©The Author(s) 2025.
World J Psychiatry. Dec 19, 2025; 15(12): 112655
Published online Dec 19, 2025. doi: 10.5498/wjp.v15.i12.112655
Published online Dec 19, 2025. doi: 10.5498/wjp.v15.i12.112655
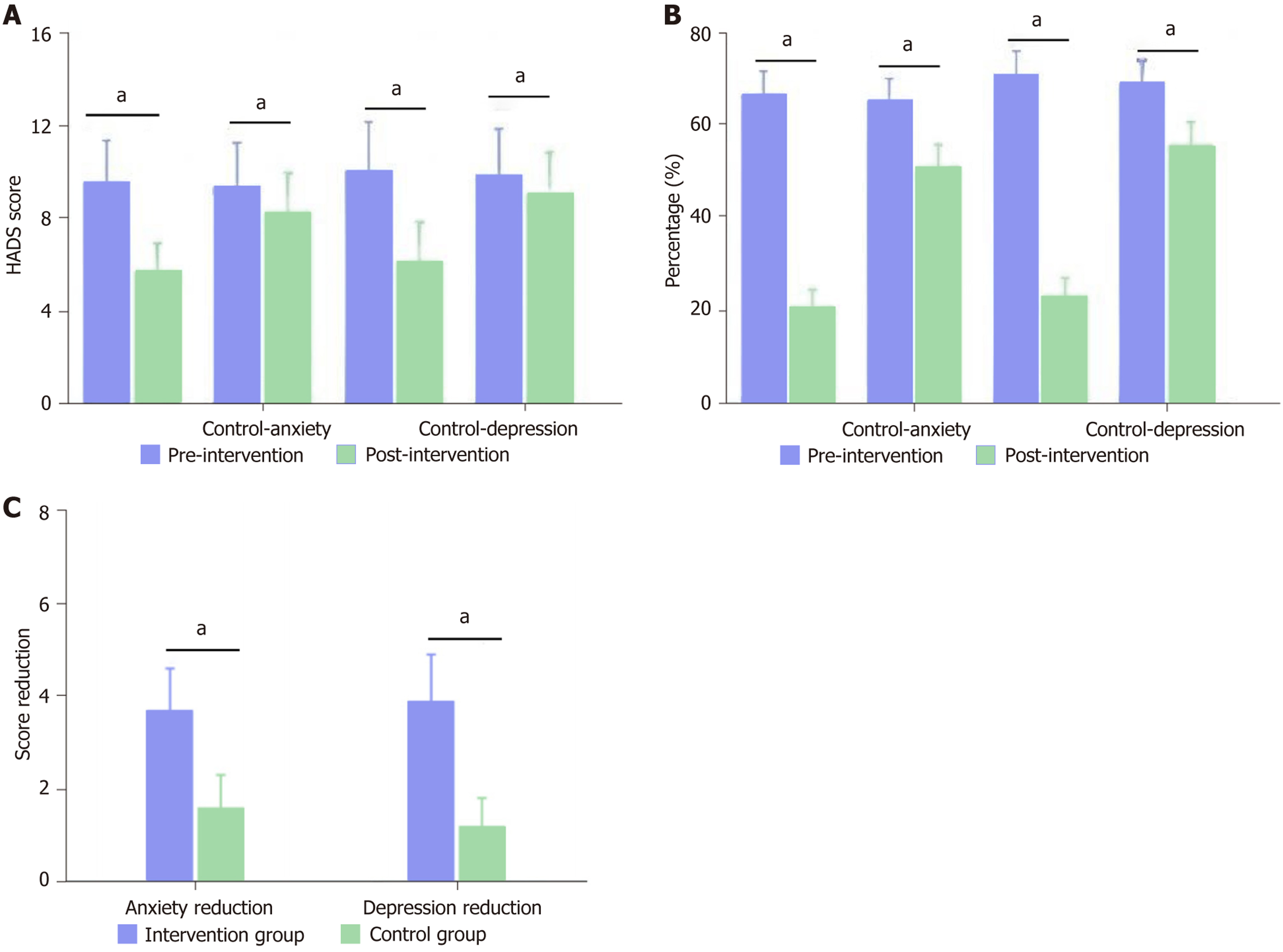
Figure 1 Effects of mindfulness-based stress reduction intervention on anxiety and depression in post-surgical cervical cancer patients.
