, Othmer SC, Powell BJ, Hall SB. Indicators of mania in depressed outpatients: a retrospective analysis of data from the Kansas 1500 study. J Clin Psychiatry. 2007;68:47-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 223. | Azorin JM, Baraille L, Gérard S, Bertsch J, Reed C, Lukasiewicz M. Mixed states with predominant manic or depressive symptoms: baseline characteristics and 24-month outcomes of the EMBLEM cohort. J Affect Disord. 2013;146:369-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 224. | Perugi G, Medda P, Swann AC, Reis J, Rizzato S, Mauri M. Phenomenological subtypes of severe bipolar mixed states: a factor analytic study. Compr Psychiatry. 2014;55:799-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 225. | Winokur G, Scharfetter C, Angst J. The diagnostic value in assessing mood congruence in delusions and hallucinations and their relationship to the affective state. Eur Arch Psychiatry Neurol Sci. 1985;234:299-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 226. | Stephens JH, McHugh PR. Characteristics and long-term follow-up of patients hospitalized for mood disorders in the Phipps Clinic, 1913-1940. J Nerv Ment Dis. 1991;179:64-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 227. | Morgan VA, Mitchell PB, Jablensky AV. The epidemiology of bipolar disorder: sociodemographic, disability and service utilization data from the Australian National Study of Low Prevalence (Psychotic) Disorders. Bipolar Disord. 2005;7:326-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 83] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 228. | Marneros A, Röttig S, Röttig D, Tscharntke A, Brieger P. Bipolar I disorder with mood-incongruent psychotic symptoms: a comparative longitudinal study. Eur Arch Psychiatry Clin Neurosci. 2009;259:131-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 229. | Rosen C, Grossman LS, Harrow M, Bonner-Jackson A, Faull R. Diagnostic and prognostic significance of Schneiderian first-rank symptoms: a 20-year longitudinal study of schizophrenia and bipolar disorder. Compr Psychiatry. 2011;52:126-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 230. | Goes FS, Hamshere ML, Seifuddin F, Pirooznia M, Belmonte-Mahon P, Breuer R, Schulze T, Nöthen M, Cichon S, Rietschel M, Holmans P, Zandi PP; Bipolar Genome Study (BiGS), Craddock N, Potash JB. Genome-wide association of mood-incongruent psychotic bipolar disorder. Transl Psychiatry. 2012;2:e180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 231. | Shinn AK, Pfaff D, Young S, Lewandowski KE, Cohen BM, Öngür D. Auditory hallucinations in a cross-diagnostic sample of psychotic disorder patients: a descriptive, cross-sectional study. Compr Psychiatry. 2012;53:718-726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 232. | Mancuso SG, Morgan VA, Mitchell PB, Berk M, Young A, Castle DJ. A comparison of schizophrenia, schizoaffective disorder, and bipolar disorder: Results from the Second Australian national psychosis survey. J Affect Disord. 2015;172:30-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 233. | Adhikari BR, Mishra S, Nepal S, Sapkota N. Psychotic symptoms in bipolar disorder: two years’ retrospective study. Health Renai. 2017;13:49-57. [DOI] [Full Text] |
| 234. | Toh WL, Castle DJ, Thomas N, Badcock JC, Rossell SL. Auditory verbal hallucinations (AVHs) and related psychotic phenomena in mood disorders: analysis of the 2010 Survey of High Impact Psychosis (SHIP) data. Psychiatry Res. 2016;243:238-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 235. | Toh WL, Castle DJ, Rossell SL. What is the future for Schneiderian first-rank symptoms, in the Diagnostic and Statistical Manual of Mental Disorders and otherwise? Aust N Z J Psychiatry. 2016;50:831-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 236. | Tanenberg-Karant M, Fennig S, Ram R, Krishna J, Jandorf L, Bromet EJ. Bizarre delusions and first-rank symptoms in a first-admission sample: a preliminary analysis of prevalence and correlates. Compr Psychiatry. 1995;36:428-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 39] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 237. | Fennig S, Bromet EJ, Karant MT, Ram R, Jandorf L. Mood-congruent versus mood-incongruent psychotic symptoms in first-admission patients with affective disorder. J Affect Disord. 1996;37:23-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 238. | Daneluzzo E, Arduini L, Rinaldi O, Di Domenico M, Petruzzi C, Kalyvoka A, Rossi A. PANSS factors and scores in schizophrenic and bipolar disorders during an index acute episode: a further analysis of the cognitive component. Schizophr Res. 2002;56:129-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 239. | Maj M, Pirozzi R, Bartoli L, Magliano L. Long-term outcome of lithium prophylaxis in bipolar disorder with mood-incongruent psychotic features: a prospective study. J Affect Disord. 2002;71:195-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 240. | Morgan VA, McGrath JJ, Jablensky A, Badcock JC, Waterreus A, Bush R, Carr V, Castle D, Cohen M, Galletly C, Harvey C, Hocking B, McGorry P, Neil AL, Saw S, Shah S, Stain HJ, Mackinnon A. Psychosis prevalence and physical, metabolic and cognitive co-morbidity: data from the second Australian national survey of psychosis. Psychol Med. 2014;44:2163-2176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 138] [Cited by in RCA: 151] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 241. | ParameshwaraNM, Mascascarenhas JJ, Mathai J. Schneider’s first rank symptoms in patients with bipolar affective disorders and schizophrenia - a clinical study. Int J Recent Sci Res. 2017;8:15642-15648. |
