©The Author(s) 2025.
World J Psychiatry. Nov 19, 2025; 15(11): 109581
Published online Nov 19, 2025. doi: 10.5498/wjp.v15.i11.109581
Published online Nov 19, 2025. doi: 10.5498/wjp.v15.i11.109581
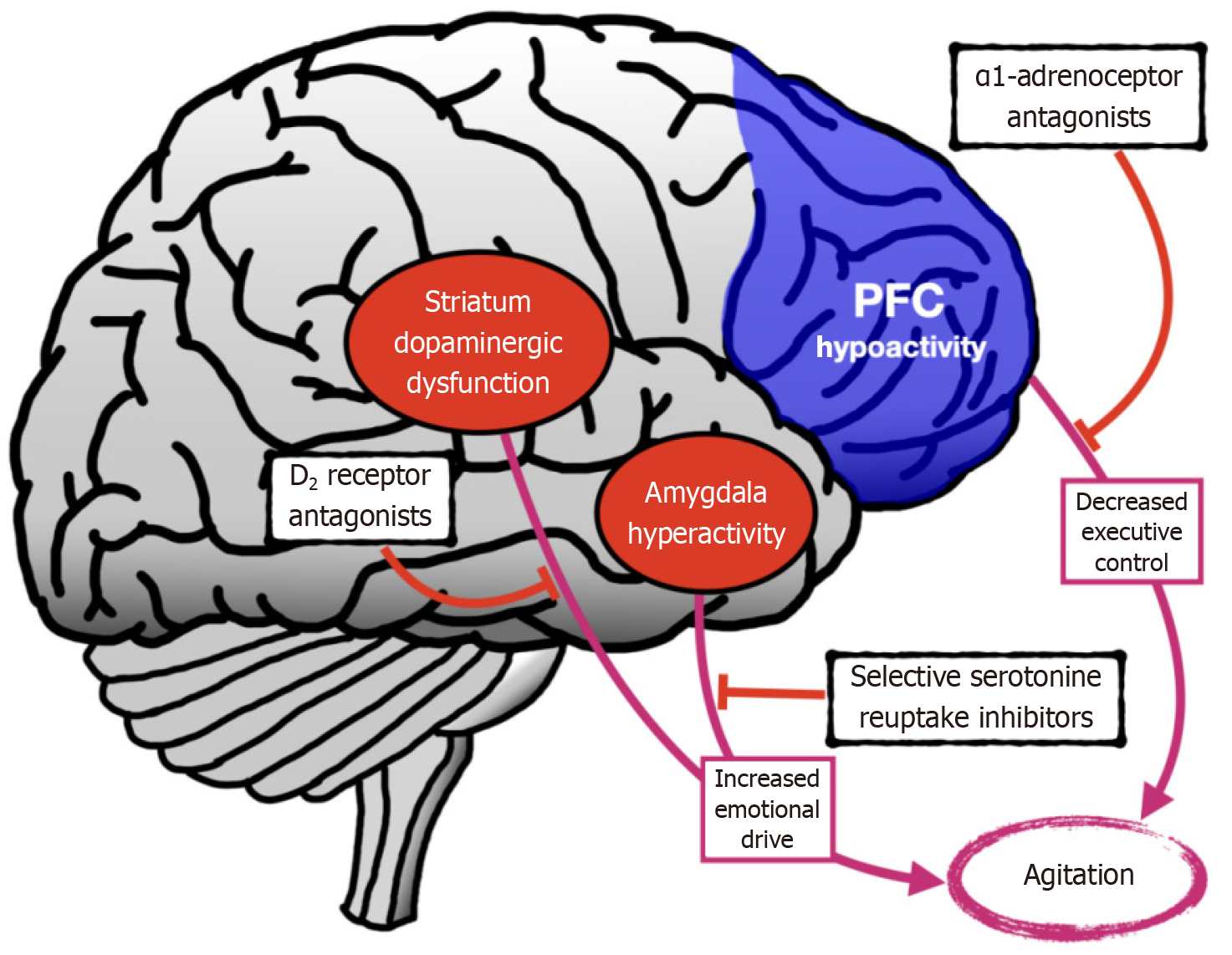
Figure 1 Neurobiological model of agitation depicting key brain regions and neurotransmitter systems.