The figure illustrates the significant improvements in psychological outcomes following mindfulness-based stress reduction therapy. A: Shows decreased Hospital Anxiety and Depression Scale (HADS) scores after intervention in both groups, with more substantial reductions in the intervention group; B and C: Demonstrates the notable decrease in the percentage of patients with clinically significant symptoms (HADS ≥ 8), while panel C quantifies the superior score reduction achieved in the intervention group compared to standard care. aP < 0.05. HADS: Hospital Anxiety and Depression Scale.
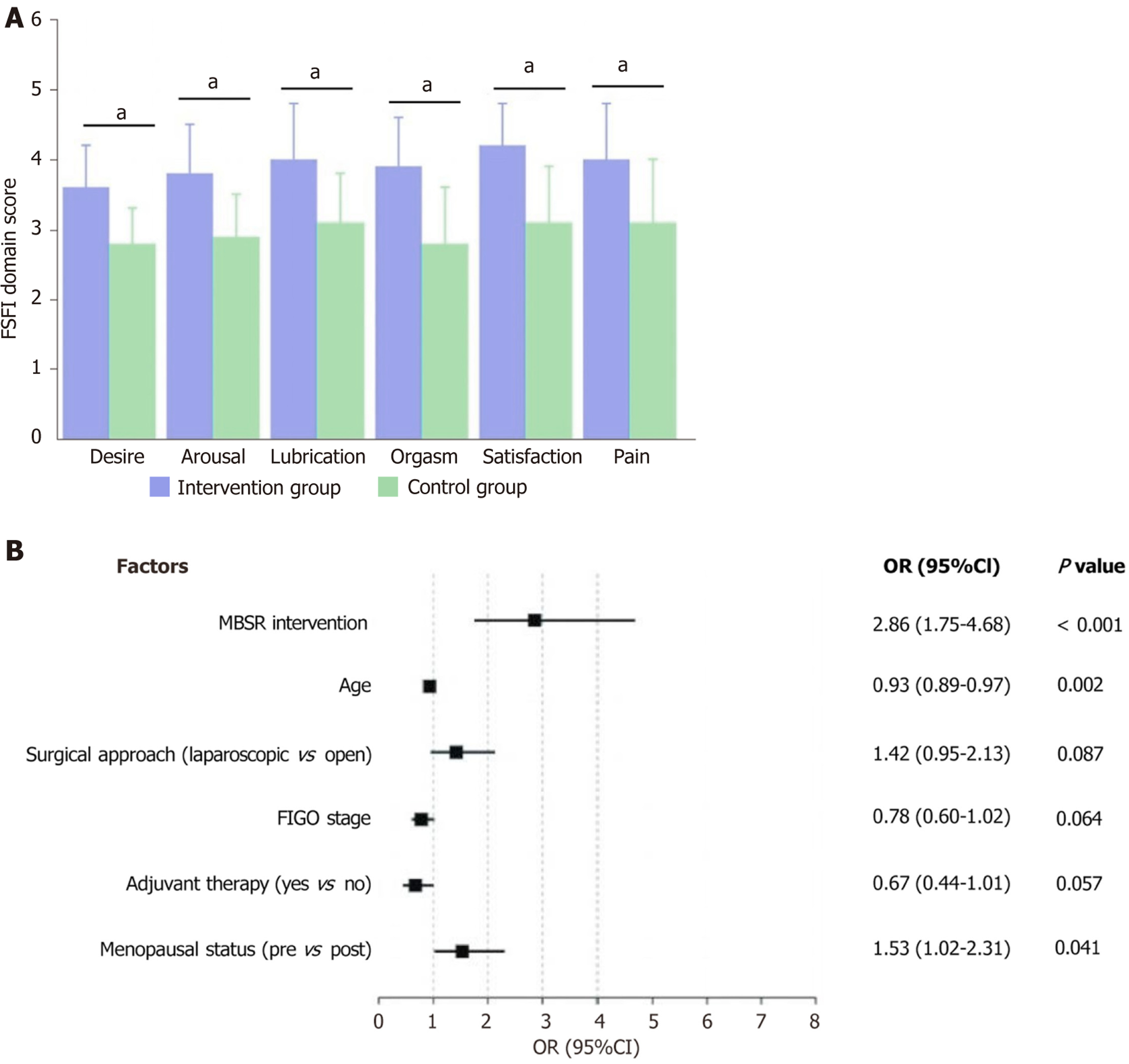
Figure 2 Mindfulness-based stress reduction intervention effects on sexual function after cervical cancer surgery.