| 242. | Lundquist G. The prognosis for the first attack of the disease. Acta Psychiatr Scand. 1945;20 (Suppl 35):39-55. [DOI] [Full Text] |
| 243. | Conus P, Abdel-Baki A, Harrigan S, Lambert M, McGorry PD, Berk M. Pre-morbid and outcome correlates of first episode mania with psychosis: is a distinction between schizoaffective and bipolar I disorder valid in the early phase of psychotic disorders? J Affect Disord. 2010;126:88-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 244. | Carpenter WT Jr, Strauss JS. Cross-cultural evaluation of Schneider's first-rank symptoms of schizophrenia: a report from the International Pilot Study of Schizophrenia. Am J Psychiatry. 1974;131:682-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 89] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 245. | Wing J, Nixon J. Discriminating symptoms in schizophrenia. A report from the international pilot study of schizophrenia. Arch Gen Psychiatry. 1975;32:853-859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 63] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 246. | Abrams R, Taylor MA. Mania and schizo-affective disorder, main type: a comparison. Am J Psychiatry. 1976;133:445-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 247. | Abrams R, Taylor MA. Importance of schizophrenic symptoms in the diagnosis of mania. Am J Psychiatry. 1981;138:658-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 29] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 248. | McGlashan TH. Adolescent versus adult onset of mania. Am J Psychiatry. 1988;145:221-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 104] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 249. | Miklowitz DJ. Longitudinal outcome and medication noncompliance among manic patients with and without mood-incongruent psychotic features. J Nerv Ment Dis. 1992;180:703-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 250. | Tohen M, Tsuang MT, Goodwin DC. Prediction of outcome in mania by mood-congruent or mood-incongruent psychotic features. Am J Psychiatry. 1992;149:1580-1584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 71] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 251. | Verdoux H, Bourgeois M. Delusional mania: what is a mood-incongruent psychotic feature? J Nerv Ment Dis. 1993;181:517-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 252. | Strakowski SM, McElroy SL, Keck PE Jr, West SA. Racial influence on diagnosis in psychotic mania. J Affect Disord. 1996;39:157-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 60] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 253. | Perugi G, Akiskal HS, Rossi L, Paiano A, Quilici C, Madaro D, Musetti L, Cassano GB. Chronic mania. Family history, prior course, clinical picture and social consequences. Br J Psychiatry. 1998;173:514-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 254. | Carlson GA, Bromet EJ, Sievers S. Phenomenology and outcome of subjects with early- and adult-onset psychotic mania. Am J Psychiatry. 2000;157:213-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 128] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 255. | Strakowski SM, Williams JR, Sax KW, Fleck DE, DelBello MP, Bourne ML. Is impaired outcome following a first manic episode due to mood-incongruent psychosis? J Affect Disord. 2000;61:87-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 256. | González-Pinto A, van Os J, Pérez de Heredia JL, Mosquera F, Aldama A, Lalaguna B, Gutiérrez M, Micó JA. Age-dependence of Schneiderian psychotic symptoms in bipolar patients. Schizophr Res. 2003;61:157-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 257. | Conus P, Abdel-Baki A, Harrigan S, Lambert M, McGorry PD. Schneiderian first rank symptoms predict poor outcome within first episode manic psychosis. J Affect Disord. 2004;81:259-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 258. | Goldberg JF, Harrow M. Consistency of remission and outcome in bipolar and unipolar mood disorders: a 10-year prospective follow-up. J Affect Disord. 2004;81:123-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 112] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 259. | Azorin JM, Bellivier F, Kaladjian A, Adida M, Belzeaux R, Fakra E, Hantouche E, Lancrenon S, Golmard JL. Characteristics and profiles of bipolar I patients according to age-at-onset: findings from an admixture analysis. J Affect Disord. 2013;150:993-1000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 260. | Azorin JM, Belzeaux R, Kaladjian A, Adida M, Hantouche E, Lancrenon S, Fakra E. Risks associated with gender differences in bipolar I disorder. J Affect Disord. 2013;151:1033-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 261. | Channa A, Aleem S, Mohsin H. First rank symptoms in mania: an indistinct diagnostic strand. Acta Med Int. 2016;3:20-23. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 262. | Olfson M, Das AK, Gameroff MJ, Pilowsky D, Feder A, Gross R, Lantigua R, Shea S, Weissman MM. Bipolar depression in a low-income primary care clinic. Am J Psychiatry. 2005;162:2146-2151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 263. | Breslau N, Meltzer HY. Validity of subtyping psychotic depression: examination of phenomenology and demographic characteristics. Am J Psychiatry. 1988;145:35-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 264. | Benazzi F. Bipolar versus unipolar psychotic outpatient depression. J Affect Disord. 