Prefrontal cortex hypoactivity contributes to decreased executive control, while amygdala hyperactivity and striatal dopaminergic dysfunction increase emotional drive, collectively leading to agitation. Pharmacological targets include D2 receptor antagonists (antipsychotics) for dopaminergic dysfunction, selective serotonin reuptake inhibitors to reduce emotional drive, and α1-adrenoceptor antagonists (e.g., prazosin) to enhance executive control. Based on the model of agitation in Alzheimer’s disease proposed by Cummings et al[9]. SSRIs: Selective serotonin reuptake inhibitors; AD: Alzheimer’s disease.
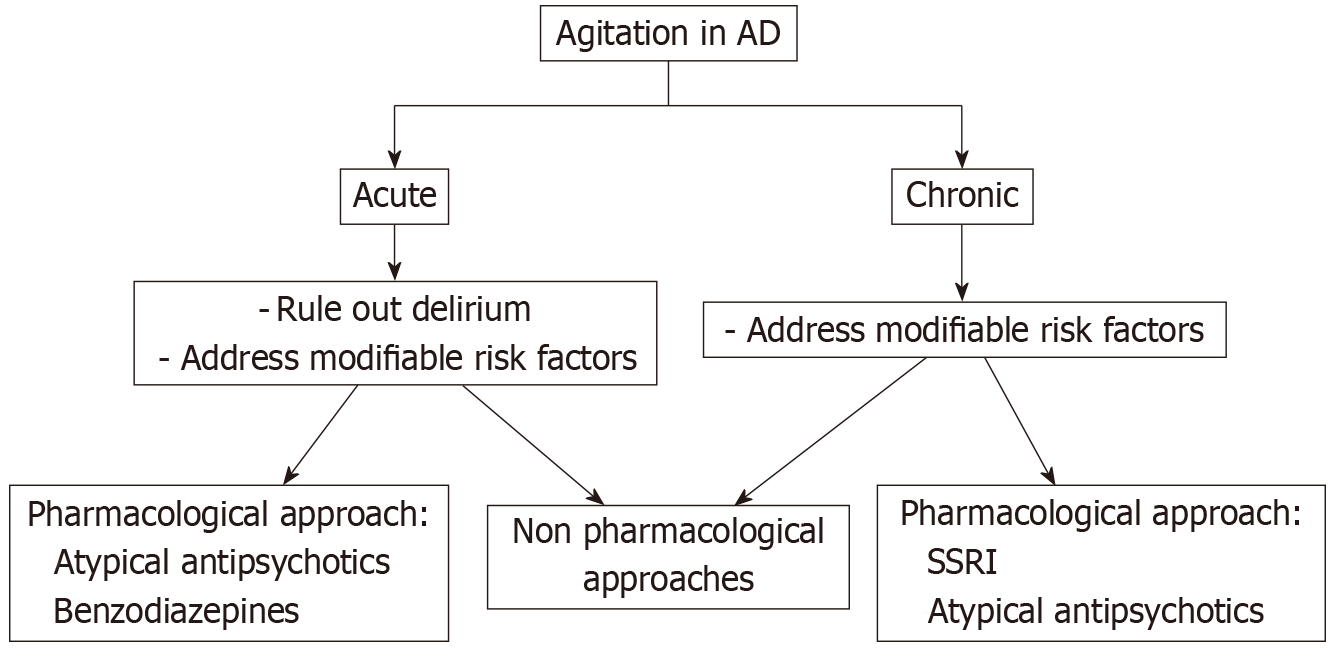
Figure 2 Flowchart outlining the management of agitation in Alzheimer’s disease.
Acute agitation requires ruling out delirium and addressing modifiable risk factors, followed by the consideration of atypical antipsychotics and/or benzodiazepines alongside non-pharmacological interventions. Chronic agitation also involves addressing modifiable factors, with treatment options including selective serotonin recapture inhibitors, atypical antipsychotics, and non-pharmacological approaches. PFC: Prefrontal cortex.
- Citation: Teixeira AL, Kim Y, Cordeiro TM, de Erausquin GA, Rocha NP. Agitation in Alzheimer’s disease: From assessment to therapeutics. World J Psychiatry 2025; 15(11): 109581
- URL: https://www.wjgnet.com/2220-3206/full/v15/i11/109581.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i11.109581