A: Significantly higher Female Sexual Function Index domain scores in the intervention group compared to the control group across all six sexual function domains (desire, arousal, lubrication, orgasm, satisfaction, and pain), with statistical significance indicated by asterisks; B: Forest plot of the multivariate analysis, showing mindfulness-based stress reduction intervention (odds ratio = 2.86) and premenopausal status as significant positive factors for improved sexual function, while age appears as a negative factor. aP < 0.05. FSFI: Female Sexual Function Index; MBSR: Mindfulness-based stress reduction; OR: Odds ratio; 95%CI: 95% confidence interval.
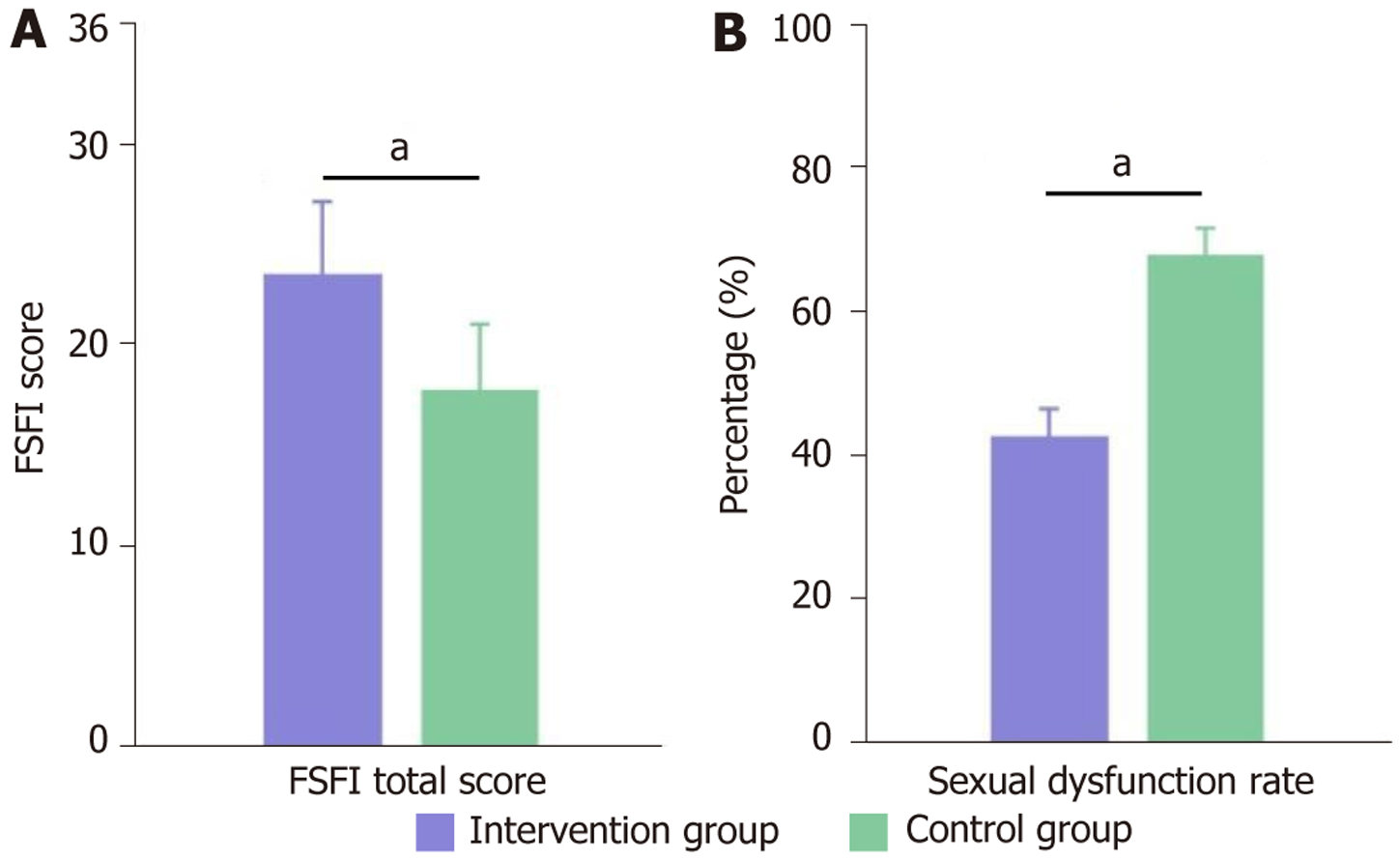