1999;55:63-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 265. | Strakowski SM, Keck PE Jr, McElroy SL, West SA, Sax KW, Hawkins JM, Kmetz GF, Upadhyaya VH, Tugrul KC, Bourne ML. Twelve-month outcome after a first hospitalization for affective psychosis. Arch Gen Psychiatry. 1998;55:49-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 201] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 266. | McGilchrist I, Cutting J. Somatic delusions in schizophrenia and the affective psychoses. Br J Psychiatry. 1995;167:350-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 267. | Maj M, Pirozzi R, Magliano L, Bartoli L. Agitated depression in bipolar I disorder: prevalence, phenomenology, and outcome. Am J Psychiatry. 2003;160:2134-2140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 103] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 268. | Shobe FO, Brion P. Long-term prognosis in manic-depressive illness. Arch Gen Psychiatry. 1971;24:334-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 269. | Coryell W, Endicott J, Keller M. Outcome of patients with chronic affective disorder: a five-year follow-up. Am J Psychiatry. 1990;147:1627-1633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 65] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 270. | Coryell W, Endicott J, Maser JD, Keller MB, Leon AC, Akiskal HS. Long-term stability of polarity distinctions in the affective disorders. Am J Psychiatry. 1995;152:385-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 216] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 271. | Gitlin MJ, Swendsen J, Heller TL, Hammen C. Relapse and impairment in bipolar disorder. Am J Psychiatry. 1995;152:1635-1640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 467] [Cited by in RCA: 434] [Article Influence: 14.0] [Reference Citation Analysis (6)] |
| 272. | Harrow M, Sands JR, Silverstein ML, Goldberg JF. Course and outcome for schizophrenia versus other psychotic patients: a longitudinal study. Schizophr Bull. 1997;23:287-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 78] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 273. | Turvey CL, Coryell WH, Solomon DA, Leon AC, Endicott J, Keller MB, Akiskal H. Long-term prognosis of bipolar I disorder. Acta Psychiatr Scand. 1999;99:110-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 54] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 274. | Harrow M, Grossman LS, Herbener ES, Davies EW. Ten-year outcome: patients with schizoaffective disorders, schizophrenia, affective disorders and mood-incongruent psychotic symptoms. Br J Psychiatry. 2000;177:421-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 116] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 275. | Goldberg JF, Harrow M, Whiteside JE. Risk for bipolar illness in patients initially hospitalized for unipolar depression. Am J Psychiatry. 2001;158:1265-1270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 202] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 276. | Carlson GA, Bromet EJ, Driessens C, Mojtabai R, Schwartz JE. Age at onset, childhood psychopathology, and 2-year outcome in psychotic bipolar disorder. Am J Psychiatry. 2002;159:307-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 87] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 277. | Dickerson FB, Boronow JJ, Stallings CR, Origoni AE, Cole S, Yolken RH. Association between cognitive functioning and employment status of persons with bipolar disorder. Psychiatr Serv. 2004;55:54-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 127] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 278. | Kassem L, Lopez V, Hedeker D, Steele J, Zandi P; Bipolar Disorder Consortium NIMH Genetics Initiative, McMahon FJ. Familiality of polarity at illness onset in bipolar affective disorder. Am J Psychiatry. 2006;163:1754-1759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 40] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 279. | Goes FS, Zandi PP, Miao K, McMahon FJ, Steele J, Willour VL, Mackinnon DF, Mondimore FM, Schweizer B, Nurnberger JI Jr, Rice JP, Scheftner W, Coryell W, Berrettini WH, Kelsoe JR, Byerley W, Murphy DL, Gershon ES; Bipolar Disorder Phenome Group; Depaulo JR Jr, McInnis MG, Potash JB. Mood-incongruent psychotic features in bipolar disorder: familial aggregation and suggestive linkage to 2p11-q14 and 13q21-33. Am J Psychiatry. 2007;164:236-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 60] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 280. | Forty L, Jones L, Jones I, Smith DJ, Caesar S, Fraser C, Gordon-Smith K, Hyde S, Craddock N. Polarity at illness onset in bipolar I disorder and clinical course of illness. Bipolar Disord. 2009;11:82-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 281. | Gutiérrez-Rojas L, Jurado D, Gurpegui M. Factors associated with work, social life and family life disability in bipolar disorder patients. Psychiatry Res. 2011;186:254-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 47] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 282. | Ballester J, Goldstein T, Goldstein B, Obreja M, Axelson D, Monk K, Hickey M, Iyengar S, Farchione T, Kupfer DJ, Brent D, Birmaher B. Is bipolar disorder specifically associated with aggression? Bipolar Disord. 2012;14:283-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 283. | Waghorn G, Saha S, Harvey C, Morgan VA, Waterreus A, Bush R, Castle D, Galletly C, Stain HJ, Neil AL, McGorry P, McGrath JJ. 'Earning and learning' in those with psychotic disorders: the second Australian national survey of psychosis. Aust N Z J Psychiatry. 2012;46:774-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 96] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 284. | Goghari VM, Harrow M, Grossman LS, Rosen C. A 20-year multi-follow-up of hallucinations in schizophrenia, other psychotic, and mood disorders. Psychol Med. 2013;43:1151-1160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 62] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 285. | Kotov R, Leong SH, Mojtabai R, Erlanger AC, Fochtmann LJ, Constantino E, Carlson GA, Bromet EJ. Boundaries of schizoaffective disorder: revisiting Kraepelin. JAMA Psychiatry. 2013;70:1276-1286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 286. | Baldessarini RJ, Tondo L, Visioli C. First-episode types in bipolar disorder: predictive associations with later illness. Acta Psychiatr Scand. 2014;129:383-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 73] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 287. | Altamura AC, Buoli M, Caldiroli A, Caron L, Cumerlato Melter C, Dobrea C, Cigliobianco M, Zanelli Quarantini F. Misdiagnosis, duration of untreated illness (DUI) and outcome in bipolar patients with psychotic symptoms: A naturalistic study. J Affect Disord. 2015;182:70-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 116] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 288. | Pallaskorpi S, Suominen K, Ketokivi M, Mantere O, Arvilommi P, Valtonen H, Leppämäki S, Isometsä E. Five-year outcome of bipolar I and II disorders: findings of the Jorvi Bipolar Study. Bipolar Disord. 2015;17:363-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 289. | Etain B, Lajnef M, Bellivier F, Henry C, M'bailara K, Kahn JP, Leboyer M, Fisher HL. Revisiting the association between childhood trauma and psychosis in bipolar disorder: A quasi-dimensional path-analysis. J Psychiatr Res. 2017;84:73-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 290. | Goghari VM, Harrow M. Twenty year multi-follow-up of different types of hallucinations in schizophrenia, schizoaffective disorder, bipolar disorder, and depression. Schizophr Res. 2016;176:371-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 291. | Heslin M, Lappin JM, Donoghue K, Lomas B, Reininghaus U, Onyejiaka A, Croudace T, Jones PB, Murray RM, Fearon P, Doody GA, Dazzan P, Craig TJ, Morgan C. Ten-year outcomes in first episode psychotic major depression patients compared with schizophrenia and bipolar patients. Schizophr Res. 2016;176:417-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 292. | Serra G, Koukopoulos A, De Chiara L, Koukopoulos AE, Sani G, Tondo L, Girardi P, Reginaldi D, Baldessarini RJ. Early clinical predictors and correlates of long-term morbidity in bipolar disorder. Eur Psychiatry. 2017;43:35-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 293. | Velthorst E, Fett AJ, Reichenberg A, Perlman G, van Os J, Bromet EJ, Kotov R. The 20-Year Longitudinal Trajectories of Social Functioning in Individuals With Psychotic Disorders. Am J Psychiatry. 2017;174:1075-1085. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 240] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 294. | Kapur V, Nadella RK, Sathur Raghuraman B, Saraf G, Mishra S, Srinivasmurthy N, Jain S, Del Zompo M, Viswanath B. Clinical factors associated with lithium treatment response in bipolar disorder patients from India. Asian J Psychiatr. 2019;39:165-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 295. | Kingston T, Scully PJ, Browne DJ, Baldwin PA, Kinsella A, O'Callaghan E, Russell V, Waddington JL. Functional outcome and service engagement in major depressive disorder with psychotic features: comparisons with schizophrenia, schizoaffective disorder and bipolar disorder in a 6-year follow-up of the Cavan-Monaghan First Episode Psychosis Study (CAMFEPS). CNS Neurosci Ther. 2018;24:633-640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 296. | Peralta V, Gil-Berrozpe GJ, Sánchez-Torres A, Cuesta MJ. The network and dimensionality structure of affective psychoses: an exploratory graph analysis approach. J Affect Disord. 2020;277:182-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 297. | Sautter FJ, McDermott BE, Garver DL. A family study of lithium-responsive psychosis. J Affect Disord. 1990;20:63-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 298. | Sax KW, Strakowski SM, Keck PE Jr, McElroy SL, West SA, Bourne ML, Larson ER. Comparison of patients with early-, typical-, and late-onset affective psychosis. Am J Psychiatry. 1997;154:1299-1301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 299. | Sanz M, Constable G, Lopez-Ibor I, Kemp R, David AS. A comparative study of insight scales and their relationship to psychopathological and clinical variables. Psychol Med. 1998;28:437-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 203] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 300. | Pini S, Dell'Osso L, Mastrocinque C, Marcacci G, Papasogli A, Vignoli S, Pallanti S, Cassano G. Axis I comorbidity in bipolar disorder with psychotic features. Br J Psychiatry. 1999;175:467-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 49] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 301. | Cassano GB, Pini S, Saettoni M, Dell'Osso L. Multiple anxiety disorder comorbidity in patients with mood spectrum disorders with psychotic features. Am J Psychiatry. 