Figure 3 Sexual function outcomes after mindfulness-based stress reduction intervention for post-cervical cancer surgery patients.
The figure illustrates significant improvements in sexual function following mindfulness-based stress reduction (MBSR) intervention. A: The intervention group achieved significantly higher Female Sexual Function Index total scores (23.5 ± 3.6) than the control group (17.8 ± 3.2); B: Sexual dysfunction rates were substantially lower in the intervention group (42.8%) compared to the control group (67.9%). Both differences were statistically significant (P < 0.001), highlighting MBSR's effectiveness in improving sexual function and reducing dysfunction after cervical cancer surgery. aP < 0.05. FSFI: Female Sexual Function Index.
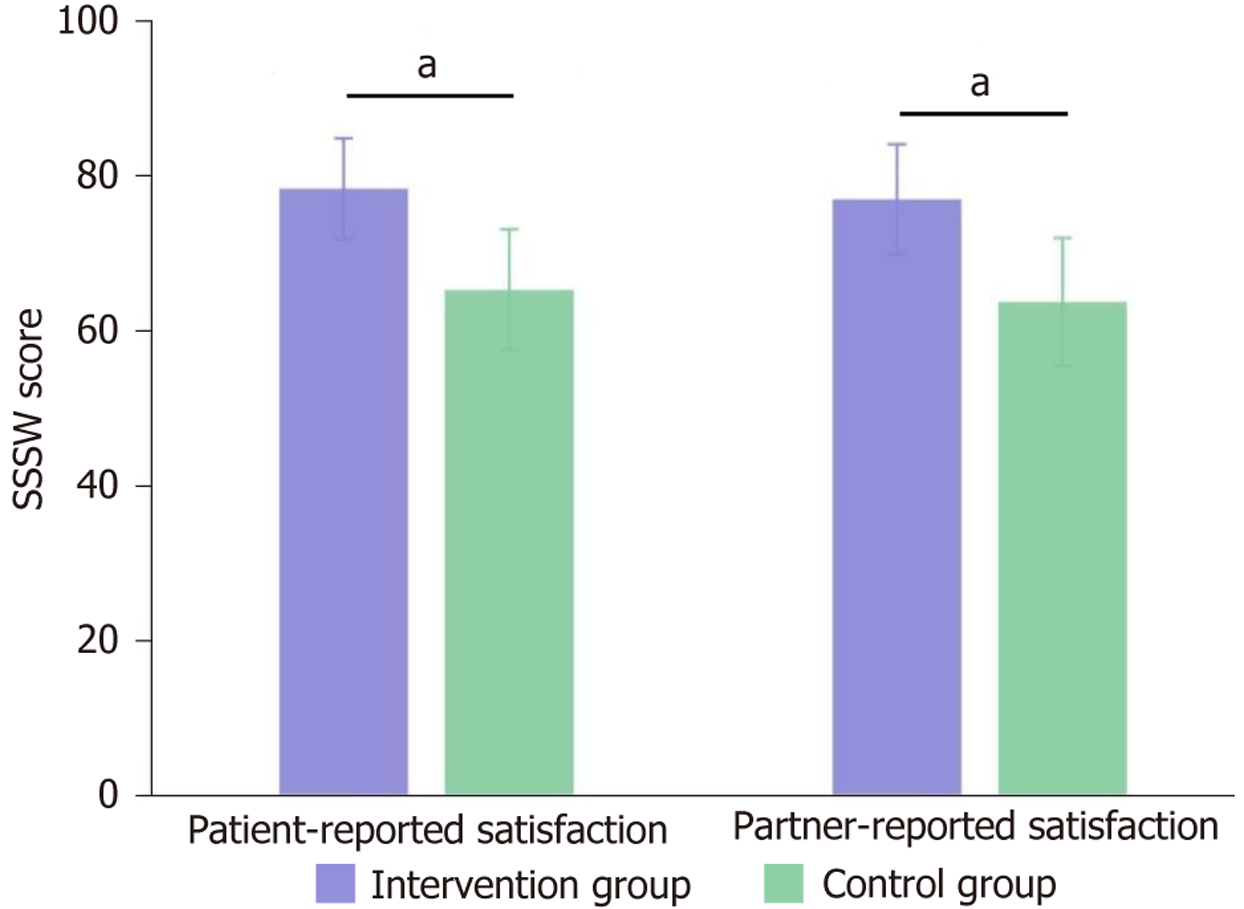
Figure 4 Sexual relationship satisfaction after mindfulness-based stress reduction intervention in post-cervical cancer surgery patients.
The chart illustrates significantly higher sexual relationship satisfaction scores in both patients and their partners following mindfulness-based stress reduction intervention. The intervention group demonstrated markedly elevated Sexual Satisfaction Scale for Women scores (78.3 ± 6.5 for patients, 76.9 ± 7.1 for partners) compared to the control group (65.2 ± 7.8 for patients, 63.6 ± 8.3 for partners), with both differences being statistically significant (P < 0.001). aP < 0.05. SSSW: Sexual Satisfaction Scale for Women.
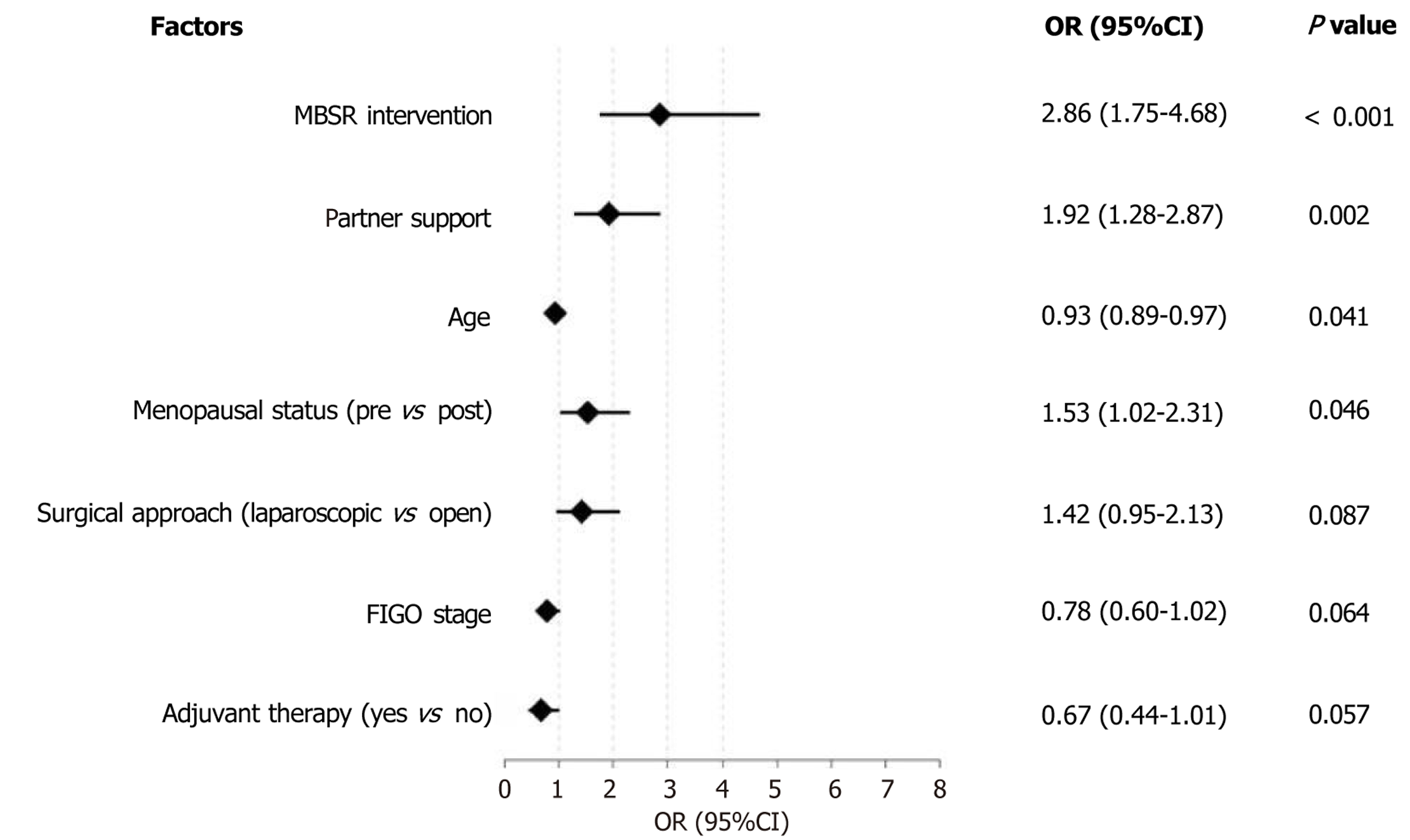
Figure 5 Independent predictors of sexual psychological adaptation after cervical cancer surgery.
The forest plot reveals mindfulness-based stress reduction intervention as the strongest independent predictor of improved sexual psychological adaptation [odds ratio (OR) = 2.86, 95% confidence interval (95%CI): 1.75-4.68, P < 0.001], followed by partner support (OR = 1.92, 95%CI: 1.28-2.87, P = 0.002). While advancing age slightly reduces adaptation potential (OR = 0.93), menopausal status shows a modest positive association (OR = 1.53); other clinical factors including surgical approach, FIGO stage, and adjuvant therapy demonstrate non-significant effects, highlighting the primacy of psychological interventions and relational support over strictly medical factors in facilitating sexual recovery. MBSR: Mindfulness-based stress reduction; OR: Odds ratio; 95%CI: 95% confidence interval.
- Citation: Sun QQ, Ke FF, Zhou HY, Zhou SJ, Lu J, Gao M. Mindfulness-based stress reduction for sexual psychological recovery after radical cervical cancer surgery: A retrospective study. World J Psychiatry 2025; 15(12): 112655
- URL: https://www.wjgnet.com/2220-3206/full/v15/i12/112655.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i12.112655