1999;156:474-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 28] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 302. | Vieta E, Calabrese JR, Hennen J, Colom F, Martínez-Arán A, Sánchez-Moreno J, Yatham LN, Tohen M, Baldessarini RJ. Comparison of rapid-cycling and non-rapid-cycling bipolar I manic patients during treatment with olanzapine: analysis of pooled data. J Clin Psychiatry. 2004;65:1420-1428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 47] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 303. | Schürhoff F, Bellivier F, Jouvent R, Mouren-Siméoni MC, Bouvard M, Allilaire JF, Leboyer M. Early and late onset bipolar disorders: two different forms of manic-depressive illness? J Affect Disord. 2000;58:215-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 193] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 304. | Oquendo MA, Waternaux C, Brodsky B, Parsons B, Haas GL, Malone KM, Mann JJ. Suicidal behavior in bipolar mood disorder: clinical characteristics of attempters and nonattempters. J Affect Disord. 2000;59:107-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 191] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 305. | Macmillan I, Howells L, Kale K, Hackmann C, Taylor G, Hill K, Bradford S, Fowler D. Social and symptomatic outcomes of first-episode bipolar psychoses in an early intervention service. Early Interv Psychiatry. 2007;1:79-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 306. | Gao K, Tolliver BK, Kemp DE, Ganocy SJ, Bilali S, Brady KL, Findling RL, Calabrese JR. Correlates of historical suicide attempt in rapid-cycling bipolar disorder: a cross-sectional assessment. J Clin Psychiatry. 2009;70:1032-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 307. | Salvatore P, Baldessarini RJ, Tohen M, Khalsa HM, Sanchez-Toledo JP, Zarate CA Jr, Vieta E, Maggini C. McLean-Harvard International First-Episode Project: two-year stability of DSM-IV diagnoses in 500 first-episode psychotic disorder patients. J Clin Psychiatry. 2009;70:458-466. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 130] [Cited by in RCA: 106] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 308. | Cassidy F. Insight in bipolar disorder: relationship to episode subtypes and symptom dimensions. Neuropsychiatr Dis Treat. 2010;6:627-631. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 309. | Güçlü O, Karaca O, Yıldırım B, Ozköse MM, Erkıran M. The relationship between insight and clinical features in bipolar disorder. Turk Psikiyatri Derg. 2011;22:230-238. [PubMed] |
| 310. | Pacchiarotti I, Nivoli AM, Mazzarini L, Kotzalidis GD, Sani G, Koukopoulos A, Scott J, Strejilevich S, Sánchez-Moreno J, Murru A, Valentí M, Girardi P, Vieta E, Colom F. The symptom structure of bipolar acute episodes: in search for the mixing link. J Affect Disord. 2013;149:56-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 311. | Jiménez-López E, Sánchez-Morla EM, Aparicio AI, López-Villarreal A, Martínez-Vizcaíno V, Rodriguez-Jimenez R, Vieta E, Santos JL. Psychosocial functioning in patients with psychotic and non-psychotic bipolar I disorder. A comparative study with individuals with schizophrenia. J Affect Disord. 2018;229:177-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 312. | Lewandowski KE, Cohen TR, Ongur D. Cognitive and clinical predictors of community functioning across the psychoses. Psych J. 2020;9:163-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 313. | Salagre E, Grande I, Vieta E, Mezquida G, Cuesta MJ, Moreno C, Bioque M, Lobo A, González-Pinto A, Moreno DM, Corripio I, Verdolini N, Castro-Fornieles J, Mané A, Pinzon-Espinosa J, Bonnin CDM, Bernardo M; Group P. Predictors of Bipolar Disorder Versus Schizophrenia Diagnosis in a Multicenter First Psychotic Episode Cohort: Baseline Characterization and a 12-Month Follow-Up Analysis. J Clin Psychiatry. 2020;81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 314. | Beigel A, Murphy DL. Unipolar and bipolar affective illness. Differences in clinical characteristics accompanying depression. Arch Gen Psychiatry. 1971;24:215-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 103] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 315. | Black DW, Winokur G, Nasrallah A, Brewin A. Psychotic symptoms and age of onset in affective disorders. Psychopathology. 1992;25:19-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 316. | Lattuada E, Serretti A, Cusin C, Gasperini M, Smeraldi E. Symptomatologic analysis of psychotic and non-psychotic depression. J Affect Disord. 1999;54:183-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 45] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 317. | Dell'Osso L, Pini S, Tundo A, Sarno N, Musetti L, Cassano GB. Clinical characteristics of mania, mixed mania, and bipolar depression with psychotic features. Compr Psychiatry. 2000;41:242-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 318. | Bottlender R, Jäger M, Strauss A, Möller HJ. Suicidality in bipolar compared to unipolar depressed inpatients. Eur Arch Psychiatry Clin Neurosci. 2000;250:257-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 49] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 319. | Mitchell PB, Wilhelm K, Parker G, Austin MP, Rutgers P, Malhi GS. The clinical features of bipolar depression: a comparison with matched major depressive disorder patients. J Clin Psychiatry. 2001;62:212-6; quiz 217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 188] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 320. | Akiskal HS, Benazzi F. Psychopathologic correlates of suicidal ideation in major depressive outpatients: is it all due to unrecognized (bipolar) depressive mixed states? Psychopathology. 2005;38:273-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 61] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 321. | Kessing LV. Diagnostic subtypes of bipolar disorder in older versus younger adults. Bipolar Disord. 2006;8:56-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 38] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 322. | Swann AC, Steinberg JL, Lijffijt M, Moeller GF. Continuum of depressive and manic mixed states in patients with bipolar disorder: quantitative measurement and clinical features. World Psychiatry. 2009;8:166-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 61] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 323. | Umamaheswari V, Avasthi A, Grover S. Risk factors for suicidal ideations in patients with bipolar disorder. Bipolar Disord. 2014;16:642-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 324. | Silva RAD, Mograbi DC, Camelo EVM, Santana CMT, Landeira-Fernandez J, Cheniaux E. Clinical correlates of loss of insight in bipolar depression. Trends Psychiatry Psychother. 2017;39:264-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 325. | He H, Chang Q, Ma Y. The Association of Insight and Change in Insight with Clinical Symptoms in Depressed Inpatients. Shanghai Arch Psychiatry. 2018;30:110-118. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 326. | Caldieraro MA, Dufour S, Sylvia LG, Gao K, Ketter TA, Bobo WV, Walsh S, Janos J, Tohen M, Reilly-Harrington NA, McElroy SL, Shelton RC, Bowden CL, Deckersbach T, Nierenberg AA. Treatment outcomes of acute bipolar depressive episode with psychosis. Depress Anxiety. 2018;35:402-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 327. | Pope HG Jr, Lipinski JF, Cohen BM, Axelrod DT. "Schizoaffective disorder": an invalid diagnosis? Am J Psychiatry. 1980;137:921-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 82] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 328. | Coryell W, Keller M, Lavori P, Endicott J. Affective syndromes, psychotic features, and prognosis. II. Mania. Arch Gen Psychiatry. 1990;47:658-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 33] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 329. | Harrow M, Goldberg JF, Grossman LS, Meltzer HY. Outcome in manic disorders. A naturalistic follow-up study. Arch Gen Psychiatry. 1990;47:665-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 197] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 330. | Harrow M, MacDonald AW 3rd, Sands JR, Silverstein ML. Vulnerability to delusions over time in schizophrenia and affective disorders. Schizophr Bull. 1995;21:95-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 331. | Conus P, Cotton S, Abdel-Baki A, Lambert M, Berk M, McGorry PD. Symptomatic and functional outcome 12 months after a first episode of psychotic mania: barriers to recovery in a catchment area sample. Bipolar Disord. 2006;8:221-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 72] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 332. | Baldessarini RJ, Salvatore P, Khalsa HM, Tohen M. Dissimilar morbidity following initial mania versus mixed-states in type-I bipolar disorder. J Affect Disord. 2010;126:299-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 333. | Harrow M, Jobe TH. How frequent is chronic multiyear delusional activity and recovery in schizophrenia: a 20-year multi-follow-up. Schizophr Bull. 2010;36:192-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 50] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 334. | Chang WC, Lau ES, Chiu SS, Hui CL, Chan SK, Lee EH, Chen EY. Three-year clinical and functional outcome comparison between first-episode mania with psychotic features and first-episode schizophrenia. J Affect Disord. 2016;200:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 335. | Taylor MA, Abrams R. Gender differences in bipolar affective disorder. J Affect Disord. 1981;3:261-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 336. | Pi EH, Surawicz FG. Schizo-affective disorder (Schneiderian positive), manic type: a comparison with mania. J Clin Psychiatry. 1982;43:235-236. [PubMed] |
| 337. | Brockington IF, Hillier VF, Francis AF, Helzer JE, Wainwright S. Definitions of mania: concordance and prediction of outcome. Am J Psychiatry. 1983;140:435-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 338. | Zemlan FP, Hirschowitz J, Garver DL. Mood-incongruent versus mood-congruent psychosis: differential antipsychotic response to lithium therapy. Psychiatry Res. 1984;11:317-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 339. | Black DW, Winokur G, Nasrallah A. Treatment of mania: a naturalistic study of electroconvulsive therapy versus lithium in 438 patients. J Clin Psychiatry. 1987;48:132-139. [PubMed] |
| 340. | Black DW, Winokur G, Nasrallah A. Effect of psychosis on suicide risk in 1,593 patients with unipolar and bipolar affective disorders. Am J Psychiatry. 1988;145:849-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 341. | Garver DL, Kelly K, Fried KA, Magnusson M, Hirschowitz J. Drug response patterns as a basis of nosology for the mood-incongruent psychoses (the schizophrenias). Psychol Med. 1988;18:873-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 27] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 342. | Tohen M, Waternaux CM, Tsuang MT, Hunt AT. Four-year follow-up of twenty-four first-episode manic patients. J Affect Disord. 1990;19:79-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 79] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 343. | Miller F, Tanenbaum JH, Griffin A, Ritvo E. Prediction of treatment response in bipolar, manic disorder. J Affect Disord. 1991;21:75-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 344. | Amador XF, Flaum M, Andreasen NC, Strauss DH, Yale SA, Clark SC, Gorman JM. Awareness of illness in schizophrenia and schizoaffective and mood disorders. Arch Gen Psychiatry. 1994;51:826-836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 654] [Cited by in RCA: 634] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 345. | Keck PE Jr, McElroy SL, Strakowski SM, West SA, Sax KW, Hawkins JM, Bourne ML, Haggard P. 12-month outcome of patients with bipolar disorder following hospitalization for a manic or mixed episode. Am J Psychiatry. 1998;155:646-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 322] [Cited by in RCA: 302] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 346. | Sato T, Bottlender R, Kleindienst N, Möller HJ. Syndromes and phenomenological subtypes underlying acute mania: a factor analytic study of 576 manic patients. Am J Psychiatry. 2002;159:968-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 89] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 347. | Swann AC, Bowden CL, Calabrese JR, Dilsaver SC, Morris DD. Pattern of response to divalproex, lithium, or placebo in four naturalistic subtypes of mania. Neuropsychopharmacology. 2002;26:530-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 98] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 348. | Volpe FM, Tavares A, Correa H. Naturalistic evaluation of inpatient treatment of mania in a private Brazilian psychiatric hospital. Braz J Psychiatry. 2003;25:72-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 349. | Swann AC, Daniel DG, Kochan LD, Wozniak PJ, Calabrese JR. Psychosis in mania: specificity of its role in severity and treatment response. J Clin Psychiatry. 2004;65:825-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 350. | Azorin JM, Akiskal H, Akiskal K, Hantouche E, Châtenet-Duchêne L, Gury C, Lancrenon S. Is psychosis in DSM-IV mania due to severity? Acta Psychiatr Scand. 2007;115:29-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 351. | Van Riel WG, Vieta E, Martinez-Aran A, Haro JM, Bertsch J, Reed C, Van Os J. Chronic mania revisited: factors associated with treatment non-response during prospective follow-up of a large European cohort (EMBLEM). World J Biol Psychiatry. 2008;9:313-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 352. | Azorin JM, Aubrun E, Bertsch J, Reed C, Gerard S, Lukasiewicz M. Mixed states vs. pure mania in the French sample of the EMBLEM study: results at baseline and 24 months--European mania in bipolar longitudinal evaluation of medication. BMC Psychiatry. 2009;9:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 353. | Azorin JM, Kaladjian A, Adida M, Hantouche E, Hameg A, Lancrenon S, Akiskal HS. Risk factors associated with lifetime suicide attempts in bipolar I patients: findings from a French National Cohort. Compr Psychiatry. 2009;50:115-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 68] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 354. | González-Ortega I, Mosquera F, Echeburúa E, González-Pinto A. Insight, psychosis and aggressive behaviour in mania. Eu J Psychiatry. 2010;24:70-77. |
| 355. | Schöttle D, Schimmelmann BG, Conus P, Cotton SM, Michel C, McGorry PD, Karow A, Naber D, Lambert M. Differentiating schizoaffective and bipolar I disorder in first-episode psychotic mania. Schizophr Res. 2012;140:31-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 356. | Delgado VB, Chaves ML. Mood congruence phenomenon in acutely symptomatic mania bipolar I disorder patients with and without psychotic symptoms. Cogn Neuropsychiatry. 2013;18:477-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 357. | Cotton SM, Lambert M, Berk M, Schimmelmann BG, Butselaar FJ, McGorry PD, Conus P. Gender differences in first episode psychotic mania. BMC Psychiatry. 2013;13:82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 358. | Smith LT, Shelton CL, Berk M, Hasty MK, Cotton SM, Henry L, Daglas R, Gentle E, McGorry PD, Macneil CA, Conus P. The impact of insight in a first-episode mania with psychosis population on outcome at 18 months. J Affect Disord. 2014;167:74-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 359. | Oldis M, Murray G, Macneil CA, Hasty MK, Daglas R, Berk M, Conus P, Cotton SM. Trajectory and predictors of quality of life in first episode psychotic mania. J Affect Disord. 2016;195:148-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 360. | Soni A, Singh P, Kumar S, Shah R, Batra L, Verma M. Role of age at onset in the clinical presentation of bipolar disorder in Indian population. Ind Psychiatry J. 2021;30:41-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 361. | Swann AC, Moeller FG, Steinberg JL, Schneider L, Barratt ES, Dougherty DM. Manic symptoms and impulsivity during bipolar depressive episodes. Bipolar Disord. 2007;9:206-212. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 122] [Cited by in RCA: 106] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 362. | Goldberg JF, Perlis RH, Bowden CL, Thase ME, Miklowitz DJ, Marangell LB, Calabrese JR, Nierenberg AA, Sachs GS. Manic symptoms during depressive episodes in 1,380 patients with bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2009;166:173-181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 237] [Cited by in RCA: 215] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 363. | Perugi G, Medda P, Reis J, Rizzato S, Giorgi Mariani M, Mauri M. Clinical subtypes of severe bipolar mixed states. J Affect Disord. 2013;151:1076-1082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 364. | Arciniegas DB. Psychosis. Continuum (Minneap Minn). 2015;21:715-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 88] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 365. | Seiler N, Nguyen T, Yung A, O'Donoghue B. Terminology and assessment tools of psychosis: A systematic narrative review. Psychiatry Clin Neurosci. 2020;74:226-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 366. | Rudnick A. On the notion of psychosis: the DSM-IV in perspective. Psychopathology. 1997;30:298-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 367. | Sanchez-Moreno J, Martinez-Aran A, Tabarés-Seisdedos R, Torrent C, Vieta E, Ayuso-Mateos JL. Functioning and disability in bipolar disorder: an extensive review. Psychother Psychosom. 2009;78:285-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 283] [Cited by in RCA: 308] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 368. | Dieperink ME, Sands JR. Bipolar mania with psychotic features: diagnosis and treatment. Psychiatr Ann. 1996;26:633-637. [RCA] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 369. | Geoffroy PA, Etain B, Jamain S, Bellivier F, Leboyer M. [Early onset bipolar disorder: validation from admixture analyses and biomarkers]. Can J Psychiatry. 2013;58:240-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 370. | Leboyer M, Henry C, Paillere-Martinot ML, Bellivier F. Age at onset in bipolar affective disorders: a review. Bipolar Disord. 2005;7:111-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 204] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 371. | Joslyn C, Hawes DJ, Hunt C, Mitchell PB. Is age of onset associated with severity, prognosis, and clinical features in bipolar disorder? Bipolar Disord. 2016;18:389-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 114] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 372. | Bonnín CDM, Reinares M, Martínez-Arán A, Jiménez E, Sánchez-Moreno J, Solé B, Montejo L, Vieta E. Improving Functioning, Quality of Life, and Well-being in Patients With Bipolar Disorder. Int J Neuropsychopharmacol. 2019;22:467-477. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 59] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 373. | MacQueen GM, Young LT, Joffe RT. A review of psychosocial outcome in patients with bipolar disorder. Acta Psychiatr Scand. 2001;103:163-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 237] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 374. | Abreu LN, Lafer B, Baca-Garcia E, Oquendo MA. Suicidal ideation and suicide attempts in bipolar disorder type I: an update for the clinician. Braz J Psychiatry. 2009;31:271-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 77] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 375. | Dong M, Lu L, Zhang L, Zhang Q, Ungvari GS, Ng CH, Yuan Z, Xiang Y, Wang G, Xiang YT. Prevalence of suicide attempts in bipolar disorder: a systematic review and meta-analysis of observational studies. Epidemiol Psychiatr Sci. 2019;29:e63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 98] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 376. | Baldessarini RJ, Undurraga J, Vázquez GH, Tondo L, Salvatore P, Ha K, Khalsa HM, Lepri B, Ha TH, Chang JS, Tohen M, Vieta E. Predominant recurrence polarity among 928 adult international bipolar I disorder patients. Acta Psychiatr Scand. 2012;125:293-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 120] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 377. | Tighe SK, Mahon PB, Potash JB. Predictors of lithium response in bipolar disorder. Ther Adv Chronic Dis. 2011;2:209-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 378. | Kendler KS. Mood-incongruent psychotic affective illness. A historical and empirical review. Arch Gen Psychiatry. 1991;48:362-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 40] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 379. | Ivleva E, Thaker G, Tamminga CA. Comparing genes and phenomenology in the major psychoses: schizophrenia and bipolar 1 disorder. Schizophr Bull. 2008;34:734-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 42] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 380. | Buoli M, Caldiroli A, Cumerlato Melter C, Serati M, de Nijs J, Altamura AC. Biological aspects and candidate biomarkers for psychotic bipolar disorder: A systematic review. Psychiatry Clin Neurosci. 2016;70:227-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 381. | Harrison PJ, Geddes JR, Tunbridge EM. The Emerging Neurobiology of Bipolar Disorder. Trends Neurosci. 2018;41:18-30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 146] [Cited by in RCA: 161] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 382. | Garety PA, Bebbington P, Fowler D, Freeman D, Kuipers E. Implications for neurobiological research of cognitive models of psychosis: a theoretical paper. Psychol Med. 2007;37:1377-1391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 237] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 383. | Goes FS, Sanders LL, Potash JB. The genetics of psychotic bipolar disorder. Curr Psychiatry Rep. 2008;10:178-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: International Society for Affective Disorders, No. P0001064; Indian Psychiatric Society, No. 03051.
Specialty type: Psychiatry
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Li ZZ, China; Sun XL, China; Wang DJ, China; S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR